Psychodynamic psychotherapy is a longstanding psychological intervention within psychiatry. As such, its positioning in the treatment of depression is important. However, whether it should be recommended within treatment guidelines and what form of therapy (short or long term) is supported by evidence, has been a point of contention with prior discussion in the pages of Australasian Psychiatry. Therefore, to provide an independent perspective, the recommendations made by the College guideline for mood disorders (MDcpg2020) are compared to those made by the recently published NICE guidelines. The latter were chosen because of the rigour with which the evidence was examined and because the time period surveyed overlapped with that examined by the MDcpg2020.
NICE guidelines (UK): On June 29th 2022, the National Institute for Health and Care Excellence (NICE) published guidelines for the management of depression (NG222). These guidelines were developed with extensive input from a broad range of stakeholders. The culmination of this tremendous effort is a document that provides succinct, clear guidance for the management of depression that is based on a detailed analysis of pertinent evidence.
Positioning of STPP
This brief article focuses on the positioning of STPP in the management of acute depression. First, it compares the approach taken by the MDcpg2020 and the NG222 with respect to the management of depression using psychological interventions. Second, the recommendations made by the NG222 are compared to those in the MDcpg2020. Third, and finally, some key points are provided – noting that by and large the NG222 reaffirm the MDcpg2020 recommendations.
Comparison of the approach taken by the MDcpg2020 and the NG222
Diagnosis
As would be expected, the NG222 underscore the importance of careful evaluation and accurate diagnosis. And as regards management, they follow the MDcpg2020 lead by assigning primacy to psychological treatments where available and emphasise the importance of a broader therapeutic approach that includes lifestyle interventions such as diet and exercise. Further, in a similar fashion to the MDcpg2020, the NG222 aim to inform and advise. In other words, they are not prescriptive per se, although clearly whenever possible, it is common sense to pursue strategies where there is evidentiary support.
In the NICE guidelines depression is defined broadly according to the criteria stipulated in the International Classification of Diseases 11 (ICD-11) and the Diagnostic and Statistical Manual of mental disorders (DSM-5). Depression is taken to refer to ‘a wide range of mental health problems characterised by the absence of a positive affect (a loss of interest and enjoyment in ordinary things and experiences), low mood and a range of associated emotional, cognitive, physical, and behavioural symptoms’. In addition to this syndromic definition, severity is mapped on a continuum that consists of three elements: these are the symptoms which can vary in frequency and intensity, the duration of the depressive disorder, and the impact it has on personal and social functioning. In other words, severity is not simply a function of the number of symptoms but also captures chronicity and the extent of impairment that the illness confers.
This is very similar to the MDcpg2020 in which depression is diagnosed according to a number of schema that are complementary and include DSM-5, severity, and subtypes that are defined according to clinical profiles. In addition, the MDcpg2020 allowed for the ACE model that emphasises similar domains to ICD-11 and provides a further dimensional aspect to severity and syndromic classification.
Consequently, the NG222 partitions new episodes of depression as ‘less severe or more severe depression’. These categories are groupings of previously used descriptors – sub-threshold, mild, moderate and severe. In this new grouping, less severe refers to sub-threshold and mild depression, whereas more severe refers to moderate and severe depression. The reason for dividing depression as such, is that the guideline developers wanted to reflect the evidence pertaining to classification and further, use a division that would enhance the uptake of guideline recommendations in clinical practice.
Again, this approach is similar to the stance adopted by the MDcpg2020, in which subtypes are acknowledged but the heterogeneity of the illness is respected and it is recognised that other than very specific kinds of depression such as psychosis and melancholia, in the main, depression is best treated more broadly and largely according to the functional impairment it confers. Thus, a single overarching schema is presented for the management of acute depression that systematically builds through Actions, Choices and Alternatives. In this schema, the clinician decides on the basis of information available to them how to characterise the illness and formulate its management.
Efficacy, effectiveness and cost
A key difference, and an important additional component that NG222 provides as compared to MDcpg2020, is the incorporation of cost alongside effectiveness. When evaluating treatments and management strategies, the MDcpg2020 focused primarily on efficacy and side-effects (tolerability). These clinical considerations were given importance because in practice the first question most clinicians will (or at least should) consider is whether a particular treatment works. In other words, does it have proven efficacy. If so, then the second consideration is whether the patient can withstand suitable therapy for a sufficient period of time for it to have an effect. The combined consideration of efficacy and tolerability provides an indication of effectiveness. However, NG222 goes one step further and additionally factors the cost of the therapy. This is an increasingly important consideration and one that is perhaps especially relevant to the Australian landscape. Notably, the inclusion of cost provides a much clearer separation of the various therapies and strategies.
The 2020 mood disorders CPG guidelines (MDcpg2020)
In the MDcpg2020, psychological interventions are a key component of Actions mandated in the management of depression. A key strength of “the psychological component is that it offers an opportunity for learning new cognitive and behavioural skills to prevent future relapse and recurrence" (section 7.1 page 62). Hence the MDcpg2020 identifies 6 psychological interventions (CBT, IPT, problem solving therapy, behavioural activation therapy, non-directive supportive therapy and STPP), chosen because each has been found to be more effective than wait list control in at least 10 RCT’s. The MDcpg2020 also note that in the outpatient treatment of major depression, there are no significant differences in the benefits derived from antidepressant therapy in comparison to psychological therapy. These recommendations within the MDcpg2020 therefore tally with those of the NG222.
NG222 recommendations for the first line treatment of less severe depression in adults
The NG222 provide a list of treatment options that are sequenced according to clinical and cost-effectiveness alongside consideration of implementation factors. The rank order of these various treatments is shown in Figure 1. In essence, group therapies are preferable, presumably largely because of cost savings. However, it is interesting to note that out of 11 first-line treatments for less severe depression, STPP is ranked last. Further, and importantly, SSRIs are positioned ahead of STPP and both individual and group CBT and behavioural activation therapy feature in the top four treatments recommended for the first-line treatment of less severe depression.
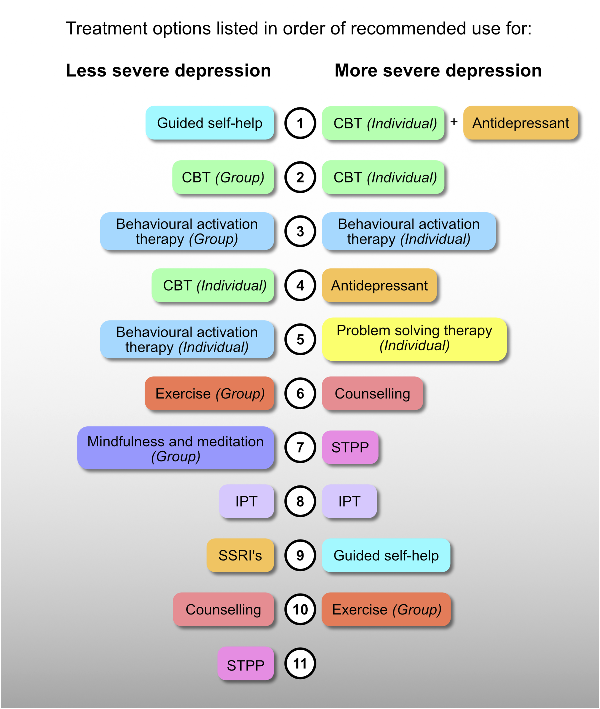
Figure 1
Schematic illustrating treatments ordered by recommended use according to NG222. Treatments are identified by separate colours, without distinguishing between mode of delivery (i.e. group or individual). In addition, SSRIs and the broader category of antidepressants are shown in the same colours for ease of interpretation. CBT = cognitive behavioural therapy; IPT = Interpersonal therapy; SSRI’s = selective serotonin reuptake inhibitors.
NG222 recommendations for the first-line treatment of more severe depression in adults
The NG222 provides 10 first-line interventions. Broadly speaking group interventions do not feature other than group exercise, which is ranked as the least cost-effective option. This may be because more severe depression often requires tailored and in-depth therapy and patients are more likely to need hospitalization. Therefore, greater emphasis is placed on individual therapies. Antidepressant medication options also become broader when treating more severe depression, extending beyond SSRIs. Further, individual problem solving that was included in the MDcpg2020 is now included as a first-line treatment.
Relevant to our present discussion, STPP features seventh out of the 10 treatments. Further, antidepressant medication is now first line alongside individual cognitive behavioural therapy, which takes pole position both in combination with antidepressants and as individual therapy.
Key points
1. Psychological interventions:
1.1. Warrant priority and should be delivered first-line either individually or in groups depending on availability and need.
1.2. Treatment should be personalised and tailored to individual needs.
2. Cognitive behavioural therapy and behavioural activation:
2.1. These are the most clinically effective and cost-effective psychological therapies.
3. Psychodynamic Psychotherapy:
3.1. Only STPP has a role in the treatment of acute depression.
3.2. STPP ranks last for less severe depression and 7th out of 10 potential therapies for more severe depression.
3.3. Counselling is ranked higher than STPP across the whole spectrum of depression (both less and more severe depression).
3.4. Long term psychodynamic therapy is not indicated for acute depression irrespective of severity.
4. Antidepressants:
4.1. Have a significant role to play in the management of depression, especially in more severe depression.
4.2. When prescribed, antidepressants should be accompanied by psychological interventions where possible.
Conclusion
Naturally, because of slightly different classificatory models there are subtle differences between the recommendations made by NG222 and by the MDcpg2020, but broadly the same therapies have been recommended and the importance attached to them is also consistent.
Disclosure The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: G.S.M. has received grant or research support from National Health and Medical Research Council, Australian Rotary Health, NSW Health, American Foundation for Suicide Prevention, Ramsay Research and Teaching Fund, Elsevier, AstraZeneca, Janssen-Cilag, Lundbeck, Otsuka and Servier; and has been a consultant for AstraZeneca, Janssen-Cilag, Lundbeck, Otsuka and Servier. P.B. has received research support from the National Health and Medical Research Council, speaker fees from Servier, Janssen and the Australian Medical Forum, educational support from Servier and Lundbeck, has been a consultant for Servier, served on an advisory board for Lundbeck, has served as DSMC Chair for Douglas Pharmaceuticals and has served on the Medicare Schedule Review Taskforce (Psychiatry Clinical Committee). M.H. has received grant or research support in the last 5 years from the National Health and Medical Research Council, Medical Research Future Fund, Ramsay Health Research Foundation, Boehringer-Ingleheim, Douglas, Janssen-Cilag, Lundbeck, Lyndra, Otsuka, Praxis and Servier; and has been a consultant for Janssen-Cilag, Lundbeck, Otsuka and Servier and has served on the Medicare Schedule Review Taskforce (Psychiatry Clinical Committee). R.M. has received support for travel to education meetings from Servier and Lundbeck, speaker fees from Servier and Committee fees from Janssen. R.P. has received support for travel to educational meetings from Servier and Lundbeck and uses software for research at no cost from Scientific Brain Training Pro. G.M. has received grant support in the last 5 years from the National Health and Medical Research Council, the Mental Illness Research Fund, Victorian Medical Research Acceleration Fund, Canadian Institutes of Health Research, Readiness, SiSU Wellness and Barbara Dicker Foundation. D.B. has received funding to host webinars by Lundbeck. All authors of this article also authored the RANZCP 2020 mood disorders guidelines. The authors E.B., R.B., P.H. and B.L. declared no further potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Malhi GS, Bell E, Bassett D, et al. The 2020 royal Australian and New Zealand college of psychiatrists clinical practice guidelines for mood disorders. Aust N Z J Psychiatry 2021; 55: 7–117. DOI:
- 2. NICE. Depression in adults: Treatment and management. London, UK: National Institute for Health Care Excellence,, 2022.
- 3. World Health Organization. International statistical classification of Diseases and related health problems (11th revision). Geneva, Switzerland: World Health Organisation, 2018.
- 4. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Fifth edition. Arlington, VA: American Psychiatric Publishing, 2013.
- 5. Cuijpers P. Four decades of outcome research on psychotherapies for adult depression: An overview of a series of meta-analyses. Canadian Psychology/Psychologie Canadienne 2017; 58: 7–19.
