Introduction
The BCR-ABL-negative myeloproliferative neoplasms (MPN) including polycythemia vera (PV), essential thrombocythemia (ET), and myelofibrosis (MF) are closely related clonal hematopoietic stem cell disorders with shared molecular pathogenesis. MPN patients have a high risk of developing venous and arterial thrombotic complications []. Venous thrombotic events in MPN include deep vein thrombosis/pulmonary embolism (DVT/PE), as well as unusual site thrombosis such as splanchnic vein thrombosis (SVT) and cerebral vein thrombosis (CVT) [-]. The risk of MPN-related venous thrombosis is significantly high in the first 3 months following MPN diagnosis (hazard ratio [HR] 9.7 compared to the general population), but is also nonnegligible during follow-up (HR 3.2 at 5 years) []. According to previous reports, up to a third of the patients with MPN-related venous thrombosis will develop recurrent thrombotic episodes, often in the same vascular system previously involved [, -]. The prevention and treatment of venous thrombosis is a major goal in managing MPN patients. Based on the results from the ECLAP trial [], the majority of newly diagnosed MPN patients receive antiplatelet agents (most commonly low-dose aspirin) as primary prevention of thrombotic complications. In high-risk MPN patients, including those with a prior thrombotic event, guidelines advocate the use of cytoreductive agents to further decrease the risk of thrombotic complications. In contrast, there is no consensus regarding the management of MPN patients who developed venous thrombosis and no clear recommendations exist. Areas of uncertainty include the choice of an anticoagulation agent, the duration of anticoagulation treatment, whether a combination of an anticoagulant and an antiplatelet agent is better than single-agent therapy, and if there is a role for additional thrombophilia screening [-]. These uncertainties were reflected in a recent survey of 73 hematologists who treat MPN routinely, which found a significant heterogeneity in the use of anticoagulant and antiplatelet agents for MPN-related venous thrombosis [].
In the current study, we collected data on MPN patients with venous thrombosis treated in 10 Israeli medical centers. Our study objectives were to determine patient, disease, and treatment-related factors associated with the index thrombosis and with thrombosis recurrence.
Patients and Methods
Patients were recruited from 10 medical centers that are members of the Israeli MPN Working Group. Participating centers searched the electronic database of coded diagnoses for all adult patients with a definite diagnosis of a BCR-ABL-negative MPN and MPN-related venous thrombotic event. Patients who were in follow-up between the years 2005 and 2015, with baseline data and follow-up of at least 12 months after the index thrombosis, were included. MPN-related venous thrombosis was defined as a venous thrombotic event that occurred up to 2 years prior to MPN diagnosis or at any time thereafter. Index thrombosis was defined as the first MPN-related venous thrombotic event. Patients with minor occlusive events only, such as erythromelalgia and superficial vein thrombosis, were not included. Sites of thrombosis were categorized into DVT/PE, unusual site thrombosis (including SVT and CVT), and others (including genitourinary, retinal, and jugular vein thrombosis). Patients who had only arterial thrombotic events were not included in the study. However, patients having both venous and arterial thrombotic events were not excluded. Patients’ demographics, data on the specific MPN diagnosis, venous thrombosis-related variables, and outcomes were extracted from the manual and electronic medical records into a common Excel data sheet. Molecular and thrombophilia investigations were performed either at diagnosis or during follow-up when the respective test was not previously available.
Index thrombosis at diagnosis was defined as an index thrombotic event that occurred prior to and up to 30 days after MPN diagnosis, and index thrombosis at follow-up was defined as an index event that occurred >30 days after the diagnosis of MPN. Blood count control was defined when the patient’s hematocrit was ≤45% and the platelet count was ≤400 109/L. Thrombophilia testing included antithrombin III, protein C, and protein S, molecular tests for factor V Leiden and the prothrombin G20210A mutation, antibodies to cardiolipin and beta-2 glycoprotein, and a lupus anticoagulant assay. The study was approved by the local IRB committees.
Statistical Analysis
Categorical variables are reported as frequency and percentage. Continuous variables were evaluated for normal distribution and are reported as mean and standard deviation (SD) or median and interquartile range (IQR). Length of follow-up was observed using reverse censoring methods. The Kaplan-Meier method was used to demonstrate the rate of venous thrombosis recurrence during the follow-up period. Univariate Cox regression was used to determine the association between each potential predictor and venous thrombosis recurrence. All statistical tests were 2 sided, and p < 0.05 was considered as statistically significant. SPSS software was used for all statistical analyses (IBM SPSS Statistics for Windows, version 25; IBM Corp., Armonk, NY, USA).
Results
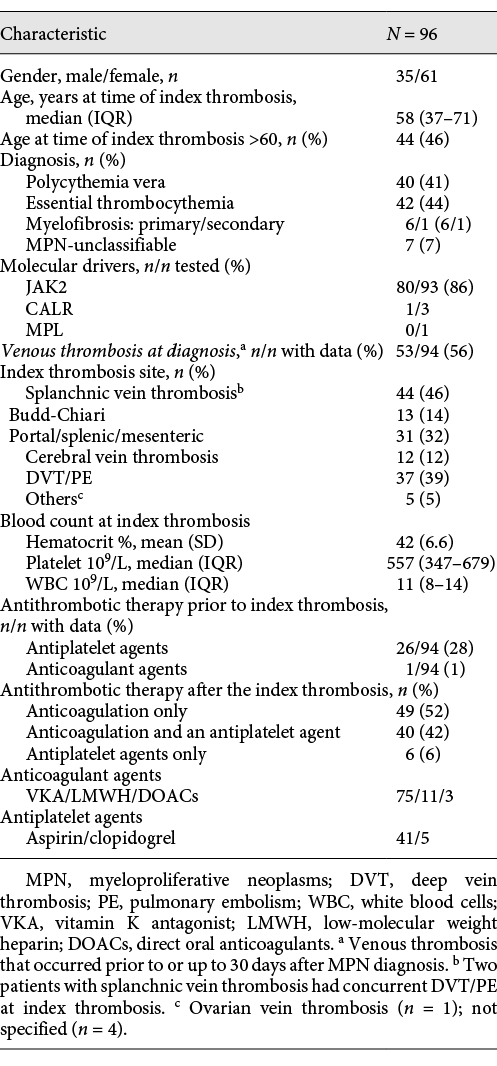
Ninety-six patients with MPN-related venous thrombosis were identified and are included in this report. Baseline characteristics of study patients are shown in Table 1. The median age at MPN diagnosis was 50 (IQR 36–67) years, and the median age at the time of index thrombosis was 58 (IQR 37–71) years. There were more females (n = 61) than males (n = 35) in the cohort. Sites of index thrombosis were DVT/PE in 35 (34%), unusual site thrombosis in 54 (56%), DVT/PE with concurrent unusual site thrombosis in 2 (2%), and other sites in 5 (5%) patients. Index thrombosis occurred at diagnosis in 53 (56%) and at follow-up in 41 (44%) patients. Blood counts were not controlled in 74 patients at the time of index thrombosis (85% of those with available data): 44/50 patients (88%) with index thrombosis at diagnosis and 30/37 patients (81%) with index thrombosis at follow-up (p = 0.38). Twenty-six patients (29%) were on an antiplatelet agent at the time of index venous thrombosis: 8/53 patients (15%) with index thrombosis at diagnosis and 18/41 (44%) with index thrombosis at follow-up (1 patient received a combination of an antiplatelet and an anticoagulant agent), p = 0.004. Compared to patients not receiving antiplatelet agents, a higher proportion of patients with index thrombosis receiving antiplatelet agents were older than 60 years (69% compared to 37%, p = 0.005). There was no significant difference in the rate of the specific MPN diagnoses, blood count control at the time of index event, and thrombophilia between these 2 subgroups of patients. The results were not significantly different when the index thrombosis was defined as at diagnosis and at follow-up by using the time points 2 years prior to MPN diagnosis up to 3 months or up to 30 days after MPN diagnosis (data not shown).
Thrombophilia was evaluated in 57 (59%) and was found in 16 patients (28% of tested). Identified thrombophilia included heterozygosity for the factor V Leiden mutation (n = 4), heterozygosity for the prothrombin G20210A mutation (n = 3), protein C deficiency (n = 2), protein S deficiency (n = 1), and positive antiphospholipid antibodies (n = 2). The nature of thrombophilia was not specified in 4 additional positive patients. There was a trend for a higher rate of thrombophilia in patients with index thromboses diagnosed 1-2 years prior to MPN diagnosis compared to index thromboses diagnosed from 1 year prior to and 30 days after MPN diagnosis and at follow-up, although the absolute numbers in the subgroups were small (2/3, 5/30, and 9/24 of patients screened for thrombophilia, respectively, p = 0.07). There was no significant difference in the rate of thrombophilia screening between older thrombotic events (before 2010) and more recently diagnosed events cases (after 2010) (25/41 vs. 32/55, p = 0.95).
Treatment of the Index Thrombosis
Data on antithrombotic therapy that was given following the diagnosis of MPN-related venous thrombosis were available in 95 patients and are shown in Table 1. Treatment included anticoagulation only (n = 49), a combination of an anticoagulant and an antiplatelet agent (n = 40), and single-agent antiplatelet (n = 6). The most frequently used anticoagulant was a vitamin K antagonist (VKA) (n = 75, 84%), followed by low-molecular weight heparin (n = 11, 12%) and direct oral anticoagulants (DOACs) (n = 3, 3%). Aspirin and clopidogrel were the antiplatelet agents used in 41 (89%) and 5 (11%) patients, respectively.
The majority of patients (n = 71, 75%) who continued treatment received long-term anticoagulation, defined as longer than 12 months following the thrombotic episode, and 18 patients discontinued treatment. The duration of treatment with anticoagulation in patients who stopped treatment was 3–6 months in 5, 6–12 months in 8, and was unknown in 5 patients. Reasons for discontinuing anticoagulation included control of MPN (n = 5), resolution of transient risk factors (n = 2), and bleeding (n = 1). Ten patients discontinued treatment for unknown reasons. Patients with DVT/PE were more likely to discontinue anticoagulation (8/32, 25%) compared to patients with unusual site thrombosis (7/52, 13%), but this difference was not statistically significant (p = 0.24). There was no difference in the rate of treatment discontinuation in patients either with or without thrombophilia (3/23, 13% and 4/32, 13%, respectively; p > 0.99).
Recurrence of Venous Thrombosis
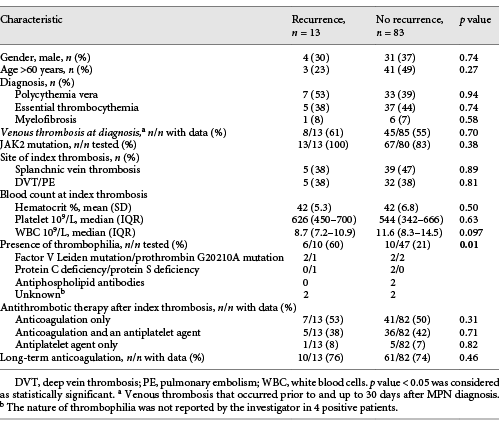
Recurrent venous thrombosis occurred in 13 patients (14%), resulting in an incidence rate of 2.36 per 100 patient-years. The median time between the index and recurrent events was 3.4 years (IQR 1.1–10). Site of recurrence was the same as the index thrombosis site in 6/13 cases (DVT/PE [n = 4] and Budd-Chiari [n = 2]). At the time of recurring event, most patients (12/13) were on antithrombotic agents including anticoagulants (n = 6), antiplatelet agents (n = 3), and a combination of an antiplatelet and an anticoagulant (n = 3). Blood counts were controlled in 7/13 patients at the time of recurrence. Patients with recurrent venous thrombosis were all JAK2V617F mutation positive.
Comparison between patients either with or without recurrence of venous thrombosis is shown in Table 2. Thrombophilia was significantly more prevalent in patients with recurrent venous thrombosis (6/10, 60%) compared to patients without recurrence (10/47, 21%; p = 0.01). There was no significant difference in the median age, gender, MPN subtype, antithrombotic agents given for the index thrombosis, and the use of long-term anticoagulation between patients with recurrent thrombosis and those who did not develop recurrence (Table 2).
Recurrent venous thrombotic events developed between 3 months and 32 years after the index thrombosis. To study if risk factors predisposing to an early or late venous thrombosis recurrence are the same, patients with recurrent venous thrombosis were subdivided into those with an early recurrence (defined as occurrence within 5 years from the index thrombosis, n = 8) and those with a late recurrence (defined as occurrence >5 years after the index thrombosis, n = 5). Features of patients with an early recurrence included a higher prevalence of thrombophilia (5/6 compared to 1/4 patients with a late recurrence), use of anticoagulation at the time of recurrence (7/8 compared to 2/5), and control of blood counts (6/8 compared to 1/5). 5/8 patients with early recurrence had controlled blood count and were on anticoagulation compared to 0/5 with late recurrence.
At a median follow-up of 4.9 years, 83 patients were alive. The thrombosis-free survival was 89.6% (SE 3.6%) after 5 years, 82.6% (SE 5.9%) after 10 years, and 62.9% (SE 13%) after 15 years (Fig. 1). Thrombosis-free survival was not significantly different between patients on long-term anticoagulation and those who stopped anticoagulation. No deaths occurred within 30 days of the index thrombosis. One patient died 10 days after a recurrent thrombotic event (PE). Median overall survival was not reached and was not different between patients either with or without recurrence of venous thrombosis (data not shown).
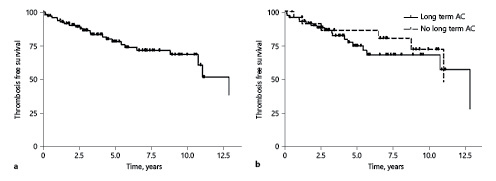
Fig. 1
Kaplan-Meier curves for (a) thrombosis-free survival in the whole cohort and (b) thrombosis-free survival in patients with or without long-term AC after the index thrombosis. AC, anticoagulation.
Discussion
In the current study, we found that following an episode of venous thrombosis, most MPN patients receive long-term anticoagulation (in combination with an antiplatelet agent in approximately half of the cases). Recurrence of venous thrombosis occurred in 14% of patients and was associated with thrombophilia, in particular when occurring in the first 5 years following the index thrombosis.
The clinical characteristics of patients enrolled in our study are similar to those of previously reported retrospective cohorts of patients with MPN-related venous thrombosis and include female predominance, median age at the index thrombosis younger than 60 years, a high prevalence of venous thrombosis occurring at diagnosis of MPN diagnosis, and a high rate of unusual site thrombosis [, , ]. Patients who were on antiplatelet agents at the time of index thrombosis tended to be older than patients who were not receiving antiplatelets at the time of index thrombosis. Importantly, we show that a majority of MPN patients with index thrombosis that occurred after the diagnosis of MPN (defined here as index thrombosis at follow-up) had uncontrolled blood counts at the time of event and were not receiving antithrombotic agents, in 81 and 56%, respectively. Furthermore, 46% of patients with recurrent thrombotic episodes had uncontrolled blood counts and 38% were not receiving anticoagulants at the time of recurrence. While some of the patients could have been in the low thrombotic risk category prior to the index thrombosis and therefore not eligible for cytoreduction; these high rates are also reflective of the difficulties in treating patients with chronic diseases including MPN, where patients’ compliance or suboptimal dosing are common clinical problems [].
The role of thrombophilia screening in the management of MPN patients is unclear. Current recommendations do not support routine thrombophilia screening in patients with MPN-related thrombosis, although such associations were described in several studies [-]. Thrombophilia in our study population was tested in 59% of patients, which is similar to screening rates in previous retrospective cohorts [, , , , , ]. We found that thrombophilia was significantly more prevalent in patients with recurrent venous thrombosis, especially those with an early recurrence. An association between thrombophilia and recurrent thrombotic episodes was also recently described in a cohort of ET and PV patients with venous or arterial thrombosis [].
There is no consensus on the use of antithrombotic agents in MPN patients with venous thrombosis. Key questions are whether anticoagulation should be used long term and if combinations of anticoagulant and antiplatelet agents should be used. Few retrospective studies addressed these questions. De Stefano et al. [] reported that 52% of patients with MPN-related DVT/PE received long-term VKA treatment. Patients who continued VKA had a significantly lower incidence of recurrent thrombotic episodes compared to patients who discontinued treatment []. Similar results were reported by Hernández-Boluda et al. and Wille et al. [, , ]. In contrast, there was no statistically significant difference in the rate of recurrence between patients with ongoing VKA treatment compared to patients off VKA in another study on MPN-related SVT patients. This could be due to a higher proportion of patients receiving long-term VKA treatment (75%) in that study [].
In our study, a relatively high proportion of patients (75%) received long-term anticoagulation and a significant number of the patients (n = 41) received a combination of an antiplatelet and an anticoagulant agent. We also could not detect a difference in venous thrombosis recurrence according to the different anticoagulant schedules.
Several guidelines advocate using prolonged anticoagulation in patients with unusual site thrombosis [, ]. Indeed, in the current cohort, only 13% of patients with unusual site thrombosis discontinued anticoagulation compared to 25% of patients with DVT/PE. These are lower rates of discontinuation compared to previous reports [, ] and could explain the relatively low rate of recurrence in our cohort.
While the rate of MPN-related venous thrombosis has decreased in recent years, possibly because of a more effective treatment [], venous thrombosis still recurs, even in patients receiving antithrombotic agents and cytoreductive therapy [, , , ]. Thirteen patients (14%) in our cohort developed recurrent venous thrombosis. Nine occurred in patients on long-term anticoagulation, 7 in patients with controlled blood counts, and 5 in patients with both controlled blood counts and on long-term anticoagulation.
We found that early recurrence was associated with a high rate of thrombophilia. These patients could represent a subgroup of patients with a very high thrombotic risk. Late recurrence was associated with uncontrolled blood counts or discontinuation of anticoagulation. This is probably reflective of the difficulties inherent treating patients with a chronic disease over long periods of time.
The limitations of the current study include the retrospective design, potential selection bias of the study cohort, and lack of data on the total MPN population. Rates of recurrent venous thrombosis could be biased by loss of patients with an early venous thrombosis recurrence who died prior to data collection. Few patients were treated with DOACS which are increasingly used nowadays. Data on thrombophilia were available only for a subset of patients, and positive finding could be overreported. We did not have data on the control of blood counts, as well as the INR, over the entire follow-up period.
In conclusion, we found that although a significant number of patients with MPN-related venous thrombosis remain on long-term anticoagulation, >10% had a recurrent event. We cautiously speculate that thrombophilia is a potential contributor to an early venous thrombosis recurrence and that suboptimal blood count control and discontinuation of anticoagulation could be related to late venous thrombosis recurrences. Thrombophilia testing could assist in personalizing the treatment of MPN patients with venous thrombosis and should be considered as part of future treatment recommendations. Prospective studies are needed in order to determine strategies to optimize management of MPN-related venous thrombosis.
Statement of Ethics
This study was approved by the local ethics committee and was conducted in accordance with the Declaration of Helsinki (IRB# 0119-15-ASF). Written informed consent was waived due to the retrospective nature of the study.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors did not receive any funding.
Author Contributions
N.L., M.E., and M.K.M. designed and performed the research. O.G. and M.K.M. analyzed the data and wrote the manuscript. M.B., A.D.A., A.L., E.C., N.D., S.P., and E.M. contributed to data acquisition and performed the research. All authors interpreted the data, took part in critical revision of the manuscript, and approved the final version of the manuscript.
References
- 1. Ball S, Thein KZ, Maiti A, Nugent K. Thrombosis in Philadelphia negative classical myeloproliferative neoplasms: a narrative review on epidemiology, risk assessment, and pathophysiologic mechanisms. J Thromb Thrombolysis. 2018;45(4):516–28.http://dx.doi.org/10.1007/s11239-018-1623-4
- 2. Smalberg JH, Arends LR, Valla DC, Kiladjian J-J, Janssen HL, Leebeek FW. Myeloproliferative neoplasms in Budd-Chiari syndrome and portal vein thrombosis: a meta-analysis. Blood. 2012;120(25):4921–8.
- 3. Martinelli I, De Stefano V, Carobbio A, Randi ML, Santarossa C, Rambaldi A, et al. Cerebral vein thrombosis in patients with Philadelphia-negative myeloproliferative neoplasms. An European Leukemia Net study. Am J Hematol. 2014;89(11):E200–5.http://dx.doi.org/10.1002/ajh.23809.
- 4. Akpan IJ, Stein BL. Splanchnic vein thrombosis in the myeloproliferative neoplasms. Curr Hematol Malig Rep. 2018;13(3):183–90.http://dx.doi.org/10.1007/s11899-018-0446-x.
- 5. Hultcrantz M, BjÖrkholm M, Dickman PW, Landgren O, Derolf ÅR, Kristinsson SY, et al. Risk for arterial and venous thrombosis in patients with myeloproliferative neoplasms: a population-based cohort study. Ann Intern Med. 2018;168(5):317–25.
- 6. Landolfi R, Di Gennaro L, Barbui T, De Stefano V, Finazzi G, Marfisi R, et al. Leukocytosis as a major thrombotic risk factor in patients with polycythemia vera. Blood. 2007;109(6):2446–52.http://dx.doi.org/10.1182/blood-2006-08-042515.
- 7. De Stefano V, Za T, Rossi E, Vannucchi AM, Ruggeri M, Elli E, et al. Recurrent thrombosis in patients with polycythemia vera and essential thrombocythemia: incidence, risk factors, and effect of treatments. Haematologica. 2008;93(3):372–80.http://dx.doi.org/10.3324/haematol.12053.
- 8. Elliott MA, Pardanani A, Lasho TL, Schwager SM, Tefferi A. Thrombosis in myelofibrosis: prior thrombosis is the only predictive factor and most venous events are provoked. Haematologica. 2010;95(10):1788–91.http://dx.doi.org/10.3324/haematol.2010.025064.
- 9. Hernández-Boluda JC, Arellano-Rodrigo E, Cervantes F, Alvarez-Larrán A, Gómez M, Barba P, et al. Oral anticoagulation to prevent thrombosis recurrence in polycythemia vera and essential thrombocythemia. Ann Hematol. 2015;94(6):911–8.http://dx.doi.org/10.1007/s00277-015-2330-2.
- 10. De Stefano V, Ruggeri M, Cervantes F, Alvarez-Larrán A, Iurlo A, Randi M, et al. High rate of recurrent venous thromboembolism in patients with myeloproliferative neoplasms and effect of prophylaxis with vitamin K antagonists. Leukemia. 2016;30(10):2032–38.
- 11. Landolfi R, Marchioli R, Kutti J, Gisslinger H, Tognoni G, Patrono C, et al. Efficacy and safety of low-dose aspirin in polycythemia vera. N Engl J Med. 2004;350(2):114–24.
- 12. Kreher S, Ochsenreither S, Trappe RU, Pabinger I, Bergmann F, Petrides PE, et al. Prophylaxis and management of venous thromboembolism in patients with myeloproliferative neoplasms: consensus statement of the Haemostasis Working Party of the German Society of Hematology and Oncology (DGHO), the Austrian Society of Hematology and Oncology (ÖGHO) and Society of Thrombosis and Haemostasis Research (GTH eV). Ann Hematol. 2014;93(12):1953–63.
- 13. Barbui T, Tefferi A, Vannucchi AM, Passamonti F, Silver RT, Hoffman R, et al. Philadelphia chromosome-negative classical myeloproliferative neoplasms: revised management recommendations from European LeukemiaNet. Leukemia. 2018 May;35(5):1057–69.
- 14. Network NCC, others. NCCN clinical practice guidelines in oncology. Myeloproliferative neoplasms. Version 2.2018. 2018.
- 15. De Stefano V, Rossi E, Carobbio A, Ghirardi A, Betti S, Finazzi G, et al. Hydroxyurea prevents arterial and late venous thrombotic recurrences in patients with myeloproliferative neoplasms but fails in the splanchnic venous district. Pooled analysis of 1500 cases. Blood Cancer J. 2018;8(11):65.http://dx.doi.org/10.1038/s41408-018-0101-8.
- 16. Ellis MH, Lavi N, Vannucchi A, Harrison C. Treatment of thromboembolic events coincident with the diagnosis of myeloproliferative neoplasms: a physician survey. Thromb Res. 2014;134(2):251–4.http://dx.doi.org/10.1016/j.thromres.2014.04.032.
- 17. Wille K, Sadjadian P, Becker T, Kolatzki V, Horstmann A, Fuchs C, et al. High risk of recurrent venous thromboembolism in BCR-ABL-negative myeloproliferative neoplasms after termination of anticoagulation. Ann Hematol. 2019;98(1):93–100.http://dx.doi.org/10.1007/s00277-018-3483-6.
- 18. Le Calloch R, Lacut K, Le Gall-Ianotto C, Nowak E, Abiven M, Tempescul A, et al. Non-adherence to treatment with cytoreductive and/or antithrombotic drugs is frequent and associated with an increased risk of complications in patients with polycythemia vera or essential thrombocythemia (OUEST study). Haematologica. 2018;103(4):607–13.http://dx.doi.org/10.3324/haematol.2017.180448.
- 19. Harrison C, Donohoe S, Carr P, Dave M, Mackie I, Machin S. Patients with essential thrombocythaemia have an increased prevalence of antiphospholipid antibodies which may be associated with thrombosis. Thromb Haemost. 2002;87(5):802–7.
- 20. Ruggeri M, Gisslinger H, Tosetto A, Rintelen C, Mannhalter C, Pabinger I, et al. Factor V Leiden mutation carriership and venous thromboembolism in polycythemia vera and essential thrombocythemia. Am J Hematol. 2002;71(1):1–6.http://dx.doi.org/10.1002/ajh.10153.
- 21. Gisslinger H, Müllner M, Pabinger I, Heis-Vahidi-Fard N, Gisslinger B, Brichta A, et al. Mutation of the prothrombin gene and thrombotic events in patients with polycythemia vera or essential thrombocythemia: a cohort study. Haematologica. 2005;90(3):408–10.
- 22. Tevet M, Ionescu R, Dragan C, LUPU AR. Influence of the JAK2 V617F mutation and inherited thrombophilia on the thrombotic risk among patients with myeloproliferative disorders. Maedica. 2015;10(1):27.
- 23. De Stefano V, Vannucchi AM, Ruggeri M, Cervantes F, Alvarez-Larrán A, Iurlo A, et al. Splanchnic vein thrombosis in myeloproliferative neoplasms: risk factors for recurrences in a cohort of 181 patients. Blood Cancer J. 2016;6(11):e493.http://dx.doi.org/10.1038/bcj.2016.103.