Introduction
The incidence of non-functioning pancreatic neuroendocrine neoplasms (NF-PanNENs) has increased recently. Traditionally, surgery has been the treatment of choice for localized NF-PanNENs, although evidence has emerged that active surveillance could be advocated for most asymptomatic tumours no larger than 2 cm. However, the practice of active surveillance varies considerably and, contrary to current recommendations, many patients still undergo surgical resection.
Current evidence is limited by the retrospective design of studies and the small number of patients. The present study is the most extensive prospective investigation to date on small, asymptomatic NF-PanNENs. The aim was to define the optimal management of incidentally found, sporadic NF-PanNENs no larger than 2 cm.
Methods
This was a prospective, non-randomized, international, multicentre, cohort study (NCT03084770). This report describes the results of the prespecified interim analysis. Overall, 41 centres have been included. The study protocol was published previously (Appendix S1). Briefly, CT or MRI was mandatory for all patients. The diagnosis must have been proven by a positive fine-needle aspiration (biopsy) (FNA(B)) or positive 68Ga-labelled DOTA PET. The treatment—active surveillance or surgical resection—was decided by the referring centre. Because current guidelines suggest surveillance for asymptomatic NF-PanNENs 2 cm or smaller in size, treating physicians were asked to indicate the reason for choosing surgery. An aggressive feature was defined by one or more of the following features: Ki-67 over 20 per cent, perineural invasion, microvascular invasion, nodal metastases, or distant metastases.
Results
The study flow diagram is shown in Fig. 1. After initial screening, all the patients had at least positive 68Ga-labelled DOTA PET and/or a positive FNA(B) for NF-PanNEN.
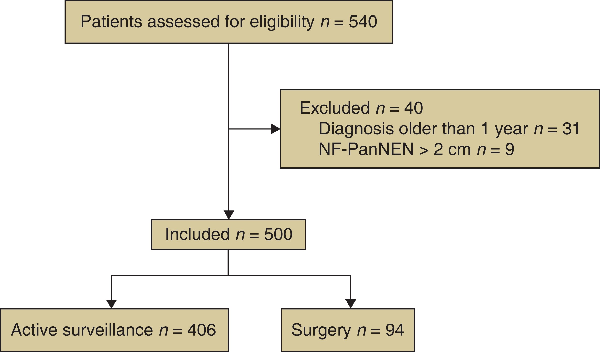
Fig. 1
Study flow chart
NF-PanNEN, non-functioning pancreatic neuroendocrine neoplasm.
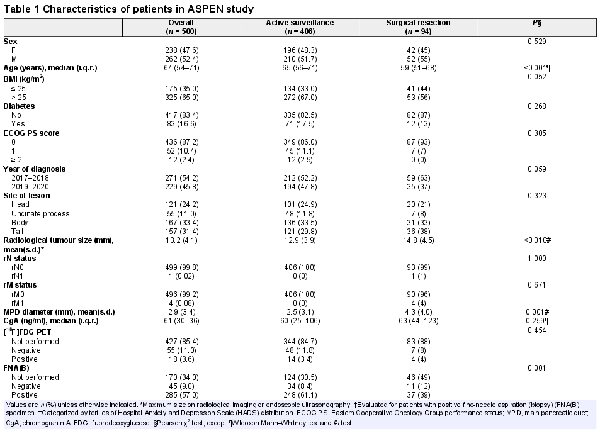
Table 1 summarizes demographics and clinical characteristics by the type of management. Younger age, larger tumour size, lower BMI, dilated main pancreatic duct (MPD), and enrolment of the patient in a surgical centre were associated more frequently with surgery. Global quality of life at diagnosis was similar in the two groups (Fig. S1). Overall, distant metastases were present in 4 patients (0.08 per cent), all of whom underwent surgery. On multivariable analysis, factors associated with surgery were: age 64 years or less (OR 2.5; P < 0.001), radiological size larger than 10 mm (OR 1.9; P = 0.030), MPD: over 3 mm (OR 3.4; P < 0.001), surgical centre (OR 2.0; P = 0.012), and Hospital Anxiety and Depression Scale—anxiety score above 3 and no more than 6 (OR 2.0; P = 0.029) (Table S1). Indication for surgery was attributed to patient’s preference in 42 instances (45 per cent), centre’s preference in 37 (39 per cent), MPD dilatation in 11 (12 per cent), and distant metastases in 4 (4 per cent).
Surgical outcomes are summarized in Table S2. Minimally invasive, either laparoscopic or robot-assisted, was the preferred approach in 55 per cent of patients. Severe complications (defined as those with a Clavien–Dindo grade of more than III) occurred in 13 per cent of patients whereas the mortality rate was zero. Final pathological examination characteristics are listed in Table S3. The choice of standard pancreatectomy over an atypical resection was justified by the need to perform an adequate lymphadenectomy in 52 patients (54 per cent) and the proximity of the nodule to the MPD in 23 (25 per cent). One or more aggressive histological features were observed in 19 patients (20 per cent). Of these 19 patients, 17 had a radiological tumour size larger than 10 mm. The remaining 2 patients with radiological tumour size less than 10 mm had a dilated MPD on preoperative imaging. In 5 of the 19 patients with aggressive features, the radiological MPD was larger than 3 mm.
After a median follow-up of 25 (i.q.r. 16–35) months, all patients were alive apart from 3 who died from causes unrelated to NF-PanNENs. Only 1 patient in the surgical group, who had liver metastases at diagnosis, eventually developed liver recurrence.
In the surveillance group, 9 patients (2 per cent) underwent surgery during follow-up. The reason for surgery was increasing tumour size in 4 patients, increased MPD dilatation in 3, and patient’s preference in 2.
Discussion
A non-operative strategy seems safe as only a negligible fraction of patients had an increase in tumour size and no patient developed distant metastases during follow-up. These results are consistent with the preliminary findings of a recent prospective study, although the present series included a five-fold larger number of patients and compared the two types of management of asymptomatic small NF-PanNENs, leaving the therapeutic decision (surveillance versus surgery) to the treating centres.
Other factors that contributed to the decision to resect a NF-PanNEN of 2 cm or smaller were younger age, tumour size over 1 cm, and the presence of MPD dilatation. Furthermore, patient’s preference was the main reason for choosing surgery in many instances. This attitude might be explained by patients’ anxiety and by the ongoing debate in the scientific community about the optimal management of these lesions. Moreover, the current guidelines suggest that surveillance is recommended, especially for older patients, and this may explain why young age was an important factor in deciding on a surgical approach more frequently. In the present experience, it was found that nearly 20 per cent of resected tumours had one or more aggressive features. Notably, nearly all the lesions that presented at least one aggressive feature were also larger than 1 cm.
The optimal cut-off for considering NF-PanNENs as low-risk lesions is a matter of ongoing controversy. The European Neuroendocrine Tumor Society and National Comprehensive Cancer Network guidelines consider observation for lesions no larger than 2 cm. On the other hand, North American Neuroendocrine Tumor Society guidelines suggest that the treatment of asymptomatic NF-PanNENs between 1 and 2 cm in size should be individualized. The present findings seem to support these latter recommendations. The presence of MPD dilatation should be promptly recognized and always considered as a major sign of concern because of the strong correlation with aggressive features, as described previously. Another possible role in predicting the biological behaviour of these small nodules may be played by novel promising biomarkers such as NETest. Finally, another important result was the detection of synchronous liver metastases in four patients, which demonstrates a real, although rare, potential for distant spread also among NF-PanNENs of 2 cm or smaller.
In conclusion, active surveillance is the preferred approach for sporadic, asymptomatic, NF-PanNENs no larger than 2 cm. An active surveillance strategy seems safe, but the measurable risk of distant metastases, as well as the presence of histological characteristics of aggressiveness in almost one-fifth of operated tumours, necessitates personalized management for lesions larger than 1 cm as well as for young patients and in the presence of measurable growth of the nodule. Moreover, surgery is always mandatory for small NF-PanNENs with a dilated MPD. According to the protocol, the study will be concluded 1 year after the enrolment of the last patient. Nevertheless, as these preliminary results showed only a very low rate of patients with tumour growth after a median follow-up of 2 years, longer follow-up is probably needed for definitive conclusions to be reached.
Acknowledgements
The authors thank F. di Salvo (Division of Pancreatic Surgery, Vita-Salute San Raffaele University, IRCCS Ospedale San Raffaele, Milan, Italy) for her contribution with acquisition and analysis of data; and the following people for their involvement in the acquisition of data: D. Horsch (Department of Gastroenterology/Endocrinology, Zentralklinik Bad Berka, Bad Berka, Germany), J. C. Percovich (Hospital Universitario Gregorio Maranon, Madrid, Spain), S. Jamdar (Manchester University NHS Foundation Trust, Manchester, UK), M. S. Khan (University Hospital of Wales, Cardiff and Vale University Health Board, Cardiff, UK), E. N. van Dijkum (Amsterdam Medical Centre, Amsterdam, the Netherlands), E. Martin Perez (University Hospital La Princesa, Madrid, Spain), and G. Donatini (Poitiers University Hospital, Poitiers, France).
References
- 1. Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y, et al Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol2017;3:1335–1342
- 2. Lee LC, Grant CS, Salomao DR, Fletcher JG, Takahashi N, Fidler JL, et al Small, nonfunctioning, asymptomatic pancreatic neuroendocrine tumors (PNETs): role for nonoperative management. Surgery2012;152:965–974
- 3. Sadot E, Reidy-Lagunes DL, Tang LH, Do RKG, Gonen M, D’Angelica MI, et al Observation versus resection for small asymptomatic pancreatic neuroendocrine tumors: a matched case–control study. Ann Surg Oncol2016;23:1361–1370
- 4. Barenboim A, Lahat G, Nachmany I, Nakache R, Goykhman Y, Geva R, et al Resection versus observation of small asymptomatic nonfunctioning pancreatic neuroendocrine tumors. J Gastrointest Surg2019;24:1366–1374
- 5. Partelli S, Cirocchi R, Crippa S, Cardinali L, Fendrich V, Bartsch DK, et al Systematic review of active surveillance versus surgical management of asymptomatic small non-functioning pancreatic neuroendocrine neoplasms. Br J Surg2017;104:34–41
- 6. Heidsma CM, Engelsman AF, Van Dieren S, Stommel MWJ, de Hingh I, Vriens M, et al Watchful waiting for small non-functional pancreatic neuroendocrine tumours: nationwide prospective cohort study (PANDORA). Br J Surg2021;108:888–891
- 7. Bettini R, Partelli S, Boninsegna L, Capelli P, Crippa S, Pederzoli P, et al Tumor size correlates with malignancy in nonfunctioning pancreatic endocrine tumor. Surgery2011;150:75–82
- 8. Partelli S, Bartsch DK, Capdevila J, Chen J, Knigge U, Niederle B, et al ENETS consensus guidelines for the standards of care in neuroendocrine tumours: surgery for small intestinal and pancreatic neuroendocrine tumours. Neuroendocrinology2017;105:255–265
- 9. Howe JR, Merchant NB, Conrad C, Keutgen XM, Hallet J, Drebin JA, et al The North American Neuroendocrine Tumor Society consensus paper on the surgical management of pancreatic neuroendocrine tumors. Pancreas2020;49:1–33
- 10. Shah MH, Goldner WS, Halfdanarson TR, Bergsland E, Berlin JD, Halperin D, et al NCCN guidelines insights: neuroendocrine and adrenal tumors, version 2.2018. J Natl Compr Canc Netw2018;16:693–702
- 11. Partelli S, Mazza M, Andreasi V, Muffatti F, Crippa S, Tamburrino D, et al Management of small asymptomatic nonfunctioning pancreatic neuroendocrine tumors: limitations to apply guidelines into real life. Surgery2019;166:157–163
- 12. Mintziras I, Keck T, Werner J, Fichtner-Feigl S, Wittel U, Senninger N, et al Implementation of current ENETS guidelines for surgery of small (≤ 2 cm) pancreatic neuroendocrine neoplasms in the German Surgical Community: an analysis of the prospective DGAV StuDoQ|Pancreas Registry. World J Surg2018;43:175–182
- 13. Chivukula SV, Tierney JF, Hertl M, Poirier J, Keutgen XM. Operative resection in early stage pancreatic neuroendocrine tumors in the United States: are we over- or undertreating patients?Surgery2020;167:180–186
- 14. Partelli S, Ramage JK, Massironi S, Zerbi A, Kim HB, Niccoli P, et al Management of asymptomatic sporadic nonfunctioning pancreatic neuroendocrine neoplasms (ASPEN) ≤ 2 cm: study protocol for a prospective observational study. Front Med2020;7:1–8
- 15. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg2004;240:205–213
- 16. Zhou B, Zhan C, Xiang J, Ding Y, Yan S. Clinical significance of the preoperative main pancreatic duct dilation and neutrophil-to-lymphocyte ratio in pancreatic neuroendocrine tumors (PNETs) of the head after curative resection. BMC Endocr Disord2019;19:123
- 17. Partelli S, Andreasi V, Muffatti F, Schiavo Lena M, Falconi M. Circulating neuroendocrine gene transcripts (NETest): a postoperative strategy for early identification of the efficacy of radical surgery for pancreatic neuroendocrine tumors. Ann Surg Oncol2020;27:3928–3936