Rapid initiation and appropriate selection of antibiotics reduce hospital stay in people with community-acquired pneumonia
- Leibovici, Professor Leonard
- Li, Jim Zhiming MD, PhD
BACKGROUND
The incidence of community-acquired pneumonia is increasing in developed countries, where it is the greatest infectious cause of death. About 25% of people with community-acquired pneumonia require hospitalisation. The length of hospital stay differs between sites, although the reasons for variation remain unclear.
OBJECTIVE
To examine the effect of quality of care factors on length of hospital stay for people with community-acquired pneumonia.
SETTING
Two community and five teaching hospitals, New York; January to December 1998.
METHOD
Retrospective chart analysis.
PARTICIPANTS
Seven hundred adults with community-acquired pneumonia were selected at random from hospital records. Direct to the floor admissions were excluded because admission times were not recorded. People with suspected immunodeficiency were excluded as were those with suspected tuberculosis or Pneumocytis carnii pneumonia, those readmitted within 30 days and those who began antibiotic therapy before arrival. Due to small numbers, in-hospital deaths and people who left hospital early against medical advice were excluded.
ANALYSIS
Demographic and clinical factors were extracted from medical records. Quality of care measures were door to needle time, appropriateness of antibiotic selection (using Infectious Disease Society of America guidelines) and site of initial antibiotic treatment (emergency department versus floor). Regression models were used to correlate quality of care factors and length of hospital stay. Age, respiratory rate at admission, nursing home residence, payer status, ethnicity, white blood cell count, chest X-ray and comorbid illness were controlled for.
OUTCOMES
Length of hospital stay.
MAIN RESULTS
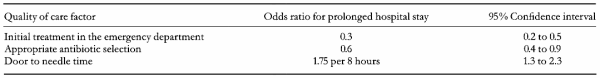
Mean stay in hospital was 7 days. Quality of care variables were associated with length of hospital stay, after adjusting for clinical and demographic factors (Table 1).
AUTHORS' CONCLUSIONS
Unlike clinical and demographic factors, processes of care are modifiable. Rapid initiation of antibiotics and selecting appropriate antibiotics in the emergency department are associated with shorter hospital stay for people with community-acquired pneumonia.
NOTES
Hospitals with a high annual incidence of pneumonia cases were selected.