Liposuction is one of the most commonly performed procedures in plastic surgery., Stimulated by the constant drive to improve patient outcomes, liposuction has dramatically evolved over the last several decades. Although it is generally considered a safe procedure with minimal risk of complications, it can be associated with significant drastic sequelae, which can lead to litigation. In this viewpoint, the authors set out to analyze all liposuction-related litigation from a medicolegal standpoint with the goal of identifying patterns and recommendations that can help surgeons avoid legal problems.
The 2 largest online legal databases, LexisNexis (RELX Group, London, United Kingdom) and Westlaw (Thomas Reuters, Toronto, Ontario, Canada), were searched to retrieve all legal cases associated with liposuction or fat grafting. The search strategy included the following keywords: “liposuction,” “negligence,” “contract,” “malpractice,” and “informed consent” linked by BOOLEAN terms. All search entries were reviewed by the authors (with legal and medical backgrounds) to determine the plaintiff’s (patient) and defendant’s (surgeon) demographics, procedural history, main complaint(s), judicial decisions, and appeals when applicable. The cases pending in court or ones that have been remanded were excluded. In addition, cases concerning non-medical matters, or ones where a physician was not a defendant, were also excluded. The American Board of Medical Specialties (ABMS) certification database was utilized to determine whether a defendant was board certified.
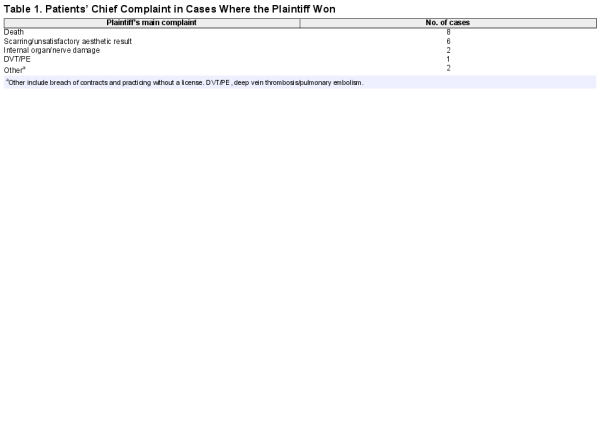
A total of 86 medical legal cases associated with liposuction were retrieved and included in this analysis, of which 50 were primary claims directly related to injury after liposuction and 36 were appeals. The cases originated from 21 different states and ranged from 1990 to 2019. The 3 states with the highest number of claims were New York (n = 10; 20%), California (n = 8; 16%), and Texas (n = 7; 14%). The majority of the plaintiffs were females (n = 43; 86%) and the majority of the defendants were males (n = 38; 76%). Liposuction involving the abdomen was the most commonly litigated procedure (n = 21; 42%), followed by thighs/gluteal area (n = 14; 28%) (Figure 1). The majority of judicial decisions were in favor of the defendant (n = 32; 64%). Furthermore, expert witnesses were present in the majority of the cases (n = 35; 70%). However, their presence was not a predictor of a judicial decision in favor of either party (P = 0.22). Of the 19 cases that were ruled in favor of the plaintiff, patient death was the most common chief complaint (n = 8; 42%), followed by unsatisfactory aesthetic outcome (n = 6; 32%) (Table 1).
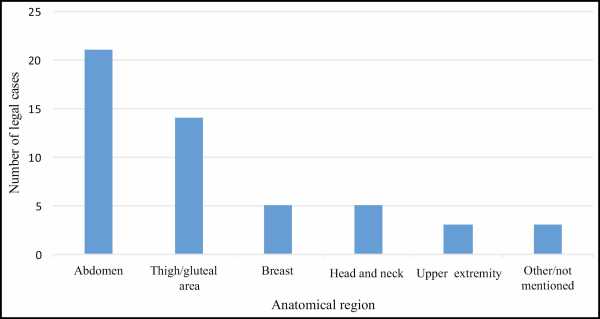
Figure 1
Number of legal cases associated with liposuction stratified on anatomical region.
A closer look at the defendants’ credentials shows that approximately one-half of the defendants (n = 23; 46%) were not board certified by an ABMS board. All 23 non-ABMS board–certified surgeons were males. Among these cases, liposuction involving the abdomen was the most commonly litigated procedure (n = 9; 39%), followed by the thigh/buttock area (n = 5; 22%). Approximately one-half (n = 10; 44%) of the initial judicial decisions in cases against non-ABMS board–certified physicians favored the patient. One-half of these cases were related to death (n = 3; 30%) or internal organ/nerve damage (n = 2; 20%).
A total of 36 cases (72%) were appealed; 14 were appealed by the surgeon, and 22 were appealed by the patient. Interestingly, although the majority of appeals resulted in the same decision as the initial ruling, surgeon appeals were significantly more likely to result in overturning of the initial decision. Specifically, 5 of the 14 cases appealed by the surgeon resulted in an overturn of the initial ruling in favor of the surgeon, whereas only 2 out of the 22 patient appeals resulted in an overturn in the judicial decision in their favor (P = 0.0005). Finally, the average monetary value awarded to plaintiffs was 1,446,652 ± 1,304,490 USD (range: 50,000-3,790,436).
Medical malpractice associated with liposuction and fat grafting has been a recent hot topic, particularly after the surge in associated severe complications such as pulmonary emboli and death. The lack of informed consent has been previously shown to be one of the main reasons why patients sue their doctors. Informed consent is a dynamic process that involves educating patients of the risks, benefits, and alternative treatments of a particular surgery/procedure and is influenced by patients’ characteristics and base knowledge. Factors such as health literacy and different cultural backgrounds can hinder patients from fully comprehending all aspects of informed consent. Although liposuction is generally a complication-free procedure with excellent aesthetic outcomes, our analysis shows that most litigation associated with it is due to major complications (death, internal organ damage, or emboli) or an unsatisfactory appearance (usually due to skin dimpling). Therefore, we highly recommend plastic surgeons to invest adequate time preoperatively to explain these uncommon but devastating complications. Physicians must do so while taking into account their patients’ cultural backgrounds and health literacy, which will undoubtedly improve the patient-surgeon relationship and decrease malpractice litigation.
Disclosures
Dr Janis receives royalties from Thieme Medical Publishers (New York, NY) and Springer Publishing (New York, NY). The other authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
- 1. Housman TS, Lawrence N, Mellen BG, et al The safety of liposuction: results of a national survey. Dermatol Surg. 2002;28(11):971–978.
- 2. Cárdenas-Camarena L, Andrés Gerardo LP, Durán H, Bayter-Marin JE. Strategies for reducing fatal complications in liposuction. Plast Reconstr Surg Glob Open. 2017;5(10):e1539.
- 3. Mofid MM, Teitelbaum S, Suissa D, et al Report on mortality from gluteal fat grafting: recommendations from the ASERF task force. Aesthet Surg J. 2017;37(7):796–806.
- 4. Therattil PJ, Chung S, Sood A, Granick MS, Lee ES. An analysis of malpractice litigation and expert witnesses in plastic surgery. Eplasty. 2017;17:e30.
- 5. ElHawary H, Salimi A, Gilardino MS. Ethics of facial transplantation: the effect of psychological trauma associated with facial disfigurement on risk acceptance and decision making. Ann Surg. 2020; doi: 10.1097/SLA.0000000000004156 [Epub ahead of print].
- 6. Barton N, Janis JE. Missing the mark: the state of health care literacy in plastic surgery. Plast Reconstr Surg Glob Open. 2020;8(5):e2856.