Introduction
Interest in the use of blood flow restriction exercise blood flow restriction exercise during training is becoming more widespread among athletes, coaches, exercise practitioners, researchers and the general healthy population., The two primary features of blood flow restriction exercise are (1) the application of a tourniquet or inflatable cuff to the most proximal part of the exercising limb designed to moderate limb blood flow throughout the contraction cycle of working muscle groups and, (2) an exercising load that is typically of light-intensity (e.g. 20–40% of one repetition maximum for resistance exercise). The primary outcomes from training with these two features are gains in muscle strength and muscle size, as well as improved objective physical function that can approach levels observed with traditional heavy-load resistance training. In addition, there is a growing interest in endurance and aerobic capacity adaptations following blood flow restriction exercise training.,
There is, however, variability in the primarily observed adaptations of muscle growth, strength,– and physical function, with blood flow restriction exercise training. This variability has been suggested to be dependent on the cuff type and other characteristics by which the restriction to flow (i.e. pressure) is applied to the active limb., These include factors such as cuff width, absolute applied pressure, duration of the pressure application and the potential interaction of these factors with participant characteristics such as limb circumference, adiposity, blood pressure and fitness., In addition, the influence of these factors may vary depending on the nature of the exercise (e.g. aerobic vs resistance, duration and intensity).
Many early studies used relatively thin (<10 cm) cuffs and relatively high pressures that were seemingly arbitrary in their selection, and where a significant restriction to limb blood flow is expected. More recently, studies have adopted the use of relatively wider cuffs (>15 cm) combined with relatively lower pressures that are often determined in relation to an individualised metric such as systolic blood pressure or the measurement of total limb occlusion pressure., Individualised pressures are proposed to be more beneficial during blood flow restriction exercise by providing the practitioner with a safer, standardised and more justifiable approach to pressure selection.,,, However, one apparently significant difference between studies that have examined outcomes from blood flow restriction exercise training is whether the pressure application is achieved with the use of cuff pressure systems that attempt to regulate the applied blood flow restriction pressure (regulated systems) or systems that do not (unregulated systems). An unregulated cuff system applies a set pressure at rest prior to exercise and does not actively or dynamically adjust the set pressure throughout the range of motion of the limb. This results in variable pressure application as the applied pressure is calculated at rest and does not account for muscle contractions under the cuff. As such, this might result in greater peak pressures being applied during contractions than intended. In contrast, a regulated cuff system applies a set pressure at rest prior to exercise, and then continuously and actively adjusts the applied pressure to maintain a constant applied pressure throughout the range of motion of the limb, accounting for muscular contractions under the cuff.,
Therefore, the aim of this systematic review and meta-analysis was to examine (compare) the effect of regulated versus unregulated cuff pressure systems on the chronic adaptations to blood flow restriction exercise training interventions, with a specific focus on the gains in muscle strength, size and physical function as the primary outcomes of focus for blood flow restriction exercise training in both research and practice. This review also identifies observed adaptations for less commonly assessed blood flow restriction exercise training adaptations such as endurance and aerobic capacity. This important distinction will support practitioner's decision-making when selecting blood flow restriction systems to suit their needs, alongside other important considerations such as device quality, safety, cost and convenience.,
Methods
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) guidelines.
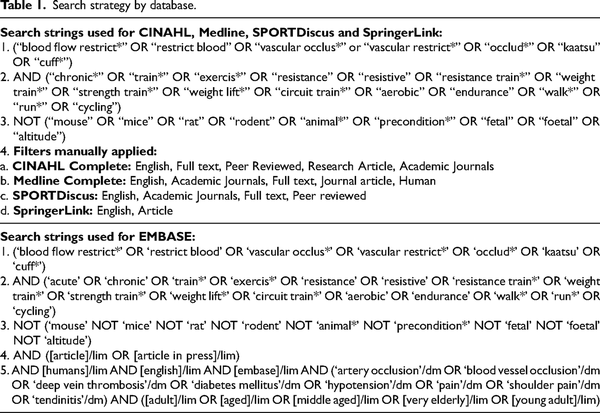
The electronic database search included using the tool EBSCOhost and other online database search engines. The search included Medline, SPORTDiscus, CINAHL, Embase and SpringerLink. Search terms were derived from ‘blood flow restriction’, ‘vascular occlusion’ and ‘chronic exercise’ (Table 1). Search results were filtered within the database where possible for the filters ‘Human’, ‘English’, ‘research article’ and/or ‘full text’. Search results included dates from inception until the date of the search (31 December 2023).
Participants, interventions and comparators
The database results were imported into Endnote X9. Duplicates were removed, and screening was completed by title and abstract and full text. The full text screening consisted of examining the details provided within the studies on the cuff pressure system (including brand), training interventions and population groups. Excluded articles were sorted in accordance with relevant inclusion and exclusion criteria noted in the PRISMA flow chart (Figure 1). This process was completed by two researchers independently (BM, MJC, SAW).
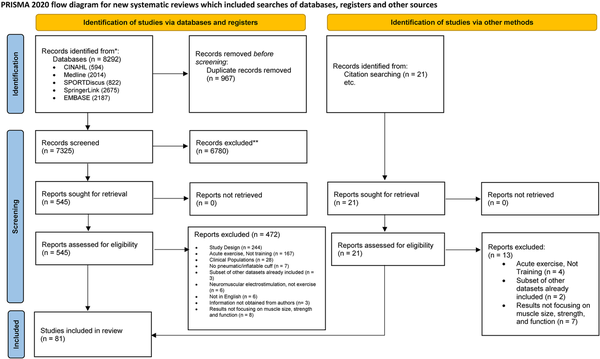
Figure 1
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart of study selection process.
The relevant inclusion criteria are identified below and reason for exclusion is noted in the PRISMA flow chart (Figure 1): The quality and risk of bias of included studies was independently evaluated by two reviewers (BM and MJC). The assessment criteria were determined by using the Cochrane Collaboration Risk of Bias 2.0 tool for individually randomised and parallel group trials. The overall quality assessment of the randomised control trials included analysing the selection bias which examined the method of recruitment for randomisation, concealment of treatment allocation and group baseline characteristics. Detection bias included blinding of participants and assessors for intervention groups. Attrition bias was determined by the level of adherence of participants, limitations and reasons for attrition. Each section of the risk of bias was assigned by rating high, low or unclear risk based on the results or the conclusions of the study.
Language: studies published in English were included in this review.
Study Design: studies that were published in a peer-reviewed journal. Systematic reviews, narrative reviews, conference abstracts, editorials, letters or publications not inclusive of original data were excluded.
Exercise component: exercise training interventions must have included chronic aerobic, resistance, combined or alternative types of progressive exercise training interventions over multiple weeks (greater than two weeks) in conjunction with blood flow restriction.
Age: subjects over the age of 18 years were included in this review.
Outcome measures: includes at least one of muscle strength, size and physical function.
Following the initial screening, information from the included studies was extracted including study design, study characteristics, participants’ age, sample size, cuff type and details, exercise training interventions, outcome measures and findings and details of the equipment used to apply blood flow restriction and assessments used. This was completed by at least two reviewers to ensure consensus of extracted data (BM, MJC, SAW).
Meta-analyses
Only 35 of the studies included in the broader systematic review were included in the meta-analyses.– Reasons for exclusion included study not having any of the measures examined in the meta-analyses, or studies had either no comparison group or the comparison group not being a non-blood flow restriction equivalent exercise. The measures assessed in the meta-analyses included repetition maximum muscle strength, muscle strength measured via dynamometry, muscle cross-sectional area and muscle anthropometry (thickness, volume, mass, etc.). Studies were included in the meta-analyses if they presented pre- and post-data for these measures for both a blood flow restriction intervention, and a non-blood flow restriction equivalent comparison group. All outcomes were treated as continuous data. The standardised mean differences between the blood flow restriction group and the non-blood flow restriction comparison's change data were calculated for each of the relevant measures. The resulting effect estimate was expressed as Hedge's g with 95% confidence intervals (95% CI). Leave-one-out meta-analyses were performed to investigate the influence of each study on the overall effect size estimate.
The outcomes were first assessed using random-effects meta-analyses. The significance of Cochrane's Q statistic was used to test for significant heterogeneity among treatment effects (P < 0.1). The percentage of heterogeneity across studies was then quantified using the I2 statistic. Analyses with an I2< 30% were considered to have low heterogeneity, I2 between 30% and 60% were considered to have moderate heterogeneity, and I2> 60% were considered to have high heterogeneity. Subgroup analyses were conducted by blood flow restriction pressure system (‘unregulated’ or ‘regulated’) for each outcome measure to compare the outcomes from studies using different blood flow restriction pressure systems. Funnel plots were used to examine potential publication bias of the included studies for each measure via visual inspection in addition to calculating the P-value of Egger's test.
Results
A total of 8292 articles were retrieved from database searches as follows: Medline (2014), SPORTDiscus (822), CINAHL (594), Embase (2187) and SpringerLink (2675). An additional 21 studies that fulfilled the inclusion criteria were identified from the reference lists of prior reviews related to the topic of blood flow restriction exercise. The studies were approved for inclusion among the original search results.
Upon the removal of duplicates 7325 articles were left to be screened by title and abstract. Of these results 6780 were excluded based on the title or abstract and the full text of the remaining 545 articles were evaluated using the inclusion and exclusion criteria. Articles removed are outlined in the PRISMA flow chart (Figure 1). Subsequently, a total of 81 articles were included for this review.
Information extracted from studies included in this review is summarised in the table of included studies (see supplementary data, Table 1). This includes details of the study design, sample size and participants, intervention, main findings and details of the blood flow restriction pressure system used in each study. Of the 81 studies included, 56 were randomised controlled trials,–,–,,,,,–,–,–,– while 25 were non-randomised controlled trials.,,–,–,,,,,– Within individual studies the number of participants ranged from 5 to 60, participants ranged in age from 18 years to 83 years, and participant sex was exclusively male in 33 studies, exclusively female in 12 studies, and a mix of males and females in 36 studies. Intervention duration ranged from 12 days to 12 weeks. The primary intervention was resistance training in 64 studies. Other interventions used were walking training (n = 8 studies), cycling training (n = 2 studies) and individual studies that used different interventions such as training using step-ups, sets of sit-to-stand exercise to failure, vertical jumping, hydrotherapy, Futsal and running.
Thirty-four (n = 34) of the included studies employed an unregulated blood flow restriction system to apply the blood flow restriction pressure throughout the intervention.–,,,,,,–,,,,,,,,,,,,,,,,–, These studies used cuff widths ranging from 5.5 to 20.5 cm and an applied blood flow restriction pressure between 96 and 350 mmHg. For those studies that measured arterial occlusion pressure, these used individualised blood flow restriction pressures between 30% and 80% arterial occlusion pressure. Two studies, used a blood pressure-based method to apply an individualised blood flow restriction pressure of 70% systolic blood pressure and 110% systolic blood pressure.
In contrast, n = 47 of the included studies employed a regulated blood flow restriction pressure system to apply the blood flow restriction pressure during the exercise intervention.–,–,–,,,,,–,,,–,,,,,,,,,,,–,,,–,–, These studies used cuff widths ranging from 2.5 to 18.5 cm and an applied blood flow restriction pressure between 71 and 270 mmHg. For those studies that measured arterial occlusion pressure, these used individualised blood flow restriction pressures between 40% and 90% arterial occlusion pressure. Three studies used a blood pressure-based method to apply an individualised blood flow restriction pressure between 130% and 144% systolic blood pressure.
Risk of bias is detailed for all included studies (Figure 2). When examining the studies overall, there was low risk of bias for random sequence generation for 93% of included studies, allocation concealment for 28% of included studies, 7% of studies for blinding of patients and personnel (an inherent limitation commonly acknowledged in training studies), 11% for blinding of outcome assessment, 70% for incomplete data and 91% for selective outcome reporting, as well as 100% for other sources of bias. Only five studies were rated as low risk in all categories.,,,, The overall results indicated a predominately low-to-moderate risk of bias, that did not prohibit or undermine the discussion points within the present review, it simply highlights the general methodological quality in blood flow restriction exercise studies and some areas where reporting could be clarified.
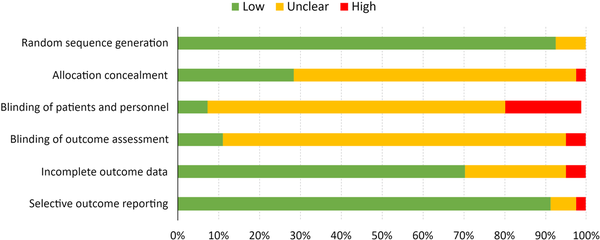
Figure 2
Risk of bias assessment for included studies evaluating training adaptations to blood flow restricted exercise.
Repetition maximum muscle strength was measured in a total of 45 studies. Typically (n = 41), this was via 1-repetition maximum,–,–,–,,,,,,,–,,,,,,–,,,,,,,,,, whereas other studies (n = 5) estimated strength using protocols ranging from 3-repetition maximum to 20-repetition maximum.,,,, Blood flow restriction interventions significantly increased repetition maximum muscle strength in 38 studies,,,–,–,–,,,,,,,,,–,,,,,,,,,,, remaining unchanged in three studies,,, while mixed results were recorded within four studies where some measures of repetition maximum muscle strength increased and others remained unchanged.,,, Of those studies that showed significant increases in repetition maximum muscle strength in response to the blood flow restriction intervention (n = 42 in total), regulated blood flow restriction pressure systems (n = 27 studies) showed repetition maximum muscle strength to increase between 3% and 32%,–,–,–,,,,,,,,,,,,,,,,,, while unregulated blood flow restriction pressure systems (n = 15) showed repetition maximum muscle strength to increase between 6% and 55%.–,,,,,,,,,,,,
Muscle strength through dynamometry was measured in a total of 44 studies. The majority (n = 40) used isometric dynamometry,,,,,,,,–,,,–,,,,,,,–,,,,,–,,–,,, whereas eight studies (n = 9) examined muscle strength using isokinetic dynamometry.,,,,,,,, One study measured anaerobic muscle performance via a Wingate anaerobic cycling test. Blood flow restriction interventions significantly increased muscle strength in 21 studies,,,,,,,,,,,,,,,,,,,,, while remaining unchanged in 13 studies,,,,,,,,,,,,, with mixed results being recorded in 11 studies where some measures of muscle strength increased and others remained unchanged.,,,,,,,,,, Of those studies that showed significant increases in muscle strength via dynamometry in response to the blood flow restriction intervention (n = 32 in total), regulated blood flow restriction pressure systems (n = 21 studies) showed muscle strength to increase between 4% and 49%,,,,,,,,,,,,,,,,,,,,, while unregulated blood flow restriction pressure systems (n = 11 studies) showed muscle strength to increase between 7% and 139%.,,,,,,,,,,
Muscle cross-sectional area was measured in a total of 34 studies. Training interventions included walking (n = 5),,,,, ergometer cycling (n = 1) and concurrent aerobic and resistance training (n = 1), but the most common intervention was resistance training (n = 27).,,,,–,,,,,,,,–,,,,,,,– Far more studies examined cross-sectional area following interventions using regulated blood flow restriction pressure systems (n = 24),,,,,,,,,,,,,,,,,,,,,– than unregulated blood flow restriction pressure systems (n = 10).,,,,,,,,, blood flow restriction interventions significantly increased muscle cross-sectional area in 29 studies,,,,,,,,,,,,,,,,,,–,,,,,,,,, remaining unchanged in three studies,,, with mixed results being recorded in two studies where some measures of muscle cross-sectional area increased and some remained unchanged., Of those studies that showed significant increases in muscle cross-sectional area in response to the blood flow restriction intervention (n = 31 in total), regulated blood flow restriction pressure systems (n = 21 studies) showed muscle cross-sectional area to increase between 2% and 24%,,,,,,,,,,,,,,,,,,,– while unregulated blood flow restriction pressure systems (n = 10 studies) showed muscle cross-sectional area to increase between 2% and 23%.,,,,,,,,,
Muscle anthropometry was measured in a total of 30 studies. The majority (n = 23) measured muscle volume (n = 12),–,,,,,,,, or muscle thickness (n = 11),–,,,,,,,, with others examining measures of muscle mass (n = 4),,, or limb circumference (n = 5).,,,, Far more studies examined muscle anthropometry following interventions using regulated blood flow restriction pressure systems (n = 23),,–,–,,,,,,,,,,,,,,, than unregulated blood flow restriction pressure systems (n = 7).,,,,,, Blood flow restriction interventions significantly increased muscle anthropometry in 23 studies,,–,–,,,,,,,,,,,,,, remaining unchanged in four studies,,,, with mixed results being recorded in three studies where some measures of muscle anthropometry increased and some remained unchanged.,, Of those studies that showed significant increases in muscle anthropometry in response to the blood flow restriction intervention (n = 26 in total), regulated blood flow restriction pressure systems (n = 20 studies) showed muscle anthropometry to increase between 2% and 18%,,,–,–,,,,,,,,,,,, while unregulated blood flow restriction pressure systems (n = 6 studies) showed muscle anthropometry to increase between 1% and 13%.,,,,,
Endurance outcomes were measured in a total of 13 studies. The majority (n = 10) measured repetitions completed during an exhaustive test,,,,,,,,,, while three (n = 3) used a test of time to exhaustion.,, Eight studies examined endurance following interventions using regulated blood flow restriction pressure systems (n = 6),,,,,,,, while five used unregulated blood flow restriction pressure systems (n = 4).,,,, Blood flow restriction interventions significantly increased endurance in 11 studies,,,,,,,,,, and remained unchanged in two studies., Of those studies that showed significant increases in endurance in response to the blood flow restriction intervention (n = 11 in total), regulated blood flow restriction pressure systems (n = 7 studies) showed endurance to increase between 19% and 140%,,,,,,, while unregulated blood flow restriction pressure systems (n = 4 studies) showed endurance to increase between 28% and 70%.,,,
Aerobic capacity was measured in a total of eight studies.,,,–,, All used measures of peak or maximal oxygen consumption. Five studies examined endurance following interventions using regulated blood flow restriction pressure systems (n = 5),,,,, while three used unregulated blood flow restriction pressure systems (n = 3).,, Blood flow restriction interventions significantly increased aerobic capacity in three studies,,, remaining unchanged in five studies.,,,, Of those studies that showed a significant increases in endurance in response to the blood flow restriction intervention (n = 3 in total), regulated blood flow restriction pressure systems (n = 2 studies) showed aerobic capacity to increase between 5% and 12%,, while the one study that used an unregulated blood flow restriction pressure system showed aerobic capacity to increase by 10%.
Physical function was measured in a total of 15 studies.,,,,,,,,,,,,,, These used a quite diverse range of tests and test batteries such as the six-minute walk test, sit-to-stand tests, timed Up-and-Go tests, short physical performance batteries and tests of balance, agility and hop/jump performance. Seven studies examined physical function following interventions using regulated blood flow restriction pressure systems (n = 7),,,,,,, while eight used unregulated blood flow restriction pressure systems (n = 8).,,,,,,, Blood flow restriction interventions significantly increased physical function in eight studies,,,,,,,, remaining unchanged in three studies,,, with mixed results being recorded in four studies where some measures of physical function increased and some remained unchanged.,,, Of those studies that showed significant increases in physical function in response to the blood flow restriction intervention (n = 12 in total), regulated blood flow restriction pressure systems (n = 6 studies) showed improvements to physical function between 5% and 24%,,,,,, while unregulated blood flow restriction pressure systems (n = 6 studies) showed improvements to physical function between 6% and 83%.,,,,,
While beyond the scope of this review, 16 studies measured other adaptations besides muscle strength, muscle size or objective physical function.,,,,,,–,,,,,,, These examined a quite diverse range of parameters focused on haemodynamics (e.g. blood pressures, vascular compliance, etc) and circulating hormones/metabolites (e.g. testosterone, immunoglobulins, myoglobin, creatine kinase, etc). Most of these studies examined adaptations following interventions using regulated blood flow restriction pressure systems (n = 14),,,,,–,,,,,,, while two studies used unregulated blood flow restriction pressure systems.,
Meta-analyses
Collectively, all the meta-analyses showed negligible to small effect sizes in favour of blood flow restriction exercise compared to non-blood flow restriction equivalent exercise (Figures 3–6). Small effect sizes (ES) were observed for repetition maximum muscle strength [ES = 0.27, 95% CI (0.13, 0.40)] with high heterogeneity across studies (Q = 38.77, P < 0.01, I2= 63.34%). This was also true for muscle cross-sectional area [ES = 0.27, 95% CI (0.09, 0.45)] with high heterogeneity (Q = 50.21, P < 0.01, I2= 77.86%). The negligible effects were observed for muscle strength via dynamometry [ES = 0.13, 95% CI (0.07, 0.19)] and muscle anthropometry [ES = 0.03, 95% CI (−0.03, 0.10)]. Heterogeneity was low for both muscle strength via dynamometry (Q = 13.34, P = 0.82, I2= 0%) and muscle anthropometry (Q = 6.29, P = 0.97, I2= 0%). The leave-one-out sensitivity analyses showed no studies had an adversely large impact on any of the estimated effect sizes (see supplementary data, Tables 2–5).
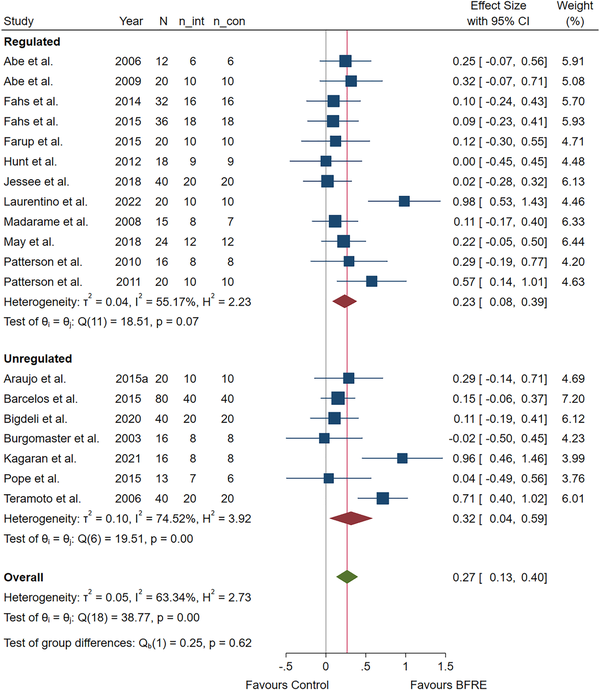
Figure 3
Forest plot of the effect estimates (ES) with 95% confidence intervals (CI) for repetition maximum muscle strength testing following blood flow restricted exercise training compared with non-blood flow restricted equivalent exercise training with subgroup analysis by regulated and unregulated cuff systems.
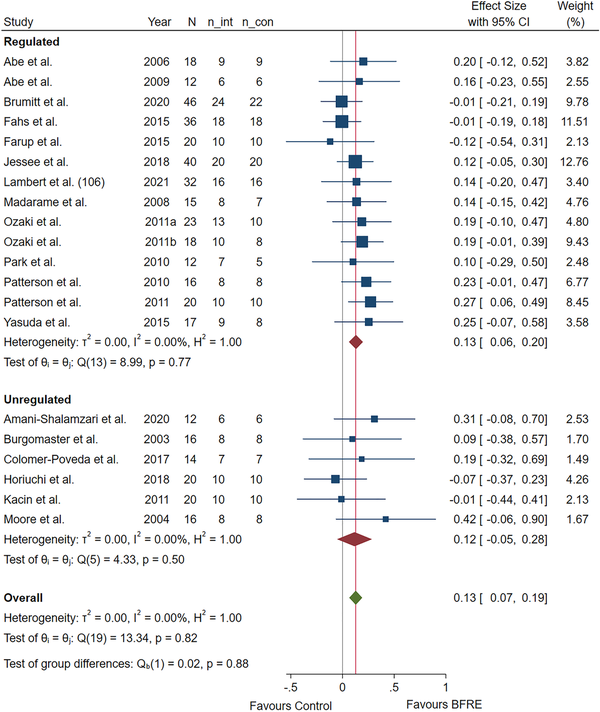
Figure 4
Forest plot of the effect estimates (ES) with 95% confidence intervals (CI) for muscle strength via dynamometry following blood flow restricted exercise training compared with non-blood flow restricted equivalent exercise training with subgroup analysis by regulated and unregulated cuff systems.
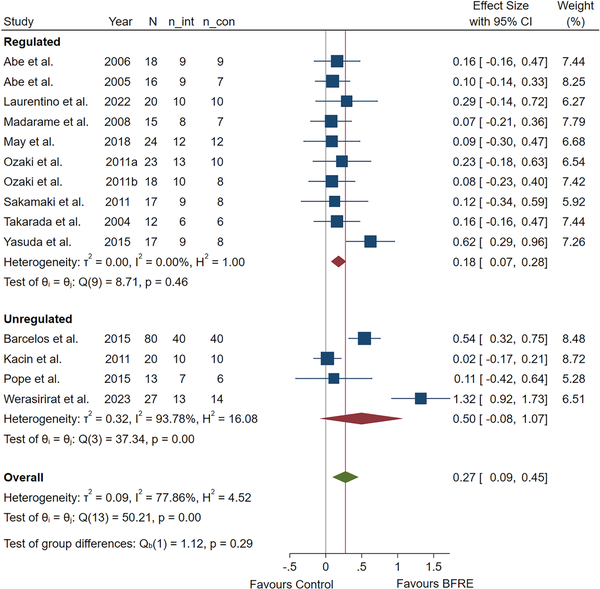
Figure 5
Forest plot of the effect estimates (ES) with 95% confidence intervals (CI) for muscle cross-sectional area following blood flow restricted exercise training compared with non-blood flow restricted equivalent exercise training with subgroup analysis by regulated and unregulated cuff systems.
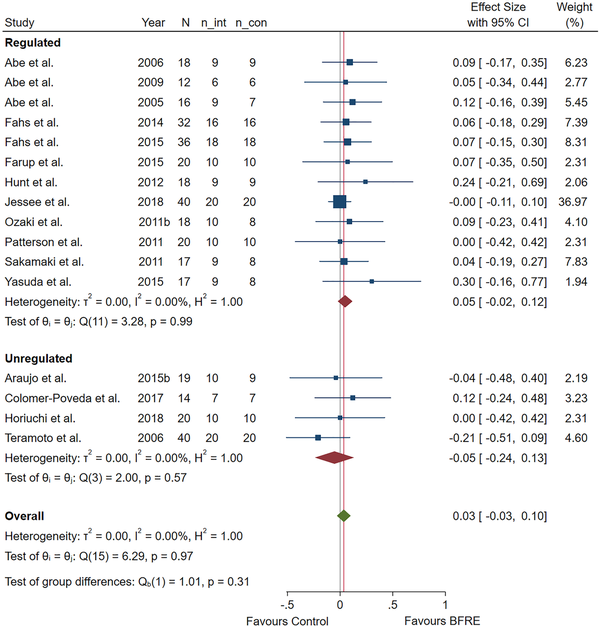
Figure 6
Forest plot of the effect estimates (ES) with 95% confidence intervals (CI) for muscle anthropometry following blood flow restricted exercise training compared with non-blood flow restricted equivalent exercise training with subgroup analysis by regulated and unregulated cuff systems.
When specifically examining the sub-group analyses contrasting unregulated and regulated blood flow restriction pressure systems (Figures 3–6), this remains largely unchanged. For repetition maximum muscle strength, unregulated blood flow restriction pressure systems [ES = 0.32, 95% CI (0.04, 0.59); heterogeneity (Q = 19.51, P < 0.01, I2= 74.52%)] and regulated blood flow restriction pressure systems [ES = 0.23, 95% CI (0.08, 0.39); heterogeneity (Q = 18.51, P = 0.07, I2= 55.17%)] were not significantly different (P = 0.62), with both groups displaying moderate-to-high heterogeneity. For muscle strength via dynamometry, unregulated blood flow restriction pressure systems [ES = 0.12, 95% CI (−0.05, 0.28); heterogeneity (Q = 4.33, P = 0.50, I2= 0%)] and regulated blood flow restriction pressure systems [ES = 0.13, 95% CI (0.06, 0.20); heterogeneity (Q = 8.99, P = 0.77, I2= 0%)] were not significantly different (P = 0.88). For muscle cross-sectional area, unregulated blood flow restriction pressure systems [ES = 0.50, 95% CI (−0.08, 1.07); heterogeneity (Q = 37.34, P < 0.01, I2= 93.78%)] and regulated blood flow restriction pressure systems [ES = 0.18, 95% CI (0.07, 0.28); heterogeneity (Q = 8.71, P = 0.46, I2= 0%)] were not significantly different (P = 0.29), although the unregulated group showed very high heterogeneity. For muscle anthropometry, unregulated blood flow restriction pressure systems [ES = −0.05, 95% CI (−0.24, 0.13); heterogeneity (Q = 2, P = 0.57, I2= 0%)] and regulated blood flow restriction pressure systems [ES = 0.05, 95% CI (−0.02, 0.12); heterogeneity (Q = 3.28, P = 0.99, I2= 0%)] were not significantly different (P = 0.31).
The funnel plots showed minor asymmetries present for all meta-analyses (see supplementary data, Figures 1–4). The standard error of the effect sizes fell outside the pseudo 95% CI for three studies for repetition maximum muscle strength,, and four studies for muscle cross-sectional area.,,, Egger's test showed no evidence for the presence of publication bias for any of the meta-analyses (repetition maximum muscle strength: z = 1.28, P = 0.20; strength dynamometry: z = 0.58, P = 0.56; muscle cross-sectional area: z = 0.52, P = 0.60; muscle volume and thickness: z = 1.49, P = 0.14).
Discussion
Commonly, blood flow restriction exercise training primarily targets gains in muscle strength, muscle size and objective physical function. However, no study has directly compared these outcomes following training with different blood flow restriction cuff pressure systems (i.e. regulated vs unregulated). Therefore, we approached this question using a systematic review and meta-analysis. The main findings show that outcomes from blood flow restriction exercise training are not different between participants training with regulated vs unregulated blood flow restriction cuff pressure systems.
The present systematic review showed blood flow restriction exercise training to significantly improve outcomes related to muscle strength (85% of studies using repetition maximum methods; 71% of studies using dynamometry), muscle size (90% of studies using cross-sectional area or anthropometry) and objective physical function (77% of studies). While significantly fewer studies examined endurance (n = 13) and aerobic capacity (n = 8), blood flow restriction exercise training also significantly improved outcomes related to endurance (92% of studies) and aerobic capacity (38% of studies). Moreover, all these outcomes appeared unaffected by whether the applied restriction to flow during the blood flow restriction exercise undertaken across the training programme was achieved using a regulated or unregulated blood flow restriction cuff pressure system. In addition, the magnitude of change for each outcome measure (e.g. strength, size, physical function, etc) was broadly similar for both regulated and unregulated blood flow restriction cuff pressure systems.
The present meta-analysis more specifically reinforced the outcomes from the systematic review. Blood flow restriction exercise training favoured significant gains in muscle strength and muscle size with effect sizes clustered around the ‘small’ range. Again, these improvements are similar for both regulated and unregulated blood flow restriction cuff pressure systems. Therefore, this systematic review and meta-analysis demonstrate that blood flow restriction exercise training achieves broadly similar outcomes for end-users independent of whether a regulated or unregulated blood flow restriction cuff pressure system is employed. In addition, these outcomes from blood flow restriction exercise training align with other similar recent reviews., This information should assist practitioners to make informed choices when selecting blood flow restriction cuff pressure systems appropriate to their needs of use (e.g. environment, clientele, cost, etc).
Despite similar outcomes from both regulated and unregulated blood flow restriction cuff pressure systems, there are likely additional considerations for practitioners when making choices about a pressure system that suits their needs and clientele. Given outcomes from blood flow restriction exercise training are likely dependent on the complex interactions between prescription variables (e.g. cuff width, cuff pressure), participant variables (e.g. age, fitness) and exercise characteristics (e.g. mode, intensity, repetition scheme, aerobic vs resistance), the considerations facing practitioners in choosing a suitable device may be broadly categorised across areas of device quality, safety and comfort, cost and convenience.,
The quality of different unregulated blood flow restriction cuff pressure systems should be relatively similar. These systems lock the set applied blood flow restriction pressure at rest prior to exercise, without this pressure being dynamically adjusted throughout the exercise bout. It is typical for studies using these systems to simply use a sphygmomanometer or something similar (see supplementary data, Table 1). In contrast, the quality of regulated blood flow restriction cuff pressure systems may be more variable. Indeed, recent evidence suggests that the autoregulation capability of different regulated blood flow restriction cuff pressure systems is variable with respect to the accuracy and speed by which the target pressure (applied blood flow restriction pressure) is maintained throughout the phases of contraction during exercise. In addition, most regulated blood flow restriction cuff pressure systems contain features to determine limb occlusion pressure that allow for prescription of an individualised applied blood flow restriction pressure. However, again the quality of these features vary between systems, with some recent evidence demonstrating one system to reliably assess limb occlusion pressure in the upper limbs, but not lower limbs.
It is accepted that blood flow restriction is safe when applied using recommended prescription guidelines, regardless of whether blood flow restriction pressure systems are regulated or unregulated. However, existing guidelines recommend the use of an individualised applied blood flow restriction pressure. In part, the intention is to moderate the magnitude of the applied blood flow restriction pressure, thereby minimising cardiovascular system stress during blood flow restriction exercise to reduce risk and incidence of adverse events. In addition, higher blood flow restriction pressures are more uncomfortable for participants/clients undertaking blood flow restriction exercise., Therefore, an additional reason to individualise the applied blood flow restriction pressure is to reduce the perceptual difficulty for participants/clients and, therefore, to improve compliance. While the perceptual discomfort for a typical fixed repetition blood flow restriction exercise bout is similar to that for high-load non-blood flow restriction exercise, it is still typically greater than for equivalent intensity non-blood flow restriction exercise. However, over time with chronic blood flow restriction exercise training participant discomfort improves over the initial training weeks, with this effect being observed for both resistance and aerobic focused blood flow restriction exercise training., While the present review and meta-analyses do not directly recommend a particular blood flow restriction cuff pressure system for the purpose of reducing the applied blood flow restriction pressure, regulated systems appear to reduce the average applied blood flow restriction pressure compared with unregulated systems. This becomes especially relevant when applying blood flow restriction in individuals unaccustomed to blood flow restriction exercise or those with a reduced exercise capacity (e.g. older adults and clinical populations), as they are at greater risk of adverse events and report higher perceptual discomfort with blood flow restriction exercise. Therefore, while it seems logical that comfort is improved with a regulated vs unregulated blood flow restriction cuff pressure system to support greater uptake and use of blood flow restriction exercise by practitioners, the limited available evidence that regulated blood flow restriction cuff pressure systems reduce discomfort is inconclusive.,
Naturally, a critical factor for practitioners when considering blood flow restriction cuff pressure systems is cost. Regulated blood flow restriction pressure systems typically include features that measure limb occlusion pressure and, therefore, the ability to apply individualised blood flow restriction pressures, and include medical-grade surgical tourniquets or systems and devices with the same blood flow restriction technology adapted into more compact forms (e.g. Delfi PTS. Vancouver, British Columbia, Canada). These more technologically advanced systems that promote greater precision have previously been prohibitively expensive for most practitioners and end-users. However, with the emergence of more affordable devices it is important to consider their validity against surgical-grade devices given their reliance upon proprietary algorithms to determine limb occlusion pressure, and their capability to set and maintain accurate applied blood flow restriction pressures. In comparison, unregulated blood flow restriction pressure systems include standard clinical sphygmomanometers (and commercialised variants), and less technical options such as elastic and non-elastic bands (sometimes referred to as ‘practical’ options). However, these are less technologically advanced, provide less precision for end-users and lack built-in safety features, with the result being a system that is cheaper to produce and more affordable to end-users. Given the present systematic review and meta-analysis demonstrate similar training outcomes for regulated and unregulated blood flow restriction pressure systems, it might appear attractive for practitioners to seek these more affordable options to implement blood flow restriction exercise. However, greater affordability, accessibility and portability of unregulated blood flow restriction pressure systems should be considered alongside any potential compromise to safety, control of blood flow restriction pressure and lack of individualisation of blood flow restriction pressure application for participants/clients that might contribute to reducing the precision in delivering blood flow restriction exercise. Additional factors for consideration between regulated and unregulated blood flow restriction pressure systems include potentially increased acute haemodynamic responses (especially if exercise is completed to failure) and perceptual responses of end-users which have potential to reduce compliance with blood flow restriction exercise training.
Most regulated, but no unregulated, blood flow restriction cuff pressure systems have the ability to assess limb occlusion pressure and subsequently to more precisely maintain application variables which results in blood flow restriction exercise that is potentially safer and more tolerable. However, most regulated blood flow restriction pressure systems are for indoor or laboratory use and require a constant AC power connection (i.e. mains/grid power), making them less suited to all blood flow restriction exercise applications. While some regulated blood flow restriction pressure systems are battery powered and portable, they are often large and heavy. The alternative presented by unregulated blood flow restriction pressure systems are that they are often small, light, portable and either battery powered or manually operated without the need to be tethered to an AC power supply. This makes unregulated pressure systems potentially more versatile and, importantly, more accessible to a range of populations and in different environments (e.g. in the clinic, the home and community). While more innovative commercialised blood flow restriction pressure systems have emerged over the last five years, the efficacy of these systems is limited when compared with the surgical grade regulated blood flow restriction pressure systems. In some cases, limitations to their advertised application have been noted. Further research incorporating these more contemporary devices is needed to determine their suitability for practitioners and whether they are improvements over basic unregulated blood flow restriction pressure systems that improve access to blood flow restriction exercise under a range of circumstances.
This systematic review and meta-analyses have some limitations. Notably, the meta-analyses utilised subgroup analyses to compare study outcomes between regulated and unregulated blood flow restriction pressure systems. Differences between studies make this a less efficacious method than analysing studies that have utilised both regulated and unregulated blood flow restriction pressure systems using the same protocol within a randomised controlled trial design. However, to the best of the authors’ knowledge, no such training studies exist. Given the recommendations for individualised pressures as ‘best practice’, and the variety of current and emerging blood flow restriction cuff pressure systems, it is also unlikely that sufficient training studies comparing exercise training outcomes between regulated and unregulated blood flow restriction cuff pressure systems will be conducted to enable a more precise synthesis of data.
The present review examined the use of regulated and unregulated blood flow restriction pressure systems, and outcomes related to muscle size, strength, physical function, endurance and aerobic capacity. However, this approach was independent of (did not take into account) other blood flow restriction exercise prescription factors known to influence the acute responses to blood flow restriction exercise, the effects of which are less understood for influencing blood flow restriction exercise training outcomes. These include factors such as prescription variables (e.g. intensity, duration, repetition scheme), the applied blood flow restriction pressure, blood flow restriction cuff width, participant age, fitness and training modality.
Finally, while our meta-analytic approach quantified the magnitude of the effect of blood flow restriction exercise training using different blood flow restriction pressure systems on variables of most interest to practitioners such as muscle strength and muscle size, there was insufficient data to use this approach to examine variables related to objective physical function, endurance or aerobic capacity.
In conclusion, despite blood flow restriction exercise being applied diversely in practice through the use of regulated or unregulated blood flow restriction pressure systems, this systematic review and meta-analysis demonstrates that neither of these generic systems is superior in producing improvements to muscle strength, muscle size and physical function following a period of training. While regulated blood flow restriction pressure systems feature more heavily across the blood flow restriction exercise literature and certainly, more recently, for their integrated capability to measure limb occlusion pressure and provide accurate, comfortable and potentially safer delivery of blood flow restriction exercise, unregulated systems provide greater versatility by being small and light, while typically being cheaper. The future emergence of functional, portable and cost effective regulated blood flow restriction pressure systems will likely improve accessibility for both practitioners and clients, and support blood flow restriction exercise implementation across a larger variety of populations and environments to benefit muscle strength, size and physical function and overall population health.
Clinical messages
Similar benefits to muscle health from blood flow restriction exercise training occur independent of practitioners using regulated or unregulated blood flow restriction pressure systems.
Practitioners should take into account factors such as device quality, perceived safety, comfort, cost and convenience when selecting equipment to deliver blood flow restriction exercise for muscle health.
Acknowledgements
The authors thank those authors contracted who provided data and/or information about their published work. This research received in-kind support from the School of Exercise and Nutrition Sciences, Deakin University.
Declaration of conflicting interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD Stuart A. Warmington https://orcid.org/0000-0002-2414-7539
Supplemental material Supplemental material for this article is available online.
References
- 1. Patterson SD, Brandner CR. The role of blood flow restriction training for applied practitioners: a questionnaire-based survey. J Sports Sci 2018; 36: 123–130.
- 2. Patterson SD, Hughes L, Warmington S, et al. Blood flow restriction exercise: considerations of methodology, application, and safety. Front Physiol 2019; 10: 533. DOI:https://doi.org/10.3389/fphys.2019.00533.
- 3. Ladlow P, Coppack RJ, Dharm-Datta S, et al. Low-load resistance training with blood flow restriction improves clinical outcomes in musculoskeletal rehabilitation: a single-blind randomized controlled trial. Front Physiol 2018; 9: 1269.
- 4. Bennett H, Slattery F. Effects of blood flow restriction training on aerobic capacity and performance: a systematic review. J Strength Cond Res 2019; 33: 572–583.
- 5. Castilla-López C, Molina-Mula J, Romero-Franco N. Blood flow restriction during training for improving the aerobic capacity and sport performance of trained athletes: a systematic review and meta-analysis. J Exerc Sci Fitness 2022; 20: 190–197.
- 6. Cook SB, Kanaley JA, Ploutz-Snyder LL. Neuromuscular function following muscular unloading and blood flow restricted exercise. Eur J Appl Physiol 2014; 114: 1357–1365.
- 7. Cook SB, LaRoche DP, Villa MR, et al. Blood flow restricted resistance training in older adults at risk of mobility limitations. Exp Gerontol 2017; 99: 138–145.
- 8. Cook SB, Scott BR, Hayes KL, et al. Neuromuscular adaptations to low-load blood flow restricted resistance training. J Sports Sci Med 2018; 17: 66–73.
- 9. Yasuda T, Fukumura K, Fukuda T, et al. Muscle size and arterial stiffness after blood flow-restricted low-intensity resistance training in older adults. Scand J Med Sci Sports 2014; 24: 799–806.
- 10. Fujita T, WF B, Kurita K, et al. Increased muscle volume and strength following six days of low-intensity resistance training with restricted muscle blood flow. Int J KAATSU Train Res 2008; 4: 1–8.
- 11. Rolnick N, Kimbrell K, de Queiros V. Beneath the cuff: Often overlooked and under-reported blood flow restriction device features and their potential impact on practice—A review of the current state of the research. Front Physiol 2023; 14: 1089065. DOI:https://doi.org/10.3389/fphys.2023.1089065.
- 12. Jessee MB, Mattocks KT, Buckner SL, et al. Mechanisms of blood flow restriction: the New Testament. Tech Orthop 2018; 33: 72–79.
- 13. Weatherholt AM, VanWye WR, Lohmann J, et al. The effect of cuff width for determining limb occlusion pressure: a comparison of blood flow restriction devices. Int J Exerc Sci 2019; 12: 136–143.
- 14. Loenneke JP, Fahs CA, Rossow LM, et al. Blood flow restriction pressure recommendations: a tale of two cuffs. Front Physiol 2013; 4: 49.
- 15. Clarkson MJ, May AK, Warmington SA. Is there rationale for the cuff pressures prescribed for blood flow restriction exercise? A systematic review. Scand J Med Sci Sports 2020; 30: 1318–1336.
- 16. McEwen JA, Owens JG, Jeyasurya J. Why is it crucial to use personalized occlusion pressures in blood flow restriction (BFR) rehabilitation? J Med Biol Eng 2019; 39: 173–177.
- 17. Day B. Personalized blood flow restriction therapy: how, when and where can it accelerate rehabilitation after surgery? J Arthrosc Related Surg 2018; 34: 2511–2513.
- 18. Loenneke JP, Fahs CA, Rossow LM, et al. Effects of cuff width on arterial occlusion: implications for blood flow restricted exercise. Eur J Appl Physiol 2012; 112: 2903–2912.
- 19. Osada T, Rådegran G. Difference in muscle blood flow fluctuations between dynamic and static thigh muscle contractions: how to evaluate exercise blood flow by Doppler ultrasound. Phys Med Rehabil Res 2016; 1: 1–7.
- 20. Laurentino G, Ugrinowitsch C, Aihara AY, et al. Effects of strength training and vascular occlusion. Int J Sports Med 2008; 29: 664–667.
- 21. Lorenz DS, Bailey L, Wilk KE, et al. Blood flow restriction training. J Athl Train 2021; 56: 937–944.
- 22. Sterne JA, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Br Med J 366: l4898. DOI:https://doi.org/10.1136/bmj.l4898.
- 23. Abe T, Kearns CF, Sato Y. Muscle size and strength are increased following walk training with restricted venous blood flow from the leg muscle, Kaatsu-walk training. J Appl Physiol 2006; 100: 1460–1466.
- 24. Abe T, Kearns CF, Fujita S, et al. Skeletal muscle size and strength are increased following walk training with restricted leg muscle blood flow: implications for training duration and frequency. Int J KAATSU Train Res 2009; 5: 9–15.
- 25. Abe T, Yasuda T, Midorikawa T, et al. Skeletal muscle size and circulating IGF-1 are increased after two weeks of twice daily “KAATSU” resistance training. Int J KAATSU Train Res 2005; 1: 6–12.
- 26. Amani-Shalamzari S, Sarikhani A, Paton C, et al. Occlusion training during specific futsal training improves aspects of physiological and physical performance. J Sports Sci Med 2020; 19: 374–382.
- 27. Araújo JP, Neto GR, Silva J, et al. Does water aerobics with blood flow restriction change the body composition. J Exerc Physiol Online 2015; 18: 25–31.
- 28. Araújo JP, Neto GR, Loenneke JP, et al. The effects of water-based exercise in combination with blood flow restriction on strength and functional capacity in post-menopausal women. Age 2015; 37: 1–9.
- 29. Barcelos LC, Nunes PRP, de Souza LRMF, et al. Low-load resistance training promotes muscular adaptation regardless of vascular occlusion, load, or volume. Eur J Appl Physiol 2015; 115: 1559–1568.
- 30. Burgomaster KA, Moore DR, Schofield LM, et al. Resistance training with vascular occlusion: metabolic adaptations in human muscle. Med Sci Sports Exercise 2003; 35: 1203–1208.
- 31. Colomer-Poveda D, Romero-Arenas S, Vera-Ibáñez A, et al. Effects of 4 weeks of low-load unilateral resistance training, with and without blood flow restriction, on strength, thickness, V wave, and H reflex of the soleus muscle in men. Eur J Appl Physiol 2017; 117: 1339–1347.
- 32. Fahs CA, Rossow LM, Thiebaud RS, et al. Vascular adaptations to low-load resistance training with and without blood flow restriction. Eur J Appl Physiol 2014; 114: 715–724.
- 33. Fahs CA, Loenneke JP, Thiebaud RS, et al. Muscular adaptations to fatiguing exercise with and without blood flow restriction. Clin Physiol Funct Imaging 2015; 35: 167–176.
- 34. Farup J, De Paoli F, Bjerg K, et al. Blood flow restricted and traditional resistance training performed to fatigue produce equal muscle hypertrophy. Scand J Med Sci Sports 2015; 25: 754–763.
- 35. Horiuchi M, Endo J, Sato T, et al. Jump training with blood flow restriction has no effect on jump performance. Biol Sport 2018; 35: 343–348.
- 36. Hunt JE, Walton LA, Ferguson RA. Brachial artery modifications to blood flow-restricted handgrip training and detraining. J Appl Physiol 2012; 112: 956–961.
- 37. Jessee MB, Buckner SL, Mouser JG, et al. Muscle adaptations to high-load training and very low-load training with and without blood flow restriction. Front Physiol 2018; 9: 1448.
- 38. Kacin A, Strazar K. Frequent low-load ischemic resistance exercise to failure enhances muscle oxygen delivery and endurance capacity. Scand J Med Sci Sports 2011; 21: e231–.
- 39. Madarame H, Neya M, Ochi E, et al. Cross-transfer effects of resistance training with blood flow restriction. Med Sci Sports Exercise 2008; 40: 258–263.
- 40. May AK, Russell AP, Warmington SA. Lower body blood flow restriction training may induce remote muscle strength adaptations in an active unrestricted arm. Eur J Appl Physiol 2018; 118: 617–627.
- 41. Moore DR, Burgomaster KA, Schofield LM, et al. Neuromuscular adaptations in human muscle following low intensity resistance training with vascular occlusion. Eur J Appl Physiol 2004; 92: 399–406.
- 42. Ozaki H, Miyachi M, Nakajima T, et al. Effects of 10 weeks walk training with leg blood flow reduction on carotid arterial compliance and muscle size in the elderly adults. Angiology 2011; 62: 81–86.
- 43. Ozaki H, Sakamaki M, Yasuda T, et al. Increases in thigh muscle volume and strength by walk training with leg blood flow reduction in older participants. J Gerontol Ser A Biomed Sci Med Sci 2011; 66: 257–263.
- 44. Park S, Kim JK, Choi HM, et al. Increase in maximal oxygen uptake following 2-week walk training with blood flow occlusion in athletes. Eur J Appl Physiol 2010; 109: 591–600.
- 45. Patterson SD, Ferguson RA. Increase in calf post-occlusive blood flow and strength following short-term resistance exercise training with blood flow restriction in young women. Eur J Appl Physiol 2010; 108: 1025–1033.
- 46. Patterson SD, Ferguson RA. Enhancing strength and postocclusive calf blood flow in older people with training with blood-flow restriction. J Aging Phys Act 2011; 19: 201–213.
- 47. Pope ZK, Willardson JM, Schoenfeld BJ, et al. Hypertrophic and strength responses to eccentric resistance training with blood flow restriction: a pilot study. Int J Sports Sci Coach 2015; 10: 919–931.
- 48. Sakamaki M, Bemben MG, Abe T. Legs and trunk muscle hypertrophy following walk training with restricted leg muscle blood flow. J Sports Sci Med 2011; 10: 338–340.
- 49. Takarada Y, Tsuruta T, Ishii N. Cooperative effects of exercise and occlusive stimuli on muscular function in low-intensity resistance exercise with moderate vascular occlusion. Jpn J Physiol 2004; 54: 585–592.
- 50. Teramoto M, Golding LA. Low-intensity exercise, vascular occlusion, and muscular adaptations. Res Sports Med 2006; 14: 259–271.
- 51. Yasuda T, Fukumura K, Uchida Y, et al. Effects of low-load, elastic band resistance training combined with blood flow restriction on muscle size and arterial stiffness in older adults. J Gerontol Ser A Biomed Sci Med Sci 2015; 70: 950–958.
- 52. Brumitt J, Hutchison MK, Kang D, et al. Blood flow restriction training for the rotator cuff: a randomized controlled trial. Int J Sports Physiol Perform 2020; 15: 1175–1180.
- 53. Lambert B, Hedt C, Daum J, et al. Blood flow restriction training for the shoulder: a case for proximal benefit. Am J Sports Med 2021; 49: 2716–2728.
- 54. Kargaran A, Abedinpour A, Saadatmehr Z, et al. Effects of dual-task training with blood flow restriction on cognitive functions, muscle quality, and circulatory biomarkers in elderly women. Physiol Behav 2021; 239: 113500.
- 55. Laurentino GC, Loenneke JP, Ugrinowitsch C, et al. Blood-flow-restriction-training-induced hormonal response is not associated with gains in muscle size and strength. J Hum Kinet 2022; 83: 235–243.
- 56. Werasirirat P, Namsawang J, Muanjai P, et al. Effect of blood flow restriction training with strengthening exercises in individuals with rounded shoulder posture: a randomized controlled trial. J Phys Educ Sport 2023; 23: 1262–1271.
- 57. Bigdeli S, Dehghaniyan MH, Amani-Shalamzari S, et al. Functional training with blood occlusion influences muscle quality indices in older adults. Arch Gerontol Geriatr 2020; 90: 104110.
- 58. Higgins JP, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. 2nd ed. Chichester, UK: John Wiley & Sons, 2019.
- 59. Abe T, Fujita S, Nakajima T, et al. Effects of low-intensity cycle training with restricted leg blood flow on thigh muscle volume and VO2max in young men. J Sports Sci Med 2010; 9: 452–458.
- 60. Abe T, Sakamaki M, Fujita S, et al. Effects of low-intensity walk training with restricted leg blood flow on muscle strength and aerobic capacity in older adults. J Geriatr Phys Ther 2010; 33: 34–40.
- 61. Amani AR, Sadeghi H, Afsharnezhad T. Interval training with blood flow restriction on aerobic performance among young soccer players at transition phase. Montenegrin J Sports Sci Med 2018; 7: 5–10.
- 62. Bryk FF, Dos Reis AC, Fingerhut D, et al. Exercises with partial vascular occlusion in patients with knee osteoarthritis: a randomized clinical trial. Knee Surg Sports Traumatol Arthrosc 2016; 24: 1580–1586.
- 63. Centner C, Zdzieblik D, Roberts L, et al. Effects of blood flow restriction training with protein supplementation on muscle mass and strength in older men. J Sports Sci Med 2019; 18: 471–478.
- 64. Chulvi Medrano I, Picón Martinez M, García Jaén M, et al. Neuromuscular adaptations after blood flow restriction training combined with nutritional supplementation: a preliminary study. Montenegrin J Sports Sci Med 2019; 8: 37–42.
- 65. Clark BC, Manini TM, Hoffman RL, et al. Relative safety of 4 weeks of blood flow-restricted resistance exercise in young, healthy adults. Scand J Med Sci Sports 2011; 21: 653–662.
- 66. Corvino RB, Oliveira Md, Santos Rd, et al. Four weeks of blood flow restricted training increases time to exhaustion at severe intensity cycling exercise. Revista Brasileira de Cineantropometria & Desempenho Humano 2014; 16: 570–578.
- 67. Gil AL, Neto GR, Sousa MS, et al. Effect of strength training with blood flow restriction on muscle power and submaximal strength in eumenorrheic women. Clin Physiol Funct Imaging 2017; 37: 221–228.
- 68. Hughes L, Rosenblatt B, Haddad F, et al. Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: a UK national health service randomised controlled trial. Sports Med 2019; 49: 1787–1805.
- 69. Karabulut M, Abe T, Sato Y, et al. The effects of low-intensity resistance training with vascular restriction on leg muscle strength in older men. Eur J Appl Physiol 2010; 108: 147–155.
- 70. Libardi CA, Chacon-Mikahil MPT, Cavaglieri CR, et al. Effect of concurrent training with blood flow restriction in the elderly. Int J Sports Med 2015; 36: 395–399.
- 71. Martín-Hernández J, Marín PJ, Menéndez H, et al. Muscular adaptations after two different volumes of blood flow-restricted training. Scand J Med Sci Sports 2013; 23: e114–.
- 72. Mueller SM, Aguayo D, Lunardi F, et al. High-load resistance exercise with superimposed vibration and vascular occlusion increases critical power, capillaries and lean mass in endurance-trained men. Eur J Appl Physiol 2014; 114: 123–133.
- 73. Ozaki H, Yasuda T, Ogasawara R, et al. Effects of high-intensity and blood flow-restricted low-intensity resistance training on carotid arterial compliance: role of blood pressure during training sessions. Eur J Appl Physiol 2013; 113: 167–174.
- 74. Ruaro MF, Santana JO, Gusmão N, et al. Effects of strength training with and without blood flow restriction on quality of life in the elderly. J Phys Educ Sport 2019; 19: 787–794.
- 75. Shimizu R, Hotta K, Yamamoto S, et al. Low-intensity resistance training with blood flow restriction improves vascular endothelial function and peripheral blood circulation in healthy elderly people. Eur J Appl Physiol 2016; 116: 749–757.
- 76. Silva J, Rodrigues Neto G, Freitas E, et al. Chronic effect of strength training with blood flow restriction on muscular strength among women with osteoporosis. J Exerc Physiol Online 2015; 18: 33–41.
- 77. Sousa JBC, Neto GR, Santos HH, et al. Effects of strength training with blood flow restriction on torque, muscle activation and local muscular endurance in healthy subjects. Biol Sport 2017; 34: 83–90.
- 78. Takarada Y, Sato Y, Ishii N. Effects of resistance exercise combined with vascular occlusion on muscle function in athletes. Eur J Appl Physiol 2002; 86: 308–314.
- 79. Vechin FC, Libardi CA, Conceição MS, et al. Comparisons between low-intensity resistance training with blood flow restriction and high-intensity resistance training on quadriceps muscle mass and strength in elderly. J Strength Cond Res 2015; 29: 1071–1076.
- 80. Kim S, Sherk VD, Bemben MG, et al. Effects of short term low intensity resistance training with blood flow restriction on bone markers and muscle cross-sectional area in young men. Int J Exerc Sci 2012; 5: 6.
- 81. Yasuda T, Fujita S, Ogasawara R, et al. Effects of low-intensity bench press training with restricted arm muscle blood flow on chest muscle hypertrophy: a pilot study. Clin Physiol Funct Imaging 2010; 30: 338–343.
- 82. Yasuda T, Ogasawara R, Sakamaki M, et al. Relationship between limb and trunk muscle hypertrophy following high-intensity resistance training and blood flow–restricted low-intensity resistance training. Clin Physiol Funct Imaging 2011; 31: 347–351.
- 83. Manimmanakorn A, Hamlin MJ, Ross JJ, et al. Effects of low-load resistance training combined with blood flow restriction or hypoxia on muscle function and performance in netball athletes. J Sci Med Sport 2013; 16: 337–342.
- 84. Yasuda T, Ogasawara R, Sakamaki M, et al. Combined effects of low-intensity blood flow restriction training and high-intensity resistance training on muscle strength and size. Eur J Appl Physiol 2011; 111: 2525–2533.
- 85. Early KS, Rockhill M, Bryan A, et al. Effect of blood flow restriction training on muscular performance, pain and vascular function. Int J Sports Phys Ther 2020; 15: 892–900.
- 86. Fernandes DZ, Weber VMR, da Silva MPA, et al. Effects of blood flow restriction training on handgrip strength and muscular volume of young women. Int J Sports Phys Ther 2020; 15: 901–909.
- 87. Lopes KG, Farinatti P, Bottino DA, et al. Exercise with blood flow restriction improves muscle strength and mass while preserving the vascular and microvascular function and structure of older adults. Clin Hemorheol Microcirc 2022; 82: 13–26.
- 88. Santos IF, Lemos LK, Biral TM, et al. Relationship between heart rate variability and performance in eccentric training with blood flow restriction. Clin Physiol Funct Imaging 2022; 42: 333–347.
- 89. Counts BR, Dankel SJ, Barnett BE, et al. Influence of relative blood flow restriction pressure on muscle activation and muscle adaptation. Muscle Nerve 2016; 53: 438–445.
- 90. Ellefsen S, Hammarström D, Strand TA, et al. Blood flow-restricted strength training displays high functional and biological efficacy in women: a within-subject comparison with high-load strength training. Am J Physiol-Regul Integr Comp Physiol 2015; 309: R767–.
- 91. Jakobsgaard JE, Christiansen M, Sieljacks P, et al. Impact of blood flow-restricted bodyweight exercise on skeletal muscle adaptations. Clin Physiol Funct Imaging 2018; 38: 965–975.
- 92. Kim D, Loenneke JP, Ye X, et al. Low-load resistance training with low relative pressure produces muscular changes similar to high-load resistance training. Muscle Nerve 2017; 56: E126–.
- 93. Kubo K, Komuro T, Ishiguro N, et al. Effects of low-load resistance training with vascular occlusion on the mechanical properties of muscle and tendon. J Appl Biomech 2006; 22: 112–119.
- 94. Lixandrão ME, Ugrinowitsch C, Laurentino G, et al. Effects of exercise intensity and occlusion pressure after 12 weeks of resistance training with blood-flow restriction. Eur J Appl Physiol 2015; 115: 2471–2480.
- 95. Loeppky JA, Gurney B, Kobayashi Y, et al. Effects of ischemic training on leg exercise endurance. J Rehabilit Res Dev 2005; 42: 511–522.
- 96. Shinohara M, Kouzaki M, Yoshihisa T, et al. Efficacy of tourniquet ischemia for strength training with low resistance. Eur J Appl Physiol Occup Physiol 1997; 77: 189–191.
- 97. Sieljacks P, Degn R, Hollaender K, et al. Non-failure blood flow restricted exercise induces similar muscle adaptations and less discomfort than failure protocols. Scand J Med Sci Sports 2019; 29: 336–347.
- 98. Takada S, Okita K, Suga T, et al. Low-intensity exercise can increase muscle mass and strength proportionally to enhanced metabolic stress under ischemic conditions. J Appl Physiol 2012; 113: 199–205.
- 99. Yasuda T, Loenneke JP, Thiebaud RS, et al. Effects of blood flow restricted low-intensity concentric or eccentric training on muscle size and strength. Plos One 2012; 7: e52843.
- 100. Bergamasco JGA, Alvarez IF, de Campos Biazon TMP, et al. Effects of blood flow restriction combined with resistance training or neuromuscular electrostimulation on muscle cross-sectional area. J Sport Rehabil 2022; 31: 319–324.
- 101. Kataoka R, Vasenina E, Hammert WB, et al. Muscle growth adaptations to high-load training and low-load training with blood flow restriction in calf muscles. Eur J Appl Physiol 2022; 122: 623–634.
- 102. Grønfeldt BM, Lindberg Nielsen J, Mieritz RM, et al. Effect of blood-flow restricted vs heavy-load strength training on muscle strength: systematic review and meta-analysis. Scand J Med Sci Sports 2020; 30: 837–848.
- 103. Labata-Lezaun N, Llurda-Almuzara L, González-Rueda V, et al. Effectiveness of blood flow restriction training on muscle strength and physical performance in older adults: a systematic review and meta-analysis. Arch Phys Med Rehabil 2022; 103: 1848–1857.
- 104. Hughes L, Swain PM, Lai T, et al. It’s time to regulate – the importance of accurate surgical-grade tourniquet autoregulation in blood flow restriction exercise applications. Phys Ther Sport 2024; 67: 41–46.
- 105. Keller M, Faude O, Gollhofer A, et al. Can we make blood flow restriction training more accessible? Validity of a low-cost blood flow restriction device to estimate arterial occlusion pressure. J Strength Cond Res 2023; 37: 1581–1587.
- 106. Jacobs E, Rolnick N, Wezenbeek E, et al. Investigating the autoregulation of applied blood flow restriction training pressures in healthy, physically active adults: an intervention study evaluating acute training responses and safety. Br J Sports Med 2023; 57: 914–920.
- 107. De Queiros VS, Rolnick N, Dos Santos ÍK, et al. Acute effect of resistance training with blood flow restriction on perceptual responses: a systematic review and meta-analysis. Sports Health 2023; 15: 673–688.
- 108. Spitz RW, Wong V, Bell ZW, et al. Blood flow restricted exercise and discomfort: a review. J Strength Cond Res 2022; 36: 871–879.
- 109. Clarkson MJ, Conway L, Warmington SA. Blood flow restriction walking and physical function in older adults: a randomized control trial. J Sci Med Sport 2017; 20: 1041–1046.
- 110. Hughes L, Rosenblatt B, Gissane C, et al. Interface pressure, perceptual, and mean arterial pressure responses to different blood flow restriction systems. Scand J Med Sci Sports 2018; 28: 1757–1765.
- 111. Rolnick N, Kimbrell K, Cerqueira MS, et al. Perceived barriers to blood flow restriction training. Front Rehabilit Sci 2021; 2: 1–14.
- 112. Rolnick N, Licameli N, Moghaddam M, et al. Autoregulated and non-autoregulated blood flow restriction on acute arterial stiffness. Int J Sports Med 2023; 45: 23–32.