Introduction
Cochlear implantation (CI) is a surgical procedure allowing hearing rehabilitation of patients with severe to profound sensorineural hearing loss who do not benefit from hearing aids [Lenarz and Laszig, 2012; Parent et al., 2020]. It can be performed at any age, from babies with congenital hearing loss in the first few months to older adults. Since the use of this procedure, many studies have reported complications of cochlear implant surgery, and various classifications have been proposed [Kempf et al., 1999; O’Donoghue and Nikolopoulos, 2002; Nikolopoulos et al., 2004; Hansen et al., 2010; Farinetti et al., 2014]. Implantation can lead to complications that may be related to the surgical technique, patient anatomy, or implanted device. In recent years, cochlear implant complication rates have decreased due to improved surgical techniques and shrinking implants [Cohen et al., 1988; Cohen and Hoffman, 1991]. Complications can simply be classified as major (requiring surgical revision or hospital management) and minor (requiring conservative management) or according to the delay to occur (perioperative, early postoperative, and late postoperative) [Bhatia et al., 2004]. Major complications include device failure, flap necrosis, electrode migration, magnet displacement, post-acute otitis media (AOM) perforated eardrum, meningitis, or cholesteatoma, and minor complications include swelling (wound seroma or hematoma), acute middle ear inflammation, transient vertigo, wound infection, transient facial palsy, or chorda tympani nerve damage [Venail et al., 2008]. All surgeons should inform also the patients about complications and their clinic’s complication rates.
The main purpose of this study was to evaluate the complications of 1,148 adult and pediatric patients who underwent CI according to the same surgical technique by a single experienced surgeon between July 2009 and September 2020. The secondary objective was to compare the complications seen in pediatric and adult populations.
Materials and Methods
Ethical Approval
The study was approved by the Local Ethics Committee (No.2567/October 30, 2020). Due to the retrospective nature of the study, the Ethics Committee determined that no patient consent was required.
Subjects and Study Design
The CIs performed in our tertiary institution between July 2009 and September 2020 were retrospectively reviewed. Severe to profound sensorineural hearing loss was confirmed preoperatively in all patients by auditory brainstem response or pure-tone audiometry testing. Preoperative computed tomography and inner ear magnetic resonance images of all patients were reviewed to determine abnormalities in the inner ear and vestibulocochlear nerve. All CI decisions were made by a council of otolaryngologist, audiologist, radiologists, speech-language therapists, and psychologists. Surgical procedures (unilateral or bilateral CI and revision surgery) were performed under general anesthesia by a single experienced surgeon. Cochlear implant surgery is not performed in our country in children younger than 1 year of age. These children are diagnosed until 3 months of age. Afterward, we recommend special education to these patients. These patients wear bilateral hearing aids until surgery. Routine plain X-ray was taken in all patients on the first postoperative day to assess the appropriate electrode placement. After intraoperative antibiotic prophylaxis, antibiotherapy was continued until the patient was discharged on the second postoperative day. All patients were invited for at least 1-year control with 2-month intervals of visits.
The complications in these series were classified as minor or major. Minor complications were complications requiring conservative management (e.g., transient facial nerve palsy, vertigo, seroma/hematoma, or wound infection). Major complications were complications resulting in a serious medical condition (e.g., meningitis) or requiring major surgical revision (e.g., for cholesteatoma, perforated eardrum, flap necrosis, or device failure).
Surgical Technique
The same experienced surgeon performed all surgeries and used the intraoperative NIM® nerve monitoring system to help reduce the risk of facial nerve damage (NIM-Response 3.0; Medtronic, Jacksonville, FL, USA). We administered single-dose intraoperative antibiotic prophylaxis to our patients as recommended by the US Food and Drug Administration (FDA). Routine surgical procedure was used in all patients. We marked the skin for the location of retro-auricular incision and also for the internal unit of the implant at a 45° angle. A retro-auricular incision (3–4 cm) was made. The anteriorly based musculoperiosteal (palva) flap was cut, which should lie anterior to the skin incision and should not be just under incision, to elevate the periosteum on the mastoid surface. A subperiostal pocket was created along the surface of the parietal region for the internal unit of the implant by using a Freer elevator on the marked skin area. Cortical mastoidectomy was performed, and the short process of the incus was identified. The round window niche was visualized after the posterior tympanotomy. Round window or promontorium cochleostomy was drilled by Visao® to enable electrode insertion into the cochlea (Visao Cochleostomy Handpiece, Medtronic, Jacksonville, FL, USA). After the electrode array was placed, the evoked stapedial reflex and electrically evoked compound action potentials were checked. Finally, the wound was closed, and pressure dressing was applied.
Implanted Devices
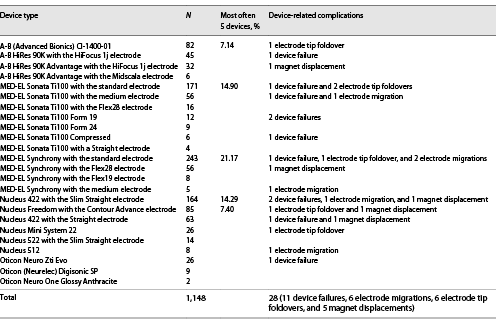
The implant devices used were MED-EL® (51.05%), Nucleus® (31.35%), Advanced Bionics® (14.38%), and Oticon® (3.22%) (MED-EL Corp., Innsbruck, Austria; Nucleus devices were manufactured by Cochlear Corp., Lane Cove, Australia; Advanced Bionics, Sylmar, CA, USA; Oticon Medical, Vallauris, France) (Table 1).
Statistical Analysis
Statistical analysis was performed using the IBM® SPSS 17.0 software (SPSS Corp.; Armonk, NY, USA). Quantitative variables are expressed as mean or medians, and ordinal variables are expressed as sample size (%). In the analysis of qualitative independent data, children and adults were compared using the Pearson χ2 test. A p value less than 0.05 was considered statistically significant.
Results
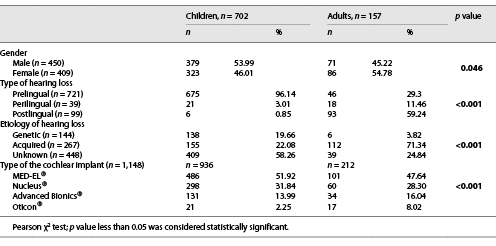
In this study, a total of 859 patients (1,148 CIs) who underwent cochlear implant surgery were retrospectively reviewed. We classified the patients under the age of 18 years as children. Seven hundred and two (81.7%) of 859 patients were children, and 157 (18.3%) were adults. The mean first implantation age of patients was 10.2 years (range 1–75 years), and 450 (52.4%) of the patients were male, while 409 (47.6%) were female.
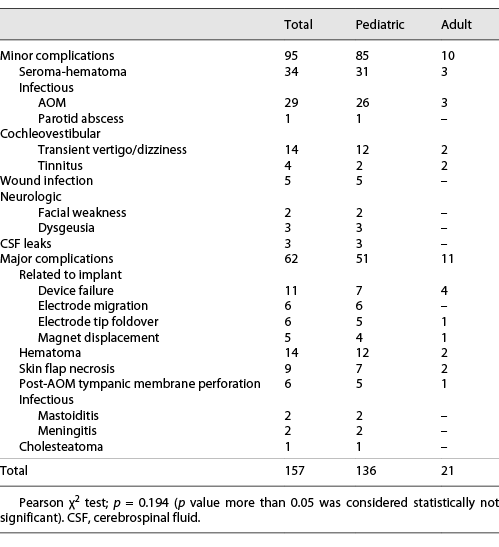
We detected complications in 157 of 859 implanted patients. The overall complication rate was 13.68%, comprising 5.4% of major complications (62 cases) and 8.28% of minor complications (95 cases). Swelling (wound seroma or hematoma) was the most common minor complication. The most common cause of major complications was related to implanted devices (e.g., device failure, electrode migration, electrode tip foldover, and magnet displacement).
We recorded clinical data including gender, the type of hearing loss, etiology of hearing loss, and the type of cochlear implant (Table 2). The most common hearing loss type was prelingual in children. The rate of those with unknown etiology of hearing loss was higher in the children than in adults, whereas the rate of acquired hearing loss history was higher in the adult group than in children. Despite the high rates of minor complications in children, there was no statistically significant difference between children and adults. We could not find any significant difference between manufactures of implanted devices in regard of complications. Additionally, there was no difference between genders.
Minor Complications
A total of 95 minor complications requiring conservative treatment were observed in 85 children and 10 adults (Table 3). The most common minor complications were seroma/hematoma (35.79% of minor complications) followed by infectious complications (31.58%), cochleovestibular complications (18.95%), skin flap-related complications (5.26%), neurologic complications (5.26%), and cerebrospinal fluid leaks (3.16%).
Swelling (wound seroma or hematoma) was observed mainly in the pediatric population (31 children and 3 adults) and regressed with needle aspiration and/or pressure dressing. No additional surgery was performed.
AOM was identified in 29 patients (26 children and 3 adults), and parotid abscess was seen in only one pediatric patient as minor infectious complications occurring in the first 2 months after implantation. All of them were treated by empirical oral antibiotic therapy (amoxicillin-clavulanic acid 80 mg/kg/day). Although pneumococcus was included in the pediatric vaccination schedule in our country, two of these AOM patients were complicated with meningitis. Six of these patients with AOM were complicated by tympanic membrane perforation and subsequently treated with myringoplasty.
Cochleovestibular complications included transient vertigo/dizziness and tinnitus in the implanted ear. Vertigo/dizziness was observed in 14 patients (12 children and 2 adults) and tinnitus in 4 patients (2 children and 2 adults). All vertigo/dizziness complaints were seen in the early postoperative period. Our youngest child with this complaint was 7 years old. The patients were followed up by extending their hospital stay, and their complaints regressed without the need for additional medical treatment. After routine vertigo tests, a 2-month posturography and rehabilitation program was applied to our adult patients with vertigo symptom.
Minor wound infections were observed in five children. All cases resolved after systemic antibiotic therapy and repeated outpatient wound dressings.
Neurological complications such as transient facial nerve palsy were observed in 2 pediatric patients, and taste disorders were reported by three children in the immediate postoperative period. The reason of these complaints might be the intraoperative heating of drill during posterior tympanotomy. All cases resolved with corticosteroid therapy.
Severe gusher was observed in 3 patients during cochleostomy. In preoperative examinations, two of these patients had incomplete partition type 3, and one had Mondini dysplasia. None of the patients required postoperative external lumbar cerebrospinal fluid drainage.
Major Complications
Sixty-two major complications were observed in 51 children (82.25%) and 11 adults (17.75%) and required revision surgery or hospital stay. The most common cause of major complications was related to implanted devices (39.29% of major complications) followed by major hematoma (25%), flap necrosis (16.07%), post-AOM tympanic membrane perforation (10.71%), infectious complications (mastoiditis and meningitis) (7.14%), and cholesteatoma (1.79%).
Device-related complications were detected during the routine control examination of 28 patients whose hearing deteriorated over time. These complications included device failure, electrode migration, electrode tip foldover, and magnet displacement. Device failure was seen in 11 patients (7 children and 4 adults), electrode migration was seen in 6 children, electrode tip foldover was seen in 6 patients (5 children and 1 adult), and magnet displacement was seen in 5 patients (4 children and 1 adult). All of these 28 patients, who had complications related to device, underwent explantation and reimplantation surgery.
Major hematoma was seen in 14 patients (12 children and 2 adults) with a history of trauma. They were hospitalized and followed up for a few days with surgical drainage under local anesthesia and pressure dressing. Streptococcal meningitis was observed in 2 children complicating AOM on the implant side, 3 and 5 months after implantation. One of these patients had incomplete partition type 3, and one had Mondini dysplasia. Mastoiditis was observed in two children. All of these cases were treated by myringotomy and intravenous antibiotic therapy in hospital.
Surgical revisions of the implantation site were required in 41 patients: 7 patients required surgical revision without explantation (myringoplasty was performed in 6 patients, and 1 patient had also iatrogenic cholesteatoma), and 34 patients required explantation followed by reimplantation (28 related to device complications and 6 related to flap necrosis). In 3 of 9 patients with flap necrosis, debridement and rotation scalp flap procedures were performed without implant explantation. The reimplantation rate was 3.57% (41 out of 1,148 cases).
Discussion
The global frequency of CI has regularly increased over the last 2 decades with the efficacy of this modality of hearing rehabilitation and the extension of the indications. As a result of the development of surgical techniques and implant devices over the years, complications have regularly decreased [Qiu et al., 2011; Tarkan et al., 2013; Farinetti et al., 2014]. The main objective of this study was to analyze the minor and major complications observed after CI in adults and children in our tertiary referral institution and to compare these results with the literature.
One of the first articles describing CI complications was published by Cohen in 1991, which corresponds to a complication rate of 11.8%. In 1995, Hoffman reported a similar global complication rate of 12.2% with major complications of 7.4% in his 4,969 implant series [Cohen and Hoffman, 1991; Hoffman and Cohen, 1995; Balkany et al., 2005]. Similar to these studies, the overall complication rate in our study was 13.68%.
Infection rates in the literature range from 1.7% to 12%. The infection rate in our series was 4.18% (AOM, skin flap necrosis, wound infections, mastoiditis, meningitis, or parotid abscess). We observed that the risk of infection was higher in children. The most common infectious complication in our study was AOM, similar to the literature [Cunningham et al., 2004; Hopfenspirger et al., 2007], and most of them responded to empirical antibiotic therapy; 6 were operated because of the tympanic membrane perforation, and 2 were treated with intravenous antibiotics for meningitis.
Risk factors associated with wound infections in CI include comorbidities, immunodeficiency, middle-ear inflammation and prolonged operation time [Theunisse et al., 2018]. Although these factors were not identified in this study, 5 patients had minor wound infection, and 9 skin flap necrosis. In our study, the rate of skin infection-related complications was 14 out of 1,148 (1.22%). Minor wound infections resolved in response to systemic antibiotic therapy, and in flap necrosis patients, debridement and rotation scalp flap procedures were performed (6 patients required explantation followed by reimplantation).
When all infectious causes were excluded, the most common minor complication was swelling (seroma/hematoma), and its rate in our study was 4.18%. Fourteen of the 48 hematoma patients were evaluated as major complications and required surgical drainage. The swelling in the minor complication group regressed with needle aspiration and/or pressure dressing. Trauma, incision type, and coagulopathy were the predisposing factors for hematoma, but most of them were idiopathic. In different studies, this rate ranges from 1.92 to 5.8% [Bhatia et al., 2004; Venail et al., 2008; Tarkan et al., 2013; Halawani et al., 2019; Dağkıran et al., 2020].
Incidence of facial paralysis had been estimated as 0.4–0.71% in the literature [Bhatia et al., 2004; Venail et al., 2008; Tarkan et al., 2013]. In our study, the facial-nerve-related complication rate was found to be compatible with the literature (0.44%) and regressed in the control examinations. In a study published by Theunisse et al. [2018], chorda tympani lesions were found to be the most common complication [Theunisse et al., 2018]. During posterior tympanotomy, irrigation with abundant water may reduce the dysfunction rate of the chorda tympani.
Vertigo is a common adverse effect of CI [Venail et al., 2008]. Young pediatric patients may not be able to fully describe their symptoms. Therefore, the rate may be higher than reported in the literature [Qiu et al., 2011]. In our series, the overall rate of vestibulocochlear complications had found to be 1.57%. All cases resolved within 1 week.
In the literature, cholesteatoma was observed in around 1% of patients after CI [Bhatia et al., 2004]. In our study, cholesteatoma was very rare, and it was seen in only one patient.
There have been some changes in our surgical technique in recent years according to the complication rates of our clinic. We diminished the incision size over the past years. We drilled out a groove for the cable of electrode between the internal unit and mastoid cavity if we use the MED-EL implant since 2018. The fixation of the cable of the implant by using ionomeric bone cement in the mastoid cavity was performed in order to prevent the electrode migration since 2018. Additionally, the rate of major complications decreased in recent years. For example, the patient with cholesteatoma formation was our one of the first implantations, and the rate of skin flap necrosis and electrode migration decreased.
Conclusions
CI is a well-defined surgery that can be safely performed by experienced otolaryngologists. It is a source of hope especially for babies born with severe to profound bilateral sensorineural hearing loss. Although the complication rates have decreased over the years, it is around 10%. Major complication rates are even lower. Children have a higher revision rate than adults. Surgeons should evaluate their patients preoperatively well, perform operations with sufficient knowledge and necessary equipment, be aware of postoperative complications, apply appropriate procedures, and inform patients about their surgical complication rates.
Statement of Ethics
This study was approved by the Institution’s Ethics Committee under protocol no. 2020/2567. Due to the retrospective nature of the study, the Ethics Committee determined that no patient consent was required.
Conflict of Interest Statement
The authors declare no conflicts of interest or any commercial relation with the contents of the manuscript.
Funding Sources
This study was not funded by any governmental or private sponsor.
Author Contributions
Ozan Ozdemir, Ozgur Yigit, Efe Can, and Cigdem Kalaycik Ertugay: drafting and editing the work, analysis and interpretation of data, providing final approval, and agreement to be accountable.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
- 1. Balkany TJ, Hodges AV, Buchman CA, Luxford WM, Pillsbury CH, Roland PS, et al. Cochlear implant soft failures consensus development conference statement. Cochlear implants int. 2005;6(3):105–22.
- 2. Bhatia K, Gibbin KP, Nikolopoulos TP, O’Donoghue GM, et al. Surgical complications and their management in a series of 300 consecutive pediatric cochlear implantations. Otol Neurotol. 2004;25(5):730–9.
- 3. Cohen NL, Hoffman RA. Complications of cochlear implant surgery in adults and children. Ann Otol Rhinol Laryngol. 1991;100(9):708–11. http://dx.doi.org/10.1177/000348949110000903.
- 4. Cohen NL, Hoffman RA, Stroschein M. Medical or surgical complications related to the Nucleus multichannel cochlear implant. Ann Otol Rhinol Laryngol Suppl. 1988;135(5_Suppl 2):8–13. http://dx.doi.org/10.1177/00034894880975s202.
- 5. Cunningham CD III, Slattery WH III, Luxford WM. Postoperative infection in cochlear implant patients. Otolaryngol Head Neck Surg. 2004;131(1):109–14. http://dx.doi.org/10.1016/j.otohns.2004.02.011.
- 6. Dağkıran M, Tarkan Ö, Sürmelioğlu Ö, Özdemir S, Onan E, Tuncer Ü, et al. Management of complications in 1452 pediatric and adult cochlear implantations. Turk Arch otorhinolaryngol. 2020;58(1):16.
- 7. Farinetti A, Ben Gharbia D, Mancini J, Mancini J, Roman S, Nicollas R, et al. Cochlear implant complications in 403 patients: comparative study of adults and children and review of the literature. Eur Ann Otorhinolaryngol Head Neck Dis. 2014 Jun;131(3):177–82.
- 8. Hoffman RA, Cohen NL. Complications of cochlear implant surgery. Ann Otol Rhinol Laryngol Suppl. 1995;166:420–2.
- 9. Halawani R, Aldhafeeri A, Alajlan S, Alzhrani F, et al. Complications of post-cochlear implantation in 1,027 adults and children. Annals of Saudi medicine. 2019;39(2):77–81.
- 10. Hansen S, Anthonsen K, Stangerup SE, Jensen JH, Thomsen J, Cayé-Thomasen P. Unexpected findings and surgical complications in 505 consecutive cochlear implantations: a proposal for reporting consensus. Acta Otolaryngologica. 2010;130(5):540–9.
- 11. Hopfenspirger MT, Levine SC, Rimell FL. Infectious complications in pediatric cochlear implants. Laryngoscope. 2007;117(10):1825–9. http://dx.doi.org/10.1097/MLG.0b013e3180de4d35.
- 12. Kempf HG, Johann K, Lenarz T. Complications in pediatric cochlear implant surgery. Eur Arch Otorhinolaryngol. 1999;256(3):128–32. http://dx.doi.org/10.1007/s004050050124.
- 13. Lenarz T, Laszig R. Cochlea-implantat versorgung und zentral-auditorische implantate. In: Guideline of the German Society for Ear, Nose and Throat Medicine, Head and Neck Surgery. Register number 017–071. Bonn: German Society of Oto-Rhino-Laryngology, Head and Neck Surgery; 2012.
- 14. Nikolopoulos TP, Dyar D, Gibbin KP. Assessing candidate children for cochlear implantation with the Nottingham Children’s Implant Profile (NChIP): the first 200 children. Int J Pediatric otorhinolaryngol. 2004;68(2):127–35.
- 15. O’Donoghue GM, Nikolopoulos TP. Minimal access surgery for pediatric cochlear implantation. Otol Neurotol. 2002;23(6):891–4. http://dx.doi.org/10.1097/00129492-200211000-00014.
- 16. Parent V, Codet M, Aubry K, Bordure P, Bozorg-Grayeli A, Deguine O, et al. The French cochlear implant registry (EPIIC): cochlear implantation complications. Eur Ann Otorhinolaryngol Head Neck Dis. 2020 Sep;137(Suppl 1):S37–S43.
- 17. Qiu J, Chen Y, Tan P, Chen J, Han Y, Gao L, et al. Complications and clinical analysis of 416 consecutive cochlear implantations. Int J Pediatr Otorhinolaryngol. 2011;75(9):1143–6.
- 18. Tarkan Ö, Tuncer Ü, Özdemir S, Sürmelioğlu Ö, Çetik F, Kıroğlu M, et al. Surgical and medical management for complications in 475 consecutive pediatric cochlear implantations. Int J Pediatr Otorhinolaryngol. 2013;77(4):473–9.
- 19. Theunisse HJ, Pennings RJ, Kunst HP, Mulder JJ, Mylanus EAM. Risk factors for complications in cochlear implant surgery. Eur Arch Otorhinolaryngol. 2018;275(4):895–903.
- 20. Venail F, Sicard M, Piron JP, Levi A, Artieres F, Uziel A, et al. Reliability and complications of 500 consecutive cochlear implantations. Arch Otolaryngol Head Neck Surg. 2008;134(12):1276–81.