Introduction
Extracorporeal shock wave therapy (ESWT) has been successfully used for over 20 years to manage a variety of orthopedic conditions.– A byproduct of extracorporeal shock wave lithotripsy (ESWL), ESWT has emerged as an acceptable and popular non-invasive management option for tendon and other pathologies of the musculoskeletal system. Prior studies on tendinopathy showed that ESWT can be as or more effective than other forms of treatment including eccentric exercise, traditional physiotherapy, steroid injections, injections of platelet-rich plasma and surgery.–
One of the primary reasons for the underuse of ESWT is a generalized unfamiliarity with the technique. Prior systematic reviews support the widely accepted notion that ESWT is safe, technically easy to perform and helpful in some conditions.,, That said, many of these reviews are dated and have also added to the already pre-existing confusion regarding terminology, protocols, energy levels and treatment parameters. The studies that form the basis of these reviews differ greatly in regards to design, protocol, application technique and length of follow-up. This heterogeneity makes it difficult for the practitioner to adopt a ‘best practice’ approach.
Yet there is no shortage in information. A search in PubMed on ‘shockwave OR shockwaves OR shock wave OR shock waves OR shock-wave OR shock-waves NOT urol* NOT stone NOT stones’ on May 17, 2015 yielded over 5000 citations. For this and the above-mentioned reasons, there remains a need for a concise summary of the evidence for the use of ESWT in clinical practice, as well as for developing a generally applicable ‘best practice’ protocol for ESWT.
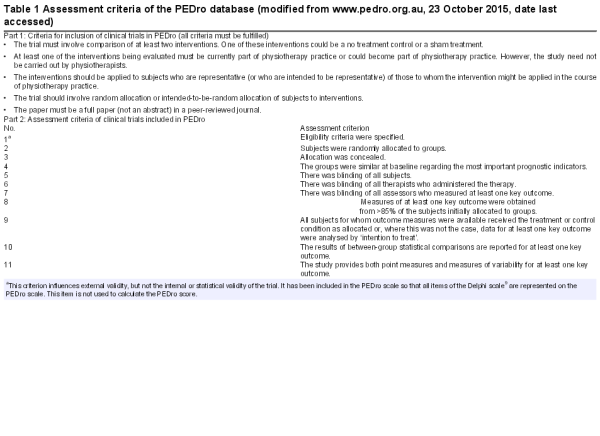
The PEDro database (www.pedro.org.au, 23 October 2015, date last accessed) is a freely available database of over 31 000 randomized controlled trials (RCTs), systematic reviews and clinical practice guidelines in physical and rehabilitation medicine. For each RCT, review or guideline, the PEDro database provides the citation details, the abstract and a link to the full text, where possible. All RCTs listed in the PEDro database (henceforth referred to as ‘RCTs in PEDro’) are independently assessed for quality (the assessment criteria are summarized in Table 1). All but two of the PEDro scale items are based on the Delphi list. PEDro is currently the largest independent database on topics related to physical and rehabilitation medicine and is often used by investigators in Norway, Australia and New Zealand; less so by other European and North American investigators.
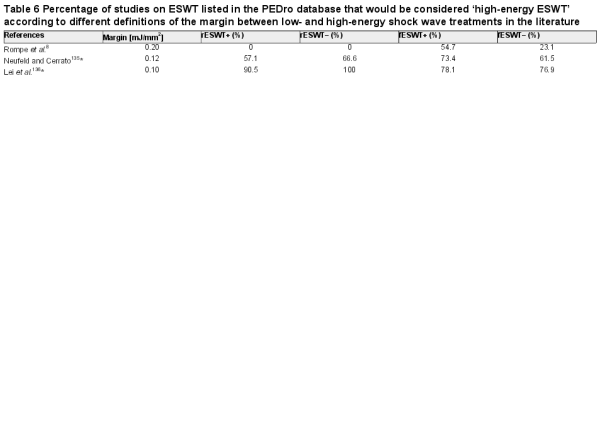
The present systematic review used data derived from the PEDro database according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to compare (i) ESWT with other non-operative treatment for tendon and other pathologies of the musculoskeletal system, (ii) radial ESWT with focused ESWT (see Figs. 1 and 2) and (iii) high-energy ESWT with low-energy ESWT.
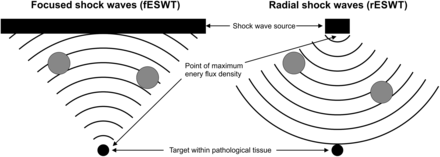
Fig. 1
Working principle of focused and radial extracorporeal shock wave technology. In case of focused shock waves, single acoustic pulses are generated either with a spark-gap (electrohydraulic principle), a technology similar to a loudspeaker (electromagnetic principle) or piezocrystals (piezoelectric principle) (details are provided in Fig. 2). By means of reflectors of certain shape, the acoustic pulses are converted into a focused acoustic pressure wave/shock wave with a point of highest pressure at the desired target within pathological tissue. In case of radial shock waves, a projectile is fired within a guiding tube that strikes a metal applicator placed on the skin. The projectile generates stress waves in the applicator that transmit pressure waves into tissue. It is of note that any disturbance in the pathway of the acoustic pulses between a focused shock wave source and the target within tissue (such as bone, calcifications, etc.; grey dots in the figures) may result in some parts of the acoustic pulse not reaching the target and, thus, weakening the shock wave energy (i.e. the energy flux density) at the target. The same disturbances would not impact the energy of radial shock waves at the target. This is most probably the reason why in muscle tissue, the energy of focused shock waves was found to be decreased by >50% compared with measurements in water, whereas for radial shock waves, measurements in muscle tissue and water were consistent.
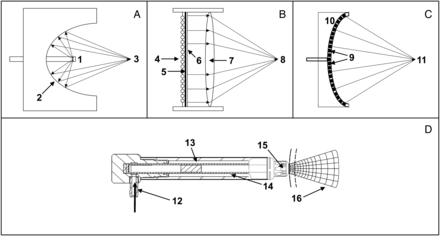
Fig. 2
Schematic representation of the mode of operation of focused (A–C) and radial (D) extracorporeal shock wave generators. (A) Electrohydraulic principle (fESWT): a high voltage discharges rapidly across two electrode tips (spark-gap) (1) that are positioned in water. The spark-gap serves as the first focal point (1). The heat generated by this process vaporizes the surrounding water. This generates a gas bubble centered on the first focal point, with the gas bubble being filled with water vapor and plasma. The result of the very rapid expansion of this bubble is a sonic pulse, and the subsequent implosion of this bubble causes a reverse pulse, manifesting a shock wave. By means of reflectors of certain shape (2), this shock wave can be converted into a convergent/focused acoustic pressure wave/shock wave with a point of highest pressure at the second focal point (3). (B) Electromagnetic principle (fESWT): a strong, variable magnetic field is generated by passing a high electric current through a coil (4). This causes a high current in an opposed metal membrane (5), which causes an adjacent membrane (6) with surrounding liquid to be forced rapidly away. Because the adjacent membrane is highly conductive, it is forced away so rapidly that the compression of the surrounding liquid generates a shock wave within the liquid. By means of an acoustic lens (7) of certain shape, this shock wave can be converted into a convergent/focused acoustic pressure wave/shock wave with a point of highest pressure at a focal point (8). (C) Piezoelectric principle (fESWT): a large number of piezocrystals (9) are mounted in a bowl-shaped device (10); the number of piezocrystals can vary from a few to several thousands (typically between 1000 and 2000). When applying a rapid electrical discharge, the piezocrystals react with a deformation (contraction and expansion), which is known as the piezoelectric effect. This induces an acoustic pressure puls in the surrounding water that can steep into a shock wave. Because of the design of the bowl-shaped device an acoustic pressure wave/shock wave can emerge with a point of highest pressure at a focal point (11). (D) Ballistic principle (rESWT): compressed air (pneumatic principle; 12) or a magnetic field (not shown) is used to fire a projectile (13) within a guiding tube (14) that strikes a metal applicator (15) placed on the patient's skin. The projectile generates stress waves in the applicator that transmit pressure waves into tissue (16).
Materials and methods
An evidence-based systematic review of literature was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to examine efficacy and safety of ESWT for orthopedic conditions.
Data source
The PEDro database (www.pedro.org.au, 23 October 2015, date last accessed) was searched from its date of inception to May 17, 2015 to find potentially relevant publications.
Study selection
A first search addressed the key terms shock wave, shock waves, shockwave, shockwaves, lithotrypsy and lithotrypter. Based on the outcome of the first search (as outlined in detail in the next paragraph), a second search was performed on the key terms plantar, Achilles, epicondylitis, subacromial, non-calcific and calcifying.
Data extraction
The outcome of the first search is shown in Figure 3. We identified n = 209 records in the PEDro database of which n = 47 were duplicates. All reviews (n = 48) were excluded, as well as records that did not address ESWT (n = 3).– Furthermore, all ESWT studies on wound healing and chronic decubitus were excluded (n = 5).– The remaining records (n = 106) were divided into studies on (i) radial ESWT with positive outcome (i.e. radial ESWT significantly better statistically than either placebo or alternative treatment modalities) (rESWT+; n = 23), (ii) radial ESWT with negative outcome (i.e. radial ESWT not significantly better statistically than either placebo or alternative treatment modalities) (rESWT−; n = 3), (iii) focused ESWT with positive outcome (fESWT+; n = 66) and (iv) focused ESWT with negative outcome (fESWT−; n = 15) (note that one RCT addressed both radial and focused ESWT and, thus, was listed in both groups rESWT+ and fESWT+).

Fig. 3
Systematic review flow chart of the first literature search according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. *, one study addressed both radial and focused ESWT and, thus, was listed in both categories rESWT+ and fESWT+.
For each of these groups (i.e. rESWT+, rESWT−, fESWT+ and fESWT−), mean and standard error of the mean (SEM) of the following variables were calculated: (i) number of treatment sessions; (ii) interval between treatment sessions for those RCTs with more than one treatment session; (iii) number of impulses per treatment session; (iv) energy flux density (EFD) of the impulses; (v) total EFD that was applied (calculated as the product of the number of treatment sessions, the number of impulses per treatment session and the EFD of the impulses) and (vi) PEDro score (between 0 and 10). Comparison of groups was performed using Kruskal–Wallis test (non-parametric analysis of variance) followed by pairwise comparisons using Dunn's multiple comparison test. Many RCTs in PEDro did not specify whether the reported EFD was the positive EFD (EFD+) or the total EFD (EFDtotal) (details about EFD+ and EFDtotal are provided in Refs.,). Accordingly, calculations of mean EFDs were based on mixed EFD+ and EFDtotal data.
Furthermore, absolute and relative numbers of studies performed with, respectively, electrohydraulic, electromagnetic or piezoelectric shock wave generators were calculated. This was done separately for the groups fESWT+ and fESWT−. Comparison of groups was performed using χ2 test.
All calculations were performed with GraphPad Prism (version 5.00 for Windows; GraphPad Software, San Diego, CA, USA). A P-value of <0.05 was considered statistically significant.
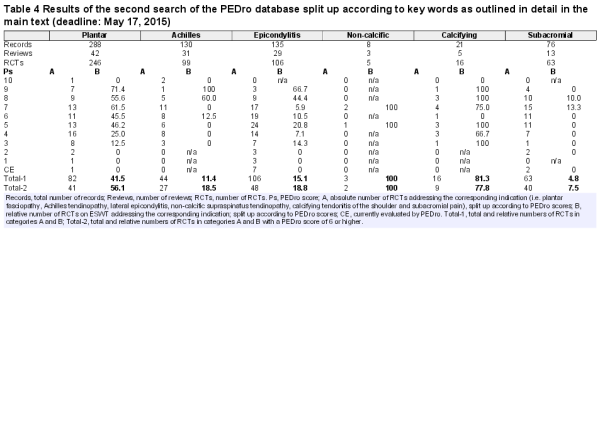
Finally, we investigated which orthopedic conditions were repeatedly (i.e. more than two times) addressed in the retrieved RCTs on ESWT in PEDro. This was the case for the indications plantar fasciopathy, Achilles tendinopathy, lateral epicondylitis, subacromial pain syndrome, non-calcific supraspinatus tendinopathy and calcifying tendonitis of the shoulder. On this basis, a second search in the PEDro database was performed. For each of the key terms plantar, Achilles, epicondylitis, subacromial, non-calcific and calcifying, we calculated (i) the total number of records, the number of reviews and the number of RCTs in PEDro, (ii) the number of RCTs in PEDro that addressed the corresponding condition and (iii) the number of RCTs on ESWT in PEDro for the corresponding condition. Full-text articles were not assessed for eligibility during the second search.
Results
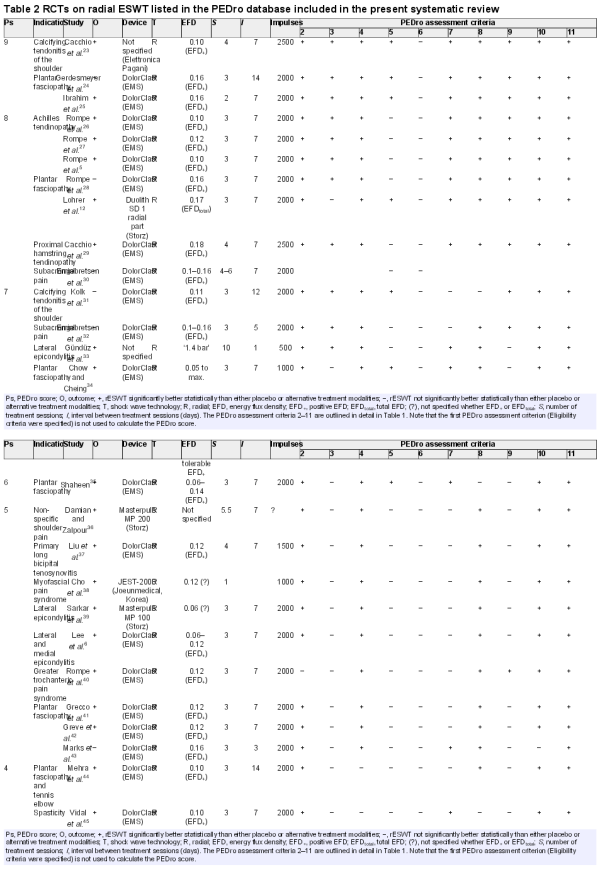
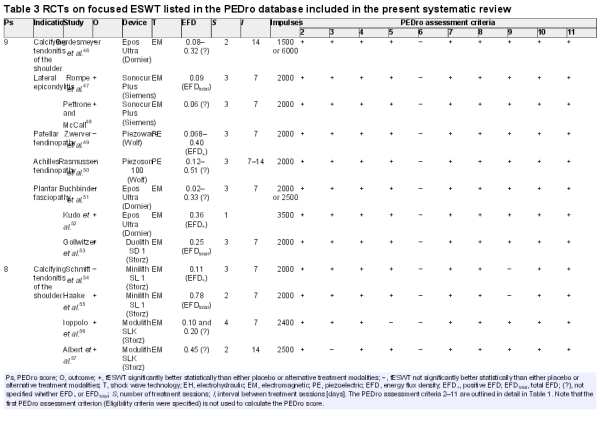
All studies included in the qualitative synthesis of the first literature search are listed in Tables 2 and 3. The average number of treatment sessions among all RCTs on ESWT in PEDro was 2.88 ± 0.15 (mean ± SEM; range: 1–12), with highest numbers in RCTs on rESWT+ and lowest numbers in RCTs on fESWT+ (Fig. 4A). The difference in the mean number of treatment sessions between these two groups was statistically significant (P < 0.01).

Fig. 4
Mean and standard error of the mean (SEM) of the number of treatment sessions (A), interval between treatment sessions (B), number of impulses per treatment session (C), energy flux density of the impulses (D), total energy flux density that was applied (E) and the PEDro score of all RCTs on radial (rESWT) and focused (fESWT) extracorporeal shock wave therapy with positive (+) or negative (−) outcome listed in the PEDro database (deadline: May 17, 2015). Details are provided in the main text.
Among those RCTs on ESWT in PEDro with more than one treatment session, the average interval between treatment sessions was 9.13 ± 0.66 days (range: 1–42 days). On average, the longest intervals between treatment sessions were reported for Group fESWT− and the shortest intervals for Group rESWT−. However, there were no statistically significant (P < 0.05) differences between the groups (Fig. 4B).
The average number of impulses per treatment session among all RCTs on ESWT in PEDro varied only slightly among the groups rESWT+, rESWT−, fESWT+ and fESWT−, with a mean value of 2029 ± 96 (range: 250–6000). There were no statistically significant (P < 0.05) differences between the groups (Fig. 4C).
The EFD of the impulses applied in all RCTs on ESWT in PEDro was on average 0.19 ± 0.01 mJ/mm2 (range: 0.03–0.78), with the highest mean value in Group fESWT+ and the lowest mean value in Group rESWT+ (Fig. 4D). The difference in the mean EFD between these two groups was statistically significant (P < 0.01). However, one cannot exclude that this resulted from the fact that for many RCTs in Groups fESWT+ and fESWT−, it remained unclear whether the reported EFD was EFD+ or EFDtotal (which is higher than EFD+; c.f. Refs.,). In contrast, for most studies in Groups rESWT+ and rESWT−, it was known that the reported EFD was EFD+.
Among all RCTs on ESWT in PEDro, the average total EFD applied (calculated as the product of the number of treatment sessions, the number of impulses per treatment session and the EFD of the impulses) was 0.99 ± 0.08 J/mm2 (range: 0.01–3.72 J/mm2), with the highest mean value in Group fESWT+ and the lowest mean value in Group rESWT+. However, there were no statistically significant (P < 0.05) differences between the groups (Fig. 4E).
The average PEDro score among all RCTs on ESWT in PEDro was 6.33 ± 0.17 (range: 1–9), with the highest mean score in Group fESWT− and the lowest mean score in Group fESWT+ (Fig. 4F). The difference in the mean PEDro score between these two groups was statistically significant (P < 0.01).
Furthermore, in 17 RCTs on fESWT with positive outcome in PEDro, an electrohydraulic (EH) device was used, in 42 RCTs an electromagnetic (EM) device and in 6 RCTs a piezoelectric (PE) device (in 1 RCT both EH and EM device were used). For the RCTs on fESWT with negative outcome in PEDro, the corresponding numbers were 1 (EH), 13 (EM) and 2 (PE) (1 study with both EH and EM devices). The distribution of numbers of EH, EM and PE devices was not statistically significant (P = 0.229) between RCTs on fESWT with positive outcome and RCTs on fESWT with negative outcome.
The results of the second search are summarized in Table 4. For the key word plantar, 82 out of 288 records (28.5%) in the PEDro database were RCTs on plantar fasciopathy, of which 41 (41/82 = 50%) had a PEDro score of 6 or higher. For the other key words, the corresponding numbers were as follows: Achilles: 44/130 = 33.8% RCTs on Achilles tendinopathy, among them 27/44 = 61.4% with PEDro score ≥6. Epicondylitis: 106/106 = 100% RCTs on lateral epicondylitis, among them 48/106 = 45.3% with PEDro score ≥6. Non-calcific: 3/8 = 37.5% RCTS on non-calcific supraspinatus tendinopathy, among them 2/3 = 66.6% with PEDro score ≥6. Calcifying: 16/21 = 76.2% RCTs on calcifying tendonitis of the shoulder, among them 9/16 = 56.3% with PEDro score ≥6. Subacromial: 63/76 = 82.9% RCTS on subacromial pain syndrome, among them 40/63 = 63.5% with PEDro score ≥6.
For plantar fasciopathy, 41.5% of the RCTs listed in the PEDro database were RCTs on ESWT (56.1% of the RCTs with PEDro score ≥6). For other indications, the corresponding relative numbers of RCTs on ESWT were as follows: Achilles tendinopathy: 11.4% of all RCTs, and 18.5% of those RCTs with PEDro score ≥6. Lateral epicondylitis: 15.1% of all RCTs, and 18.8% of those RCTs with PEDro score ≥6. Non-calcific supraspinatus tendinopathy: 100% of all RCTs. Calcifying tendonitis of the shoulder: 81.3% of all RCTs, and 77.8% of those RCTs with PEDro score ≥6. Subacromial pain syndrome: 4.8% of all RCTs, and 7.5% of those RCTs with PEDro score ≥6.
Discussion
Methodological considerations
Prior systematic reviews attempted to assimilate the raw data from hundreds of studies investigating ESWT so as to draw meaningful conclusions. Unfortunately, many of these reviews, by not defining terminology, and by not drawing a distinction between the various types of ESWT have at times added to the confusion. Concepts such as radial ESWT, focused ESWT, low-energy ESWT and high-energy ESWT have clinical, practical and economic implications and therefore need explanation by reviewers.
The reliability of the PEDro scale for rating the quality of RCTs was demonstrated and subsequently confirmed independently. Using RCTs derived only from the PEDro database, we sought to (i) clarify some common misconceptions regarding ESWT and (ii) for specific indications, compare ESWT with other forms of non-operative treatment.
A meta-analysis is often very helpful when the efficacy of an intervention is not known. The preponderance of the RCTs derived from our search of the PEDro database demonstrated that ESWT is better than placebo, no treatment or an alternative treatment (>80% of all studies on ESWT in PEDro). However, there are substantial differences among RCTs on ESWT listed in PEDro with regard to clinical condition, study design, ESWT technology and device, treatment protocol and follow-up period. Therefore, we felt a clinical review would be the more appropriate format for our purposes.
We have derived 10 main statements about ESWT based on the RCTs on rESWT and fESWT in PEDro (Table 5). Each statement is briefly substantiated by scientific evidence developed in the present systematic review. References to studies not listed in PEDro were kept at the absolute minimum and marked by an asterisk.
ESWT is effective
The efficacy of ESWT is clearly supported by the cumulative data. 88.5% (23 out of 26) of all RCTs on rESWT and 81.5% (66 out of 81) of all RCTs on fESWT in PEDro had positive outcome (i.e. rESWT or fESWT significantly better statistically than either placebo or alternative treatment modalities).
ESWT is safe
The safety of ESWT was also clearly supported by the cumulative data. There were no reports of serious adverse events in any of the studies included in this analysis.
For certain orthopedic conditions, RCTs on ESWT were the predominant type of RCT listed in the PEDro database and/or obtained the highest PEDro scores among all investigated treatment modalities
Both criteria (i.e. predominant type of RCT in PEDro, and highest PEDro scores among all investigated treatment modalities) were fulfilled for the indications plantar fasciopathy, non-calcific supraspinatus tendinopathy and calcifying tendonitis of the shoulder (Table 4). For Achilles tendinopathy and lateral epicondylitis, respectively, 11.4 and 15.1% of all RCTs in PEDro were RCTs on ESWT, but these RCTs also obtained among the highest PEDro scores among all investigated treatment modalities for these conditions.
For other indications (greater trochanteric pain syndrome, patellar tendinopathy, knee osteoarthritis, long bone fracture, osteonecrosis of the femoral head, proximal hamstring tendinopathy, primary long bicipital tenosynovitis, myofascial pain syndrome, myogelosis of the masseter muscle and spasticity), there are not enough RCTs on rESWT and fESWT in PEDro to draw meaningful conclusions regarding the significance of ESWT for the corresponding conditions.
There was no difference in the ‘quality’ of RCTs on ESWT in PEDro with positive or negative outcome
RCTs on ESWT with either positive or negative outcome had almost the same averaged PEDro scores. This finding contradicts the belief that ‘better’ RCTs (i.e. RCTs with a higher PEDro score) generally demonstrate that ESWT is not effective.
Application of local anesthesia adversely affects outcome of ESWT
Two studies*,* demonstrated that application of local anesthesia in the area of treatment (as done in Refs.,) adversely affects outcome of ESWT. The molecular mechanisms underlying this phenomenon are not yet fully understood, but substantial evidence points to a central role of the peripheral nervous system in mediating molecular and cellular effects of shock waves applied to the musculoskeletal system.*–* These effects could be blocked by local anesthesia.* Thus, it is now generally recommended to apply shock waves without local anesthesia to the musculoskeletal system.
Application of insufficient energy adversely affects outcome of ESWT
The averaged EFD applied in all RCTs on rESWT and fESWT for calcifying tendonitis of the shoulder with positive outcome in PEDro (‘averaged EFD’) was 0.28 ± 0.04 mJ/mm2. This was ∼2.6 times more than the EFD applied in a negative RCT on rESWT for this indication (EFD = 0.11 mJ/mm2). A similar situation was found for treating plantar fasciopathy. Here, the averaged EFD was 0.19 ± 0.02 mJ/mm2, which was more than two times the EFD applied in a negative RCT on fESWT as well as in another negative RCT on fESWT (0.08 mJ/mm2). Regarding Achilles tendinopathy, averaged EFD was equal to 0.17 ± 0.04 mJ/mm2 in RCTs on ESWT with positive outcome in PEDro, compared with EFD = 0.06 mJ/mm2 applied in an RCT on fESWT with negative outcome.
There is no scientific evidence in favor of either rESWT or fESWT with respect to treatment outcome
‘Which is better, rESWT or fESWT?’ A review of the PEDro database demonstrated no scientific evidence in favor of either rESWT or fESWT with respect to treatment outcome. There are very few studies comparing the two techniques. In one such study, better results were reported with fESWT than with rESWT for treating patients with plantar fasciopathy (EFD was higher in fEWST than in rESWT in this study). However, using the same rESWT and fESWT devices than in Ref. and the same EFD in fESWT and rESWT, other authors found no difference in effectiveness between rESWT and fESWT for patients with patellar tendinopathy.*
The distinction between radial ESWT as ‘low-energy ESWT’ and focused ESWT as ‘high-energy ESWT’ is not correct and should be abandoned
Rompe et al. arbitrarily defined an EFD of 0.2 mJ/mm2 as the margin between low- and high-energy shock wave treatments. Following this definition, 100% of the RCTs on rESWT, ∼45% of the fESWT+ RCTs and ∼77% of the fESWT− RCTs in PEDro were performed with low-energy shock waves (c.f. Tables 2 and 3). However, other definitions of the margin between low- and high-energy shock wave treatments were published*,* (Table 6). Accordingly, it is not correct to characterize rESWT as low-energy shock wave treatment and fESWT as high-energy shock wave treatment, as different authors have used different thresholds for this distinction. Because there is no consensus in the literature about the difference between low- and high-energy ESWT, this distinction appears arbitrary and should be abandoned.
There is no scientific evidence that a certain fESWT technology is superior to other technologies
Focused shock waves can be produced by electrohydraulic, electromagnetic and piezoelectric shock wave generators. In 2001, Ogden et al. in an early review of ESWT technology stated that ‘the electrohydraulic method … has been shown to be superior to other generation methods (electromagnetic, piezoelectric)’. These authors used literature derived from urology (i.e. from ESWL) to substantiate this claim. However, we found no statistically significant (P < 0.05) difference in the distribution of numbers of RCTs on fESWT in PEDro using electrohydraulic, electromagnetic and piezoelectric shock wave generators among studies with positive outcome and studies with negative outcome. Hence, the RCTs on fESWT in PEDro do not indicate an advantage of a certain fESWT technology over other technologies.
An optimum treatment protocol for ESWT appears to be three treatment sessions at 1-week intervals, with 2000 impulses per session and the highest EFD that can be applied
This recommendation is based on the quantitative analysis shown in Figure 4 and reflects the average number of treatment sessions and the average interval between treatment sessions among all RCTs on ESWT in PEDro. With respect to the EFD of the impulses (to be as high as possible, i.e. what can be tolerated by the individual patient without application of local anesthesia), this recommendation is based on findings of one study on rESWT for plantar fasciopathy with positive outcome and another study on fESWT for calcifying tendonitis of the shoulder with positive outcome that ‘more is better’. There is not a single RCT on ESWT in PEDro, contradicting this ‘more is better’ recommendation.
Limitations
There are three main limitations inherent to the present systematic review on ESWT. First, with few exceptions, only RCTs on ESWT in PEDro were considered. This approach was adopted to minimize selection bias by using the selection process and criteria of an independent third party that has never been involved in planning, performing and funding any study on ESWT, and to rely on the proven reliability of the PEDro scale for rating the quality of RCTs. Accordingly, all analyses, interpretations and conclusions of the present study are only valid for those RCTs on ESWT in PEDro.
Second, no meta-analysis was performed. This was because of the substantial differences among RCTs on ESWT in PEDro with regard to clinical condition, study design, ESWT technology and device, treatment protocol and follow-up period.
Third, because of the first and second limitations, all conclusions of the present study are only valid for those shock wave generators that were used in the RCTs on ESWT in PEDro (Tables 2 and 3). This is particularly important considering the substantial variability in treatment success and rates of unwanted side effects found when treating the same clinical condition (lateral epicondylitis) with different electromagnetic and piezoelectric fESWT devices operated at comparable energy settings.,
Conclusion
ESWT has been proven as effective and safe non-invasive treatment option for tendon and other pathologies of the musculoskeletal system in a multitude of high-quality RCTs. For plantar fasciopathy, non-calcific tendinopathy of the supraspinatus tendon and calcifying tendonitis of the shoulder RCTs on ESWT are the predominant type of RCT in PEDro and obtained the highest PEDro scores among all investigated treatment modalities for these conditions. The latter criterion was also achieved for Achilles tendinopathy and lateral epicondylitis, albeit in a smaller number of RCTs. Therefore, ESWT should be considered by medical doctors, therapists, patients and payers when discussing treatment options for certain musculoskeletal pathologies. Future RCTs on ESWT should primarily address systematic tests of the optimum treatment protocol identified in this systematic review (three treatment sessions at 1-week intervals, with 2000 impulses per session and the highest EFD that can be applied) and direct comparisons between radial and focused ESWT.
Conflict of interest statement
N.B.M.C., S.M., M.S., J.-D.R. and J.P.F. declare that no competing financial interests exist. C.S. serves as a paid consultant for and receives benefits from Electro Medical Systems (Nyon, Switzerland), the manufacturer and distributor of the Swiss DolorClast radial shock wave device. However, C.S. has not received any honoraria or consultancy fee in writing this manuscript. No other potential conflicts of interest relevant to this article were reported.
References
- 1. Schmitz C, Császár NB, Rompe JD, et al.. Treatment of chronic plantar fasciopathy with extracorporeal shock waves (review). J Orthop Surg Res 2013;8:31–41.
- 2. Ioppolo F, Rompe JD, Furia JP, et al.. Clinical application of shock wave therapy (SWT) in musculoskeletal disorders. Eur J Phys Rehabil Med 2014;50:217–30.
- 3. Speed C. A systematic review of shockwave therapies in soft tissue conditions: focusing on the evidence. Br J Sports Med 2014;48:1538–42.
- 4. Cacchio A, Giordano L, Colafarina O, et al.. Extracorporeal shock-wave therapy compared with surgery for hypertrophic long-bone nonunions. J Bone Joint Surg Am 2009;91:2589–97.
- 5. Rompe JD, Furia JP, Maffulli N. Eccentric loading versus eccentric loading plus shock-wave treatment for midportion Achilles tendinopathy: a randomized controlled trial. Am J Sports Med 2009;37:463–70.
- 6. Lee SS, Kang S, Park NK, et al.. Effectiveness of initial extracorporeal shock wave therapy on the newly diagnosed lateral or medial epicondylitis. Ann Rehabil Med 2012;36:681–7.
- 7. Vetrano M, Castorina A, Vulpiani MC, et al.. Platelet-rich plasma versus focused shock waves in the treatment of jumper's knee in athletes. Am J Sports Med 2013;41:795–803.
- 8. Rompe JD, Furia J, Weil L, et al.. Shock wave therapy for chronic plantar fasciopathy. Brit Med Bul 2007;81 and 82:183–208.
- 9. Verhagen AP, de Vet HC, de Bie RA, et al.. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol 1998;51:1235–41.
- 10. Liberati A, Altman DG, Tetzlaff J, et al.. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Br Med J 2009;339:b2700.
- 11. Kearney CJ, Prevost T, Socrate S, et al.. Pressure-time profiles of a focused and a radial shockwave device: measurements in tissue, ex vivo, and in a water bath. J Acoust Soc Am 2010;128:2364.
- 12. Lohrer H, Nauck T, Dorn-Lange NV, et al.. Comparison of radial versus focused extracorporeal shock waves in plantar fasciitis using functional measures. Foot Ankle Int 2010;31:1–9.
- 13. Grabow L. Controlled study of the analgetic effectivity of acupuncture. Arzneimittel-Forschung [Drug Research] 1994;44:554–8.
- 14. Milgrom C, Finestone A, Lubovsky O, et al.. A controlled randomized study of the effect of training with orthoses on the incidence of weight bearing induced back pain among infantry recruits. Spine 2005;30:272–5.
- 15. al-Bluwi MT, Sadat-Ali M, al-Habdan IM, et al.. Efficacy of EZStep in the management of plantar fasciitis: a prospective, randomized study. Foot Ankle Special 2011;4:218–21.
- 16. Dumfarth J, Zimpfer D, Vögele-Kadletz M, et al.. Prophylactic low-energy shock wave therapy improves wound healing after vein harvesting for coronary artery bypass graft surgery: a prospective, randomized trial. Ann Thorac Surg 2008;86:1909–13.
- 17. Larking AM, Duport S, Clinton M, et al.. Randomized control of extracorporeal shock wave therapy versus placebo for chronic decubitus ulceration. Clin Rehabil 2010;24:222–9.
- 18. Ottomann C, Hartmann B, Tyler J, et al.. Prospective randomized trial of accelerated re-epithelization of skin graft donor sites using extracorporeal shock wave therapy. J Am Coll Surg 2010;211:361–7.
- 19. Wang CJ, Wu RW, Yang YJ. Treatment of diabetic foot ulcers: a comparative study of extracorporeal shockwave therapy and hyperbaric oxygen therapy. Diabetes Res Clin Pract 2011;92:187–93.
- 20. Ottomann C, Stojadinovic A, Lavin P, et al.. Prospective randomized phase II Trial of accelerated reepithelialization of superficial second-degree burn wounds using extracorporeal shock wave therapy. Ann Surg 2012;255:23–9.
- 21. Gerdesmeyer L, Maier M, Haake M, et al.. Physikalisch-technische Grundlagen der extrakorporalen Stosswellentherapie (ESWT). [Physical-technical principles of extracorporeal shockwave therapy (ESWT)] [Article in German]. Orthopäde 2002;31:610–7.
- 22. Ogden JA, Tóth-Kischkat A, Schultheiss R. Principles of shock wave therapy. Clin Orthop Relat Res 2001;387:8–17.
- 23. Cacchio A, Paoloni M, Barile A, et al.. Effectiveness of radial shock-wave therapy for calcific tendinitis of the shoulder: single-blind, randomized clinical study. Phys Ther 2006;86:672–82.
- 24. Gerdesmeyer L, Frey C, Vester J, et al.. Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled multicenter study. Am J Sports Med 2008;36:2100–9.
- 25. Ibrahim MI, Donatelli RA, Schmitz C, et al.. Chronic plantar fasciitis treated with two sessions of radial extracorporeal shock wave therapy. Foot Ankle Int 2010;31:391–7.
- 26. Rompe JD, Nafe B, Furia JP, et al.. Eccentric loading, shock-wave treatment, or a wait-and-see policy for tendinopathy of the main body of tendo Achillis: a randomized controlled trial. Am J Sports Med 2007;35:374–83.
- 27. Rompe JD, Furia JP, Maffulli N. Eccentric loading compared with shock wave treatment for chronic insertional Achilles tendinopathy. A randomized, controlled trial. J Bone Joint Surg Am 2008;90:52–61.
- 28. Rompe JD, Cacchio A, Weil L Jr, et al.. Plantar fascia-specific stretching versus radial shock-wave therapy as initial treatment of plantar fasciopathy. J Bone Joint Surg Am 2010;92:2514–22.
- 29. Cacchio A, Rompe JD, Furia JP, et al.. Shockwave therapy for the treatment of chronic proximal hamstring tendinopathy in professional athletes. Am J Sports Med 2011;39:146–53.
- 30. Engebretsen K, Grotle M, Bautz-Holter E, et al.. Radial extracorporeal shockwave treatment compared with supervised exercises in patients with subacromial pain syndrome: single blind randomised study. Br Med J 2009;339:b3360.
- 31. Kolk A, Yang KG, Tamminga R, et al.. Radial extracorporeal shock-wave therapy in patients with chronic rotator cuff tendinitis: a prospective randomised double-blind placebo-controlled multicentre trial. Bone Joint J 2013;95-B:1521–6.
- 32. Engebretsen K, Grotle M, Bautz-Holter E, et al.. Supervised exercises compared with radial extracorporeal shock-wave therapy for subacromial shoulder pain: 1-year results of a single-blind randomized controlled trial. Phys Ther 2011;91:37–47.
- 33. Gündüz R, Malas FÜ, Borman P, et al.. Physical therapy, corticosteroid injection, and extracorporeal shock wave treatment in lateral epicondylitis. Clinical and ultrasonographical comparison. Clin Rheumatol 2012;31:807–12.
- 34. Chow IHW, Cheing GLY. Comparison of different energy densities of extracorporeal shock wave therapy (ESWT) for the management of chronic heel pain. Clin Rehabil 2007;21:131–41.
- 35. Shaheen AAM. Comparison of three different treatment protocols of low-energy radial extracorporeal shock wave therapy for management of chronic plantar fasciitis. Ind J Physiother Occup Ther 2010;4:8–12.
- 36. Damian M, Zalpour C. Trigger point treatment with radial shock waves in musicians with nonspecific shoulder-neck pain: data from a special physio outpatient clinic for musicians. Med Probl Perform Art 2011;26:211–7.
- 37. Liu S, Zhai L, Shi Z, et al.. Radial extracorporeal pressure pulse therapy for the primary long bicipital tenosynovitis a prospective randomized controlled study. Ultrasound Med Biol 2012;38:727–35.
- 38. Cho YS, Park SJ, Jang SH, et al.. Effects of the combined treatment of extracorporeal shock wave therapy (ESWT) and stabilization exercises on pain and functions of patients with myofascial pain syndrome. J Physical Ther Sci 2012;24:1319–23.
- 39. Sarkar B, Das PG, Equebal A, et al.. Efficacy of low-energy extracorporeal shockwave therapy and a supervised clinical exercise protocol for the treatment of chronic lateral epicondylitis: a randomised controlled study. Hong Kong Physiother J 2013;31:19–24.
- 40. Rompe JD, Segal NA, Cacchio A, et al.. Home training, local corticosteroid injection, or radial shock wave therapy for greater trochanter pain syndrome. Am J Sports Med 2009;37:1981–90.
- 41. Grecco MV, Brech GC, Greve JM. One-year treatment follow-up of plantar fasciitis: radial shockwaves vs. conventional physiotherapy. Clinics 2013;68:1089–95.
- 42. Greve JM, Grecco MV, Santos-Silva PR. Comparison of radial shockwaves and conventional physiotherapy for treating plantar fasciitis. Clinics 2009;64:97–103.
- 43. Marks W, Jackiewicz A, Witkowski Z, et al.. Extracorporeal shock-wave therapy (ESWT) with a new-generation pneumatic device in the treatment of heel pain. A double blind randomised controlled trial. Acta Orthop Belg 2008;74:98–101.
- 44. Mehra A, Zaman T, Jenkin AI. The use of a mobile lithotripter in the treatment of tennis elbow and plantar fasciitis. Surgeon 2003;1:290–2.
- 45. Vidal X, Morral A, Costa L, et al.. Radial extracorporeal shock wave therapy (rESWT) in the treatment of spasticity in cerebral palsy: a randomized, placebo-controlled clinical trial. NeuroRehabilitation 2011;29:413–9.
- 46. Gerdesmeyer L, Wagenpfeil S, Haake M, et al.. Extracorporeal shock wave therapy for the treatment of chronic calcifying tendonitis of the rotator cuff: a randomized controlled trial. JAMA 2003;290:2573–80.
- 47. Rompe JD, Decking J, Schoellner C, et al.. Repetitive low-energy shock wave treatment for chronic lateral epicondylitis in tennis players. Am J Sports Med 2004;32:734–43.
- 48. Pettrone FA, McCall BR. Extracorporeal shock wave therapy without local anesthesia for chronic lateral epicondylitis. J Bone Joint Surg Am 2005;87:1297–304.
- 49. Zwerver J, Hartgens F, Verhagen E, et al.. No effect of extracorporeal shockwave therapy on patellar tendinopathy in jumping athletes during the competitive season: a randomized clinical trial. Am J Sports Med 2011;39:1191–9.
- 50. Rasmussen S, Christensen M, Mathiesen I, et al.. Shockwave therapy for chronic Achilles tendinopathy: a double-blind, randomized clinical trial of efficacy. Acta Orthopaedica 2008;79:249–56.
- 51. Buchbinder R, Ptasznik R, Gordon J, et al.. Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: a randomized controlled trial. J Am Med Assoc 2002;288:1364–72.
- 52. Kudo P, Dainty K, Clarfield M, et al.. Randomized, placebo-controlled, double-blind clinical trial evaluating the treatment of plantar fasciitis with an extracoporeal shockwave therapy (ESWT) device: a North American confirmatory study. J Orthop Res 2006;24:115–23.
- 53. Gollwitzer H, Diehl P, von Korff A, et al.. Extracorporeal shock wave therapy for chronic painful heel syndrome: a prospective, double blind, randomized trial assessing the efficacy of a new electromagnetic shock wave device. J Foot Ankle Surg 2007;46:348–57.
- 54. Schmitt J, Haake M, Tosch A, et al.. Low-energy extracorporeal shock-wave treatment (ESWT) for tendinitis of the supraspinatus. A prospective, randomised study. J Bone Joint Surg Br 2001;83–B:873–6.
- 55. Haake M, Deike B, Thon A, et al.. Exact focusing of extracorporeal shock wave therapy for calcifying tendinopathy. Clin Orthop Relat Res 2002;397:323–31.
- 56. Ioppolo F, Tattoli M, Di Sante L, et al.. Extracorporeal shock-wave therapy for supraspinatus calcifying tendinitis: a randomized clinical trial comparing two different energy levels. Phys Ther 2012;92:1376–85.
- 57. Albert JD, Meadeb J, Guggenbuhl P, et al.. High-energy extracorporeal shock-wave therapy for calcifying tendinitis of the rotator cuff: a randomised trial. J Bone Joint Surg Br 2007;89:335–41.
- 58. Speed CA, Nichols D, Richards C, et al.. Extracorporeal shock wave therapy for lateral epicondylitis – a double blind randomised controlled trial. J Orthop Res 2002;20:895–8.
- 59. Staples MP, Forbes A, Ptasznik R, et al.. A randomized controlled trial of extracorporeal shock wave therapy for lateral epicondylitis (tennis elbow). J Rheumatol 2008;35:2038–46.
- 60. Haake M, Konig IR, Decker T, et al.. Extracorporeal shock wave therapy in the treatment of lateral epicondylitis: a randomized multicenter trial. J Bone Joint Surg Am 2002;84-A:1982–91.
- 61. Chung B, Wiley JP. Effectiveness of extracorporeal shock wave therapy in the treatment of previously untreated lateral epicondylitis: a randomized controlled trial. Am J Sports Med 2004;32:1660–7.
- 62. Buch M, Knorr U, Fleming L, et al.. Extracorporeal shock wave therapy in plantar fasciitis: a review. Orthopaede 2002;31:637–44.
- 63. Haake M, Buch M, Schoellner C, et al.. Extracorporeal shock wave therapy for plantar fasciitis: randomised controlled multicentre trial. Br Med J 2003;327:75–9.
- 64. Speed CA, Nichols D, Wies J, et al.. Extracorporeal shock wave therapy for plantar fasciitis. A double blind randomised controlled trial. J Orthop Res 2003;21:937–40.
- 65. Peters J, Luboldt W, Schwarz W, et al.. Extracorporeal shock wave therapy in calcific tendinitis of the shoulder. Skeletal Radiol 2004;33:712–8.
- 66. Hearnden A, Desai A, Karmegam A, et al.. Extracorporeal shock wave therapy in chronic calcific tendonitis of the shoulderd – is it effective? Acta Orthop Belg 2009;75:25–31.
- 67. Pleiner J, Crevenna R, Langenberger H, et al.. Extracorporeal shockwave treatment is effective in calcific tendonitis of the shoulder. A randomized controlled trial. Wien Klin Wochenschr 2004;116:536–41.
- 68. Tornese D, Mattei E, Bandi M, et al.. Arm position during extracorporeal shock wave therapy for calcifying tendinitis of the shoulder: a randomized study. Clin Rehabil 2011;25:731–9.
- 69. Sabeti M, Dorotka R, Goll A, et al.. A comparison of two different treatments with navigated extracorporeal shock-wave therapy for calcifying tendinitis – a randomized controlled trial. Wien Klin Wochenschr 2007;119:124–8.
- 70. Haake M, Sattler A, Gross MW, et al.. Comparison of extracorporeal shockwave therapy (ESWT) with roentgen irradiation in supraspinatus tendon syndrome – a prospective randomized single-blind parallel group comparison. Z Orthop Ihre Grenzgeb 2001;139:397–402.
- 71. Groß MW, Sattler A, Haake M, et al.. The value of radiotherapy in comparison with extracorporeal shockwave therapy for supraspinatus tendinitis. Strahlenther Onkol 2002;178:314–20.
- 72. Galasso O, Amelio E, Riccelli DA, et al.. Short-term outcomes of extracorporeal shock wave therapy for the treatment of chronic non-calcific tendinopathy of the supraspinatus: a double-blind, randomized, placebo-controlled trial. BMC Musculoskeletal Disord 2012;13:86.
- 73. Rompe JD, Decking J, Schoellner C, et al.. Shock wave application for chronic plantar fasciitis in running athletes. A prospective, randomized, placebo-controlled trial. Am J Sports Med 2003;31:268–75.
- 74. Ogden JA, Alvarez RG, Levitt RL, et al.. Electrohydraulic high-energy shock-wave treatment for chronic plantar fasciitis. J Bone Joint Surg Am 2004;86:2216–28.
- 75. Theodore GH, Buch M, Amendola A, et al.. Extracorporeal shock wave therapy for the treatment of plantar fasciitis. Foot Ankle Int 2004;25:290–7.
- 76. Porter MD, Shadbolt B. Intralesional corticosteroid injection versus extracorporeal shock wave therapy for plantar fasciopathy. Clin J Sport Med 2005;15:119–24.
- 77. Liang HW, Wang TG, Chen WS, et al.. Thinner plantar fascia predicts decreased pain after extracorporeal shock wave therapy. Clin Orthop Relat Res 2007;460:219–25.
- 78. Malay DS, Pressman MM, Assili A, et al.. Extracorporeal shockwave therapy versus placebo for the treatment of chronic proximal plantar fasciitis: results of a randomized, placebo-controlled, double-blinded, multicenter intervention trial. J Foot Ankle Surg 2006;45:196–210.
- 79. Vahdatpour B, Sajadieh S, Bateni V, et al.. Extracorporeal shock wave therapy in patients with plantar fasciitis. A randomized, placebo-controlled trial with ultrasonographic and subjective outcome assessments. J Res Med Sci 2012;17:834–8.
- 80. Radwan YA, Mansour AM, Badawy WS. Resistant plantar fasciopathy: shock wave versus endoscopic plantar fascial release. Int Orthop 2012;36:2147–56.
- 81. Chen TW, Lin CW, Lee CL, et al.. The efficacy of shock wave therapy in patients with knee osteoarthritis and popliteal cyamella. Kaohsiung J Med Sci 2014;30:362–70.
- 82. Kraus M, Reinhart E, Krause H, et al.. Niederenergetische extrakorporale Stosswellentherapie (ESWT) zur Behandlung von Myogelosen des M. masseter. [Low energy extracorporeal shockwave therapy (ESWT) for treatment of myogelosis of the masseter muscle]. Mund Kiefer Gesichtschir 1999;3:20–3.
- 83. Pan PJ, Chou CL, Chiou HJ, et al.. Extracorporeal shock wave therapy for chronic calcific tendinitis of the shoulders: a functional and sonographic study. Arch Phys Med Rehabil 2003;84:988–93.
- 84. Perlick L, Luring C, Bathis H, et al.. Efficacy of extracorporal shock-wave treatment for calcific tendinitis of the shoulder: experimental and clinical results. J Orthop Sci 2003;8:777–83.
- 85. Sabeti-Aschraf M, Dorotka R, Goll A, et al.. Extracorporeal shock wave therapy in the treatment of calcific tendinitis of the rotator cuff. Am J Sports Med 2005;33:1365–8.
- 86. Rompe JD, Hope C, Küllmer K, et al.. Analgesic effect of extracorporeal shock-wave therapy on chronic tennis elbow. J Bone Joint Surg Br 1996;78:233–7.
- 87. Haake M, Boddeker IR, Decker T, et al.. Side-effects of extracorporeal shock wave therapy (ESWT) in the treatment of tennis elbow. Arch Orthop Trauma Surg 2002;122:222–8.
- 88. Melikyan EY, Shahin E, Miles J, et al.. Extracorporeal shock-wave treatment for tennis elbow. A randomised double-blind study. J Bone Joint Surg Br 2003;85:852–5.
- 89. Melegati G, Tornese D, Bandi M, et al.. Comparison of two ultrasonographic localization techniques for the treatment of lateral epicondylitis with extracorporeal shock wave therapy: a randomized study. Clin Rehabil 2004;18:366–70.
- 90. Wang CJ, Liu HC, Fu TH. The effects of extracorporeal shockwave on acute high-energy long bone fractures of the lower extremity. Arch Orthop Trauma Surg 2007;127:137–42.
- 91. Costa ML, Shepstone L, Donell ST, et al.. Shock wave therapy for chronic Achilles tendon pain: a randomized placebo-controlled trial. Clin Orthop Relat Res 2005;440:199–204.
- 92. Ogden JA, Alvarez R, Levitt R, et al.. Shock wave therapy for chronic proximal plantar fasciitis. Clin Orthop Relat Res 2001;387:47–59.
- 93. Rompe JD, Schoellner C, Nafe B. Evaluation of low-energy extracorporeal shock-wave application for treatment of chronic plantar fasciitis. J Bone Joint Surg Am 2002;84:335–41.
- 94. Chew KT, Leong D, Lin CY, et al.. Comparison of autologous conditioned plasma injection, extracorporeal shockwave therapy, and conventional treatment for plantar fasciitis: a randomized trial. PM R 2013;5:1035–43.
- 95. Tornese D, Mattei E, Lucchesi G, et al.. Comparison of two extracorporeal shock wave therapy techniques for the treatment of painful subcalcaneal spur. A randomized controlled study. Clin Rehabil 2008;22:780–7.
- 96. Saxena A, Fournier M, Gerdesmeyer L, et al.. Comparison between extracorporeal shockwave therapy, placebo ESWT and endoscopic plantar fasciotomy for the treatment of chronic plantar heel pain in the athlete. Muscles Ligaments Tendons J 2013;2:312–6.
- 97. El-Shamy SM, Eid MA, El-Banna MF. Effect of extracorporeal shock wave therapy on gait pattern in hemiplegic cerebral palsy: a randomized controlled trial. Am J Phys Med Rehabil 2014;93:1065–72.
- 98. Cosentino R, De Stefano R, Selvi E, et al.. Extracorporeal shock wave therapy for chronic calcific tendinitis of the shoulder: single blind study. Ann Rheum Dis 2003;62:248–50.
- 99. Hsu CJ, Wang DY, Tseng KF, et al.. Extracorporeal shock wave therapy for calcifying tendinitis of the shoulder. J Shoulder Elbow Surg 2008;17:55–9.
- 100. Farr S, Sevelda F, Mader P, et al.. Extracorporeal shockwave therapy in calcifying tendinitis of the shoulder. Knee Surg Sports Traumatol Arthrosc 2011;19:2085–9.
- 101. Speed CA, Richards C, Nichols D, et al.. Extracorporeal shock-wave therapy for tendonitis of the rotator cuff. A double-blind, randomised, controlled trial. J Bone Joint Surg Br 2002;84:509–12.
- 102. Rompe JD, Krischek O, Eysel P, et al.. Chronische Insertionstendopathie am lateralen Epicondylus humeri. Ergebnisse der extrakorporalen Stosswellenapplikation [Results of extracorporeal shock-wave application in lateral elbow tendopathy] [Article in German]. Schmerz 1998;12:105–11.
- 103. Rompe JD, Riedel C, Betz U, et al.. Chronic lateral epicondylitis of the elbow: a prospective study of low-energy shockwave therapy and low-energy shockwave therapy plus manual therapy of the cervical spine. Arch Phys Med Rehabil 2001;82:578–82.
- 104. Chung B, Wiley JP, Rose MS. Long-term effectiveness of extracorporeal shockwave therapy in the treatment of previously untreated lateral epicondylitis. Clin J Sport Med 2005;15:305–12.
- 105. Ozturan KE, Yucel I, Cakici H, et al.. Autologous blood and corticosteroid injection and extracoporeal shock wave therapy in the treatment of lateral epicondylitis. Orthopedics 2010;33:84–91.
- 106. Wang CJ, Ko JY, Chan YS, et al.. Extracorporeal shockwave for chronic patellar tendinopathy. Am J Sports Med 2007;35:972–8.
- 107. Rompe JD, Kullmer K, Riehle H-M, et al.. Effectiveness of low-energy extracorporal shock waves for chronic plantar fasciitis. Foot Ankle Surg 1996;2:215–21.
- 108. Krischek O, Rompe JD, Herbsthofer B, et al.. Symptomatische niedrig-energetische Stosswellentherapie bei Fersenschmerzen und radiologisch nachweisbarem plantaren Fersensporn [Symptomatic low-energy shockwave therapy in heel pain and radiologically detected plantar heel spur] [Article in German]. Z Orthop Ihre Grenzgeb 1998;136:169–74.
- 109. Cosentino R, Falsetti P, Manca S, et al.. Efficacy of extracorporeal shock wave treatment in calcaneal enthesophytosis. Ann Rheum Dis 2001;60:1064–7.
- 110. Hammer DS, Adam F, Kreutz A, et al.. Extracorporeal shock wave therapy (ESWT) in patients with chronic proximal plantar fasciitis: a 2-year follow-up. Foot Ankle Int 2003;24:823–8.
- 111. Seil R, Rupp S, Hammer DS, et al.. Extrakorporale Stosswellentherapie bei der Tendionosis calcarea der Rotatorenmanschette: Vergleich verschiedener Behandlungsprotokolle. [Extracorporeal shockwave therapy in tendionosis calcarea of the rotator cuff: comparison of different treatment protocols] [Article in German]. Z Orthop Ihre Grenzgeb 1999;137:310–5.
- 112. Loew M, Daecke W, Kusnierczak D, et al.. Shock-wave therapy is effective for chronic calcifying tendinitis of the shoulder. J Bone Joint Surg Br 1999;81:863–7.
- 113. Schmitt J, Tosch A, Hünerkopf M, et al.. Die extrakorporale Stosswellentherapie (ESWT) als therapeutische Option beim Supraspinatussehnensyndrom? Ein-Jahres-Ergebnisse einer placebokontrollierten Studie. [Extracorporeal shockwave therapy (ESWT) as therapeutic option in supraspinatus tendon syndrome? One year results of a placebo controlled study] [Article in German]. Orthopade 2002;31:652–7.
- 114. Haake M, Willenberg T, Sauer F, et al.. Einfluss der Extrakorporalen Stosswellentherapie auf die Gefassregulation. Infrarotthermographie bei Epicondylitis humeri radialis. [Effect of extracorporeal shockwave therapy on vascular regulation. Infrared thermography in epicondylitis humeri radialis] [Article in German]. Swiss Surg 2002;8:176–80.
- 115. Wang CJ, Wang FS, Huang CC, et al.. Treatment for osteonecrosis of the femoral head: comparison of extracorporeal shock waves with core decompression and bone-grafting. J Bone Joint Surg Am 2005;87:2380–7.
- 116. Rompe JD, Hopf C, Nafe B, et al.. Low-energy extracorporeal shock wave therapy for painful heel: a prospective controlled single-blind study. Arch Orthop Trauma Surg 1996;115:75–9.
- 117. Wang CJ, Wang FS, Yang KD, et al.. Long-term results of extracorporeal shockwave treatment for plantar fasciitis. Am J Sports Med 2006;34:592–6.
- 118. Yucel I, Ozturan KE, Demiraran Y, et al.. Comparison of high-dose extracorporeal shockwave therapy and intralesional corticosteroid injection in the treatment of plantar fasciitis. J Am Podiatr Med Assoc 2010;100:105–10.
- 119. Hammer DS, Rupp S, Kreutz A, et al.. Extracorporeal shockwave therapy (ESWT) in patients with chronic proximal plantar fasciitis. Foot Ankle Int 2002;23:309–13.
- 120. Notarnicola A, Maccagnano G, Tafuri S, et al.. CHELT therapy in the treatment of chronic insertional Achilles tendinopathy. Lasers Med Sci 2014;29:1217–25.
- 121. Rompe JD, Bürger R, Hopf C, et al.. Shoulder function after extracorporal shock wave therapy for calcific tendinitis. J Shoulder Elbow Surg 1998;7:505–9.
- 122. Crowther MA, Bannister GC, Huma H, et al.. A prospective, randomised study to compare extracorporeal shock-wave therapy and injection of steroid for the treatment of tennis elbow. J Bone Joint Surg Br 2002;84:678–9.
- 123. Rompe JD, Hopf C, Küllmer K, et al.. Low-energy extracorporal shock wave therapy for persistent tennis elbow. Int Orthop 1996;20:23–7.
- 124. Rompe JD, Eysel P, Hopf C, et al.. Extrakorporale Sstosswellentherapie in der Orthopädie. Positive Ergebnisse beim Tennisellenbogen und der Tendinosis calcarea der Schulter [Extracorporeal shockwave therapy in orthopedics. Positive results in tennis elbow and tendinosis calcarea of the shoulder] [Article in German]. Fortschr Med 1997;115:26,29–33.
- 125. Saggini R, Cavezza T, Di Pancrazio L, et al.. Treatment of lesions of the rotator cuff. J Biol Regul Homeost Agents 2010;24:453–9.
- 126. Maher CG, Sherrington C, Herbert RD, et al.. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther 2003;83:713–21.
- 127. De Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother 2009;55:129–33.
- 128. Rompe JD, Meurer A, Nafe B, et al.. Repetitive low-energy shock wave application without local anesthesia is more efficient than repetitive low-energy shock wave application with local anesthesia in the treatment of chronic plantar fasciitis. J Orthop Res 2005;23:931–41.
- 129. Labek G, Auersperg V, Ziernhöld M, et al.. Einfluss von Lokalanasthesie und Energieflussdichte bei niederenergetischer extrakorporaler Stosswellentherapie der chronischen Plantaren Fasziitis – Eine prospektiv-randomisierte klinische Studie. [Influence of local anesthesia and energy level on the clinical outcome of extracorporeal shock wave-treatment of chronic plantar fasciitis] [Article in German]. Z Orthop Ihre Grenzgeb 2005;143:240–6.
- 130. Maier M, Averbeck B, Milz S, et al.. Substance P and prostaglandin E2 release after shock wave application to the rabbit femur. Clin Orthop Relat Res 2003;406:237–45.
- 131. Hausdorf J, Lemmens MA, Kaplan S, et al.. Extracorporeal shockwave application to the distal femur of rabbits diminishes the number of neurons immunoreactive for substance P in dorsal root ganglia L5. Brain Res 2008;1207:96–101.
- 132. Schmitz C, DePace R. Pain relief by extracorporeal shockwave therapy: an update on the current understanding. Urol Res 2009;37:231–4.
- 133. Klonschinski T, Ament SJ, Schlereth T, et al.. Application of local anesthesia inhibits effects of low-energy extracorporeal shock wave treatment (ESWT) on nociceptors. Pain Med 2011;12:1532–7.
- 134. van der Worp H, Zwerver J, Hamstra M, et al.. No difference in effectiveness between focused and radial shockwave therapy for treating patellar tendinopathy: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 2014;22:2026–32.
- 135. Neufeld SK, Cerrato R. Plantar fasciitis: evaluation and treatment. J Am Acad Orthop Surg 2008;16:338–46.
- 136. Lei H, Liu J, Li H, et al.. Low-intensity shock wave therapy and its application to erectile dysfunction. World J Mens Health 2013;31:208–14.