Introduction
Tinnitus is the most common ear disease and represents a global issue [Langguth et al., 2013; Tunkel et al., 2014], with a prevalence of 5.1–42.7% around the world, and increases with age [McCormack et al., 2016]. Guidelines of different countries stratify chronic tinnitus differently, with 3 months in Japan [Ogawa et al., 2020] and 6 months in China, the USA, and Europe [Editorial Board of Chinese Journal of Otorhinolaryngology, Head and Neck Surgery, 2012; Tunkel et al., 2014; Cima et al., 2019]. According to guidelines, acute tinnitus resolves spontaneously [Nyenhuis et al., 2013; Tunkel et al., 2014], but patients with chronic tinnitus are less likely to achieve self-improvement [Tunkel et al., 2014]; however, that may not be correct. Previous studies on chronic tinnitus have shown that 20–50% of patients may recover within 5 years [Nondahl et al., 2002; Gopinath et al., 2010].
Tinnitus is only a clinical symptom with a complex etiology. Although hearing loss (HL) is indeed an initiating factor for tinnitus, the association is not simple and direct [Lai and Ma, 2017]. Among the various classifications and severities of HL, sudden HL has the most definite association with tinnitus as >80% of sudden sensorineural HL (SSNHL) cases have been found to be accompanied by tinnitus [Schreiber et al., 2010]. Tinnitus in SSNHL patients often lasts for >6 months. Although several studies have focused on the prognosis of tinnitus accompanied by SSNHL, the follow-up times were mostly within 1 year [Michiba et al., 2013; Mühlmeier et al., 2016; Noguchi et al., 2016; Ding et al., 2018; Zhong et al., 2019]. Therefore, we investigated the long-term outcomes of tinnitus in 161 patients with SSNHL after standard treatments. We also analyzed possible factors affecting tinnitus recovery to provide clarification and counseling for patients with residual tinnitus after SSNHL to build reasonable confidence and set appropriate expectations.
Subjects and Methods
Study Design and Participants
From January 2014 to December 2015, 161 patients with unilateral SSNHL accompanied by newly developed tinnitus who were hospitalized in the Department of Otorhinolaryngology, Peking University People’s Hospital, were enrolled. All of the patients’ hearing was assessed by the same doctor. After admission, treatments were applied in accordance with the Chinese Guideline for Sudden Deafness [Editorial Board of Chinese Journal of Otorhinolaryngology, Head and Neck Surgery, 2015]. Systemic corticosteroids and hemodilution agents were administered as therapeutic measures. All patients received 40 mg of intravenous methylprednisolone for 5 consecutive days and hemodilution agents for 10 days, including 87.5 mg of intravenous EGb-761 (Ginkgo Biloba Extracts; Dr. Willmar Schwabe GmbH & Co., Germany) every day and 5 BU of intravenous batroxobin (Beijing Tobishi Pharmaceutical Co.), only the first dose was doubled, every other day based on fibrinogen levels. (We usually retest the fibrinogen level the next day after the first use. If the fibrinogen level is >100 mg/dL, use batroxobin; if not, use batroxobin again until the fibrinogen level is >100 mg/dL.)
Inclusion and Exclusion Criteria
Inclusion Criteria. (1) First-onset SSNHL. (2) Unilateral HL. (3) A time between onset and treatment ≤60 days. (4) Ipsilateral newly developed tinnitus associated with SSNHL. (5) Normal hearing or age-related HL in the contralateral ear. (6) No hearing aid devices are fit. No restrictions on sex and age were set.
Exclusion Criteria. (1) Recurrent sudden deafness, pregnancy, or middle ear infections. (2) A definitive cause of deafness identified during treatment. (3) A history of tinnitus. (4) Bilateral tinnitus. (5) No treatment according to the Chinese Guidelines for Sudden Deafness during the inpatient process for any reason [Editorial Board of Chinese Journal of Otorhinolaryngology, Head and Neck Surgery, 2015]. (6) Anxiety and insomnia.
Evaluation of Tinnitus and HL
Evaluation of Tinnitus Severity. Tinnitus in the patients was classified into seven grades according to the Chinese standard of tinnitus in 2012 [Editorial Board of Chinese Journal of Otorhinolaryngology, Head and Neck Surgery, 2012] based on the structured tinnitus interview by Biesinger et al. [1998]: (1) 0, no tinnitus; (2) 1, occasional tinnitus that does not affect the patient’s daily life; (3) 2, persistent tinnitus that is more prominent in quiet surroundings; (4) 3, persistent tinnitus even in a noisy environment; (5) 4, persistent tinnitus combined with attention and sleep disorders; (6) 5, persistent severe tinnitus affecting the patient’s ability to work; and (7) 6, severe tinnitus provoking suicidal tendencies.
Improvement Evaluation of Tinnitus. The evaluation was based on the Chinese classification of tinnitus severity [Editorial Board of Chinese Journal of Otorhinolaryngology, Head and Neck Surgery, 2012]: (1) recovered: tinnitus had disappeared or improved to grade 1; (2) markedly effective: tinnitus was alleviated by 1–3 grades but had not yet reached grade 1; (3) effective: tinnitus was alleviated to some extent but remained in the same grade; (4) ineffective: tinnitus was unchanged or even worsened. In this study, level 1 intermittent tinnitus was also counted as recovered in this article.
Grades of HL Severity. The hearing thresholds at 0.50, 1.00, 2.00, and 4.00 kHz were measured. When the hearing thresholds at some frequencies could not be detected, the frequency threshold was considered the maximum audiometric intensity. The degrees of HL were categorized as mild (26–40 dB HL), moderate (41–60 dB HL), severe (61–80 dB HL), and profound (>80 dB HL) [Editorial Board of Chinese Journal of Otorhinolaryngology, Head and Neck Surgery, 2015].
Classification of HL. Four audiogram shapes were defined in relation to the pattern of HL [Editorial Board of Chinese Journal of Otorhinolaryngology, Head and Neck Surgery, 2015]: ascending, flat, profound, and descending. “Ascending” referred to cases in whom the average threshold of 0.25–0.5 kHz was 20 dB higher than normal. When the difference in the hearing threshold did not exceed 20 dB at any frequency, the audiogram shape was classified as “flat.” For patients with a flat audiogram and a hearing threshold >81 dB, the audiogram shape was classified as “profound.” The audiogram shape was described as “descending” if the average threshold of 4–8 kHz was 20 dB higher than normal.
Hearing Recovery Evaluation. Based the results of pure-tone audiometry [Editorial Board of Chinese Journal of Otorhinolaryngology, Head and Neck Surgery, 2015], patients were divided into four groups: (1) recovered: a final hearing level <25 dB regardless of the size of the gain; (2) markedly effective: >30 dB of gain for the average hearing threshold; (3) effective: gains >15 dB and <30 dB; and (4) ineffective: <15 dB of gain.
Evaluation of Associated Factors
The participants were interviewed mainly regarding their health conditions. Clinical and demographic data were collected from medical records. Demographic data included age and sex. The presence of the following chronic diseases or disorders was ascertained during the interviews: hypertension, diabetes, hyperlipidemia and a history of cholesteatoma, otitis media with effusion, or chronic otitis media. In addition, dizziness episodes were also recorded.
Follow-Up
All patients participated in two separate telephone follow-ups conducted by two different independent doctors from January 2016 to April 2016 and from April 2018 to October 2018. The patients were asked about changes in tinnitus and when the changes had occurred (Fig. 1).
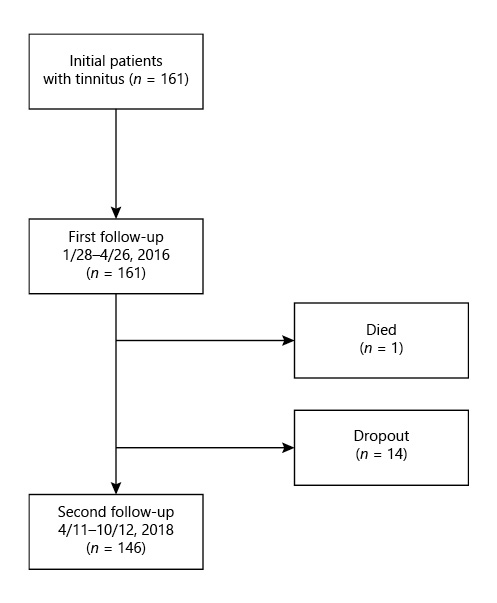
Fig. 1
Follow-up flowchart.
Main Outcome Measures
Several possible factors were considered, including sex, age, the duration between disease onset and treatment, laterality, the tone of tinnitus, the initial level of tinnitus, the severity of HL at admission, hearing recovery, follow-up tinnitus, follow-up time points, and other factors.
Statistical Analysis
The clinical and epidemiological characteristics of the patients were summarized by descriptive statistics. Data sets were described with the median and/or range. Numerical data were compared using t test, and categorical data were compared using the χ2 test. Here we set the recovery of tinnitus as the endpoint. The recovery rate of tinnitus was calculated using the Kaplan-Meier method, and the log-rank test evaluated differences between tinnitus recovery rate distributions. Multivariate analyses were performed to analyze factors related to the outcome of tinnitus at discharge, and Cox proportional hazard models were applied to examine the recovery rate with adjustments for other variables using a limited backward selection procedure. Risk ratios are presented with 95% confidence intervals. Statistical significance was defined as a two-tailed p < 0.05 for all analyses. Statistical analyses were performed using SPSS software version 23.0 and GraphPad Prism 7.0.
Results
Study Populations
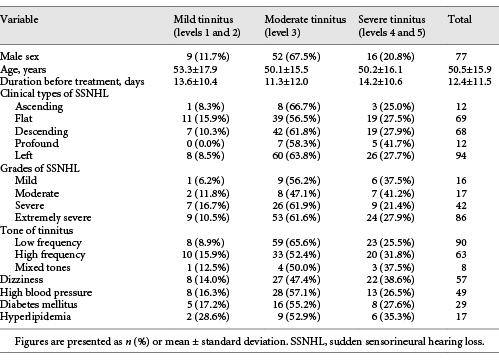
A total of 161 subjects meeting the criteria were included, with an average age of 50.5 ± 15.9 years (range, 9–83). The male:female ratio was 77:84. Among all the subjects, 57 patients had vertigo symptoms. The proportion of patients with chronic diseases was not high, as 49 patients had high blood pressure, 29 patients had diabetes, and 17 patients had hyperlipidemia.
In this study, none of the 161 enrolled patients had level 0 or 6 tinnitus. There were 3 cases of level 1 (1.9%), 16 cases of level 2 (9.9%), 96 cases of level 3 (59.6%), 41 cases of level 4 (25.5%), and 5 cases of level 5 (3.1%). To avoid large difference between the groups, we divided all the patients into three groups according to their initial level of tinnitus: 19 were in the mild group (levels 1 and 2), 96 were in the moderate group (level 3), and the remaining 46 were in the severe group (levels 4 and 5). The basic information of the 161 patients at admission is presented in Table 1.
General Tinnitus Improvement at Discharge and Analysis of Correlated Factors
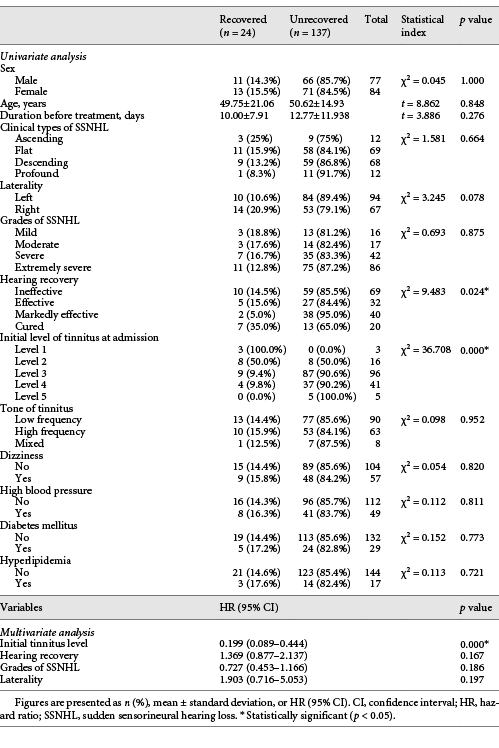
According to the improvement evaluation of tinnitus, we divided the 161 patients into four groups at discharge: 24 cases were cured (14.9%), 11 cases were markedly effective (6.8%), 75 cases were effective (46.6%), and the remaining 51 cases were invalid (31.7%). The total effective rate was 68.3%. A t test and the χ2 test were used for statistical analysis of related factors (Table 2). There was no obvious correlation between general health conditions of patients, including hypertension, hyperglycemia, hyperlipidemia, and dizziness, with the outcome of tinnitus at discharge. The improvement of tinnitus at discharge was related to the initial level of tinnitus at admission, hearing recovery, and laterality (p < 0.1). Then, binary logistic regression analysis was applied to explore the independent related factors of tinnitus improvement at discharge. Here, we incorporated statistically remarkable factors including the initial level of tinnitus at admission, hearing recovery, laterality, and SSNHL grades, which were not statistically moderate but were clinically remarkable, into a multivariate analysis. The analysis showed that the initial level of tinnitus was an independent relevant factor for the improvement of tinnitus at discharge (p = 0.000).
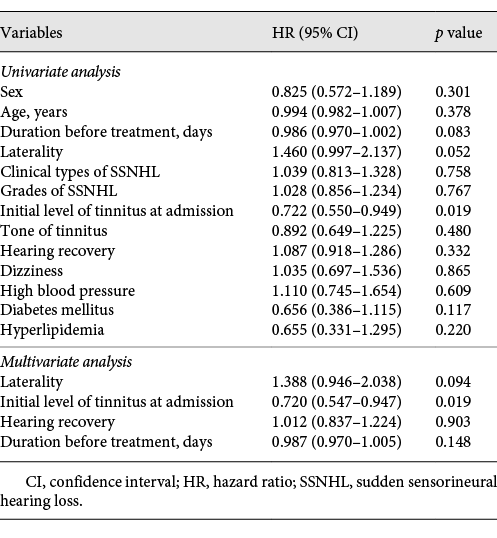
Influencing Factors of the Long-Term Prognosis for Residual Tinnitus after SSNHL
Based on the results of two follow-ups, among all the 161 patients, 115 were recovered (levels 0 and 1), 14 were dropouts, 1 had died, and the other 31 cases were in level 2 (n = 15), level 3 (n = 13), level 4 (n = 2), and level 5 (n = 1). Because of the large differences in the group numbers among different tinnitus levels, we divided the final tinnitus prognoses of all the subjects into recovered (including grades 0 and 1) and unrecovered. First, univariate Cox regression analysis was used to screen the possible influencing factors (Table 3). The analysis showed that the laterality of SSNHL and the initial tinnitus degree may be related to the long-term prognosis of tinnitus (p < 0.05). Then, the duration before treatment (0.05 < p < 0.10), the laterality of SSNHL, and the initial level of tinnitus, as well as hearing recovery at discharge, which was not statistically remarkable but was clinically remarkable, were all included in the multivariate Cox regression analysis. The results showed that the initial level of tinnitus was an independent factor for the long-term prognosis of residual tinnitus after SSNHL.
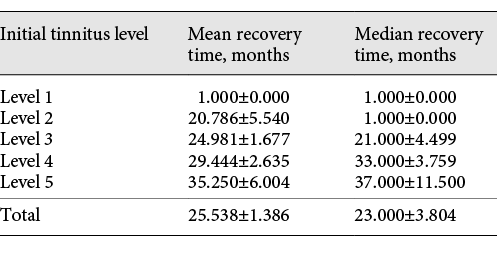
Finally, the recovery rate of patients with different initial tinnitus levels were calculated using the Kaplan-Meier method (Fig. 2). Moreover, the median recovery time of patients with different initial tinnitus levels can be used to predict the recovery time of tinnitus for patients with different initial levels (Table 4). The analysis showed that tinnitus at all levels tended to recover with time. A higher initial degree of tinnitus corresponded to a prolonged recovery time. The median times for tinnitus recovery for patients with initial tinnitus levels of 1–5 were as follows: 1.00 ± 0.00 months, 21.00 ± 4.50 months, 33.00 ± 3.76 months, and 37.00 ± 11.50 months, respectively. The median recovery time for all cases was 23.00 ± 3.80 months (Table 4).
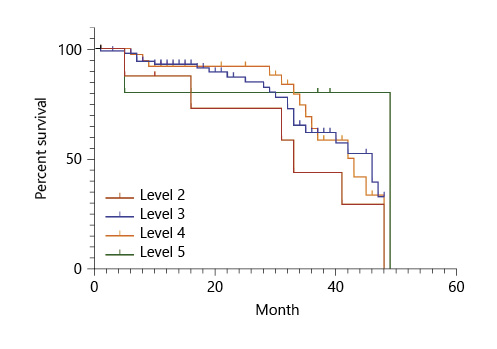
Fig. 2
Recovery rate curves of patients with different initial tinnitus levels (K-M curve).
Discussion
Summary of the Main Results
In this study, we found that most initial tinnitus along with the onset of SSNHL of the cases was classified as level 3 and 4. The prognosis of tinnitus after SSNHL had no relationship with grades of HL or hearing recovery. Initial tinnitus level was remarkably associated with tinnitus improvement at discharge and an independent risk factor for the long-term prognosis of residual tinnitus after SSNHL. The median recovery time was 23.00 ± 3.80 months.
Hearing Recovery Is Related to the Short-Term Prognosis of Tinnitus after SSNHL
A total of 68.3% of the patients showed improvement in tinnitus to varying degrees at discharge, and hearing recovery was found to be a nonindependent factor related to the short-term prognosis of tinnitus, but had nothing to do with the long-term prognosis of tinnitus. Regarding the pathology of tinnitus described earlier, HL is the trigger of tinnitus. At the time of discharge, 92 patients (57.1%) showed improvement in hearing, but the degree of hearing recovery is not completely consistent with the prognosis of tinnitus. Even if hearing improves to some extent, the effect on the intensity of tinnitus is minimal. Therefore, we cannot simply use hearing recovery to explain the relief of tinnitus. The occurrence of tinnitus consisted of two components: perception and reaction [Tunkel et al., 2014]. Reaction represents a complex connection between the auditory and the emotional system. Several investigations have verified the spontaneous remission of psychiatric symptomatology over a waiting period [Belli et al., 2008; Geocze et al., 2013]. The social desirability hypothesis states that no true change occurs in the number or intensity of symptoms, but instead, an increase in the threshold for reporting their presence occurs. The item content-priming cue-recall hypothesis states that over time and after repeated exposure to these items, subjects will report less negative states due to habituation or extinction [Arrindell, 2001]. A meta-analysis of 11 studies with 314 individuals distressed by tinnitus who were randomly allocated to a waiting period of 6–12 weeks revealed mean decreases in symptoms of 3–8% [Hesser et al., 2011]. The short-term prognosis of tinnitus may be related to a decrease in the reaction [Michiba et al., 2013; Mühlmeier et al., 2016; Ding et al., 2018]. As HL improves, patients’ psychological reaction to tinnitus decreases. This result is also in line with the research of Nogueira-Neto et al. [2016], in which there was a correlation between tinnitus and hearing improvement in patients with SSNHL only in the emotional domain of Handicap Inventory, but this correlation is considered poor. On the other hand, the long-term prognosis of tinnitus is thought to be more related to brain plasticity. Moreover, studies have suggested that tinnitus did not impair the perception of external sounds, and proposed that there is a bottom-up pathway for the external sound and a separate top-down pathway for tinnitus. The hearing difficulty complained of by tinnitus patients is mainly due to tinnitus comorbid conditions and secondary effects [Zeng et al., 2020].
Long-Term Prognosis of Residual Tinnitus after SSNHL
Over time, the degrees of tinnitus in patients with different initial tinnitus levels were all alleviated to a certain extent. The degree of tinnitus relief and recovery time are only related to the initial degree of tinnitus and the median recovery time for all patients was 23 months.
Previous studies on residual tinnitus after SSNHL have shown a tendency for gradual improvement [Michiba et al., 2013; Zhong et al., 2019]. In 2013, Michiba et al. found that tinnitus appeared to improve 6 months after treatment but did not remarkably change between 6 and 24 months. In this article the median recovery time showed that 2–3 years may be required for tinnitus to recover, different from that of Michiba et al. [2013], which may be due to the fact that the initial tinnitus levels of the patients included in this study were generally severe (the proportion of moderate to severe tinnitus was as high as 87.65%). A large cohort study found that 55% of patients with severe tinnitus reported only moderate, or mildly bothersome, symptoms 5 years later [Gopinath et al., 2010]. Conversely, 45% of tinnitus patients in the same cohort progressed from mildly annoying symptoms at baseline to moderate or severely annoying symptoms after 5 years. Tinnitus may improve spontaneously. In 2002, Nondahl et al. found that nearly 50% of patients with significant tinnitus (moderate severity, sleep problems, or both) improved after 5 years, with 43% of those improved reporting complete resolution and the remaining 57% reporting only mild symptoms. Gopinath et al. [2010] also reported that 82% of patients who reported tinnitus at baseline had persistent tinnitus after 5 years, suggesting close to a 20% rate of spontaneous improvement. Such improvements may be associated with the plasticity of the central auditory pathway. The tinnitus habituation theory [Cima et al., 2019] proposes that the brain selects which stimuli to ignore, and only the information that is considered valuable or dangerous will be perceived by the brain. According to this theory, most people consider the tinnitus of low informational value and that it does not require a reaction. However, tinnitus-related distress occurs when this processes is malfunctioning, which is more likely at times of increased stress, subsequently straining the cognitive resources causing chronic tinnitus and creating a vicious cycle with the emotional system [Cima et al., 2019]. Recent studies have confirmed that once HL starts, the most active compensation occurs in the thalamus, but not all of these signals can be transmitted to the auditory cortex. Meaningless and nonhazardous sounds are adapted to and ignored by the frontal-striatal circuits in the midbrain when patients do not pay attention to tinnitus over time. The frontal-striatal circuit region mainly consists of the ventromedial prefrontal cortex, the nucleus accumbens, and other important areas. These circuits can be collectively called the tinnitus clearance system as a gatekeeper of tinnitus. This explanation accounts for the clinical observation that most tinnitus cases resolve naturally [Lai et al., 2017, 2018; Cima et al., 2019]. However, if a problem arises with this “gatekeeper”, the ability to clear tinnitus signals will be impaired. As a result, tinnitus may persist for a prolonged period. Factors affecting the function of this gatekeeper may include, but are not limited to, sleep, migraine, estrogen decline [Lai et al., 2017], trauma, depression, and sleep-disordered breathing [Yu and Ma, 2017; Lai et al., 2018; Ma et al., 2021]. However, some patients cannot self-recover and continue to experience slight intermittent tinnitus. Such patients should be given adequate education and counseling to relay that tinnitus is a “scar” on the auditory system, which may rationalize tinnitus, thus eliminating patients’ irrational thoughts and fear of tinnitus.
Limitations
This study concentrated on the Chinese population, so the treatment and evaluation standard for tinnitus are all based on Chinese guidelines, which may result in certain regional limitations. Second, this study was a retrospective analysis and patient follow-up was done by telephone, which could have caused a information bias in the statistical analysis. Third, an anxiety and depression scale was not used to score the subjects’ mental state, which may have impacted the analysis of the influencing factors. Moreover, most of the patients enrolled in this study had severe HL and the hearing recovery rate was low, which may have resulted in a bias in the analysis of the relationship between hearing recovery and tinnitus prognosis. In the end, the follow-up interval in this study was relatively long at nearly 2 years, which can only reflect the status of tinnitus during the follow-up and illustrate the trend of tinnitus outcomes, but cannot accurately locate the time point when tinnitus began to improve.
Conclusion
Residual tinnitus after SSNHL has a tendency of self-recovery. The short-term prognosis of tinnitus may be related to psychological changes caused by hearing recovery, while the long-term prognosis of residual tinnitus after SSNHL is related only to the initial tinnitus level and has no obvious correlation with the degree of HL and the general condition of the patients. Finally, the median recovery time is approximately 2 years.
Statement of Ethics
This cohort research was approved by the Peking University People’s Hospital Research Ethics Committee (Beijing, China; No. 2015phb224-01). Written informed consent for publication of the clinical data was received from each patient or from the guardians of the patients who were under 18 years of age.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors have not funding sources to declare.
Author Contributions
T. Diao designed and conceptualized the study, collected and analyzed the data, and drafted the manuscript for intellectual content. J. Li helped collect and analyze the data. X. Ma and J.-T. Lai (co-corresponding authors) designed and conceptualized the study, interpreted the data, and revised the manuscript. L. Yu helped interpret the data. J. Zhang, Y. Wang, H. Zheng, Y. Jing, and L. Han all participated in data collection.
References
- 1. Arrindell WA. Changes in waiting-list patients over time: data on some commonly-used measures. Beware! Behav Res Ther. 2001 Oct;39(10):1227–47.
- 2. Belli S, Belli H, Bahcebasi T, Ozcetin A, Alpay E, Ertem U. Assessment of psychopathological aspects and psychiatric comorbidities in patients affected by tinnitus. Eur Arch Otorhinolaryngol. 2008;265(3):279–85.
- 3. Biesinger E, Heiden C, Greimel V, Lendle T, Höing R, Albegger K. [Strategies in ambulatory treatment of tinnitus]. HNO. 1998;46(2):157–69.
- 4. Cima RF, Mazurek B, Haider H, Kikidis D, Lapira A, Noreña A, et al A multidisciplinary European guideline for tinnitus: diagnostics, assessment, and treatment. HNO. 2019;67(S1Suppl 1):10–42.
- 5. Ding X, Zhang X, Huang Z, Feng X. The Characteristic and Short-Term Prognosis of Tinnitus Associated with Sudden Sensorineural Hearing Loss. Neural Plast. 2018;2018:6059697.
- 6. "[Interpretation of Chinese 2012 tinnitus experts consensus]." 2012. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 47 (9): 709-12.
- 7. "[Guideline of diagnosis and treatment of sudden deafness (2015)]." 2015. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 50 (6): 443-7.
- 8. Geocze L, Mucci S, Abranches DC, Marco MA, Penido NO. Systematic review on the evidences of an association between tinnitus and depression. Rev Bras Otorrinolaringol (Engl Ed). 2013;79(1):106–11.
- 9. Gopinath B, McMahon CM, Rochtchina E, Karpa MJ, Mitchell P. Incidence, persistence, and progression of tinnitus symptoms in older adults: the Blue Mountains Hearing Study. Ear Hear. 2010;31(3):407–12.
- 10. Hesser H, Weise C, Rief W, Andersson G. The effect of waiting: a meta-analysis of wait-list control groups in trials for tinnitus distress. J Psychosom Res. 2011 Apr;70(4):378–84.
- 11. Lai JT, Liu CL, Liu TC. Hormone replacement therapy for chronic tinnitus in menopausal women: our experience with 13 cases. Clin Otolaryngol. 2017;42(6):1366–9.
- 12. Lai RZ, Ma X. [Hearing loss and the switch of tinnitus-NAc]. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2017;31(7):493–5.
- 13. Lai JT, Shen PH, Lin CY, Liu CL, Liu TC. Higher prevalence and increased severity of sleep-disordered breathing in male patients with chronic tinnitus: our experience with 173 cases. Clin Otolaryngol. 2018;43(2):722–5.
- 14. Langguth B, Kreuzer PM, Kleinjung T, De Ridder D. Tinnitus: causes and clinical management. Lancet Neurol. 2013;12(9):920–30.
- 15. Ma X, Li JJ, Lai JT, Yu LS. An Integrated Physical Regulation Theory and Classification of Acute Tinnitus. Curr Med Sci. 2021;41(1):84–6.
- 16. McCormack A, Edmondson-Jones M, Somerset S, Hall D. A systematic review of the reporting of tinnitus prevalence and severity. Hear Res. 2016;337:70–9.
- 17. Michiba T, Kitahara T, Hikita-Watanabe N, Fukushima M, Ozono Y, Imai R, et al Residual tinnitus after the medical treatment of sudden deafness. Auris Nasus Larynx. 2013;40(2):162–6.
- 18. Mühlmeier G, Baguley D, Cox T, Suckfüll M, Meyer T. Characteristics and Spontaneous Recovery of Tinnitus Related to Idiopathic Sudden Sensorineural Hearing Loss. Otol Neurotol. 2016;37(6):634–41.
- 19. Noguchi Y, Takahashi M, Ito T, Fujikawa T, Kawashima Y, Kitamura K. Delayed restoration of maximum speech discrimination scores in patients with idiopathic sudden sensorineural hearing loss. Auris Nasus Larynx. 2016;43(5):495–500.
- 20. Nogueira-Neto FB, Gallardo FP, Suzuki FA, Penido NO. Prognostic and Evolutive Factors of Tinnitus Triggered by Sudden Sensorineural Hearing Loss. Otol Neurotol. 2016;37(6):627–33.
- 21. Nondahl DM, Cruickshanks KJ, Wiley TL, Klein R, Klein BE, Tweed TS. Prevalence and 5-year incidence of tinnitus among older adults: the epidemiology of hearing loss study. J Am Acad Audiol. 2002;13(6):323–31.
- 22. Nyenhuis N, Zastrutzki S, Weise C, Jäger B, Kröner-Herwig B. The efficacy of minimal contact interventions for acute tinnitus: a randomised controlled study. Cogn Behav Ther. 2013;42(2):127–38.
- 23. Ogawa K, Sato H, Takahashi M, Wada T, Naito Y, Kawase T, et al Clinical practice guidelines for diagnosis and treatment of chronic tinnitus in Japan. Auris Nasus Larynx. 2020;47(1):1–6.
- 24. Schreiber BE, Agrup C, Haskard DO, Luxon LM. Sudden sensorineural hearing loss. Lancet. 2010;375(9721):1203–11.
- 25. Tunkel DE, Bauer CA, Sun GH, Rosenfeld RM, Chandrasekhar SS, Cunningham ER Jr, et al Clinical practice guideline: tinnitus. Otolaryngol Head Neck Surg. 2014;151(2Suppl):S1–40.
- 26. Yu LS, Ma X. [Compensation and decompensation of tinnitus]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2017;52(8):630–3.
- 27. Zeng FG, Richardson M, Turner K. Tinnitus Does Not Interfere with Auditory and Speech Perception. J Neurosci. 2020;40(31):6007–17.
- 28. Zhong., Xiaosheng, Haidi Yang., and Yiqing Zheng. 2019. "Treatment and outcome of tinnitus in sudden deafness." Otolaryngol Ophthalmol Shandong Univ 33 (4) : 43-46.
T. Diao, X. Ma, and J. Li are co-first authors.