Personal contact with researchers may increase policy-makers' use of evidence in decision-making
- Bedregal, Professor Paula MD, MPH, MSC
BACKGROUND
Healthcare managers and policy-makers may recognise the importance of using evidence when making decisions, but do not always put evidence into practice. There have been several attempts to increase the use of research evidence in health policy decisions.
OBJECTIVE
To identify factors which facilitate and act as barriers to health policy-makers' use of research evidence, based on interview studies.
METHOD
Systematic review.
SEARCH STRATEGY
MEDLINE, EMBASE, Sociofile, Psychlit, PAIS, IBSS, IPSA and HealthSTAR were searched to June 2000. Key journals and personal files were hand searched and experts were contacted for additional studies.
INCLUSION/EXCLUSION CRITERIA
Interview studies were eligible if they focused on policy-makers' use of research in health policy decisions at a national, regional or organisational level. Only health policy-makers responsible for decisions on behalf of a large organisation or jurisdiction were included. There were no language restrictions. Of more than 3000 references identified, 24 studies were included with 2041 interviews. Ten studies were based in the United States, three in Canada, three in the United Kingdom and one in each of Australia, Burkina Faso, Mexico, the Netherlands, Pakistan, South Africa, Sweden and combined US/UK.
DATA EXTRACTION
Two reviewers independently assessed the relevance of retrieved articles, described methods and extracted data. Data were summarised in tables and analysed qualitatively.
MAIN OUTCOMES
Facilitators of and barriers to using research in health policy decisions.
MAIN RESULTS
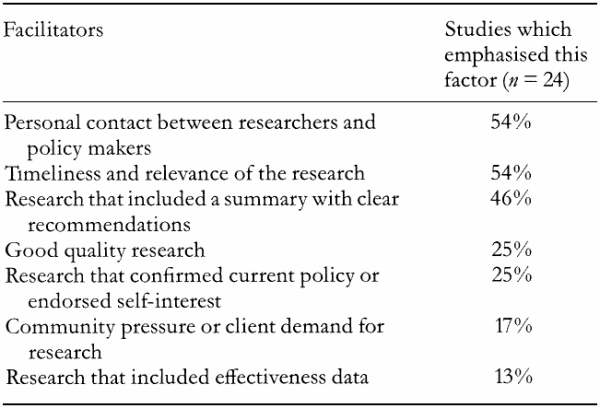
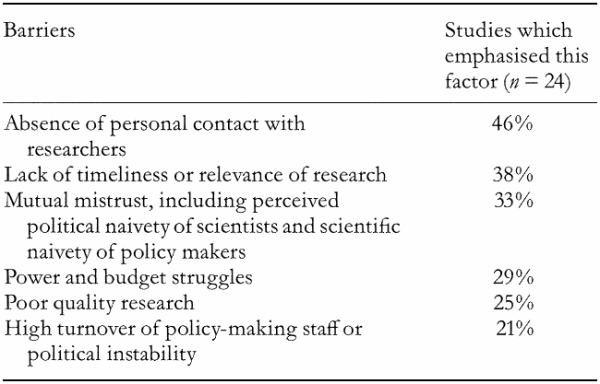
Perceived facilitators of and barriers to using evidence varied (Tables 1 and 2). The most commonly reported facilitators were personal contact with researchers (54% of studies), timeliness and relevance (54%) and clear policy recommendations in research reports (46%). Commonly reported barriers were absence of personal contact (46% of studies), lack of timeliness or research relevance (38%), mistrust of research(ers) (33%) and power and budget struggles (29%).
AUTHORS' CONCLUSIONS
Personal two-way communication between researchers and policy-makers may facilitate the use of evidence in healthcare decision-making. Two-way communication may inform researchers about what decision-makers consider timely and relevant while educating policy-makers about how to obtain valid answers to their questions.