INTRODUCTION
Penile prosthetic devices are the primary treatment for medication for refractory erectile dysfunction (ED). These devices come in various forms, such as the malleable penile prosthesis (MPP) and the two-piece and three-piece inflatable penile prostheses (IPPs). IPPs have been in use for over four decades. Recent research indicates that IPP devices account for the vast majority (96.2%) of penile prostheses implanted in the USA, with MPPs comprising the rest. Several studies have demonstrated high satisfaction rates among patients and their partners when ED is treated with a penile prosthesis.
Conditions contributing to ED, such as Peyronie’s disease (PD), corporal fibrosis from priapism, and treatments for prostate cancer (e.g., radical prostatectomy), are known contributors to penile shortening. These not only affect penile length but also significantly impact patients’ quality of life. Notably, up to 80% of PD patients report a perceived reduction in penile length, which adversely affects their emotional well-being, self-esteem, and intimate relationships. IPP insertion does not typically change the stretched penile length, though patients often report subjective loss, impacting metrics such as the International Index of Erectile Function (IIEF) and Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS). Despite this, patients experiencing penile shortening along with severe ED can find relief through penile lengthening surgical techniques performed during penile prosthesis insertion. Various techniques to maintain or enhance penile length and girth during IPP and MPP insertion have been documented in the literature and are discussed in detail in this review.
A comprehensive literature search was performed using PubMed, to identify peer-reviewed articles on penile implants with cosmetic surgery. Medical Subject Heading (MeSH) terms and keywords such as “Penile Prosthesis corporal length”, “Inflatable Penile Prosthesis and short penis”, “Buried Penis”, “Inflatable Penile Prosthesis and hyaluronic acid”, “Inflatable Penile Prosthesis and penile fibrosis”, “functional outcomes”, and “satisfaction outcomes” were used. No date limits were imposed. Case series, as well as review articles, were included. The search was restricted to English papers. Animal studies were excluded.
The review prioritized articles from the past decade to provide current information, while also considering older, highly referenced studies. The reference lists of articles identified by this search strategy were also reviewed, and the working group selected relevant references. The authors reviewed the relevant published literature up to March 2024 for inclusion in this narrative review. Each publication was reviewed by at least two reviewers (MLR and MAI), and when there was no consensus, a third reviewer (JRO) decided on its inclusion.
PENILE PROSTHESIS PLACEMENT TECHNIQUES MAXIMIZE CORPORAL LENGTH
Cavernosal sparing and channeling without dilatation
Cavernosal sparing and channeling without dilation aim to preserve penile vascular integrity and maximize postoperative stretched penile length. Cavernosal tissue sparing during penile prosthesis implant surgery, achieved through minimal dilation of the corpora (with an 8 Fr dilator), has been shown to enhance spontaneous penile tumescence, girth, and postoperative stretched penile length.
Studies have demonstrated that minimal dilation of the corpora results in better preservation of cavernosal tissue, potentially improving both penile length and patient satisfaction.
Moncada et al. were among the first to report on the benefits of this approach and observed significantly greater penile length immediately postoperatively, as well as at 3 months and 6 months, in the group undergoing cavernous sparing technique compared to the group undergoing the classic technique (P < 0.05). They also noted an improvement in the mean IIEF scores at 3 months postoperatively in patients who underwent corporal preservation versus classic technique (12 [range: 10–14] vs 7 [range: 6–8]). Zaazaa et al. evaluated the penile hemodynamic response to phosphodiesterase type 5 inhibitors after cavernosal sparing inflatable penile prosthesis implantation. A penile dynamic Doppler ultrasound study was conducted by a blinded operator, at 4–6 weeks postimplantation. A cavernosal artery was successfully probed in 16 out of 17 (94%) patients in the cavernosal-sparing group, compared to 5 out of 16 (31%) patients in the conventional group, showing a significant statistical difference (P = 0.001). This indicated that the cavernosal sparing technique outperforms the conventional approach in preserving the cavernosal artery, thus maintaining some residual erectile function and leading to increased penile girth.
Subcoronal incision with circumferential penile degloving
Long-standing ED can lead to loss of penile length, but also can lead to loss of elasticity due to corporal fibrosis. As a result, dartos fascia tethering the underlying tunica albuginea can occur. In theory, this dartos fascia may have inherent restrictive properties that limit lengthening of the tunica albuginea.
The subcoronal approach to penile prosthesis placement has been thoroughly described by Weinberg et al. In their experience, two hundred men underwent IPP placement through a subcoronal incision using a modified no-touch technique. The penis was degloved to the level of the penoscrotal junction, and the dartos muscle was everted and secured to the drapes, effectively excluding the scrotal and penile skin from the operative field. The subcoronal incision provides access to the entire length of the tunica albuginea, allowing for penile modeling, plication stitches, relaxing incisions, and glans fixation to correct any abnormal curvature or hypermobile glans. In this series, the authors noted that patients experienced an average penile length gain of 0.6 cm (from 12.5 [range: 9 –16.5] cm preoperatively to 13.1 [range: 9.1–17.2] cm at 6 months of follow-up; Table 1), and 44% of patients received adjunct procedures due to Peyronie’s disease. Therefore, the chosen surgical approach can significantly impact penile length following IPP placement.
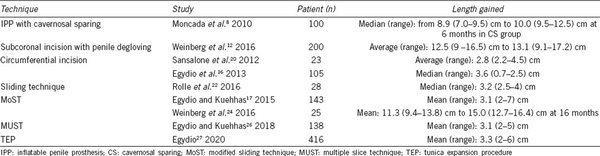
Table 1
Results from different techniques of penile lengthening
CONCURRENT PENILE PROSTHESIS IMPLANT AND CORPORA CAVERNOSA LENGTHENING
Several advanced surgical techniques and adjuvant maneuvers to increase penile length during penile prosthesis insertion have been described in the literature. They include circumferential incision of the tunica albuginea with graft implantation, the sliding technique with a double dorsal-ventral approach, the modified sliding technique, and the multiple slice technique.
These lengthening surgeries are mainly indicated in patients with severe penile shortening secondary to PD. They require aggressive mobilization of neurovascular bundles and urethra, incision and/or excision of coexisting penile plaque, and complete transection of corpora to stretch the penis to the maximum corrected length. The maximum length gain is likely limited by the elasticity of the neurovascular bundles and the urethra. The complete disassembly of the penis and the tension applied on the vascular bundle and the urethra may lead to severe complications such as glans ischemia and eventually necrosis. Therefore, patients undergoing this kind of surgery should be carefully selected and properly counseled.
Circumferential incision
Egydio et al., Egydio and Kuehhas, and Wilson et al. have extensively described this technique of circumferential incision. The circumferential technique has been largely abandoned as long as the reconstructed penis presents a reduced axial rigidity that may result in a higher risk of IPP aneurysm, herniation, or, eventually fracture.
Surgery is carried out through a combined subcoronal and penoscrotal approach to guarantee adequate exposure of the penile shaft. Once Buck’s fascia and urethra have been completely dissected off the corpora, a full erection is induced with saline solution injection (Figure 1a). Then, a circumferential incision of the tunica albuginea is then carried out at the point of maximum curvature, and the width of the tunica defect is measured on the convex and concave aspect of the shaft with the penis fully stretched (Figure 1b).
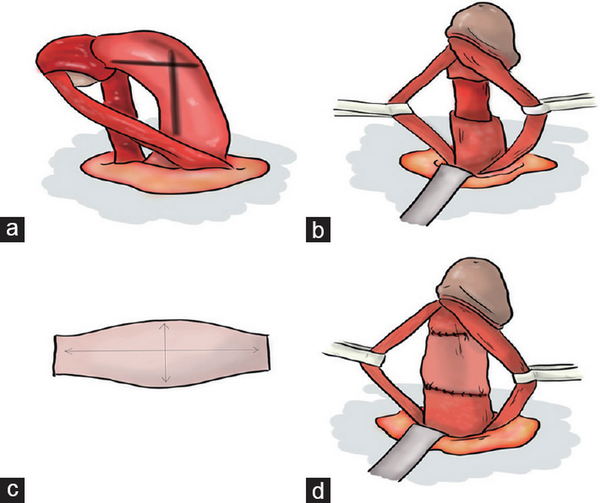
Figure 1
(a) Once Buck’s fascia and urethra have been completely dissected off the corpora, the point of maximum curvature is identified after induction of an artificial erection. (b) A circumferential incision is carried out at the level of maximum curvature, and the dimension of the defect is measured with the penis in traction. (c) The graft presents a trapezoidal shape with large width at the level of maximum curvature. (d) The tunical defect is covered with the graft that is sutured with graft.
Tunica defects have to be covered with a patch. The election of the material depends on surgeon preference and/or experience, as long as none have demonstrated superiority against others. The only clear principles are that synthetic grafts should be avoided. To avoid herniation of the prothesis, graft should be attached to the remaining albuginea with continuous 4-0 absorbable sutures (Figure 1c and 1d).
Both corpora cavernosa are then dilated through two proximal paraurethral corporotomies, and cylinders of prosthesis are inserted. When placing an IPP, the cylinders are inflated to around 80% of maximum capacity to confirm the straightening of the penis. The procedure is then completed with the closure of Buck’s and Dartos’ fascias and replacement of the skin.
Egydio et al. published their results of 105 men. The mean functional penile length gain was 3.6 (standard deviation [s.d.]: 0.7; range: 2–5) cm. Patient satisfaction with penile length gain was 95.2% and no major complication was recorded. Furthermore, Sansalone et al. reported their findings on 20 patients, with an average length gain of 2.8 (range: 2.2–4.5) cm. Recorded patient complications included diminished glans sensitivity in 4 (20%) patients and persistent dorsal curvature of <15° in 3 (15%) patients.
Sliding technique
For the first time, Rolle et al. described this modification of the circumferential enlargement technique in 2012. The approach is also through a combined subcoronal and penoscrotal incision, degloving the skin and penile fascias to achieve the exposure of the entire penile shaft. After that, neurovascular bundle is isolated circumferentially for the length of the penis (penopubic junction to coronal sulcus). After creating an artificial erection (while also instilling the corpora with lidocaine), the corpus spongiosum is mobilized off the corpora cavernosa from the corona to the proximal penis.
Both corpora cavernosa are then marked for the proposed incisions. The length of the incision should be adapted to the possible stretching of the neurovascular bundle. A gain of 3–4 cm lateral incision is usually obtained. With the penis stretched, a semicircumferential line is marked on the ventral surface of the corpora 2 cm proximal to the coronal sulcus (ventral incision is distal). The line should extend from the 3-o’clock position to the 9-o’clock position on the corpora. A second semi-circumferential marking is created on the dorsal corpora, 1–2 cm distal to the penoscrotal junction (dorsal incision is proximal). The semicircular lines are connected by longitudinal lines on the lateral aspects of both corpora cavernosa (3-o’clock and 9-o’clock positions).
After incision and dissection of the tunica albuginea from the cavernous tissue and from the septum, a gentle traction is applied on the glans, causing a slide of the distal part of the penis from the proximal one (Figure 2a). The stretching is stopped when the neurovascular bundle reaches the maximum length. Two 3/0 absorbable sutures are applied between the two lateral portions of the albuginea still mated. Two rectangular and bow-shaped defects of tunica albuginea remain: the first one, dorsal and proximal, and the second one, distal and ventral. From the proximal part, dilation of both corpora cavernosa and the measurement of their length are performed. This dilation can be easily performed without the risk of longitudinal traction on the neurovascular bundle or urethra, as the distal and proximal parts of the penis are well established by the sutures on the two longitudinal incisions previously applied. The two cylinders of the prosthesis are easily inserted in the two corpora cavernosa. The two losses of substance were then covered with two rectangular grafts (Figure 2b). In the case of an IPP implantation, it is suggested to place the double dorsal-ventral patch graft before inserting the two cylinders in the corpora cavernosa to prevent the risk of damaging them.
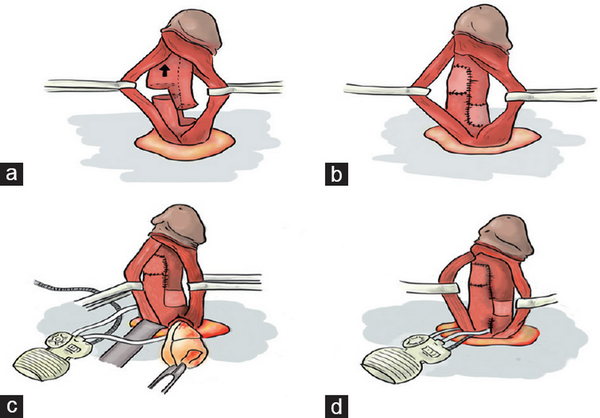
Figure 2
(a) Sliding technique. The stretching (in the direction of the arrow) is arrested when the neurovascular bundle reached the maximum length. (b) The two losses of substance are covered with two rectangular grafts. (c) Insertion of the prosthesis in modified sliding technique. (d) Proximal corporotomies are closed using the stay sutures.
In 2016, Rolle et al. reported results from a multicenter series of 28 patients, where postoperative functional data showed a progressive improvement in the score of all questionnaires, peaking at 12 months postoperatively. The median penile lengthening was 3.2 (range: 2.5–4) cm, and no patient reported recurrence of the curvature.
Modified sliding technique (MoST)
The so-called MoST combined with penile lengthening with urethral mobilization and neurovascular bundle followed by IPP placement, is performed using the same technical principles as the sliding technique, but just through a single subcoronal incision (Figure 2c and 2d). The concept of splitting a larger defect into two smaller ones moved Egydio et al. toward elimination of grafting altogether. While retaining the essential elements of the sliding technique, they made two key modifications: (1) utilization of complementary longitudinal ventral and/or dorsal tunica incisions for girth restoration and (2) avoidance of grafts by covering of the tunica defects with Buck’s fascia only. The MoST technique eliminated grafts, saved time, and decreased infection risk and cost of surgery.
Egydio et al. performed this procedure on 143 patients (133 MPP and 10 IPP) patients with an average length gain of 3.1 cm. In a multicenter series of Weinberg et al. with a cohort of 65 patients, curvature, when present, improved by 90%–95% and postoperative length increased by 3.6 (interquartile range [IQR]: 1.8–5) cm. Regrettably, while conducting both the sliding technique and its variant, the MoST technique, surgeons observed an exceedingly rare complication of prosthesis surgery–glans ischemia and consequent glans necrosis. A seminal publication in 2017 compiled 21 cases of this catastrophic condition from 8 centers across 5 countries. According to this report, 33% of patients underwent some form of the sliding technique.
Multiple slice technique (MUST)
The MUST is an evolution of the aforementioned techniques. The main difference is that both the sliding technique and the MoST form two wide tunical gaps that must be covered with a graft attached to the albuginea; whereas in the MUST, multiple smaller tunical defects are made to achieve the result (Figure 3). Egydio and Kuehhas reported results of 138 patients underwent the procedure. In PD cases, the mean deviation of the penile axis was 55° (range: 0°–90°). Mean subjective penile length loss reported was 3.1 (range: 2–7) cm, and shaft constriction was present in 44.9% cases. Median follow-up was 15.2 (range: 6–36) months. Mean penile length gain was 3.1 (range: 2–5) cm. No penile prosthesis infection caused device explanation.
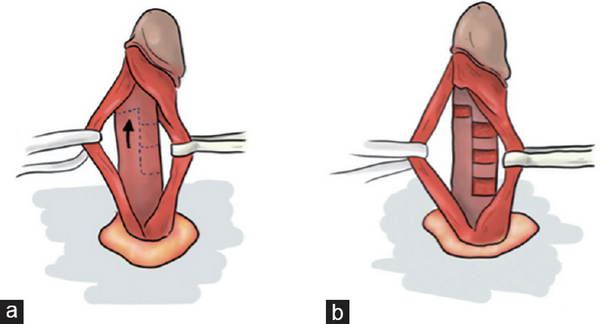
Figure 3
(a) Sliding approached used for the MUST technique; multiple small tunical defects are created instead of one large incision, then the penis is stretched in the direction of the arrow. (b) These defects will be covered with Buck’s fascia instead of using a conventional graft. MUST: multiple slice technique.
Tunica expansion procedure (TEP)
The TEP strategy entails a sequence of numerous small incisions strategically positioned on the tunica albuginea in a meshed pattern, with a focus on two primary goals: preserving tunica strength and maximizing length and width expansion (Figure 4). In the most extensive studies regarding the development of this technique, Egydio presented outcomes from 416 patients. The average surgical duration was 1.5 h for malleable prostheses and 2 h for inflatable ones. Patients experienced a mean penile gain of 3.3 (IQR: 2–6 cm). Moreover, all patients achieved curvature correction. Glanspexy to stabilize the cylinder tips was performed in 93% of cases. The mean follow-up period was 12 (range: 6–36) months. Hematoma incidence was 20%, though none required drainage, and prosthesis infection rate was 0.24% (1 case). There were no instances of glans necrosis.
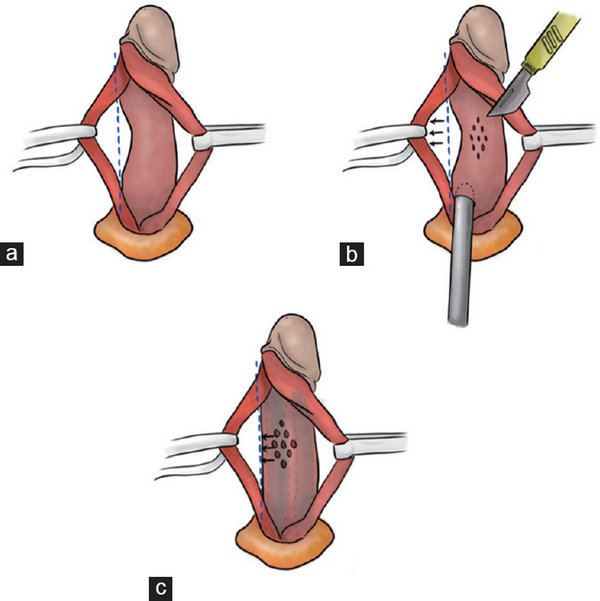
Figure 4
(a) Complete isolation of the neurovascular bundle is performed and then urethra is dissected from the cavernosa. (b) In order to counteract a narrowing phenomenon, multiple small relaxing tunical incisions/slits are performed in a rhomb-like configuration, in order to distend the corpora in the direction of the arrow. (c) This will lead to penile girth restoration.
TECHNIQUES THAT IMPROVE PERCEIVED PENILE LENGTH WHEN IMPLANTING A PENILE PROSTHESIS
Some other surgical techniques have been described to improve the subjective perception of increased length of the penis, but without a direct impact on the tunica albuginea. They include ventral phalloplasty, suprapubic lipectomy, and suspensory ligament release.
Ventral phalloplasty
Ventral phalloplasty is a procedure widely described in the pediatric literature to correct webbed penis. This technique effectively allows to reduce the penoscrotal web and its simultaneous use during the implantation of a penile prosthesis may improve patient satisfaction after surgery. It is relatively easy to perform and reproducible, and could be offered to any patient with a webbed penis undergoing a penoscrotal implantation with no significant additional complications.
Several techniques were developed to repair penoscrotal web, including Heineke–Mikulicz scrotoplasty, V-Y scrotoplasty, double-V scrotoplasty, and Z scrotoplasty. Technique is performed by stretching the penis and the scrotum away along the median raphe and then drawing a check mark on both sides of the skin of the scrotum. This checkmark shape is supposed to prevent the ulterior formation of a residual “dog-ear” in the middle of the scrotum, in contrast to a V-shape incision. Then, the skin contained in the interior of the check mark is removed preserving a thick layer of dartos, and closure is performed in two layers, with interrupting stitches of absorbable sutures, in order to decrease the probability of incision breakdown.
Suprapubic lipectomy and liposuction
Overweight patients with an excessive suprapubic fat pad, often with a “double belly” appearance when standing, may benefit from a suprapubic lipectomy in order to improve satisfaction rates. This procedure can be performed simultaneously with penile prosthesis implantation, or as a second-stage surgery. The main complication is the formation of underlying seromas or hematomas that impede appropriate closure of the skin and lead to exposure of some parts of the penile prosthesis, causing a higher risk of device infection. Therefore, to perform both procedures simultaneously, it is recommended to use a malleable prosthesis.
To perform lipectomy (Figure 5), 1 cm medial to the anterior superior iliac spine marks are made bilaterally and then connected by a horizontal line. A third mark is made around 1 cm above the dorsal base of the penis, and a second curvilinear line is drawn to connect this last mark to the previous iliac marks. The incision is carried down to the underlying lower abdominal fascia carefully, avoiding injury to the underlying spermatic cords. After removal of the fat pad, both spermatic cords and corporal bodies can be identified, and a penile prosthesis can be easily implanted using this large infrapubic approach.
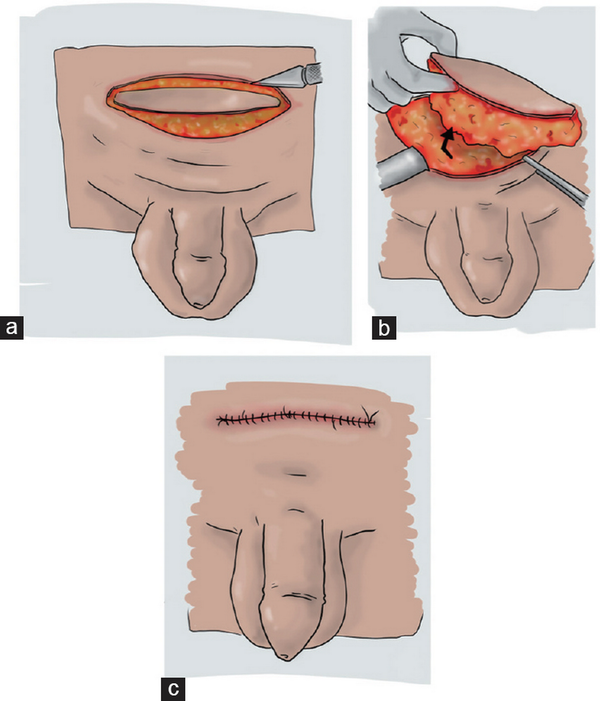
Figure 5
Lipectomy. (a) Preoperative marking before incision. (b) Suprapubic fat pad is removed (as showed from the arrow). (c) Final aspect after the defect is sutured.
Several methods have been outlined for addressing the buried penis. Hakky et al. and Horton et al. detailed a procedure involving the removal of suprapubic fat and securing the suprapubic skin to the rectus fascia. Shaeer et al. employed a technique that involves tucking the penile pubic junction using a suture connecting the periosteum of the symphysis pubis to the subdermal region of the penopubic junction, aiming to enhance visible penile length. More intricate cosmetic reconstructions, such as panniculectomy, Z-plasty, split-thickness skin grafting to the penile shaft, and preputial flaps, have also been described and typically fall under the purview of plastic surgery.
Suspensory ligament release
The suspensory ligament release is a procedure aimed at enhancing perceived penile length by releasing the ligament that attaches the penis to the pubic bone. During the surgery, careful dissection and release of the ligament are performed, allowing the penis to project further outward in the flaccid state. This technique is often combined with other procedures, such as suprapubic lipectomy, to optimize visual and functional outcomes.
Postoperative management is critical to prevent ligament reattachment, often involving partial inflation of the prosthesis and downward traction exercises. Complications, such as hematoma or infection, can occur but are mitigated with meticulous surgical technique and proper postoperative care.
If suspensory ligament release alone is performed, there is a high risk of spontaneous reattachment of the ligament during the healing process, resulting in a decrease of phallic length. Different materials could be used as spacers (silicone buffer and fat interposition) to avoid this complication. On the other hand, it increased the risk of infection, in addition to the surgical risks of injury to the external pudendal vessels or the dorsal vascular bundle of the penis, which could result in a local hematoma. In the largest study regarding the placement of an infrapubic penile prosthesis with concomitant suspensory ligament section, the results on 303 patients demonstrated that the technique can maintain or even increase length. A subanalysis of length measurements reports an increase of 1.73 (IQR: 1.1–2.2 cm) cm in erection, with no patient reporting a reduction in length.
In this case, to prevent rescarring of the suspensory ligament, patients were left with the prosthesis inflated between 50% and 70%. Downward pressure could be applied to avoid reattachment of the ligament ends, thus avoiding the need for an additional external agent to minimize the risk of infection.
CONCLUSION
While current literature supports the safety and efficacy of penile lengthening procedures performed during IPP placement, evidence remains limited due to the lack of large, randomized controlled trials. Future research should aim to establish standardized protocols and gather more robust data to better inform clinical practice.
AUTHOR CONTRIBUTIONS
MLR, MAI, and JRO have given substantial contributions to the conception and the design of the manuscript. MLR, CM, EGR, FS and MP drafted the manuscript. AC, AFP, AM and JRO critically revised the manuscript. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declare no competing interests.
REFERENCES
1.
Mulcahy JJ. The development of modern penile implants. Sex Med Rev 2016;4:177–89.2.
Segal RL, Camper SB, Burnett AL. Modern utilization of penile prosthesis surgery: a national claim registry analysis. Int J Impot Res 2014;26:167–71.3.
Trost LW, McCaslin R, Linder B, Hellstrom WJ. Long-term outcomes of penile prostheses for the treatment of erectile dysfunction. Expert Rev Med Devices 2013;10:353–66.4.
Park KK, Lee SH, Chung BH. The effects of long-term androgen deprivation therapy on penile length in patients with prostate cancer: a single-center, prospective, open-label, observational study. J Sex Med 2011;8:3214–9.5.
Haliloglu A, Baltaci S, Yaman O. Penile length changes in men treated with androgen suppression plus radiation therapy for local or locally advanced prostate cancer. J Urol 2007;177:128–30.6.
Vasconcelos JS, Figueiredo RT, Nascimento FL, Damião R, da Silva EA. The natural history of penile length after radical prostatectomy: a long-term prospective study. Urology 2012;80:1293–6.7.
Zaazaa A, Mostafa T. Spontaneous penile tumescence by sparing cavernous tissue in the course of malleable penile prosthesis implantation. J Sex Med 2019;16:474–8.8.
Moncada I, Martínez-Salamanca JI, Jara J, Cabello R, Moralejo M, et al. Inflatable penile prosthesis implantation without corporeal dilation: a cavernous tissue sparing technique. J Urol 2010;183:1123–6.9.
Zaazaa A, Bayerle-Eder M, Elnabarawy R, Elbitar M, Mostafa T. Penile hemodynamic response to phosphodiesterase type V inhibitors after cavernosal sparing inflatable penile prosthesis implantation: a prospective randomized open-blinded end-point (PROBE) study. Adv Urol 2021;2021:5548494.10.
Tran H, Goldfarb R, Ackerman A, Valenzuela RJ. Penile lengthening, girth, and size preservation at the time of penile prosthesis insertion. Sex Med Rev 2017;5:403–12.11.
Gaffney CD, Pagano MJ, Weinberg AC, Small AC, Kuehas FE, et al. Lengthening strategies for Peyronie's disease. Transl Androl Urol 2016;5:351–62.12.
Weinberg AC, Pagano MJ, Deibert CM, Valenzuela RJ. Sub-coronal inflatable penile prosthesis placement with modified no-touch technique: a step-by-step approach with outcomes. J Sex Med 2016;13:270–6.13.
Hakky TS, Suber J, Henry G, Smith D, Bradley P, et al. Penile enhancement procedures with simultaneous penile prosthesis placement. Adv Urol 2012;2012:314612.14.
Chung E, Bettocchi C, Egydio P, Love C, Osmonov D, et al. The International Penile Prosthesis Implant Consensus Forum: clinical recommendations and surgical principles on the inflatable 3-piece penile prosthesis implant. Nat Rev Urol 2022;19:534–46.15.
De Bonis WO, Dangelo A, Medel R, Casabe A, Bechara AJ. Necrosis of the glans penis after penile prosthesis implantation. Rev Mex Urol 2018;78:447–51.16.
Egydio PH, Kuehhas FE, Sansalone S. Penile length and girth restoration in severe Peyronie's disease using circular and longitudinal grafting. BJU Int 2013;111:E213–9.17.
Egydio PH, Kuehhas FE. Penile lengthening and widening without grafting according to a modified ‘sliding’ technique. BJU Int 2015;116:965–72.18.
Wilson SK, Wen L, Egydio PH. Evolution of techniques for aesthetic penile enlargement during prosthesis placement: a chronicle of the Egydio non-grafting strategy. Int J Impot Res 2023;35:1–8.19.
Garcia-Gomez B, Ralph D, Levine L, Moncada-Iribarren I, Djinovic R, et al. Grafts for Peyronie's disease: a comprehensive review. Andrology 2018;6:117–26.20.
Sansalone S, Garaffa G, Djinovic R, Egydio P, Vespasiani G, et al. Simultaneous penile lengthening and penile prosthesis implantation in patients with Peyronie's disease, refractory erectile dysfunction, and severe penile shortening. J Sex Med 2012;9:316–21.21.
Rolle L, Ceruti C, Timpano M, Sedigh O, Destefanis P, et al. A new, innovative, lengthening surgical procedure for Peyronie's disease by penile prosthesis implantation with double dorsal-ventral patch graft: the “sliding technique”. J Sex Med 2012;9:2389–95.22.
Rolle L, Falcone M, Ceruti C, Timpano M, Sedigh O, et al. A prospective multicentric international study on the surgical outcomes and patients' satisfaction rates of the ‘sliding’ technique for end-stage Peyronie's disease with severe shortening of the penis and erectile dysfunction. BJU Int 2016;117:814–20.23.
Egydio PH, Kuehhas FE, Valenzuela RJ. Modified sliding technique (MoST) for penile lengthening with insertion of inflatable penile prosthesis. J Sex Med 2015;12:1100–4.24.
Weinberg A, Pagano M, Zhao L, Valenzuela R. Multi-institutional and lasting results with the most (modified sliding technique) for penile lengthening with penile prosthesis insertion. J Urol 2016;195:e638.25.
Wilson SK, Mora-Estaves C, Egydio P, Ralph D, Habous M, et al. Glans necrosis following penile prosthesis implantation: prevention and treatment suggestions. Urology 2017;107:144–8.26.
Egydio PH, Kuehhas FE. The multiple-slit technique (MUST) for penile length and girth restoration. J Sex Med 2018;15:261–9.27.
Egydio PH. An innovative strategy for non-grafting penile enlargement: a novel paradigm for tunica expansion procedures. J Sex Med 2020;17:2093–103.28.
Shah BB, Kent M, Valenzuela R. Advanced penile length restoration techniques to optimize penile prosthesis placement outcomes. Sex Med Rev 2021;9:641–9.29.
Miranda-Sousa A, Keating M, Moreira S, Baker M, Carrion R. Concomitant ventral phalloplasty during penile implant surgery: a novel procedure that optimizes patient satisfaction and their perception of phallic length after penile implant surgery. J Sex Med 2007;4:1494–9.30.
Bonitz RP, Hanna MK. Correction of congenital penoscrotal webbing in children: a retrospective review of three surgical techniques. J Pediatr Urol 2016;12:161.e1–5.31.
Baumgarten AS, Beilan JA, Shah BB, Loeb A, Bickell M, et al. Suprapubic fat pad excision with simultaneous placement of inflatable penile prosthesis. J Sex Med 2019;16:333–7.32.
Staniorski CJ, Myrga JM, Vasan RV, Klein RD, Rusilko PJ. Surgical outcomes and prediction of complications following high-complexity buried penis reconstruction. J Urol 2023;210:782–90.33.
Thornton SM, Seitz AJ, Edalatpour A, Poore SO. Surgical management of adult acquired buried penis syndrome: a systematic review of patient-reported outcome instruments. J Plast Reconstr Aesthet Surg 2024;91:181–90.34.
Horton CE, Vorstman B, Teasley D, Winslow B. Hidden penis release: adjunctive suprapubic lipectomy. Ann Plast Surg 1987;19:131–4.35.
Shaeer O, Shaeer K, AbdelRahman IF. Simultaneous suprapubic lipectomy and penile prosthesis implantation. J Sex Med 2018;15:1818–23.36.
Filipoiu FM, Ion RT, Filipoiu ZF, Tulin AD, Enciu O, et al. Suspension of the penis – dissection, anatomical description and highlighting of anatomical risks in sectioning the suspensory ligaments. Basic Clin Androl 2023;33:26.37.
Borges F, Hakim L, Kline C. Surgical technique to maintain penile length after insertion of an inflatable penile prosthesis via infrapubic approach. J Sex Med 2006;3:550–3.
