Introduction
Cervical pain is a problem with a high prevalence, affecting ~13% of the population, especially women (16.5%). The most affected age group is 65–74 years., In the different Spanish autonomous communities, including Madrid where this study was performed, osteomuscular pathologies of the neck and shoulders rank fifth or sixth among the 10 most prevalent chronic issues by age and gender, and their prevalence further increases when considering relapses throughout life. The aim of this study was to assess the effectiveness of acupressure applied in combination with standard treatment for the relief of cervical pain of benign origin. In spite of its benign origin and favorable evolution, mechanical cervical pain has a substantial economic and social impact and severely affects the quality of life (QoL) of millions of people, who are often incapable of working or even accomplishing the simplest of tasks without proper treatment.
Usual treatments delivered at healthcare centers for chronic or acute cervical pain normally consist of non-steroidal anti-inflammatory drugs (NSAIDs), but there is no evidence for their effectiveness. No differences have been observed between non-pharmacological treatments (training on pain handling, stress, performance of activities of daily life, pain relief, functional capability, or QoL) and placebo. Combining physical exercise with medication appears to influence treatment outcome. Studies estimating the effectiveness of acupressure for acute cervical pain have obtained better results than those using massage or placebo or transcutaneous electrical nerve stimulation (TENS) at 3 months, but this is not the case for chronic cervical pain in the long term., Kinesiology reduces recovery time by 7–23 weeks compared to usual pharmacological treatment and physical exercise, but with no noticeable differences at 1-year follow-up; compared with chiropractic, it further decreases pain at rest and increases mobility immediately after being applied. There are still no conclusive data on the effectiveness of TENS.
Finding an effective, satisfactory solution for the patient among usual treatments is difficult. The World Health Organization (WHO) has issued a call for public health systems to make the necessary cultural and regulatory changes to maintain the population’s wellbeing by reconciling different therapies with usual practice, including manual techniques and exercises, with or without medication, especially when conventional treatments fail, taking into account their effectiveness and safety.,
Scientific evidence on the effectiveness of acupressure is limited to a few clinical trials with limited casuistry, or deficient methodology., This trial, based on a pilot study by our research team,, attempted to provide answers to this question.
Methods
Patient and public involvement
Given the few existing clinical studies, usually with limited casuistry or poor methodology, scientific evidence for the effectiveness of the acupressure technique is limited. This project aimed to assess a complementary treatment relative to the usual practice offered during our medical consultations for cervical pain. A former intervention by our research group included organization of a total of four workshops (during which 46 patients were trained in the technique without any adverse effects reported) that showed a reduction in pain of 1–2 points. For these reasons, an intervention consisting of a complementary treatment was designed and administered in a healthcare center. A series of workshops were held, during which different professionals (doctors, nurses, pediatricians, clinical assistants, midwives, and administrative staff) were taught to apply a technique with static postures similar to Tui na to reduce osteomuscular pain. Older patients were also asked to participate since they could also potentially benefit from this method beyond only receiving usual treatment.
Setting and participants
Patients were recruited during nursing or medicine consultations for cervical pain. Included subjects provided written signed consent for participation and were randomly assigned to an intervention or control group by a computer program. Patients were not informed about data analysis, although information regarding the study outcome was provided upon request. Those not assigned to the intervention group were later offered the opportunity to learn the technique during a medical or nursing consultation, or to attend the workshops that have been held periodically since 2016 in these healthcare centers.
This was a controlled, clinical trial of a non-pharmacological intervention randomized by healthcare center. A pragmatic design was chosen to assess the effectiveness of the intervention, while taking into consideration the different ways to implement the technique under real practice conditions. The sample included patients between 18 and 65 years of age who attended primary care consultations at one of the 12 healthcare centers included in the study between 25 July 2013 and 31 August 2017 and provided written consent to participate. They were recruited by consecutive sampling after they reported suffering from cervical pain with muscle contracture and functional and postural limitations, but without structural damage or irradiation. Criteria for exclusion were: injury to the massage area (i.e. skin or osteomuscular damage, presence of and/or tendency to hemorrhage); chronic, severe, or decompensated disease; malignant illness or significant physical deterioration; mental disorders; sensory alterations; receipt of physiotherapy in the past month or intention to do so; use of analgesic medications described in the second and third rungs of the WHO analgesic pain ladder (e.g. codeine with or without acetaminophen, dihydrocodeine, dexketoprofen, tramadol, morphine, or fentanyl, alone or in combination with acetaminophen, metamizol, aspirin, or other NSAIDs); and difficulty reading or visual impairment hindering completion of the questionnaires.
Study physicians and nurses voluntarily engaged with the trial: five of them were already trained in acupuncture and all received training and materials on the intervention technique on at least one occasion at their work centers, which is similar to a pilot experience by our research group. In order to detect a decrease in pain of 1.5 points on the visual analogue scale (VAS) with a type I error rate of 0.05 and a power of 95%, and considering anticipated losses to follow-up of 20%, the sample size required was calculated to be 160 patients (80 in each group).
Patients who signed informed consent were allocated to the intervention or control group by simple random sampling automatically performed by the data collection notebook software. This software, which is based on PHP, jQuery and MySQL web technologies, was developed for this trial and allowed access from any browser independently of the device or operative system. A relational database was employed based on data from studies, consultations, and patients. After checking for inclusion and exclusion criteria, the patient was automatically included and randomly assigned to one study group. The system allowed for the data to be exported in .csv format for subsequent analysis.
Both groups were treated following usual practice, which, in the case of the intervention group, was supplemented by acupressure. This technique, based on the Tui na massage method, consisted of finding a hardened painful point on which a circular massage of 3–5 mm was applied with the fingers for a period of 5 s to 2–3 min, until the area reddened. The intention was for the patient to benefit from its relaxing effect and a decrease in resistance at the site of stimulation, as well as the production of neurotransmitters and substances including noradrenaline or adenosine, without suffering the pounding that is usually performed as part of the Tui na method. The painful point was then pressed and released bilaterally, starting at the most distal points. At certain points, such as the shoulders, the contralateral hand could be used. This maneuver was repeated 60 times per minute, with a pause every five. Supplemental Figure 1 describes the detailed, complex intervention in accordance with the proposal of Pereda et al. Acupressure was applied at the locations of the following traditional acupuncture points, stimulation at which is believed to have a beneficial effect on cervical pain: GV20 (Baihui), GB19 (Naokong), GB20 (Fenchi), GB21 (Jianjing), GB34 (Yangaglingquan), LI4 (Hegu), SI3 (Houxi), SI6 (Yanglao), SI9 (Jianzhen), SI10 (Naoshu), SI11 (Tianzong), SI12 (Bingfeng), SI13 (Quyuan), SI14 (Jianwaishu), SI15 (Jianzhongshu), and BL60 (Kunlun).
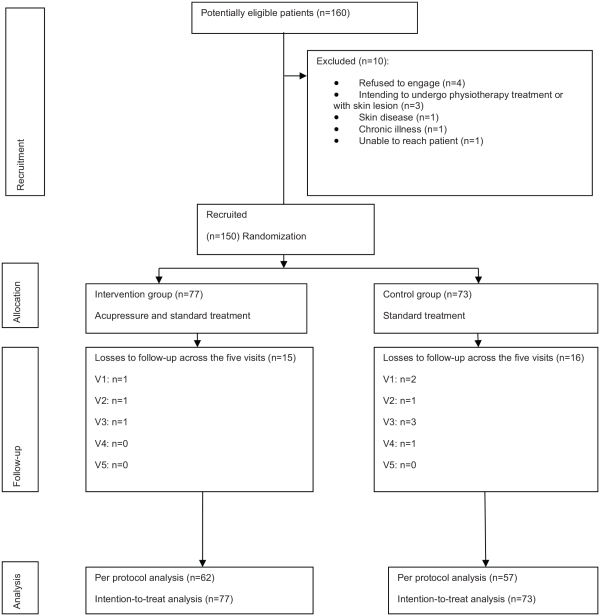
Figure 1
Flowchart of patients and losses to follow-up between baseline visit (V1) and subsequent visits at 3 days (V2), 7 days (V3), 30 days (V4), and 90 days (V5).
Outcome variables
The main outcome variable was pain intensity as measured on a 10-point, 10-cm-long VAS, where 0 stands for absence of pain and 10 for the worst conceivable pain. Secondary variables were: number and type of analgesics used, according to the WHO classification; the defined daily dose (DDD) in mg/day; adverse effects; QoL measured using EuroQol-5D; neck disability index (NDI); and days of temporary working disability. The following variables were recorded: socio-demographic (age, gender, educational level, work activity); clinical (previous cervical pain episodes during the past year, diagnostic tests, evaluation by specialized care); and previous treatment (pharmacological, physical). Upon completion of the study, participants in both groups were questioned about the professional that delivered the intervention, with respect to information provided and clarity of the explanation. Patients in the intervention group also answered questions regarding the technique and side effects.
Data analysis
Patients’ characteristics were analyzed in a multivariate model where the main independent variable was the intervention group and the dependent variable was the post-intervention change in pain, measured on the VAS. Continuous variables were defined by their measures of central tendency, dispersion, and mean with 95% confidence intervals (95% CIs). Discrete variables were described by the estimation of proportions with 95% CI. Independent measurements on the pain VAS at 1, 3, and 7 days (baseline visit V1 and follow-up visits V2 and V3, respectively) were compared between the two groups. In order to check if the effectiveness of the intervention persisted over time, measurements were repeated after 30 and 90 days (follow-up visits V4 and V5, respectively). Mean values were compared using a Student’s t-test or Mann–Whitney U-test. A generalized estimating equation (GEE) model was built to compare the evolution of pain measurements over time between groups, taking into account repeated measurements over time and the lack of independence between observations. The dependent variable was the change in pain between V1 and V5 measured on the VAS, and independent variables were the allocation group and subjects’ characteristics, including their baseline self-perception of QoL. A multilevel mixed model was built to explain the variability resulting from the professional (cluster) responsible for the patient’s training in the technique.
Both per protocol and intention-to-treat analyses were performed. For the cases where data from the pain VAS or QoL was missing, the last value provided by the patient (namely “last observation carried forward”) was used for the analysis. For the assessment of secondary outcome data, scores from the QoL questionnaires (days: 7, 30, and 90), mean number of days free of symptoms, and mean DDD of NSAIDs were compared between the intervention and control groups. This trial was approved by the Ethics Committee of Hospital Fundación Alcorcón de Madrid and the Central Board for Research in Primary Care on 28 February 2013, and was prospectively registered at ClinicalTrials.gov (NCT01855893) on 17 May 2013, prior to recruitment of the first participant on 25 July 2013.
Results
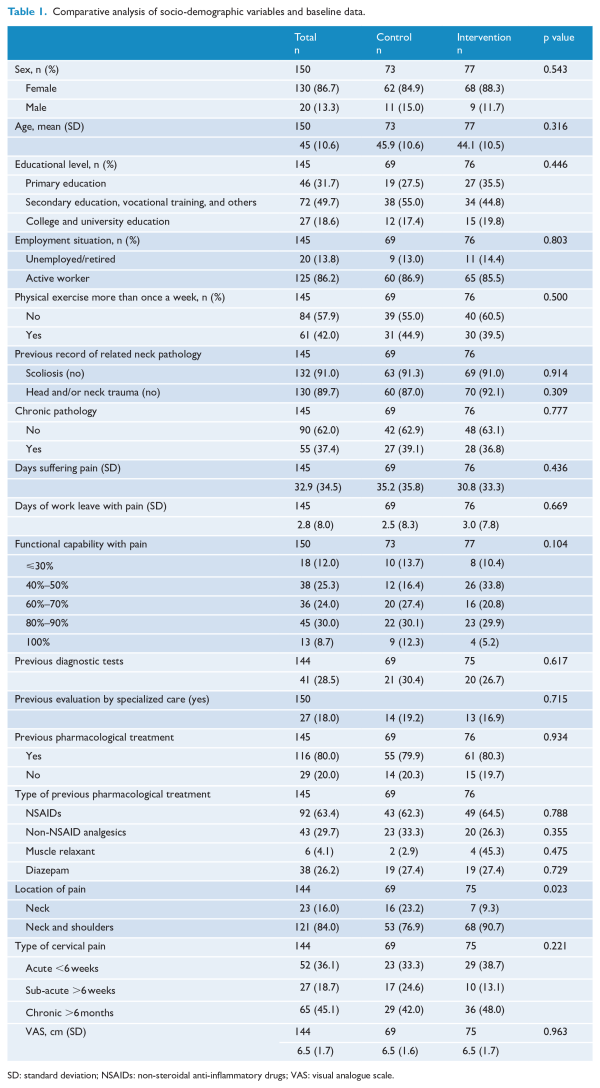
Of the 160 patients invited to participate, 150 agreed and 144 completed the five scheduled visits. No differences were observed between groups in terms of rates of study completion. Mean age was 45 years (SD: 1.06) and 86.7% were women. Table 1 describes the population characteristics, which were similar between groups at baseline. Figure 1 shows the flow of participants throughout the study.
The mean baseline value of pain was 6.5 points (SD: 0.13) on the VAS. No differences were observed between groups after 3, 7, and 30 days. However, a significant difference on the pain VAS was found after 90 days; VAS scores were 1.6 points higher (95% CI: 0.54–2.71) in the control group (Table 2). Immediately after patients in the intervention group received training in the acupressure technique, the majority (41%) reported lower levels of pain by 1–2 points on the VAS, 26% stated that they did not feel any change, and 8% experienced an increase in pain of 1–2 points.
In terms of QoL, utility values from the EuroQol-5D measured at 30 and 90 days did not significantly differ for intervention versus control groups (0.05 points; 95% CI: 0.00–0.09). The average number of patients that were prescribed medication after the first medical consultation differed between groups, being higher (p ≤ 0.01) for the control group (94%; 95% CI: 88.7–99.7) versus the intervention group (76; 95% CI: 66.3–85.7). Comparing the control and intervention groups, medication rates were: 73% (n = 50) versus 58% (n = 43) for NSAIDs (p = 0.058); 45% (n = 31) versus 27% (n = 20) for non-NSAIDs like acetaminophen and metamizole (p = 0.022); 19% (n = 13) versus 21% (n = 16) for relaxant-type drugs like cyclobenzaprine (p = 0.709); and 42% (n = 29) versus 23% (n = 17) for diazepam (p = 0.013). In terms of the type of prescribed pain relievers, there were no significant differences in the demand by patients between the groups across the five follow-up visits. In terms of inability to work, the impact of acupressure on the NDI was measured but no differences were found between groups (Table 2). Among subjects in the intervention group, 10% of the change observed on the pain scale along the follow-up visits was due to the recruiting professional in terms of the observed results of the technique on the first visit, prior acupuncture training, and their ability to transmit information, but not their personal characteristics.
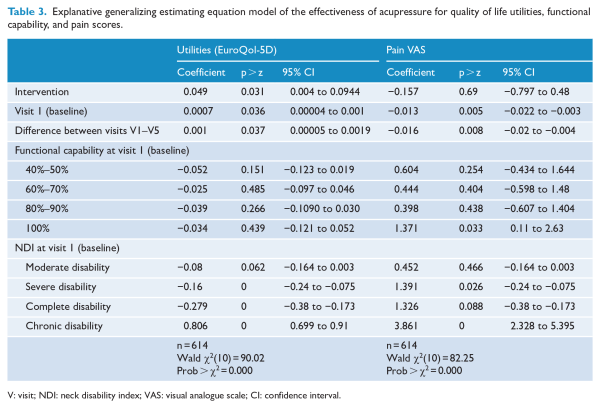
In the adjusted model (Table 3), the mean value of pain reported on the VAS by subjects in the intervention group was 0.16 points (95% CI: −0.80 to 0.48) lower than that in the control group (p > 0.05). In the acupressure group, the mean score on the pain VAS decreased 0.17 points (95% CI: −0.80 to 0.46) per intervention day, which did not significantly differ from that achieved by the control group. Individuals with a moderate, severe or complete degree of disability obtained a mean QoL utility index that was 0.09 (95% CI: −0.17 to 0.02), 0.16 (95% CI: −0.24 to −0.09), and 0.26 (95% CI: −0.35 to −0.17) points lower, respectively, than that of individuals who reported a low NDI at the baseline visit. After 90 days, the treatments’ effects on functional capability with pain and initial neck disability did not significantly differ between groups.
The final questionnaire about the health professional that informed patients about the intervention and their clarity of presentation was answered by 104 patients (69%), 37% of the intervention group, and 32% of the control group. Of these, 97% received the trial information from their general practitioner and 74% considered the presentation to be very clear. Fifty-six participants (70%) answered the relevant questions. Of them, 41 (73%) received the information from their family doctor, 40 (71%) thought it was very clear, and 32 (57%) considered the information from the support leaflet to be very clear. Finally, 43 (77%) considered the technique to be simple or very simple, 33 (59%) thought it was very useful, and 34 (61%) would recommend it.
Adverse effects
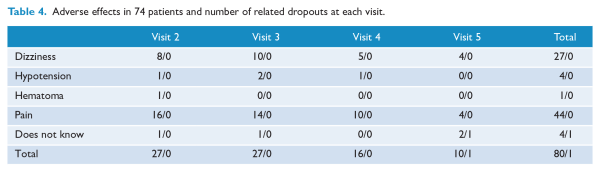
The intervention group was also asked about different aspects of the technique, including side effects, which were then checked by the research team. Four types of adverse effects were observed (pain, dizziness, hypotension, and hematoma at the site of pressure application), which usually appeared in combination in the same subject. Only one participant dropped out of the study (Table 4).
Discussion
Cervical pain is a pathology mainly present in adults, and women., Socio-demographic characteristics, personal background, and baseline anamnesis of patients in this study were similar to those already published by different authors.– The high level of engagement by participants, with only 5% loss to follow-up, must be highlighted.
This study was conducted under pragmatic conditions and involved a high number of professionals training patients in the applied technique. This resulted in high variability, with the professional accounting for 10% of the intervention’s effectiveness. Patients whose trainers had undergone at least two or three intervention workshops obtained better results, which should be taken into consideration for future implementation and application.
A similar reduction in pain without significant differences was observed in both groups in the short term. Even though no differences were observed between groups at follow-up visit V2, around 55% of patients in the intervention group experienced a pain decrease of 1–3 points on the VAS immediately after receiving the training (V1) (Figure 2), which can be explained by the fact that the intervention arm received less pharmacological treatment, although their treatment included both acupressure and medication. This may stem from overestimation of the potential effect of the intervention technique by some professionals after receiving the training and observing the first results, and in some cases due to the previous personal experience of acupuncture among the training professionals.
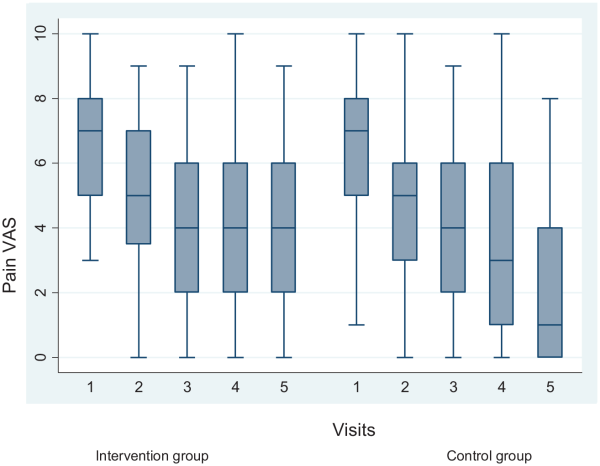
Figure 2
Evolution of pain in both groups measured on a visual analogue scale (VAS) at baseline visit (V1) and follow-up visits at 3 days (V2), 7 days (V3), 30 days (V4), and 90 days (V5).
At 90-days post-intervention, there was a difference of 1.63 points on the pain VAS in favor of the intervention group. This outcome is in agreement with other studies comparing different types of low-risk massage that did not find statistically significant differences among their effects. A literature review by Chou et al. (n = 190) noted that acupuncture was more effective than Swedish massage at decreasing pain (mean difference (MD) of 0.8 points on a 10-point VAS) and improving functional capability (MD of 7 points in the 0–100 scale Hanover functional ability questionnaire) in the short term. Another trial (n = 268) that compared massage techniques did not find differences between structural and relaxation massages (MD of 0.4 points) but observed different mean values of pain in terms of discomfort after application (~0.3 points on a 0–10 point scale). Other studies with smaller sample sizes (n = 26–140) also found small differences between massage techniques, with Chinese massage obtaining better scores. There are reviews on pharmacological treatments, postural interventions and physical exercise (like yoga) that were not able to determine the ideal treatment.
After examining the opinions of manual techniques reported by patients in the literature, these seem to be outlines on acceptability, mainly focused on effectiveness, as is the case for our study where 69% of subjects completed the final questionnaire. Patients thought the explanations of the technique were very clear (74%). Most of them considered it very simple and useful (76.7% and 59%, respectively), and 96.4% of them would recommend it.
Scientific literature suggests that health-related QoL is worse in patients with cervical pain compared to healthy individuals, although the power of this association differs between studies. Our trial found this difference in the utility index to be 0.63, which is similar to other studies of the same pathology, such as that of Stenberg et al., which obtained a EuroQol-5D utility value of 0.73. A study by Rezai et al. employed a population survey by mail to examine the association between the different levels of severity of cervical pain and QoL. Patients with levels II–IV of cervical pain reported a significantly worse QoL, both physical and mental, when compared to healthy individuals (MD CI 95%: −13.9 to −10.8).
A clinical trial by Jeitler et al. in patients with chronic cervical pain compared two groups during an 8-week intervention; one group did meditation (n = 18) whereas the other group followed a program of physical exercise (n = 16). In the meditation group, they found a reduction from 45.5 ± 23.3 mm to 21.6 ± 17.2 mm on a 100-mm pain VAS. The authors concluded that meditation with no physical activity achieves a reduction in pain, but does not improve disability measured using the NDI.
A study by Southerst et al. found evidence for different supervised programs of physical exercise being effective for handling cervical pain, although they were not able to determine the benefits of one program over another. The exercises were to be performed at home and included 12 different sitting postures. At 1-week post-intervention, the clinically significant differences between groups were 23.8 mm (CI 95%: 17.8–29.8) on the pain-at-rest VAS, 21.5 mm (CI 95%: 15.6–27.4) on the pain-on-movement VAS, 18.3 mm (CI 95%: 12.6–24.0) on the discomfort VAS, and 5.7 points (CI 95%: 4.2–7.3) in the NDI. Strength exercises alone were not more effective at decreasing pain, with a reduction of 17.7 mm on the pain VAS (CI 95%: 12.5–22.9) compared to baseline values. Differences in cervical pain and functional ability were clinically significant after 6 months, with improvements of 12.7% (CI 95%: 6.0–19.4) on the VAS. Another study also found differences when conducting physical therapy individually, like the intervention applied in our study, compared to group therapy.,
Our outcome is in agreement with a study by Carragee et al., which was a summary of scientific literature (1980–2006) assessing the evidence for non-invasive interventions to treat cervical pain and related disorders. In the case of non-benign cervical pain, the evidence suggests that manual interventions or supervised physical exercises, and perhaps acupressure, are more effective than no treatment or alternative interventions. However, none of the reviewed treatments were clearly more effective than the others, either in the short or long term, and they concluded by recommending further research focusing on strategies for preventing cervical pain in both society and work places.
Strengths and limitations
This study suggested that acupressure is an effective technique for improving cervical pain in the long term. In addition, it is easy to apply, has no significant adverse effects, and overall improved the QoL of patients more than pharmacological treatment with analgesics.
Among the limitations of the trial is the fact that it was difficult to isolate the placebo effect of the intervention. Even if the training on the technique was adequate, some patients may not have learnt or applied it according to the instructions given. This would likely have worked against the alternative hypothesis, minimizing the magnitude of effect of the intervention and potentially limiting our ability to demonstrate it. However, for the same reason, observing an effect of the intervention would further support its utility and, moreover, demonstrate effectiveness under realistic conditions.
Another limitation is the potential intergroup interference. Subjects who were trained in the intervention may have informed other patients who, in turn, self-applied the acupressure technique. To minimize this problem, and once the effectiveness of the intervention is established, workshops will be organized at every healthcare center.
Conclusion
Acupressure, used as a complementary therapy to usual practice, appeared to be an encouraging treatment option for cervical pain of benign origin in primary care that reduces pain and improved QoL utilities in the long term, but did not affect functional ability. It also failed to show short-term differences compared to usual practice. The participants considered the technique simple and easy to apply.
We would like to thank Jesús Martín Fernández and Gloria Ariza Cardiel (Multiprofessional Teaching Unit of Family and Community Care West) for his support for design. A Esperanza Escortell Mayor, Marcial Caboblanco Muñoz, Silvia Rodriguez Mireles, Isabel del Cura of the Research Support Unit of primary care management for their suggestions, comments, and support in the study analysis. And to the entire Research Unit for its support during the stay carried out by SCT with the Help to intensify the research activity FIIBAP. Clinical care group EDIDO—HC Becerril: MLTM, Alicia Martín López; HC Almendrales: Aurora García Lerín; HC Comillas: Olga García Vallejo; HC Maqueda: María Teresa Mingo Moreno; HC El Soto in Móstoles: Juan Carlos Muñoz García, Carmen Villar Velasco; HC Entrevías: Rocío López Recio; HC Martínez de la Riva: Pilar Marín Solano, Olga Nieto García; HC La Rivota: Julia Dorado Quesada, Inés Manzanas Ruiz; HC Sta Mónica de Alcorcón: PDS, Elena López Nogales, Arancha Cubero Muñoz, Jesús Bravo Rodriguez, Rocío Mateo Ciria; HC Dr Trueta in Alcorcón: SCT, Mª Trinidad García Alegre, Mª Angeles Blanco; HC Villanueva de Perales: Irina López Larrayoz, Pedro Pablo Sánchez de la Calle.
Contributors SCT, VMG, MLTM, and PDS conceived the trial and coordinated the field research at the healthcare centers (HC). SCT, JMF, and GAC designed the trial. The field research was conducted by the clinical care group EDIDO. SRM and IDC analyzed the data and collaborated with SCT to write the article. SCT, VMG, MLTM, and PDS provided relevant contributions to produce the results and discussion. All authors approved the final version of the manuscript accepted for publication.
Declaration of conflicting interests The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was financed by the Fondo of Investigaciones Sanitarias ISCIII (grant no. PI12/00203) and the European Regional Development Fund (ERDF) (“A way to build Europe”). SCT has recived a grant for the promotion of research activity by the Fundación for Investigación and Innovación Biosanitaria of Atención Primaria (FIIBAP) Call 2016. This article received a grant for the publication of from the Foundation for Biomedical Research and Innovation in Primary Care (FIIBAP) Call 2017 for grants to promote research programs.
Patient consent All patients signed informed consent.
Supplemental material Supplemental material for this article is available online.
References
- 1. Webb R, Brammah T, Lunt M, et al. Prevalence and predictors of intense, chronic, and disabling neck and back pain in the UK general population. Spine (Phila Pa 1976) 2003; 28(11): 1195–1202.
- 2. Calvo J, Collantes E. Protocolo diagnóstico de la cervicalgia inflamatoria. Medicine 2013; 11(31): 1949–1953.
- 3.
- 4.
- 5. Haines T, Gross A, Burnie SJ, et al. Patient education for neck pain with or without radiculopathy. Cochrane Database Syst Rev 2008; 8: CD005106.
- 6. Revel M, Minguet M, Gregory P, et al. Changes in cervicocephalic kinesthesia after a proprioceptive rehabilitation program in patients with neck pain: a randomised controlled study. Arch Phys Med Rehabil 1994; 75: 895–899.
- 7. Trinh KV, Graham N, Gross AR, et al. Acupuncture for neck disorders. In: The Cochrane Library: Issue 2, 2007. Chichester: John Wiley& Sons. Cochrane Database Syst Rev 2016; 11: CD004870.
- 8. Vas J, Perea-Milla E, Mendez C, et al. Efficacy and safety of acupuncture for chronic uncomplicated neck pain: a randomised controlled study. Pain 2006; 126: 245–255.
- 9. Witt CM, Jena S, Brinkhaus B, et al. Acupuncture for patients with chronic neck pain. Pain 2006; 125: 98–106.
- 10. Vernon H, Humphreys K, Hagino C. Chronic mechanical neck pain in adults treated by manual therapy: a systematic review of change scores in randomized clinical trials. J Manipulative Physiol Ther 2007; 30(3): 215–227.
- 11. Hoving JL, de Vet HC, Koes BW, et al. Manual therapy, physical therapy, or continued care by the general practitioner for patients with neck pain: long-term results from a pragmatic randomized clinical trial. Clin J Pain 2006; 22: 370–377.
- 12. Marti-nez-Segura R, Fernandez-de-las-Penas C, Ruiz-Saez M, et al. Immediate effects on neck pain and active range of motion after a single cervical high-velocity low-amplitude manipulation in subjects presenting with mechanical neck pain: a randomized controlled trial. J Manipulative Physiol Ther 2006; 29(7): 511–517.
- 13. Kroeling P, Gross A, Goldsmith CH. Electrotherapy for neck disorders. Cochrane Database Syst Rev 2007; 4: CD004251.
- 14.
- 15. Carragee EJ, Hurwitz EL, van der Velde G, et al. Treatment of neck pain: noninvasive interventions results of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Spine 2008; 33(4S): S123–S152.
- 16. Kurland HD. Treatment of headache pain with auto -acupressure. Dis Nerv Syst 1976; 37(3): 127–129.
- 17. Nguyen HP, Le DL, Tran QM, et al. A therapy advice system based on chrono-massage and acupressión using the method of ZiWuLiuZhu. Medinfo 1995; 8(2): 998.
- 18.
- 19. Mingxiao Y, Yue Feng HP, Shufang De, Minyu W, et al. Effectiveness of Chinese massage therapy (Tui Na) for chronic low back pain: study protocol for a randomized controlled trial. Trials 2014; 15: 418.
- 20. Perera R, Heneghan C, Yudkin P. Graphical method for depicting randomized trials of complex interventions. BMJ 2007; 334: 127–129.
- 21. Herdman M, Badia X, Berra S. El EuroQol-5D: una alternativa sencilla para la medición de la calidad de vida relacionada con la salud en atención primaria. Rev Aten Primaria 2001; 28: 425–430.
- 22. Fairbank JC, Cooper J, Davies JBJP, et al. The Owestry low back pain disability questionnaire. Physiotheraphy 1980; 66: 271–273.
- 23. León Vázquez F, González AB, Álvarez ACG, et al. Incapacidad Temporal. Manual Para El Manejo En Atención Primaria Gráficas Loureiro. Somamfyc Y AMAT 2008; 5: 75.
- 24. Hamer RM, Simpson PM. Last observation carried forward versus mixed models in the analysis of psychiatric clinical trials. Am J Psychiatry 2009; 166(6): 639–641.
- 25. Stenberg G, Lundquist A, Fjellman-Wiklund AC, et al. Patterns of reported problems in women and men with back and neck pain: similarities and differences. J Rehabil Med 2014; 46(7): 668–675.
- 26. Jeitler M, Brunnhuber S, Meier L, et al. Effectiveness of Jyoti meditation for patients with chronic neck pain and psychological distress—a randomized controlled clinical trial. J Pain 2015; 16(1): 77–86.
- 27. Kasumovic M, Gorcevic E, Gorcevic S, et al. Cervical syndrome: the effectiveness of physical therapy interventions. Med Arth 2013; 67: 414–417.
- 28. Rezai M, Cote P, Cassidy JD, et al. The association between prevalent neck pain and health-related quality of life: a cross-sectional analysis. Eur Spine J 2009; 18(3): 371–381.
- 29.
- 30. Southerst D, Nordin MC, Cote P, et al. Is exercise effective for the management of neck pain and associated disorders or whiplash-associated disorders? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Spine J 2016; 16: 1503–1523.
- 31. Antúnez Sánchez LG, De la casa Almeida M, Roldan JR, et al. Eficacia ante el dolor y la discapacidad cervical de un programa de fisioterapia individual frente a uno colectivo en la cervicalgia mecánica aguda y subaguda. Aten Primaria 2016; 49: 417–425.