Background and purpose
Conditions of the work environment within healthcare organizations are thought to represent a significant contributing problem to occupational stress (). Nurses working in acute care hospitals often practice with competing organizational demands that conflict with their professional expectations, (; ) such as hospital system efficiency initiatives that pull nurses away from care () or when nurses are required to perform the clerical duties of an absent unit clerk (). Nurses are also subject to incompatible expectations from patients and their families, managers, administrators, and other healthcare providers (; ; ), such as administrators’ expectations that nurses quickly and efficiently discharge older patients who, in turn, need more time to be prepared (). When nurses are unable to reconcile these differences, they experience role conflict. Role conflict occurs when an employee experiences competing, incompatible, and/or conflicting sets of expectations and demands in the workplace (; , ). Defined as the “incongruity or incompatibility of expectations associated with a role” (, p. 474), role conflict represents a significant occupational stressor ().
Role conflict has been associated with burnout (; ; ), an extended response to chronic occupational-related stressors (), poor mental health and high turnover in nurses working in acute care hospitals (). Meta-analytic studies have found that role conflict is associated with nurses’ intent to leave their current workplaces ().
In Ontario Canada, there are three categories of nurses: registered nurses (RNs), registered practical nurses (RPNs) and nurse practitioners which require different levels of education and responsibility. This study focused on RNs and RPNs. Since 2005, Ontario RNs require a 4-year bachelor’s degree in nursing for entry into practice () whereas RPNs require a 2-year diploma in practical nursing. RNs’ education permits for greater foundational knowledge in clinical practice, decision-making, critical thinking, leadership and resource management (). Canadian acute care hospitals have begun hiring more RPNs to reduce nursing care costs (). Acute care hospitals in Ontario are the second largest (22.4%) employer of RPNs (). Prior studies have found that different employees, exposed to the same work environment, can perceive and/or react to their work environment differently (). We found few studies that describe and compare nurses’ perceptions of role conflict by professional designation (RNs and RPNs). Research that advances understanding of the perceptions of role conflict that RNs and RPNs experience is needed to help administrators develop strategies to address the sources of conflict, tailored to the needs of RNs and RPNs in different areas of practice and therefore, sustain the acute care nursing workforce. This study addresses this needthese gaps in knowledge. The objectives were to describe and compare nurses’ perceptions of role conflict by professional designation (RN vs RPN) in three primary areas of practice (emergency department, medical unit, and surgical unit).
Methods and procedures
Design
The data for this study were obtained from a large cross-sectional survey that had a 55% response rate () and used the Tailored Design Method by Dillman. The survey, which was approved by the research ethics board at York University, included questions about nurses’ work environments, roles and demographic and occupational characteristics.
Data collection
Nurses whose names were randomly selected from the College of Nurses’ (CNO) database were provided a mailed introductory letter stating the objectives of the study and informing them that a package would be sent containing the study cover letter, a description of the study and respondents’ rights as research participants, and a questionnaire. One week after the package was mailed, a postcard was sent thanking nurses who had responded and reminding non-responding nurses about the survey. Up to two reminders and a replacement, survey were sent to nurses who had not responded to the survey.
Sample
The names and home addresses of potential participants were randomly selected from the CNO database, using a random number generator in a statistical package, and stratified to create a sampling frame for the project. A proportional stratified random sampling strategy was employed to select RN and RPN participants. The sampling frame was structured to reflect the distribution of eligible RNs (72%) and RPNs (28%) working in acute care hospitals, as tabulated by the CNO specifically for this study ().
All RNs and RPNs who met the following eligibility criteria were selected from the larger database to participate in the current study: 1) actively registered with the CNO, 2) Ontario was their clinical practice location, 3) employed in an acute care hospital, 4) position as a staff nurse providing direct patient care, and 5) primary area of practice was emergency department, medical unit, or surgical unit.
In total, 1,981 nurses met this study’s eligibility criteria. We applied a sample size calculation formula () to determine that this sample size was adequate to detect small to moderate differences in the level of role conflict as perceived RNs and RPNs employed in three primary areas of practice (emergency department, medical unit, and surgical unit).
Measures
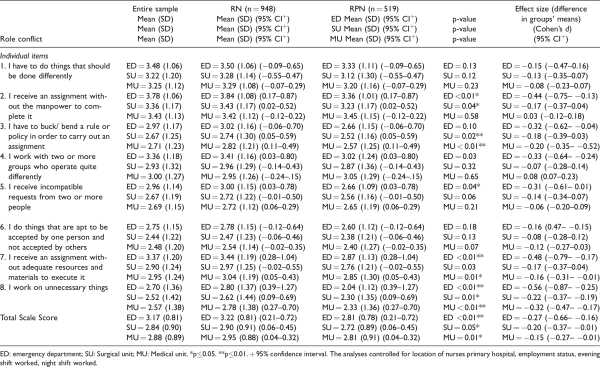
Role conflict was measured by the Role Conflict Scale, developed by . The scale has eight items that assess the extent to which an employee experiences competing or conflicting sets of expectations and demands in different situations at the workplace (Table 2). For example, one item states “I receive incompatible/conflicting requests from two or more people”. A five-point scale ranging from 1 (Strongly Disagree) to 5 (Strongly Agree) was used in the rating. A total scale score is computed as the sum of the items’ scores and can range from 8 to 40, with higher scores indicating higher levels of perceived role conflict. The psychometric properties of the scale have been previously validated and the scale has been used in numerous studies (; ). The scale demonstrated construct validity; findings of confirmatory factor analysis supported a one-factor structure (goodness-of-fit index = 0.94, root-mean square residual = 0.06, normed fix index = 0.89) (), with item loadings >0.80 (; ). The scale demonstrated internal consistency reliability (Cronbach’s alpha coefficients ranged from 0.78 to .95) in samples of acute care nurses (González‐Romá & Lloret, 1998; ); and test-retest reliability (r = 0.44) (). In the current study sample, the scale demonstrated high internal consistency reliability with a Cronbach’s alpha coefficient of 0.87 in the total sample, and 0.87 and 0.86 in the RN and RPN sub-sample, respectively.
Primary area of practice (e.g. medical unit) and professional designation (e.g. RN or RPN) were measured using standard self-report questions as were other demographic and occupational variables. These included age, gender, employment status (e.g. full-time), highest level of education attained in nursing, shifts worked (e.g., days, evenings, nights, weekends) and the name and location of nurses’ primary hospital. We used information from the latter to derive a variable on the Local Health Integrated Network hospital region. As nurses worked multiple shifts, we created four dichotomous shifts worked variables: day, evening, night, and weekend. We reported the results that were statistically significant and their effect sizes were included to aid us in interpreting the statistically significant results.
Data analysis
Preliminary analyses included tests of the assumptions of the planned inferential statistics. Although we found no evidence in the literature that role conflict differs by nurses’ demographic or occupational characteristics, preliminary analyses also included examining if RNs and RPNs differed by age, gender, hospital region, employment status, and shifts worked to identify potential confounding variables. Differences were examined using the chi-square test for categorical variables (e.g., gender) and t-test for continuous variables (e.g. age).
Descriptive statistics were used to characterize the sample regarding its demographic and occupational characteristics. To describe nurses’ perceptions of role conflict by professional designation in the three primary areas of practice (first research objective), we computed the mean and standard deviation of the Role Conflict Scale as well as the score of each individual item separately for RNs and RPNs in each primary area of practice (emergency department, medical unit, and surgical unit). To compare nurses’ perceptions of role conflict by professional designation in the three primary areas of practice (second research objective), we planned to perform either an independent t-test or an analysis of covariance (ANCOVA) if the preliminary analyses indicated the need to control for nurses’ age, gender, hospital region, employment status, and shifts worked. The five-point Likert Role Conflict Scale was considered a continuous variable similar to other researchers (; ; ; ; ; ) and analyzed the total scale score of the Role Conflict Scale as well as each individual item for separately for RNs and RPNs in each primary area of practice. Similar to other studies (), the latter was performed to better understand where RNs and RPNs in each area of practice differed in their perceptions of role conflict.
The effect size (Cohen’s d) was estimated to determine the magnitude of the differences in the mean scores for the Role Conflict Scale and its individual items, between the RN and the RPN groups. Effect sizes ranging from 0.2 to 0.3 indicated a small, 0.3 to 0.6 medium and >0.6 large between-group differences (). All analyses, other than effect sizes, were performed using SPSS PC, version 24.0 (). Effect sizes were estimated using ‘effsize’ () package developed in the R language ().
Results
Preliminary results
Preliminary analysis of the total Role Conflict Scale score and the item scores identified no violations of the statistical assumptions of the planned inferential tests. The assumption of homogeneity was met for the main effects of role conflict total scale score of the Role Conflict Scale and each individual item. As such, use of the planned parametric statistics was supported.
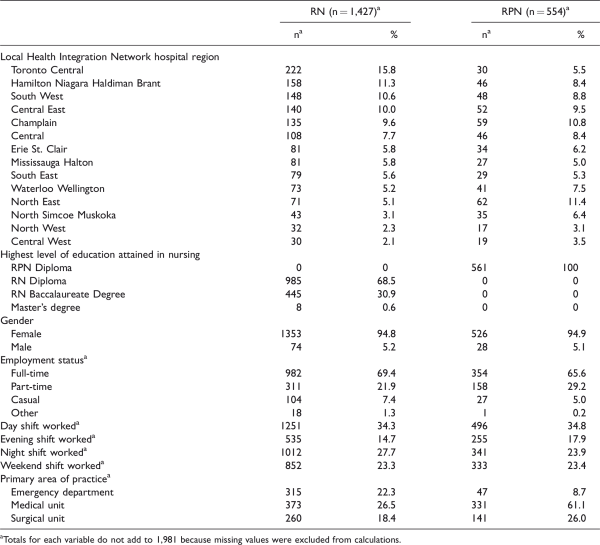
There were statistically significant differences between nurses’ hospital region (N = 1,946 df = 13, Χ2 = 79.5, p < 0.01). Most RNs worked in the Toronto Central (n = 222; 15.8%) whereas most RPNs worked in the North East (n = 62; 11.4%). There were also statistically significant differences between nurses’ employment status (N = 1,955 df = 3, Χ2 = 17.5, p < 0.01) with more RNs (n = 982; 69.4%) working full-time than RPNs (n = 354; 65.6%). Lastly, there were statistically significant differences between RNs and RPNs in terms of evening (N = 790 df = 1 Χ2 = 11.6, p < 0.01) and night shifts (N = 1,353 df = 1, Χ2 = 16.8, p < 0.01) worked. Among RNs, 14.7% (n = 535) worked evening shifts and 27.7% (n = 1,012) worked night shifts. Among RPNs, 17.9% (n = 255) worked evening shifts and 23.9% (n = 341) worked night shifts. There were no statistically significance differences between RNs and RPNs for age (t(1,947) = 0.06, p = 0.95), gender (N = 1,981 df = 1, Χ2 = 0.01, p = 0.91), day shift worked (N = 1,747 df = 1, Χ2 = 0.79, p = 0.37), or weekend shift worked (N = 1,185 df = 1, Χ2 = 0.004, p = 0.95).
Descriptive results of RN and RPN demographic and occupational characteristics
A total of 1,981 participants (RN = 1,427, RPN = 554) met this study’s eligibility criteria and provided data, representing 98.8% of the sample from the larger database. The completion rate for this current study was 99.4%. The mean ages of RNs and RPNs were comparable at 45.6 years (SD ± 10.5) and 45.6 years (SD ± 11.6), respectively (Table 1). A diploma was the highest level of education attained in nursing for the majority of RNs (68.5%) and RPNs (100%).
Comparison of RNs’ and RPNs’ perceived role conflict by total role conflict scale scores in each primary area of practice
An ANCOVA was used to compare level of overall role conflict (i.e., total scale score) as perceived by RNs and RPNs within each primary area of practice (emergency department, medical unit and surgical unit), controlling for hospital region, employment status and evening and night shifts worked; these variables showed significant differences by professional designation. RNs’ total mean scores on the role conflict scale were higher than those of RPNs, in the three primary areas of practice (Table 2).
Comparison of RNs’ and RPNs’ perceived role conflict by individual scale item scores in each primary area of practice
An ANCOVA was performed to compare the level of role conflict perceived by RNs and RPNs in each of the three primary areas of practice (emergency department, medical unit, and surgical unit). In this analysis, we also controlled for hospital region, employment status and evening and night shifts worked.
At the item level (Table 2), there were statistically significant differences, of negligible to small magnitude, between RNs and RPNs on medical units on three items of the Role Conflict Scale; these items reflected having to buck/bend the rules to carry out an assignment, receiving an assignment without adequate resources, and working on unnecessary things. The item scores were higher for RNs than RPNs, indicating that the average RN on medical units perceived a higher level of role conflict on these three items than the average RPN on medical units.
For the surgical area of practice, there were statistically significant differences, of negligible to small magnitude, between RNs and RPNs on the following three items: receiving an assignment without the manpower to complete it, having to buck/bend a rule or policy in order to carry out an assignment, and working on unnecessary things. The item scores were higher for RNs than RPNs, indicating that the average RN on surgical units perceived a higher level of role conflict on these three items than the average RPN on surgical units.
For the emergency department, there were significant between-group differences, of medium magnitude, across four items: receiving an assignment without the manpower to complete it, receiving incompatible requests from two or more people, receiving an assignment without adequate resources and materials to execute it, and working on unnecessary things. The item scores were higher for RNs than RPNs, indicating that the average RN in emergency departments perceived a higher level of role conflict on these items than the average RPN in emergency departments.
Discussion
To our knowledge, this is the first study to use a randomly selected sample to describe and compare acute care RNs’ and RPNs’ perceptions of role conflict. The sample mean age and gender are comparable to those of nurses in Ontario but slightly higher than the national average of 47.6 for RNs and 44.6 for RPNs ().
The study identified that RNs and RPNs in general reported medium levels of perceived role conflict, reflected by scores slightly below the scale midpoint with the exeption of RNs practicing in emergency departments whose scores were slightly above the scale midpoint. Our findings are similar to those included in an integrative review reporting that RNs and RPNs report experiencing role conflict (Kusi‐Appiah et al., 2018). The few studies that included RPNs did not exclusively examine acute care RNs’ and RPNs’ perceptions but rather included RNs and RPNs with unregulated healthcare providers, clerical workers, educators and administrators in the same Ontario sample () and acute care hospitals with long-term and community care settings across Canada (). Other studies administered items asking respondents to indicate the extent to which the role of the RPN was clear, not how RPNs themselves perceived their own roles (). By surveying a random sample of acute care RNs and RPNs that was representative of the target population of Ontario staff nurses on demographic variables (; Ontario Ministry of Health & Long-Term Care, 2014), this study overcomes the generalizability limitations of prior research, which tended to rely on non-probability samples and to not administer validated measures of role conflict.
Our study identified that the mean scores on the Role Conflict Scale and its individual items were generally higher for RNs than RPNs employed in medical and surgical primary areas of practice. Although differences were negligible to medium in magnitude, RNs practicing on medical and surgical units perceived higher levels of role conflict than RPNs practicing on medical and surgical units on the individual items inquiring about the extent to which they work on unnecessary things and having to buck/bend a rule or policy in order to carry out an assignment. RNs practicing on medical units additionally reported more role conflict than RPNs on the individual item inquiring about receiving an assignment without adequate resources and materials to execute it, although the effect size was negligible. RNs on medical units would be responsible for more acutely ill patients than would be RPNs as well as being responsible for providing leadership for the entire nursing team, which could include unregulated providers such as care aides (). This means that RNs may be required to complete nursing tasks for RPNs’ patients, or even assume full responsibility of RPNs’ patients who become unstable, in addition to managing their own patient assignment (which includes the most acutely ill patients). British Columbia study suggested that RNs perceived that RPNs did not always reciprocate them for the extra work they had to assume related to the RPNs’ unstable patient assignment. Thus, it is conceivable that RNs may have perceived that they had received an additional assignments without the human resources to complete it.
The mean scores on the role conflict scale and its individual items were consistently higher for RNs than RPNs practicing in the emergency department, indicating that RNs reported more role conflict than RPNs. Statistically significant between-group differences were all small to medium in magnitude. Compared to RPNs practicing in emergency departments, RNs practicing in emergency departments reported more role conflict on the individual items inquiring about the extent to which they receive an assignment without the manpower to complete it; receive incompatible requests from two or more people; receive an assignment without adequate resources and materials to execute it; and work on unnecessary things. Emergency departments are high stress, fast-paced, unpredictable work environments (). Patients admitted to the emergency department vary in levels of acuity. Most patients who visit the emergency department are not acutely ill or injured, do not require hospital care, and are not admitted to hospital (). Other patients are critically and seriously ill or injured and are admitted to hospital. RPNs work with stable patients and report a change in patient status and ask for direction from the RNs. It is likey that RNs would be assigned to care for more critically and seriously ill patients than RPNs () which might account for the between-group differences in perceived levels of role conflict. Therefore, RNs in emergency departments may be working with more acutely ill or injured patients and have increased responsibilities that may necessitate working with multiple groups who may operate differently. Also, with a more acutely ill and injured patient care assignment, RNs may perceive that they do not have the adequate human and material resources to carry out their assignments.
As well, RNs in all areas of practice are expected to be the leader of the nursing team. Leadership tasks include overseeing the evolving acuity of the unit, communicating unit workload to the team and delegating tasks accordingly. The need for leadership skills has become more necessary due to the increasing shifting of work from more educated workers to less educated workers related to cost containment initiatives (). Although further research is needed, it is possible that RNs in this study may not have been formally prepared to fully assume a leadership role given that most had a diploma level of education.
It is also possible that the expectations of the leadership role may place RNs at risk of experiencing higher levels of role conflict than RPNs. These leadership expectations, and increased patient acutiy can occur simultaneously leading RNs to experience competing demands.
This findings of this study have implications for administrators who can develop strategies to address the sources of conflict, tailored to the needs of RNs and RPNs in the different areas of practice. For example, managers may use the items of the Role Conflict Scale to help foster communication surrounding roles that could help team members understand their own and one another’s sources of role conflict. Managers could help team members understand one another’s roles and the necessity of reciprocity in tasks tailored to the unit setting, thereby supporting nurses in managing role conflict. For example, if an RN is required to perform an acute intervention for an RPN’s patient, the RPN could complete less acute tasks for the RNs’ patients.
Managers could also foster communication about the unit workload and how all members of the healthcare team could support one another. For example, if the RN has many competing demands and was able to explain this to other team members, requests for assistatnce with less acute tasks would be understood. Other professionals who understand the nursing workflow and RNs competing demands could structure their work with patients in ways that supported both patients and RNs. Nurses could also learn to explain their competing demands in the moment and suggest a time when they would be available or other nursing team members who might be available to assist other professionals.
The study has some limitations. We recognize that while the study has identified differences in role conflict between RNs and RPNs, the study does not explain why these differences exist. Future qualitative studies are needed to better understand why these differences exist between RNs and RPNs. The generalizability of the study findings outside of Ontario is limited. Future research is needed to validate the findings of this study in other jurisdictions.
Conclusions
This study identified that RNs and RPNs experience a medium level of role conflict with RNs experiencing higher levels of role conflict in all three areas of practice. The largest differences noted between RNs and RPNs were found in the emergency department and the effect sizes were negligible to medium in magnitude. The findings from this study may provide information for administators to address sources of role conflict.
Authors’ contributions All authors substantially contributed to the conception of the work and the interpretation of the data. Furthermore, all authors substantially contributed to the drafting and revising of the work. All authors are in agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy and integrity of any part of the work are appropriately investigated and resolved. All authors approve of the final version to be published.
Consent for publication We have received consent from all participants for publication.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Ontario Ministry of Health and Long-term Care (Grant: 06651), the Ontario Ministry of Research and Innovation, and York University. Dr. Souraya Sidani’s contribution was supported by Canadian Institutes of Health Research.
ORCID iDs Behdin Nowrouzi-Kia https://orcid.org/0000-0002-5586-4282 Mary Fox https://orcid.org/0000-0003-0572-3892
ORCID iDs Souraya Sidani https://orcid.org/0000-0002-9115-2389
ORCID iDs Sherry Dahlke https://orcid.org/0000-0001-6599-3101
References
- Bacharach S. B., Bamberger P., Conley S. C. (1990). Work processes, role conflict, and role overload: The case of nurses and engineers in the public sector. Work and Occupations, 17(2), 199–228.
- Creswick N., Westbrook J. I., Braithwaite J. (2009). Understanding communication networks in the emergency department. BMC Health Services Research, 9(1), 1–9.
- Dahlke S., Baumbusch J. (2015). Nursing teams caring for hospitalised older adults. Journal of Clinical Nursing, 24(21–22), 3177–3185. https://doi.org/10.1111.jocn.12961
- Ferguson C. J. (2009). An effect size primer: A guide for clinicians and researchers. Professional Psychology: Research and Practice, 40(5), 532–538.
- Fox M. T., Butler J. I., Persaud M., Tregunno D., Sidani S., McCague H. (2016). A multi‐method study of the geriatric learning needs of acute care hospital nurses in Ontario, Canada. Research in Nursing & Health, 39(1), 66–76.
- Fox M. T., Sidani S., Butler J. I., Tregunno D. (2017). Nurses’ perspectives on the geriatric nursing practice environment and the quality of older people’s care in Ontario acute care hospitals. Canadian Journal of Nursing Research, 49(2), 94–100.
- González-Romá V., Lloret S. (1998). Construct validity of Rizzo et al.’s (1970) Role Conflict and Ambiguity Scales: A multisample study. Applied Psychology: An International Review, 47(4), 535–545.
- Hercelinskyj G., Cruickshank M., Brown P., Phillips B. (2014). Perceptions from the front line: Professional identity in mental health nursing. International Journal of Mental Health Nursing, 23(1), 24–32.
- House R., Rizzo J. (1972). Role conflict and ambiguity as critical variables in a model of organizational behavior. Organizational Behavior and Human Performance, 7(3), 467–505.
- IBM Corporation. (2016). SPSS for Windows, version 24. IBM Corporation.
- Jackson S. E., Schuler R. S. (1985). A meta-analysis and conceptual critique of research on role ambiguity and role conflict in work settings. Organizational Behavior and Human Decision Processes, 36(1), 16–78.
- Kahn RL, Wolfe DM, Quinn RP, et al. Occupational stress: Studies in role conflict and ambiguity. New York: Wiley, 1964.
- Kang K. H., Lim Y. J. (2016). Influence of professionalism, role conflict and work environment in clinical nurses with expanded role on job embeddedness. Journal of Korean Academy of Nursing Administration, 22(5), 424–436.
- Katz D., Kahn R. L. (1978a). Organizations and the system concept. Classics of Organization Theory, 80, 480.
- Katz D., Kahn R. L. (1978b). The social psychology of organizations (Vol. 2). Wiley.
- Kelloway E. K., Barling J. (1990). Item content versus item wording: Disentangling role conflict and role ambiguity. Journal of Applied Psychology, 75(6), 738–742.
- Khan A., Yusoff R. B. M., Khan M. M., Yasir M., Khan F. (2014). Psychometric analysis of role conflict and ambiguity scales in academia. International Education Studies, 7(8), 104.
- Kusi‐Appiah E., Dahlke S., Stahlke S. (2018). Nursing care providers’ perceptions on their role contributions in patient care: An integrative review. Journal of Clinical Nursing, 27(21–22), 3830–3845.
- Lankshear S., Rush J., Weeres A., Martin D. (2016). Enhancing role clarity for the practical nurse: A leadership imperative. JONA: The Journal of Nursing Administration, 46(6), 300–307.
- Lu H., Barriball K. L., Zhang X., While A. E. (2012). Job satisfaction among hospital nurses revisited: A systematic review. International Journal of Nursing Studies, 49(8), 1017–1038.
- McGillis H. L., Doran D. (2007). Nurses’ perceptions of hospital work environments. Journal of Nursing Management, 15(3), 264–273.
- Nei D., Snyder L. A., Litwiller B. J. (2015). Promoting retention of nurses: A meta-analytic examination of causes of nurse turnover. Health Care Management Review, 40(3), 237–253.
- O'Brien‐Pallas L., Murphy G. T., Shamian J., Li X., Hayes L. J. (2010). Impact and determinants of nurse turnover: A pan‐Canadian study. Journal of Nursing Management, 18(8), 1073–1086.
- Piko B. F. (2006). Burnout, role conflict, job satisfaction and psychosocial health among Hungarian Health Care Staff: A questionnaire survey. International Journal of Nursing Studies, 43(3), 311–318.
- R Core Team. (2013). R: A language and environment for statistical computing.
- Reknes I., Einarsen S. V., Gjerstad J., Nielsen M. B. (2019). Dispositional affect as a moderator in the relationship between role conflict and exposure to bullying behaviors. Frontiers in Psychology, 10, 44.
- Schuler R. S. (1977). Role conflict and ambiguity as a function of the task—structure—technology interaction. Organizational Behavior and Human Performance, 20(1), 66–74.
- Sidani S., Manojlovich M., Doran D., Fox M., Covell C. L., Kelly H., Jeffs L., McAllister M. (2016). Nurses’ perceptions of interventions for the management of patient‐oriented outcomes: A key factor for evidence‐based practice. Worldviews on Evidence-Based Nursing, 13(1), 66–74.
- Spooner-Lane R., Patton W. (2007). Determinants of burnout among public hospital nurses. Australian Journal of Advanced Nursing, 25(1), 8.
- Stordeur S., D'hoore W., Vandenberghe C. (2001). Leadership, organizational stress, and emotional exhaustion among hospital nursing staff. Journal of Advanced Nursing, 35(4), 533–542.
- Stretton J. G., Currie B. K., Chauhan U. K. (2014). Inflammatory bowel disease nurses in Canada: An examination of Canadian gastroenterology nurses and their role in inflammatory bowel disease care. Canadian Journal of Gastroenterology and Hepatology, 28(2), 89–93.
- Taherdoost H. (2017). Determining sample size; how to calculate survey sample size. International Journal of Economics and Management Systems, 2, 237–239.
- Torchiano, M. (2016). effsize: efficient effect size computation (R package). Vienna: R Foundation for Statistical Computing. software.
- Tran D. T., Johnson M., Fernandez R., Jones S. (2010). A shared care model vs. a patient allocation model of nursing care delivery: Comparing nursing staff satisfaction and stress outcomes. International Journal of Nursing Practice, 16(2), 148–158.
- Tunc T., Kutanis R. O. (2009). Role conflict, role ambiguity, and burnout in nurses and physicians at a university hospital in Turkey. Nursing & Health Sciences, 11(4), 410–416.
- Uscher-Pines L., Pines J., Kellermann A., Gillen E., Mehrotra A. (2013). Deciding to visit the emergency department for non-urgent conditions: A systematic review of the literature. The American Journal of Managed Care, 19(1), 47.