Introduction
Multiple sclerosis (MS) is one of the frequent reasons for the increased disability length of different age groups of patients. The most common symptoms of MS are muscle weakness and instability in walking, spasticity, pathological fatigue, and other symptoms of CNS lesions that may occur at various levels. More than 65% of patients have trouble moving, and up to 85% of patients have gait disorders. Thus, all MS patients need comprehensive rehabilitation and very often at early disease stage. There is evidence that physical exercises improve MS patients’ functionality (mobility, walking, and endurance) and quality of life.− There is also evidence that more than 60% of patients are willing to use additional approaches to drug treatment, including exercises.
The effectiveness of physical therapy (PT) has been examined in many studies. A review of 26 randomized trials found a reduction in the risk of aggravation in the group of patients with MS performing exercise compared to the patients without gymnastics (6.3% vs 4.6%) and additionally demonstrated the safety of exercise. Thus, exercises can influence the course of the disease in patients with MS. The effectiveness of exercise on the reduction of specific MS symptoms was also demonstrated in numerous studies., Thus, 45 studies were conducted to evaluate the effects of 69 different types of exercise in 2,250 patients with MS-associated pathological fatigue.
Many studies, as well as the meta-analysis, have obtained the effectiveness of yoga in patients with MS in reducing the level of depression, pain, pathological fatigue, bladder dysfunction, postural disorders, and improvement in the quality of life and mobility., – The safety and efficiency of yoga compared to the non-exercise group of patients are demonstrated in a variety of studies ranging in duration from 8 weeks to 6 months.– Currently, yoga is often even more accessible to a wide range of patients as a method of rehabilitation compared to PT, conducted only in specialized medical centers. In large cities, there are many yoga or fitness centers, where rehabilitation programs could be applied, and regular attendance also increases social activity and social adaptation of patients.
Despite a large number of positive results of using yoga and PT for patients with MS, there are only a limited number of publications, where these methods of non-drug rehabilitation would be compared in a randomized controlled trial., ,
At the same time, the correct comparison of these methods is of great interest for both researchers and specialists in the rehabilitation of patients with MS. This approach can expand our understanding of the mechanisms of functional disorders during MS and the ways to correct them. As a result, specialists will be able to combine the advantages of different approaches, improving the quality of rehabilitation.
It should also be noted that contrary to the well-defined physical exercises protocols,, in most of the available at the moment studies, there is no detailed description for the performance of yoga protocols, that is, those complexes of asanas (special physical exercises), pranayama (breathing exercises), and techniques of mental relaxation, which were offered to patients, as well as the ways of their implementation. We can find an exception only in some articles, where the images and names of poses and the sequence of their performance are given.– In other articles, the method of exercise and the use of yoga techniques are described only in general terms, such as hatha yoga, classical yoga, pranayama, yoga poses, and breathing exercises. Typically, the frequency and duration of regular classes, the total number of classes, and the period of research are also specified.
Therefore, for this study, we used B.K.S. Iyengar’s method of yoga training, which is one of the most recognized, time-tested, and systematic methods of classical hatha yoga. At the moment, the efficiency of Iyengar yoga has been demonstrated for the treatment of different symptoms, common for patients with MS, such as chronic pain, depression, and anxiety fatigue., Our own experience of conducting Iyengar yoga classes for patients with MS shows that specially designed complexes of asanas have a beneficial effect on the condition and quality of life of the participants.
In this regard, the main aim of this study is to examine the effect of the Iyengar yoga program on symptoms (such as walking and balance difficulties) and quality of life in patients with MS, vs physical therapy (exercise therapy) and no exercise.
Methods
Participants
This study involved outpatient adult subjects with remitting or secondary-progressive MS of both genders. The inclusion criteria were as follows: written informed consent, age ≥18 years, diagnosis of remitting or secondary-progressive MS, presence of walking, balance impairment or pathological fatigue (based on clinical decision of the Physician), Expanded Disability Status Scale (EDSS) score from 2.0 to 6.0, possibility to visit classes and perform the protocol procedures (completion of questionnaires, passing tests), and no history of previous regular physical exercises assigned for MS treatment. The exclusion criteria were as follows: the exacerbation of MS within 30 days before the study and the botulinum therapy of low limbs within six months before the study.
In the event of an exacerbation of MS or for other safety-related reasons (e.g., side effects of exercise), the patients were excluded from the study.
During the period of participating in the trial, all patients continued the MS treatment according to local standards and guidelines, as prescribed by the treating neurologist.
Study Design and Outcomes
This study was a 12-week prospective, randomized, 3-arm clinical trial conducted in two large centers specialized in MS. The informed consent forms were obtained from all participants of the study. All methods were carried out in accordance with relevant guidelines and regulations. Participants were recruited from April 2018 to March 2019.
After a baseline assessment, patients were randomly assigned to three groups at 1:1:1 ratio: yoga, PT, or no exercise. Patients from the no-exercise group had an opportunity to enter the free-of-charge yoga program after the end of the trial period. According to local treatment protocols, patients of this group did not receive regular PT or yoga training, so there was no ethical barrier to allocate the patient to no PT group for two weeks with the opportunity to get free-of-charge yoga practice at the end of the study.
Simple randomization was used. The list of randomization codes (where patient number corresponded to randomly generated group; number 1, 2, or 3) was created before initiation of the study using random number generator function in Microsoft Excel. Eligible patients were allocated to the groups at the study centers according to the randomization list. The observation group (1, 2, or 3) was known to both the patient and the doctor, but it was blinded for the rater (as participants were identified in the study by patient numbers, only patient number without group was provided to the rater).
The data were collected during two visits to the research center: at baseline and at the end of the 12-week training period. The survey on the visits included an investigator’s assessment of the EDSS, the SF-36 quality of life questionnaire, the Fatigue Assessment Scale, the Berg balance scale and the 6-min walking test.
For each patient. participation in the study lasted up to 14 weeks, including screening (up to 1 week), intervention period (12 weeks), and the final assessment (up to 1 week after the last exercise).
The primary outcome was balancing ability measured using mean Berg Balance Scale score after 12 weeks of intervention period. The secondary outcomes were tolerance of physical activity measured using the 6-min walk test result (m), general well-being measured using the SF-36 questionnaire, fatigue measured using Fatigue Assessment Scale, proportion of patients who successfully completed the study measured using attendance records at baseline and after 12 weeks of intervention, and adverse events related to physical activity appeared during the study measured using interview at baseline and in 12 weeks.
Study Intervention
Yoga Group
The yoga and exercise classes were held twice a week, for 12 weeks. Each session lasted about 60–75 min. The classes were held in a specially equipped hall, using supporting materials, under the guidance of experienced trainers and a trainer assistant. All exercises were performed by the study participants together, in accordance with the detailed instructions of the trainer.
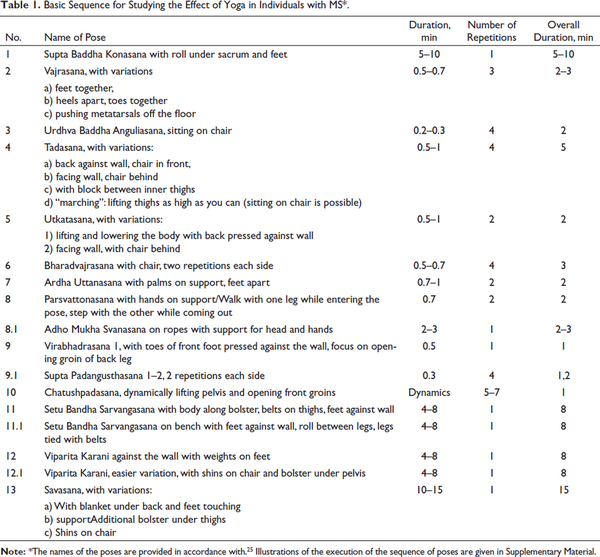
The yoga group practiced a special complex consisting of 13 basic and alternative (8.1, 9.1, 11.1, 12.1) poses described in Table 1 and Supplementary Material. The complex is basic, universal for patients with MS, and is designed to ensure safety, but at the same time gives practitioners the opportunity to progress and improve their condition. Alternatively, lighter versions of those poses that may cause difficulties were also suggested, and basic postures were performed using additional materials to ensure comfortable exercise. The names of poses and the basic principles of their implementation correspond to the classification given in B.K.S. Iyengar’s book “Clarification of Yoga”.
During the exercises, special attention was paid not only to the time of performance and the correct location of body parts but also to the correct actions on tension, stretching, and relaxation of the muscles of synergists and antagonists, as well as to getting patients’ feedback after practicing a posture, increasing awareness and sensitivity of their body and its parts during the exercises. The alteration of activity and rest cycles was also an extremely important condition in the sequence so that participants did not get tired during the lessons. This is why the sequence involved both more active and more regenerative poses, with alternatives to some postures offered to the participants when fatigue or tension occurred during the main exercise sequences. Throughout the study, the participants were also provided with illustrated brochures with detailed descriptions and photographic illustrations of the exercises performed (Supplementary Material).
Physical Therapy Group
The PT classes were also held twice a week, for 12 weeks. Each session lasted about 60–75 min. The classes were held in a specially equipped hall, under the guidance of PT instructor. The usual class consisted of three parts: 10–15 min─a warm-up, which included exercises on stretching of the main muscle groups, and flexibility in combination with breathing training; 25–35 min─endurance training, muscle strength, coordination, and balance exercises, aerobic exercises; 10–15 min─relaxing techniques in combination with breathing exercises. More detailed description of PT program is provided in this study.
No Exercise Group
In the no-exercise group, the participants led their normal lifestyle without regular practice of yoga, PT, or other regular physical exercises.
Statistical Analyzes
Descriptive statistics were used to describe demographics and all the data collected in the course of the study. For interval variables, the number of patients for each variable was calculated, as the average arithmetic (calculating the absolute change relative to the original value), standard deviation, median, minimum, and maximum values. For one-order variables, the values of the median, 25% and 75% were calculated. For nominal variables, the frequency of categories was calculated for each visit in the course of the study. The number of values missed was specified for each variable.
Interval study outcomes were analyzed using ANCOVA (evaluation of Time*Group factor). Nominal variables were analyzed using Fisher exact test. The statistical significance level was set at 0.05.
Statistical analysis was conducted using SPSS/PASW Statistics, SPSS Inc.
The sample size was estimated for testing hypothesis of superiority of yoga or PT over “no exercise” in terms of primary endpoint. Assuming clinically significant margin of 10 points, variability (SD) of 12 points by Berg balance scale (Tarakci), study power of 80%, one-sided alpha level of 0.025, and estimated sample size for analysis was 23 participants per group.
Results
The distribution of study participants is presented in Figure 1. In total, 80 people contacted the organizers of the study. Of these, 61 people were screened and 56 patients with MS were included in the study: 26 in the yoga group, 16 in the PT group, and 14 in the waiting list. The remaining five people had no neurological symptoms of MS and therefore were not included in the study.
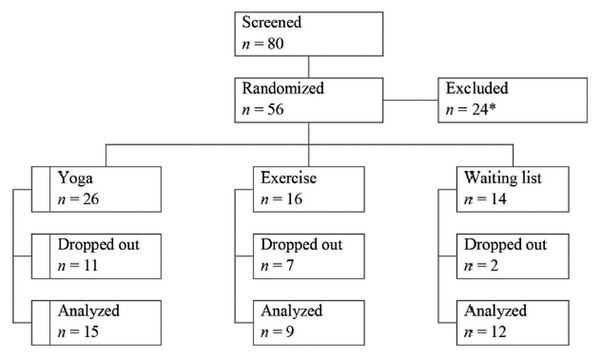
Flow Diagram of Distribution of Study Participants.
Note: *5 patients didn’t meet inclusion/exclusion criteria, 12 declined to participate, and 7 other reasons.
Twenty patients (11 in the yoga group, 7 in the PT group, and 2 in the waiting list) dropped out before passing the second test. The most frequent reasons for dropping out of the yoga group were exacerbation of MS and non-compliance with the protocol, in the PT group─non-compliance with the protocol; two patients of the third group dropped out at their own request.
The number and the proportion of patients who successfully participated to the end of the study were 15 (57.7%) in the yoga group, 9 (56.3%) in the PT group, and 12 (85.7%) in waiting list (p = .157, Fisher’s exact test).
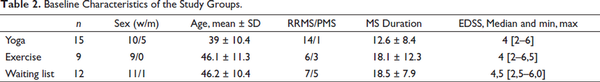
According to the protocol, the endpoint analysis was carried out regarding the patients who had undergone the first and second examinations (Per Protocol, PP). The number of the analyzed patients was 36 (15 in the first group, 9 in the second group, and 12 in the third group). The analysis was performed by original assigned groups. The results of the scale assessment are presented in Table 2. Of these, 30 patients were women and 6 were men. The number and proportion (%) of women in the groups were the following: 10/15 (66.7%) in the yoga group, 9/9 (100%) in the PT group, and 11/12 (91.7%) in the waiting list. The average age of patients (average ± standard deviation) was 39 ± 10.4 years in the yoga group, 46.1 ± 11.3 years in the exercise group (PT), and 46.2 ± 10.4 years in the no-exercise group (waiting list); the difference between the averages in the study groups is statistically insignificant (by Student’s t-test: (t-test value and df-value) 0.011023 and 40; 0.477188 and 28; 0.010097 and 38). The average MS duration prior to the study was 12.6 ± 8.4 in the yoga group, 18.1 ± 12.3 in the exercise group, and 18.5 ± 7.9 in the no-exercise group. There were 14 patients with remitting MS, one patient with secondary-progressive MS in the yoga group; six patients with remitting MS, two patients with secondary-progressive MS, and one patient with primary-progressive MS in the PT group; seven patients with remitting MS, five patients with secondary-progressive MS in the waiting list. At the time of inclusion in the study, 15 (100%) patients in the yoga group, five (55.6%) patients in the PT group, and eight (66.7%) patients in the waiting list were taking DMT. The most commonly taken drug was glatiramer acetate. In second place in frequency was interferon beta-1b. According to the survey on previously done types of exercise, most often, the patients exercised at home or just walked. However, nobody did exercise regularly for rehabilitation purposes. The median of EDSS was 4 points, same as in the yoga and PT groups and 4,5 points in the waiting list group.
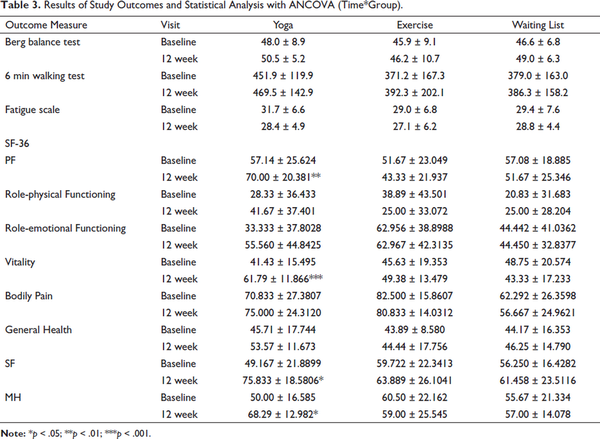
There was no statistically significant difference between the groups in terms of improvement in MS symptoms as measured by the balance, walking test, and fatigue scales. However, at the same time, in the analysis of eight criteria of SF-36 quality-of-life questionnaire by the covariation analysis (assessment of the influence of the group factor based on time dynamics, Time*Group) statistically significant differences were found in favor of the yoga group in terms of physical functioning (PF) (p = .003), life activity (VT) (p < .001), mental health (MH) (p = .013), and social functioning (SF) (p = .028) (Table 3).
In the course of the study, only two patients with adverse events were registered as having: pain (without clarification) and back pain, both cases in the PT group. There were no side effects during the yoga classes.
Discussion
In this randomized controlled trial, we have demonstrated the efficiency of specially designed Iyengar yoga program over the PT program in PF, VT, MH, and SF of MS patients.
Our experience of teaching yoga, both in regular classes and for students with specific health problems, including patients with MS, shows that for each particular disease or symptom, yoga exercises should be performed according to specially developed techniques. At the same time, each component of this technique: the choice of a set of poses, sequence, duration, and correctness of their performance, plays a crucial role in achieving the goals and is extremely important for ensuring the reproduction, verification, and further practical use of the results.
Therefore, all yoga classes were conducted according to the program, specially designed for patients with MS, under the guidance of a qualified teacher. This article provides a detailed description of the sequence of exercises (poses), accompanied also by illustrative materials (Supplementary Material). We believe that such an approach can be useful also for subsequent studies, for standardizing the use of yoga in rehabilitation of patients with MS.
The main strengths of this trial are as follows: the group under research of non-drug rehabilitation (yoga) was compared not only with the control group without exercise, but also with the group, treated by the standard method─PT, the sufficient duration of observation (12 weeks) was planned to assess the effect.
The focus group may not be fully representative of the general population of patients with MS, but it is close to the population, which is treated by the researched methods (yoga, PT) in routine practice. In addition, there were no demographic restrictions on inclusion in the study. In general, the plan of the study corresponded to its’ goals. The main limitations of the plan of this study can be attributed to the relatively small sample size, which reduces the power of the statistical tests. In addition, the planned number of patients (75) was not recruited for organizational reasons, including the introduction of restrictions in connection with the COVID-19 pandemic. However, the obtained sample size allowed performing the analysis of study outcomes planned by the protocol.
Our comparative study assessed two different types of indicators – indicators of the patient’s physical condition (balance test, walking test, fatigue scale, and functional disability by EDSS scale) and indicators of the patient’s psycho-emotional state, according to the SF-36 quality of life questionnaire (Table 3). The first type of indicators depends on the degree of CNS damage due to the cause and the duration of the accumulated functional limitations, that is, the duration of the disease. In our study, the duration of MS averaged approximately 15 years, and the average degree of functional limitation was 4.5 points on the scale (Table 2). It was shown, that although the indicators of the first group did not show statistically significant change as a result of the 12-week yoga program, some improvements for most of these parameters were registered in the yoga group (Table 3).
Currently, mixed results have been reported for the studies, which implemented relatively short (8–12 weeks) yoga programs for MS patient’s treatment. Thus, one such research papers showed improvements in the fatigue, balance, and walking indicators as a result of a 12-week yoga program, but the study group was relatively small (eight patients) and no control group was used. Similarly, the positive effect of an 8-week integrative yoga program on walking and fatigue was reported. However, again the single-group design with limited number (14 people) of participants was used. At the same time, several randomized controlled trials showed that the use of yoga complexes during 8–12 weeks did not lead to statistically significant changes in fatigue or walking. Nevertheless, it is interesting to mention a group of studies, which examined the effects of longer (6-month) yoga programs. They demonstrated statistically significant improvement in balance, fatigue, and walking.
Therefore, it can be concluded that, despite the obvious positive effect, for MS patients who have a long duration of the disease (in our study, it was about 15 years), as well as significant changes in neurological status (EDSS in the region of 4–5), a 12-week training program might be not enough for statistically significant improvement in balance, walking, and fatigue.
The second group of indicators reflects the psycho-emotional state of the patients, their subjective perception of the degree of illness and experienced limitations. As shown by the statistical analysis with ANCOVA (Time*Group), regular classes on the proposed yoga program were enough to produce statistically significant improvements in some of these indicators, such as physical and SF, vitality, and MH (Table 3), which proves the ability of correctly applied rehabilitation programs to significantly improve the subjective perception of the illness and psychological state of patients. These findings also correspond to the studies, in which similar yoga protocols were applied, resulting in significant improvements in the quality of life indicators., ,
Thus, to observe more significant improvements in the first group of indicators (i.e., balance, walking, and fatigue), it is necessary to use longer rehabilitation programs.
However, it should also be noted that we observed a relatively high drop-out of patients. Unfortunately, one of the frequent reasons for dropping out from yoga and PT groups was non-compliance with the protocol. This demonstrates the non-sufficient motivation for physical rehabilitation in MS patients. Interestingly, two patients of the third (yoga) group dropped out at their own request to regularly attend usual yoga classes. This decision, on the contrary, shows high motivation to improve their health state, because these patients preferred to refuse participation in the researched yoga group in favor of actively practicing yoga in regular classes.
In this study, we did not have a goal to observe the motivation of our patients and to compare it in different study groups. However, It is clear that the overall dropout rate due to protocol non-compliance requires special studies of the motivation of MS patients. These studies are very important because they could allow finding approaches to increase the motivation of MS patients and to improve their rehabilitation.
Further trials should explore the development of such rehabilitation programs that will increase patients’ commitment to continuing regular self-practice after their completion, and scaling up the proposed rehabilitation methods for widespread use in yoga and fitness centers.
Conclusion
Regular yoga classes under the guidance of qualified staff are a promising method of non-drug rehabilitation of patients with MS with motor disorders. More research is needed to examine the impact of yoga on clinical patient improvement and quality of life indicators.
Acknowledgements
We thank Natalia Zryacheva, the vice-president of the Russian Society of Patients with Multiple Sclerosis, for her invaluable help in communicating with the community of MS patients and coordinating the study participants; and Dr. Olesya Mokienko, PhD, for consulting on scientific writing.
Declaration of Conflicting Interests The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The public noncommercial organization Yoga Practika Federation (Russia) funded the study (Grant 9-c/17).
Elena Lysogorskaia
https://orcid.org/0000-0002-7253-4736
Maxim Youshko
https://orcid.org/0000-0001-8464-2841
- 1. Skierlo S, Rommer PS, Zettl UK. Symptomatic treatment in multiplesclerosis-interim analysis of a nationwide registry. Acta Neurol Scand 2017; 135(4): 394–399. DOI:10.1111/ane.12612.
- 2. Rogers KA, MacDonald M. Therapeutic yoga: Symptom management for multiple sclerosis. J Altern Complement Med 2015; 21(11): 655–659. DOI:10.1089/acm.2015.0015.
- 3. Khan F, Turner-Stokes L, Ng L, . Multidisciplinary rehabilitation for adults with multiple sclerosis. Cochrane Database Syst Rev 2007; 2007(2): CD006036. DOI:10.1002/14651858.CD006036.pub2.
- 4. Alphonsus KB, Su Y, Arcy CD. The effect of exercise, yoga, and physiotherapy on the quality of life of people with multiple sclerosis: Systematic review and meta-analysis. Complement Ther Med 2019; 43: 188–195. DOI:10.1016/j.ctim.2019.02.010.
- 5. Motl RW. Exercise and multiple sclerosis. Adv Exp Med Biol 2020; 1228: 333–343. DOI: 10.1007/978-981-15-1792-1_22.
- 6. Miller P, Soundy A. The pharmacological and non-pharmacological interventions for the Fatigue related multiple sclerosis. J Neurol Sci 2017; 381: 41–54. DOI:10.1016/j.jns.2017.08.012.
- 7. Pilutti LA, Platta ME, Motl RW, . The safety of exercise training in multiple sclerosis: A systematic review. J Neurol Sci 2014; 343(1–2): 3–7. DOI:10.1016/j.jns.2014.05.016.
- 8. Wens I, Dalgas U, Vandenabeele F, . High intensity exercise in multiple sclerosis: Effects on muscle contractile characteristics and exercise capacity, a randomised controlled trial. PLoS One 2015; 10(9): e0133697. DOI: 10.1371/journal.pone.0133697.
- 9. Razazian N, Yavari Z, Farnia V, . Exercising impacts on fatigue, depression, and paresthesia in female patients with multiple sclerosis. Med Sci Sports Exerc 2016; 48(5): 796–803. DOI:10.1249/MSS.0000000000000834.
- 10. Heine M, van de Port I, Rietberg MB, . Exercise therapy for fatigue in multiple sclerosis. Cochrane Database Syst Rev 2015; (9): CD009956. DOI:10.1002/14651858.CD009956.pub2.
- 11. Patil NJ, Nagaratna R, Garner C, . Effect of integrated yoga on neurogenic bladder dysfunction in patients with multiple sclerosis: A prospective observational case series. Complement Ther Med 2012; 20: 424–430. DOI:10.1016/j.ctim.2012.08.003.
- 12. Salgado BC, Jones M, Ilgun S, . Effects of a 4-month Ananda yoga program on physical and mental health outcomes for persons with multiple sclerosis. Int J Yoga Therap 2013; 23: 27–38.
- 13. Karbandi S, Gorji MA, Mazloum SR, . Effectiveness of group versus individual yoga exercises on fatigue of patients with multiple sclerosis. N Am J Med Sci 2015; 7(6): 266–270. DOI:10.4103/1947-2714.159332.
- 14. Chobe S, Bhargav H, Raghuram N, . Effect of integrated yoga and physical therapy on audiovisual reaction time, anxiety and depression in patients with chronic multiple sclerosis: A pilot study. J Complement Integr Med 2016; 13(3): 301–309. DOI: 10.1515/jcim-2015-0105.
- 15. Cohen ET, Kietrys D, Fogerite SG, . Feasibility and impact of an 8-week integrative yoga program in people with moderate multiple sclerosis-related disability: A pilot study. Int J MS Care 2017; 19(1): 30–39. DOI:10.7224/1537-2073.2015-046.
- 16. Kahraman T, Ozdogar AT, Yigit P, . Feasibility of a 6-month yoga program to improve the physical and psychosocial status of persons with multiple sclerosis and their family members. Explore (NY) 2018; 14(1): 36–43. DOI:10.1016/j.explore.2017.07.006.
- 17. Nejati S, Esfahani SR, Rahmani S, . The effect of group mindfulness-based stress reduction and consciousness yoga program on quality of life and fatigue severity in patients with MS. J Caring Sci 2016; 5(4): 325–335. DOI: 10.15171/jcs.2016.034.
- 18. Oken BS, Kishiyama S, Zajdel D, . Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology 2004; 62(11): 2058–2064. DOI: 10.1212/01.wnl.0000129534.88602.5c.
- 19. Garrett M, Hogan N, Larkin A, . Exercise in the community for people with minimal gait impairment due to MS: An assessor-blind randomized controlled trial. Mult Scler 2013; 19(6): 782–789. DOI: 10.1177/1352458512461966.
- 20. Halabchi F, Alizadeh Z, Sahraian MA, . Exercise prescription for patients with multiple sclerosis; potential benefits and practical recommendations. BMC Neurol 2017; 17(1): 185. DOI: 10.1186/s12883-017-0960-9.
- 21. Guner S, Inanici F. Yoga therapy and ambulatory multiple sclerosis assessment of gait analysis parameters, fatigue, and balance. J Bodyw Mov Ther 2015; 19(1): 72–81. DOI:10.1016/j.jbmt.2014.04.004.
- 22. Kishiyama S, Carlsen J, Lawrence J, . Yoga as an experimental intervention for cognition in multiple sclerosis. Int J Yoga Therap 2002; 12: 57–62.
- 23. de Oliveira G, Tavares M da C, de Faria Oliveira JD, . Yoga training has positive effects on postural balance and its influence on activities of daily living in people with multiple sclerosis: A pilot study. Explore 2016, 12: 325–332. DOI: 10.1016/j.explore.2016.06.005.
- 24. Najafi P, Moghadasi M. The effect of yoga training on enhancement of adrenocorticotropic hormone (ACTH) and cortisol levels in female patients with multiple sclerosis. Complement Ther Clin Pract 2017; 26: 21–25. DOI:10.1016/j.ctcp.2016.11.006.
- 25. Iyengar BKS. Light on yoga. New York: Schocken Books, 1966.
- 26. Crow EM, Jeannot E, Trewhela A. Effectiveness of Iyengar yoga in treating spinal (back and neck) pain: A systematic review. Int J Yoga 2015; 8(1): 3–14. DOI: 10.4103/0973-6131.146046.
- 27. Scott T, Gerbarg P, Silveri M, . Psychological function, Iyengar yoga, and coherent breathing: A randomized controlled dosing study. J Psychiatr Pract 2019; 25(6): 437–450. DOI: 10.1097/PRA.0000000000000435.
- 28. Bower J, Garet D, Sternlieb B, . Yoga for persistent fatigue in breast cancer survivors: A randomized controlled trial. Cancer 2012; 118(15): 3766–3775. DOI: 10.1002/cncr.26702.
- 29. Kurtzke JF. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983; 33(11): 1444–1452. DOI:10.1212/wnl.33.11.1444.
- 30. Ware JE SF-36 health survey update. Spine (Phila Pa 1976) 2000; 25(24): 3130–3139. DOI:10.1097/00007632-200012150-00008.
- 31. Michielsen HJ, De Vries J, Van Heck GL. Psychometric qualities of a brief self-rated fatigue measure: The fatigue assessment scale. J Psychosom Res 2003; 54(4): 345–352. DOI:10.1016/s0022-3999(02)00392-6.
- 32. Cattaneo D, Jonsdottir J, Repetti S. Reliability of four scales on balance disorders in persons with multiple sclerosis. Disabil Rehabil 2007; 29(24): 1920–1925. DOI:10.1080/09638280701191859.
- 33. Goldman MD, Marrie RA, Cohen JA. Evaluation of the six-minute walk in multiple sclerosis subjects and healthy controls. Mult Scler 2008; 14(3): 383–390. DOI:10.1177/1352458507082607.
- 34. Halabchi F, Alizadeh Z, Sahraian MA, . Exercise prescription for patients with multiple sclerosis; potential benefits and practical recommendations. BMC Neurol 2017; 17(1): 185. DOI: 10.1186/s12883-017-0960-9.
- 35. Tarakci E, Yeldan I, Huseyinsinoglu BE, . Group exercise training for balance, functional status, spasticity, fatigue, and quality of life in multiple sclerosis: A randomized controlled trial. Clin Rehabil 2013; 27(9): 813–822. DOI: 10.1177/0269215513481047.
- 36. Velikonja O, Curić K, Ozura A, . Influence of sports climbing and yoga on spasticity, cognitive function, mood and fatigue in patients with multiple sclerosis. Clin Neurol Neurosurg 2010; 112(7): 597–601. DOI:10.1016/j.clineuro.2010.03.006.
- 37. Hogan N, Kehoe M, Larkin A, . The effect of community exercise interventions for people with MS who use bilateral support for gait. Mult Scler Int 2014; 2014: 109142. DOI: 10.1155/2014/109142.