Introduction
The COVID-19 pandemic is causing an unprecedented challenge for hospital systems across the world. Limited resources, strict infectious disease control measures, and public perception have stressed all facets of healthcare, particularly acute care systems such as stroke, acute coronary syndrome, and trauma workflows. As the pandemic was beginning to take hold in North America, Tam and colleagues [] reported the impact of COVID-19 outbreak on ST-segment elevation myocardial infarction in Hong Kong, China, where they observed an increase in treatment times for 7 STEMI patients after implementation of stringent infection control measures. These 7 patients were not infected with COVID-19, highlighting the pandemic response effects on acute care unrelated to infectious disease [].
As the world became further entrenched in the current pandemic, there has been a concomitant surge of observations and implementation of dynamic guidelines regarding acute stroke care [-]. A common observation from numerous hospitals and hospital systems has been a sharp decrease in patients presenting with stroke-like symptoms [-]. Conversely, Oxley et al. [] reported a disturbing incidence of large vessel stroke as a presenting feature of COVID-19 in the young.
We sought to investigate the impact of COVID-19 emergency response measures on acute stroke care in Los Angeles County (LAC), with a collaborative effort involving multiple comprehensive stroke centers. LAC holds >10 million residents and unfortunately has seen a high incidence of COVID infection numbers when compared to other major metropolitan cities across the USA []. Participating CSCs are located across different areas of LAC and include a range of hospital sizes in a range of socioeconomic regions: Cedars-Sinai Medical Center (CSMC), University of California, Los Angeles (UCLA), Kaiser Permanente, Los Angeles Medical Center (KP-LAMC), Providence Saint Joseph Medical Center in Burbank (Burbank), Providence Saint John’s Health Center in Santa Monica (Santa Monica), Providence Little Company of Mary Medical Center in Torrance (LCM), PIH Health Whittier Hospital (PIH), PIH Health Good Samaritan Hospital (Good Sam), and Torrance Memorial Medical Center (TMMC).
In an effort to mitigate healthcare worker COVID-19 exposure, telemedicine (telestroke) has been widely implemented in Emergency Departments and within residency training programs []. Acute care workflows have been adjusted as necessary, with the focus remaining on efficiently providing emergency stroke care and recanalization treatment for eligible acute ischemic stroke patients. CSMC, the coordinating CSC, provided acute stroke care in the Emergency Department while limiting the physical presence to a single team member from the Stroke Team, incorporating InTouch Provider® software and Multipresence (InTouch Health, Goleta, CA, USA) [].
We also sought to measure the effect of COVID-19 on hospital metrics of acute stroke care. Acute stroke care relies heavily on strict time windows; we postulated a decrease in patients presenting within said windows due to anxiety surrounding safety of healthcare centers during the pandemic. Patients treated with intravenous thrombolytics (IVT) must present within 4.5 h of the last well known or symptom discovery, while the window for mechanical thrombectomy (MT) patients who present with a large vessel occlusion must present within 24 h [-]. Recent reports indicate COVID-19 has disproportionately impacted Latinx communities in Southern California, and thus we sought to evaluate if there is correlation between participating CSCs, geographic COVID-19 positivity rates, and acute stroke admissions [].
Methods
We evaluated acute stroke care admissions in 2019 and during the COVID-19 pandemic in the same quarter in 2020 across 9 participating CSCs. County demographics were obtained via Community Health Needs Assessment reports produced by each CSC. COVID-19 testing during the time period in question was highly variable, and thus there is much uncertainty regarding true infectious rates for each individual institution. However, the Los Angeles Public Health Department and Los Angeles Times would later publish their findings regarding regional differences in positive cases as testing became more reliable in subsequent months [].
Volume of Emergency Department stroke code activations, patient characteristics (age/gender), stroke severity presentation (NIH Stroke Scale), reperfusion therapy rates, and treatment times in a 3-month period from February 1 to April 30, 2020, were compared with the same time period in 2019 []. There were no significant changes to Emergency Medical Services routing procedures throughout LA county nor any significant change to each institution’s acute stroke care pathways between the 2 time periods in 2019 and 2020, aside from more use of telemedicine in 2020 as described previously. Reperfusion treatments were categorized into 4 groups: (1) no reperfusion treatment, (2) thrombolytic treatment only (IVT), (3) MT only, or (4) combined recanalization therapies (IVT and MT). Many of these data points are tracked by each CSC including door-to-needle (DTN) times for IVT and door-to-groin puncture (DTG) times for MT. Outcomes were based on discharge locations: home, skilled nursing facility, or expired.
All institutions obtained individual IRB waivers and data use agreements in place with coordinating center, CSMC, for data sharing, study analysis, and publication. All sites participated in weekly virtual meetings to clarify data collection and address questions regarding data validity whilst performing extensive chart review. Deidentified patient information was secured in a master database.
Statistical Methods
Categorical variables were summarized by frequencies and percentages and compared across the year using the χ2 or Fisher’s exact test. Numerical variables were summarized by mean and standard deviation and compared across the year by the Wilcoxon rank sum test. A 2-sided 0.05 significance level was used throughout. As this was an exploratory study, we did not adjust from multiple comparisons. Statistical calculations were made using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
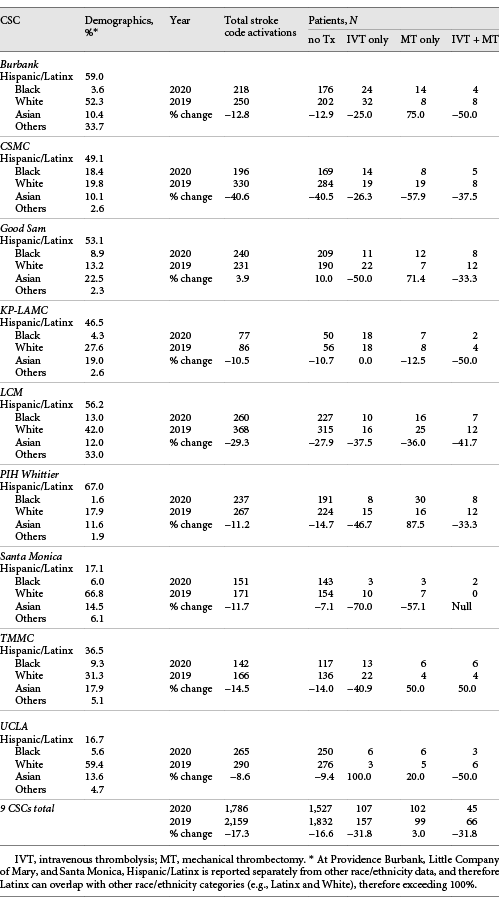
From February 1, 2020, to April 30, 2020, there were 1,786 activated stroke codes compared to 2,159 in 2019 (17.3% decrease, χ2 goodness of fit test p < 0.0001) in the same time frame across 9 participating CSCs. Patients who did not receive any reperfusion therapy similarly decreased by 16.6% in 2020 (1,527 vs. 1,832 patients). There was a larger drop in IVT in 2020, with a 31.8% decrease across CSCs (107 vs. 157 patients). Patients who received only MT increased by 3% in 2020 (102 vs. 99 patients). Patients who received both IVT and MT decreased by 31.8% (45 vs. 66 patients), mostly explained by the drop in the IVT-arm of combination recanalization treatment. Individual CSC demographics, stroke code activations, and reperfusion treatment numbers are depicted in Table 1. Individual CSC changes in reperfusion therapy treatment numbers are depicted in Figure 1, and regional changes are depicted in Figure 2.
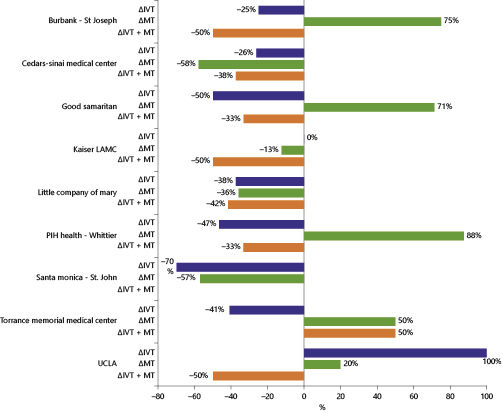
Fig. 1
Individual CSC change in reperfusion therapy rate. Forest plot showing percentage change of patients treated with IVT, MT, and combined IVT + MT as reported by each participating comprehensive stroke center. IVT, intravenous thrombolysis; MT, mechanical thrombectomy.
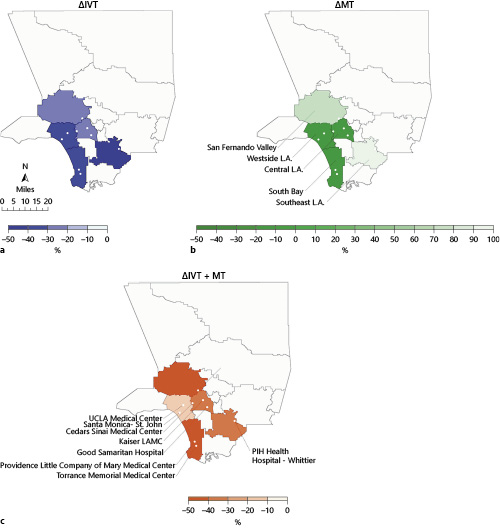
Fig. 2
Regional change in patients receiving reperfusion therapies. a The percentage change in number of patients treated with IVT (milder symptoms, presenting within 4.5 h of symptom onset) in 2020 as compared to 2019. b The percentage change in number of patients treated with MT alone (more severe presentations, presenting within 24 h of symptom onset). c Combined IVT and MT (more severe presentations within 4.5 h of symptom onset). IVT, intravenous thrombolysis; MT, mechanical thrombectomy.
DTN and DTG times remained similar throughout both timeframes across all patient populations. In patients receiving only IVT, mean DTN 2020 was 55.7 ± 27.0 min compared to 55.6 ± 34.5 min in 2019 (Wilcoxon rank sum test p = 0.31). In patients receiving only MT, average DTG 2020 was 99.2 ± 60.5 min compared to DTG 2019 of 110.2 ± 65.3 min (p = 0.26). In patients receiving both IVT and MT, 2020 DTN was 44.2 ± 17.6 min compared to 2019 DTN 43.7 ± 27.2 min (p = 0.21) and 2020 DTG was 96.5 ± 24.5 min compared to 2019 DTG 99.4 ± 40.1 min (p = 0.94).
There was a significant increase in mean NIHSS in 2020 compared to 2019 (8.95 vs. 8.23, p = 0.046), while median NIHSS remained the same at 4. There was no significant difference in age or sex between both years.
A higher percentage of patients were discharged home in 2020 compared to 2019 (59.5 vs. 56.1%, p = 0.034). A lower percentage of patients were discharged to skilled nursing facilities in 2020 compared to 2019 (16.1 vs. 20.7%, p = 0.0004). A higher percentage of acute ischemic stroke patients expired in 2020 compared to 2019 (8.6 vs. 6.3%, p = 0.008).
Discussion
In 9 CSCs across LAC that represent a range of demographic and socioeconomic regions, there was an observed decrease in stroke code activations at the start of the COVID-19 pandemic. There was a concomitant larger decrease in patients with acute ischemic stroke treated with IVT (presenting <4.5 h), while patients with large vessel occlusion who qualified for MT (more severe symptoms, presenting <24 h) slightly increased in 2020 compared to 2019, most notable in the eastern parts of LAC. Patients are presenting with more severe symptoms as evidenced by slight but statistically significant observed increase in presenting NIHSS. As patients in both IVT and IVT + MT groups decreased, this is consistent with patient reports of hesitation in seeking emergency medical care during the pandemic, especially in those with milder stroke symptoms []. While the incidence of acute ischemic stroke remained constant, fewer patients were presenting within 4.5 h of symptom onset to receive IVT.
This study has some limitations, most notably it does not capture stroke patients who presented outside the window for reperfusion therapies, as no stroke code was activated. Demographic data are not reported in uniform manner across institutions.
While IVT patient volumes decreased across all institutions, there are notable differences between individual institutions and MT frequency. Burbank, Good Sam, and PIH all report a remarkable >70% increase in MT patients in 2020 compared to 2019. These CSCs serve a population that has consistently seen a higher COVID-19 infection burden as reported by the Los Angeles Department of Health and Los Angeles Times. These CSCs also serve a higher Latinx population relative to LA County.
As this study captures the beginning of the pandemic in LAC, reliable COVID-19 testing was not available until late March 2020. Therefore, it is difficult to make a clear correlation between COVID-19 infection rates driving the increase in MT rates and stroke severity. However, the notable regional differences across LAC along with the differences in community ethnicity breakdown highlight the big differences seen among CSCs, even within the same county in a large metropolitan US city. The 9 CSCs represented in this study provide a unique perspective, with more than half of LAC’s 16 total CSCs participating in this observational study. However, this study does not report findings from LAC’s primary stroke centers, which also treat a large proportion of IVT eligible patients. We are actively collaborating with the LAC EMS Medical Director to address these access issues, with a goal to reach more patients who need emergency stroke care with the use of telemedicine, connecting stroke expertise to our ER colleagues on the front lines.
DTN and DTG treatment times remain comparable to prepandemic metrics. Dynamic workflow changes such as donning and doffing PPE and incorporating telestroke have not significantly changed recanalization treatment times. Discharge disposition data suggest that there was a stronger push from both patient and care teams to discharge home rather than nursing facilities given concerns of COVID infection spreading at high rates in nursing homes. Outcome data also show increased mortality in emergency acute ischemic stroke patients during the pandemic compared to the year prior with patients presenting with greater stroke severity in 2020.
Overall, the 9 CSCs continue to provide emergency stroke recanalization treatments with comparable care, before pandemic and during the pandemic in LAC. Pragmatic updates to acute stroke workflows as stated in the AHA/ASA Stroke Guidelines during the pandemic have ensured emergency recanalization treatments can occur without delay [].
Statement of Ethics
Every participating institution had individual IRB approval. As this was a retrospective study on data already being collected, ethical approval was not required.
Conflict of Interest Statement
Jason W. Tarpley, MD, is a consultant for Medtronic – Modest. Otherwise, the authors have no conflicts of interest to declare.
Funding Sources
The authors did not receive any funding.
Author Contributions
All authors participated in weekly meetings throughout the pandemic. M. Maximillian Padrick, MD: study design, data acquisition, data analysis, manuscript draft, and revisions. Navdeep Sangha, MD: study design, data acquisition, and data analysis. Laurie Paletz, RN: study design, data acquisition, and data integrity validation. James Mirocha, MS: statistical analysis. Sonia Figueroa: data acquisition and data integrity validation. Vicki Manoukian, MA: DUA approval, IRB approval, data acquisition, and data integrity validation. Konrad Schlick, MD: data acquisition, data analysis, and manuscript edits. Patrick D. Lyden, MD: data acquisition, data analysis, and manuscript edits. David S. Liebeskind, MD: data acquisition, data analysis, and manuscript edits. Fiona K. Chatfield, RN, MSN, MBA: data acquisition and data integrity validation. Jason W. Tarpley, MD: data acquisition, data analysis, and data integrity validation. Adrian Burgos, MD: data acquisition, data analysis, and data integrity validation. Matthew Tenser, MD: data acquisition, data analysis, and data integrity validation. Denise Gaffney, MSN, RN: data acquisition and data integrity validation. Marco A. Pech, MSN, RN: data acquisition and data integrity validation. Edward Nazareth, MSN-Ed RN: data acquisition and data integrity validation. Robert Jackson, MD: data acquisition and data integrity validation. Helaine Kauffman, RN: data acquisition and data integrity validation. Lisa Arnold, RN: data acquisition and data integrity validation. Jennifer Cox, RN, MSN: data acquisition and data integrity validation. Treasure Joyce, LVN: data acquisition and data integrity validation. Catrice Nakamura, RN, MSN: data acquisition and data integrity validation. Darcie Fitzgerald, OT: data acquisition and data integrity validation. Kyle Ogami, MD: data acquisition and data integrity validation. Nili Steiner, RN: data acquisition and data integrity validation. Nicole Wolber, RN: data acquisition and data integrity validation. Betty Robertson, RN: data acquisition and data integrity validation. Rachel Izzo, RN: data acquisition and data integrity validation. Stefanie Gorski, MSN: data acquisition and data integrity validation. Heather Manuel: data acquisition and data integrity validation. Krystal Valdez, MSN: data acquisition and data integrity validation. Liliana Reyes: data acquisition and data integrity validation. Latisha K. Sharma, MD: study design, data acquisition, and data analysis. Shlee S. Song, MD: study design, data acquisition, data analysis, and manuscript revisions.
References
- 1. Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on st-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4):e006631.
- 2. AHA/ASA Stroke Council Leadership. Temporary emergency guidance to US stroke centers during the COVID-19 pandemic. Stroke. 2020;51(6):1910.
- 3. Baracchini C, Pieroni A, Viaro F, Cianci V, Cattelan AM, Tiberio I, et al. Acute stroke management pathway during coronavirus-19 pandemic. Neurol Sci. 2020;41(5):1003–5.http://dx.doi.org/10.1007/s10072-020-04375-9.
- 4. Bhaskar S, Sharma D, Walker AH, McDonald M, Huasen B, Haridas A, et al. Acute neurological care in the COVID-19 era: the pandemic health system resilience program (REPROGRAM) consortium pathway. Front Neurol. 2020;11:579.http://dx.doi.org/10.3389/fneur.2020.00579.
- 5. Smith MS, Bonomo J, Knight WA, Prestigiacomo CJ, Richards CT, Ramser E, et al. Endovascular therapy for patients with acute ischemic stroke during the COVID-19 pandemic: a proposed algorithm. Stroke. 2020;51(6):1902.
- 6. Sharma D, Rasmussen M, Han R, Whalin MK, Davis M, Kofke WA, et al. Anesthetic management of endovascular treatment of acute ischemic stroke during COVID-19 pandemic: consensus statement from society for neuroscience in anesthesiology & critical care (SNACC): endorsed by society of vascular & interventional neurology (SVIN), society of neurointerventional surgery (SNIS), neurocritical care society (NCS), European society of minimally invasive neurological therapy (ESMINT) and American association of neurological surgeons (AANS) and congress of neurological surgeons (CNS) cerebrovascular section. J Neurosurg Anesthesiol. 2020;32(3):193–201.
- 7. Salahuddin H, Castonguay AC, Zaidi SF, Burgess R, Jadhav AP, Jumaa MA. Interventional stroke care in the era of COVID-19. Front Neurol. 2020;11:468.http://dx.doi.org/10.3389/fneur.2020.00468.
- 8. Nguyen TN, Abdalkader M, Jovin TG, Nogueira RG, Jadhav AP, Haussen DC, et al. Mechanical thrombectomy in the era of the COVID-19 pandemic: emergency preparedness for neuroscience teams: a guidance statement from the society of vascular and interventional neurology. Stroke. 2020;51(6):1896.
- 9. Esenwa C, Parides MK, Labovitz DL. The effect of COVID-19 on stroke hospitalizations in New York city. J Stroke Cerebrovasc Dis. 2020;29(10):105114.http://dx.doi.org/10.1016/j.jstrokecerebrovasdis.2020.105114.
- 10. Khosravani H, Rajendram P, Notario L, Chapman MG, Menon BK. Protected code stroke: hyperacute stroke management during the coronavirus disease 2019 (COVID-19) pandemic. Stroke. 2020;51(6):1891–5.http://dx.doi.org/10.1161/STROKEAHA.120.029838.
- 11. Qureshi AI, Abd-Allah F, Al-Senani F, Aytac E, Borhani-Haghighi A, Ciccone A, et al. Management of acute ischemic stroke in patients with COVID-19 infection: report of an international panel. Int J Stroke. 2020;15(5):540–54.
- 12. de Havenon A, Ney J, Callaghan B, Delic A, Hohmann S, Shippey E, et al. A rapid decrease in stroke, acute coronary syndrome, and corresponding interventions at 65 United States hospitals following emergence of COVID-19. MedRxiv. 2020.
- 13. Diegoli H, Magalhães PSC, Martins SCO, Moro CHC, França PHC, Safanelli J, et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Stroke. 2020;51(8):2315.
- 14. Tejada Meza H, Lambea Á, Sancho Saldaña A, Martínez-Zabaleta MT, de la Riva P, López-Cancio E, et al. EXPRESS: Impact of COVID-19 outbreak in ischemic stroke admissions and in-hospital mortality in North-West Spain. Int J Stroke. 2020:1747493020938301.
- 15. Morelli N, Rota E, Terracciano C, Immovilli P, Spallazzi M, Colombi D, et al. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. Eur Neurol. 2020;83:213–5.http://dx.doi.org/10.1159/000507666.
- 16. Montaner J, Barragán-Prieto A, Pérez-Sánchez S, Escudero-Martínez I, Moniche F, Sánchez-Miura JA, et al. Break in the stroke chain of survival due to COVID-19. Stroke. 2020;51(8):2307.
- 17. Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP, et al. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020;382:e60.http://dx.doi.org/10.1056/NEJMc2009787.
- 18.
- 19. Zha AM, Chung LS, Song SS, Majersik JJ, Jagolino-Cole AL. Training in neurology: adoption of resident teleneurology training in the wake of COVID-19: telemedicine crash course. Neurology. 2020;95(9):404.
- 20.
- 21. Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375(9727):1695–703.http://dx.doi.org/10.1016/S0140-6736(10)60491-6.
- 22. Thomalla G, Simonsen CZ, Boutitie F, Andersen G, Berthezene Y, Cheng B, et al. MRI-guided thrombolysis for stroke with unknown time of onset. N Engl J Med. 2018;379(7):611–22.http://dx.doi.org/10.1056/NEJMoa1804355.
- 23. Schwamm LH, Wu O, Song SS, Latour LL, Ford AL, Hsia AW, et al. Intravenous thrombolysis in unwitnessed stroke onset: mr witness trial results. Ann Neurol. 2018;83(5):980–93.http://dx.doi.org/10.1002/ana.25235.
- 24. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6–24 h after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378(1):11–21.http://dx.doi.org/10.1056/NEJMoa1706442.
- 25. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6–16 h with selection by perfusion imaging. N Engl J Med. 2018;378(8):708–18.http://dx.doi.org/10.1056/NEJMoa1713973.
- 26. Lin R-GI. Latinos now twice as likely as whites to get coronavirus in L.A. County: Los Angeles Times; 2020.
- 27.
- 28.
- 29. Nguyen-Huynh MN, Tang XN, Vinson DR, Flint AC, Alexander JG, Meighan M, et al. Acute stroke presentation, care, and outcomes in community hospitals in Northern California during the COVID-19 pandemic. Stroke. 2020;51(10):2918.