Introduction
Heart failure (HF) with reduced ejection fraction (HFrEF) has a well-known epidemic relevance in western countries. It affects up to 1–2% of patients > 60 years and reaches a prevalence of 12% in octogenarian patients [, ].
Although a significant improvement in the survival of these patients has been reported in the last 30 years, 5-year mortality is still about 50%, which is worse than that of cancer disease []. Therefore, an accurate prognosis is essential not only to estimate the probability of adverse events in the short term, but also to optimize treatment and refer patients to heart transplantation or implantation of a ventricular assistance device in a timely fashion.
Nowadays, cardiovascular (CV) biomarkers such as N-terminal pro-B-type natriuretic peptide (NT-proBNP) and high-sensitive troponin I (hsTnI) have been ascribed an important role in risk stratifying HFrEF patients []; however, published evidence is exclusively based on one-time assessments (i.e., performed at the first clinical evaluation), and the prognostic usefulness of serum biochemical assessments in this population still remains to be elucidated.
Therefore, the aim of our prospective longitudinal study was to evaluate the additional role of serially repeated NT-proBNP and hsTnI assessments, beyond the simpler measurement performed at baseline, to predict CV morbidity (i.e., hospitalizations) and mortality in HFrEF patients.
Methods
We prospectively recruited 226 patients with chronic HFrEF (left-ventricular [LV] ejection fraction [EF] < 35%), all referred to the Outpatient Clinic of our institution from November 2011 through September 2014.
HF patients with preserved EF (i.e., LV-EF > 50%), hospitalized for acute HF, or referred for revascularization or cardiac resynchronization therapy within 30 days and 6 months before the enrollment, respectively, were all excluded from the study.
Recruited patients underwent full clinical evaluation with complete history taking and physical examination, as well as ECG, biochemical assessment, and standard 2D and Doppler flow echocardiography at the first visit, and then again at each visit during the follow-up, repeated every 6 months.
Blood tests for routine biochemical analysis included serum levels of standard C-reactive protein, NT-proBNP, and hsTnI, and a urine test for the evaluation of microalbuminuria and urinary neutrophil gelatinase-associated lipocalin (Dimension® Clinical Chemistry System, Immunoassay Module and VITROS Immunodiagnostic Products, Triage® Biosite, Alere, respectively).
Serum NT-proBNP assessment was performed on venous blood samples, which were drawn into vacutainers containing EDTA, while hsTnI levels were determined from heparinized plasma, in agreement with current recommendations []; the hsTnI assay we used has a lower detection limit (0.009 ng/ml), corresponding to the median value of hsTnI at baseline.
Echocardiography
All echocardiographic examinations were performed with a commercially available instrument (Vivid 7 System; Vingmed, General Electric, Milwaukee, WI, USA). Standard LV systolic and diastolic parameters from 2D and Doppler echocardiography, as well as pulsed-wave tissue Doppler imaging of the mitral medial and anterolateral annulus were acquired and measured as previously described. To obtain tricuspid annular plane systolic excursion (TAPSE), the apical 4-chamber view was used, and an M-mode cursor was placed through the lateral tricuspid annulus in real time. TAPSE was measured as the total displacement of the tricuspid annulus (in cm) from end diastole to end systole. Right-ventricular systolic pressure was calculated by inserting the tricuspid regurgitation velocity, obtained with continuous-wave Doppler, into the simplified Bernoulli equation [, ].
Statistical Analysis
Statistical analysis was performed using JMP and STATA 13.1 software packages; data were described as means ± SD or n (%). Group comparisons were performed using two-sample independent t and Pearson/Fisher tests.
The primary endpoint of our study was mortality for CV causes, and hospitalization for acute HF or both were secondary endpoints. Median follow-up was 27 months, and the last follow-up assessment was on January 31, 2015.
Logistic univariate analysis was applied to evaluate the association between the variables analyzed and the study endpoints (mortality for CV causes, hospitalization for acute HF, and both combined: mortality for CV causes/hospitalization for acute HF); independent significant predictors of CV outcome were assessed by multivariate regression analysis.
A standard Kaplan-Meier curve was used to estimate patient survival, whose distribution was studied using the log-rank test. Values of p < 0.05 were considered statistically significant.
Eventually, we applied the recent statistical “multistate model”: it describes chronic diseases as a process in which an individual goes through a series of states in continuous time []. Multistate models are models for a process, which at any time occupies one of a few possible states. This can describe several possible events for a single individual or the dependence between several individuals. The events are the transitions between the states. This class of models allows for an extremely flexible approach that can model almost any kind of longitudinal failure time data. This is particularly relevant for modeling different events, which have an event-related dependence, like the occurrence of disease changing the risk of death []. A commonly used model is the illness-death model, with 3 states representing health, illness (acute HF), and death: in our study, transitions, which can be monodirectional or bidirectional, are permitted from health to illness (transition 1), illness to death (transition 2), illness to health (transition 3), and health to death (transition 4) (Fig. 1). We estimated the role of the biomarkers NT-proBNP and hsTnI to favor this process.
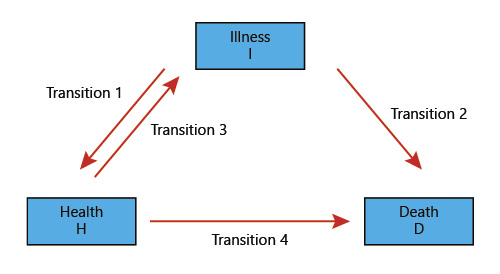
Fig. 1
Illness-death model.
Results
Baseline Characteristics
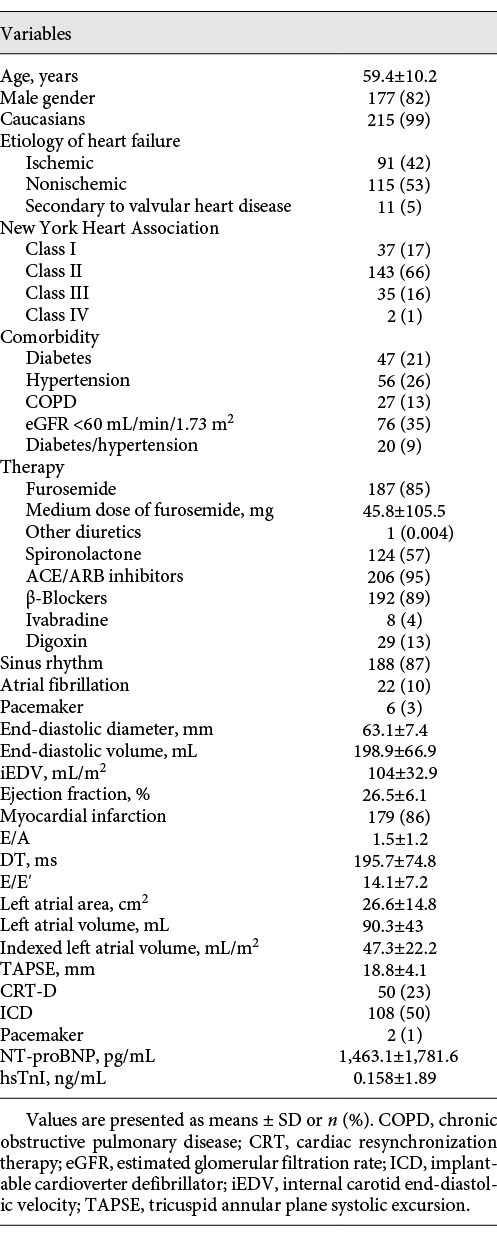
Our population was composed of 226 patients; 9 patients were excluded: 3 patients were heart transplant recipients and 6 patients were lost to follow-up.
The baseline characteristics of the patients are summarized in Table 1; the mean age of the overall population was 59 ± 10 years, 82% were males, and 99% were Caucasians. Ischemic HFrEF patients (average EF 26.5%) was noted in 42%; 66% were in New York Heart Association (NYHA) functional class II. Among CV risk factors, hypertension and type II diabetes were present in 26 and 21% of the patients; respectively. Chronic kidney disease, classified according to the National Kidney Foundation [], was found in 35% of the patients.
Guideline-based therapies were highly prevalent (95% angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, 89% β-blockers, and 57% aldosterone antagonists); 85% of the patients were treated with loop diuretics (furosemide; average daily dose of 46 ± 105.5 mg), while only 13% of patients were treated with digoxin. Regarding device therapy, an implantable cardioverter defibrillator was inserted in 73% of the patients; 23% of these cases were also referred for cardiac resynchronization therapy.
As expected, patients enrolled had altered cardiac geometry with a dilated left atrium and LV. LV end-diastolic pressure was also abnormally high according to the E/E′ ratio.
NT-proBNP and hsTnI were also abnormally increased in our study population compared to normal ranges reported.
At the last follow-up (January 31, 2015), 69 clinical events were recorded: 53 hospitalizations for acute HF and 16 CV deaths; these events, which were considered as study endpoints, occurred in 19% of the overall population, as shown in Figure 2.
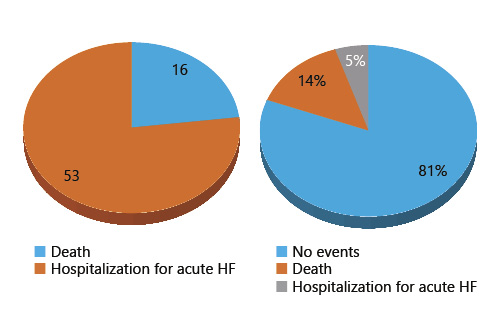
Fig. 2
Distribution of clinical events.
Multistate/Survival Analysis
During the follow-up period, CV death was observed in 16 patients; there was no statistical correlation with gender (p = 0.088) and age (p = 0.1636); baseline serum levels of NT-proBNP, however, which were 3 times higher in deceased patients, were significantly related to this clinical event (p = 0.001) (Fig. 3). Kaplan-Meier analysis confirmed these data: it demonstrated, in particular, that concentrations of NT-proBNP > 1,250 pg/mL are predictors of reduced survival (p = 0.0003) (Fig. 4).
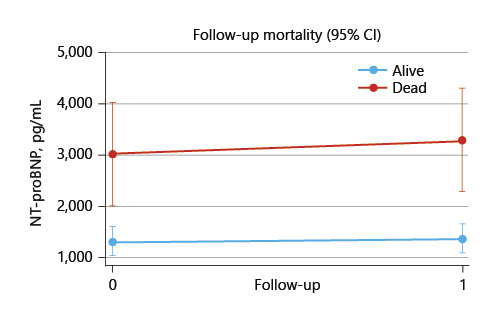
Fig. 3
Regression analysis: cardiovascular death.
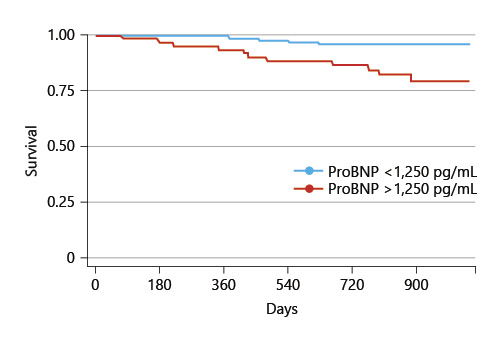
Fig. 4
Kaplan-Meier analysis: cardiovascular death.
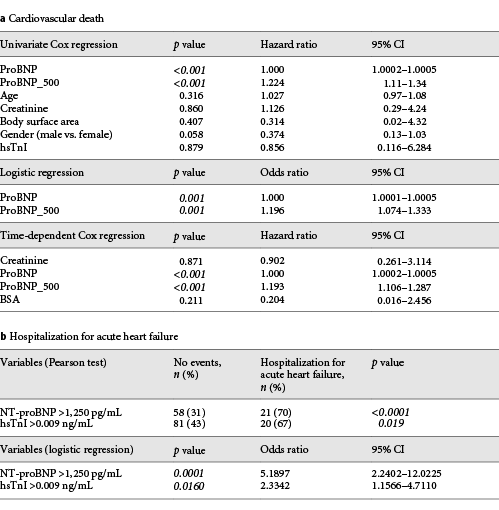
In contrast to hsTnI, univariate Cox analysis revealed that an increase in NT-proBNP of 500 units compared to baseline was related to a relative risk of CV death of 22.4%; similar results were obtained through univariate logistic regression. We also analyzed time-dependent variations in the study variables: we observed that an increase in NT-proBNP of 500 units compared to baseline was anytime correlated to a 20% increase in the relative risk of CV death, even after adjustment for gender, age, and body surface area (Table 2a).
Regarding the secondary study endpoint (hospitalization for acute HF), it was pointed out that in hospitalized patients serum levels of NT-proBNP and hsTnI were higher than in patients with no hospital readmission (in particular: NT-proBNP > 1,250 pg/mL and hsTnI > 0.009 ng/mL); using regression analyses, we demonstrated a significant correlation between an increase in the risk of hospitalization and serum concentrations of both biomarkers (Table 2b).
Applying the recent statistical illness-death model, we observed 122 transitions: 53 from health to illness (transition 1), 53 from illness to health (transition 3), and 16 from health to death (transition 4). None of the transitions from illness to death (transition 2) verified, because all patients hospitalized were discharged home. Using the Cox model, we demonstrated that a statistical correlation existed between an increase in NT-proBNP of 500 units compared to baseline and the risk of transition both from health to illness (hazard ratio 1.278, p < 0.001, 95% CI 1.215–1.343) and from health to death (hazard ratio 1.234, p < 0.001, 95% CI 1.124–1.356); we were not able to evaluate the role of this biomarker to favor transition from illness to health (transition 3) since serum values were not assessed at discharge.
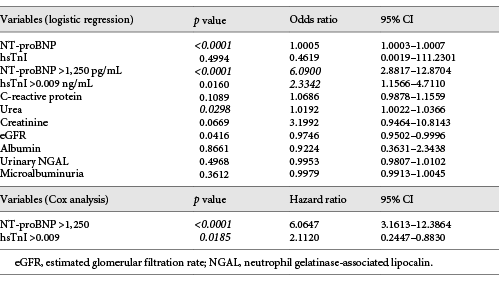
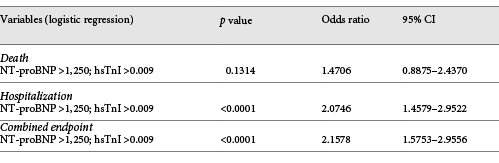
We also studied the composite of CV mortality and hospitalization to be able to determine the true burden of the HF syndrome; we demonstrated that high serum levels of NT-proBNP were associated with an increased risk of the composite endpoint, which is in contrast to hsTnI. Stratifying our population according to the serum levels of NT-proBNP and hsTnI, we found that the risk of CV death combined with hospitalization was significantly associated with NT-proBNP and hsTnI concentrations > 1,250 pg/mL and > 0.009 ng/mL, respectively; we obtained similar results using univariate Cox analyses. The independent prognostic role of NT-proBNP was subsequently confirmed by multivariate regression (Table 3). With respect to the statistical value of the multimarker strategy to assess the prognosis of patients with chronic HF [], the predictive role of the association between NT-proBNP and hsTnI was evaluated. Our population was divided into 4 subgroups on the basis of plasma NT-proBNP and hsTnI levels: the relative risk of both hospitalization for acute HF and the composite of CV mortality and hospitalization, but not the risk of CV death alone, was apparently correlated to increases in the levels of both biomarkers (Table 4).
Discussion
Despite advances in the management of chronic HF, it still represents the leading cause of hospitalization in industrialized countries, with a 5-year mortality of about 50%; thus, it becomes mandatory to be able to identify individuals at increased HF risk and to predict the prognosis of patients affected.
According to literature data, the assessment of natriuretic peptides, markers of myocardial stress, may enhance risk stratification in all clinical HF stages [-]; in patients with chronic HF, particularly NT-proBNP plays an important role in prognosis [].
In our study, NT-proBNP represents a strong predictor of CV outcome: an increase in NT-proBNP of 500 units compared to baseline is anytime correlated to an increased relative risk of CV death, and it also influences the “transition” from the state of health to the state of illness/death; moreover, patients with serum levels > 1,250 pg/mL are at increased risk of hospitalization for acute HF. These associations persist considering also the composite of CV mortality and hospitalization.
Scientific evidence demonstrates that cardiac troponins, which represent markers of myocyte injury, play a considerable role in the prognostic stratification of HF patients regardless of ischemic etiology; in particular, in subjects with chronic HF, high serum hsTnI levels are predictors of an increased risk of mortality for all causes [].
Although there is no statistical correlation between the serum concentration of hsTnI and CV death, probably because of clinically stable disease in our patients, our data confirm the role of hsTnI as a prognostic indicator of an increased risk for acute HF hospitalization.
In a recent multicenter study, a cohort of chronic HF outpatients was analyzed in order to evaluate the prognostic role of 9 biomarkers: among these, BNP and TnI exhibited the strongest association with the risk of cardiac hospitalization overall regardless of ischemic etiology; they have been shown to be associated independently with morbidity and mortality and to have an additive ‘‘dose-response’’ effect, with stronger associations seen with elevations in both biomarkers over either biomarker alone [-]. Similar results have been obtained through our statistical analyses, which, therefore, confirm the power of the multimarker strategy to predict the relative risk of both hospitalization for acute HF and the composite of CV mortality and hospitalization.
A limitation of this study is the single-center design of our study and that results have to be confirmed in a larger population of HFrEF patients.
Conclusion
In summary, we found that NT-proBNP, a marker of myocardial stress, represents a strong and independent predictor of CV outcome; serum hsTnI levels, which significantly correlated with an increased risk of hospitalization, cannot properly predict the relative risk of CV mortality. Our study validates eventually the multimarker strategy, which reflects the complexity of the HF pathophysiology.
Further studies are required to evaluate the implications of our results also in the therapeutic management of chronic HF patients (biomarker-guided therapy).
Statement of Ethics
All study patients provided written informed consent, and our IRRB approved the study.
Disclosure Statement
The authors have no conflict of interest.
References
- 1. Jhund PS, Macintyre K, Simpson CR, Lewsey JD, Stewart S, Redpath A, et al Long-term trends in first hospitalization for heart failure and subsequent survival between 1986 and 2003: a population study of 5.1 million people. Circulation. 2009;119(4):515–23.
- 2. Laribi S, Aouba A, Nikolaou M, Lassus J, Cohen-Solal A, Plaisance P, et alGREAT network. Trends in death attributed to heart failure over the past two decades in Europe. Eur J Heart Fail. 2012;14(3):234–9.
- 3. Askoxylakis V, Thieke C, Pleger ST, Most P, Tanner J, Lindel K, et al Long-term survival of cancer patients compared to heart failure and stroke: a systematic review. BMC Cancer. 2010;10(1):105.
- 4. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et alESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200.
- 5. Apple FS, Jesse RL, Newby LK, Wu AH, Christenson RHNational Academy of Clinical BiochemistryIFCC Committee for Standardization of Markers of Cardiac Damage. National Academy of Clinical Biochemistry and IFCC Committee for Standardization of Markers of Cardiac Damage Laboratory Medicine Practice Guidelines: analytical issues for biochemical markers of acute coronary syndromes. Circulation. 2007;115(13):e352–5.
- 6. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015;16(3):233–70.
- 7. Irvine T, Li XK, Sahn DJ, Kenny A. Assessment of mitral regurgitation. Heart. 2002;88Suppl 4:iv11–9.
- 8. Collett D. Multiple events and event history modelling. David Collet. Modelling survival data in medical research. 3rd ed.CRC press.
- 9. Hougaard P. Multi-state models: a review. Lifetime Data Anal. 1999;5(3):239–64.
- 10. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2Suppl 1):S1–266.
- 11. Ahmad T, Fiuzat M, Neely B, Neely ML, Pencina MJ, Kraus WE, et al Biomarkers of myocardial stress and fibrosis as predictors of mode of death in patients with chronic heart failure. JACC Heart Fail. 2014;2(3):260–8.
- 12. Tsutamoto T, Wada A, Maeda K, Hisanaga T, Maeda Y, Fukai D, et al Attenuation of compensation of endogenous cardiac natriuretic peptide system in chronic heart failure: prognostic role of plasma brain natriuretic peptide concentration in patients with chronic symptomatic left ventricular dysfunction. Circulation. 1997;96(2):509–16.
- 13. Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, et alBreathing Not Properly Multinational Study Investigators. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347(3):161–7.
- 14. Januzzi JL, van Kimmenade R, Lainchbury J, Bayes-Genis A, Ordonez-Llanos J, Santalo-Bel M, et al NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study. Eur Heart J. 2006;27(3):330–7.
- 15. Moe GW, Howlett J, Januzzi JL, Zowall HCanadian Multicenter Improved Management of Patients With Congestive Heart Failure (IMPROVE-CHF) Study Investigators. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation. 2007;115(24):3103–10.
- 16. Doust JA, Pietrzak E, Dobson A, Glasziou P. How well does B-type natriuretic peptide predict death and cardiac events in patients with heart failure: systematic review. BMJ. 2005;330(7492):625.
- 17. Masson S, Latini R, Anand IS, Vago T, Angelici L, Barlera S, et alVal-HeFT Investigators. Direct comparison of B-type natriuretic peptide (BNP) and amino-terminal proBNP in a large population of patients with chronic and symptomatic heart failure: the Valsartan Heart Failure (Val-HeFT) data. Clin Chem. 2006;52(8):1528–38.
- 18. Latini R, Masson S, Anand IS, Missov E, Carlson M, Vago T, et alVal-HeFT Investigators. Prognostic value of very low plasma concentrations of troponin T in patients with stable chronic heart failure. Circulation. 2007;116(11):1242–9.
- 19. Vorovich E, French B, Ky B, Goldberg L, Fang JC, Sweitzer NK, et al Biomarker predictors of cardiac hospitalization in chronic heart failure: a recurrent event analysis. J Card Fail. 2014;20(8):569–76.