Non-directive counselling and cognitive behaviour therapy have short-term benefits over usual GP care for depression but are not more cost-effective in the long termRandomised controlled trial of non-directive counselling, cognitive-behaviour therapy, and usual general practitioner care for patients with depression. I: clinical effectiveness.
- Oei, Tian P. S PhD, FAPS
- Ward, E
- King, M
- Lloyd, M
- Bower, P
- Sibbald, B
- Farrelly, S
- Gabbay, M
- Tarrier, N
- Addington-Hall, J
BACKGROUND
Short courses of psychotherapy are common in British general practice. Although the effectiveness of these methods has been established in more specialised settings, the efficacy of GP-based psychological depression strategies is less clear. Little is known about their cost-effectiveness.
OBJECTIVE
To compare the clinical efficacy and cost-effectiveness of counselling, behaviour therapy and usual GP care for people with depression.
SETTING
Thirteen general practices in North London and 11 in greater Manchester; recruitment February 1996-November 1997.
METHOD
'Patient preference' controlled trial with one randomised arm.
LITERATURE REVIEW
No explicit strategy; 19 references (Bower et al), 25 references (Ward et al).
PARTICIPANTS
One hundred and ninety-seven out of 464 eligible adults (mean age 37) presenting to their GP with a Beck depression inventory score of 14 + were fully randomised. One hundred and thirty-seven chose their own treatment and 130 were randomised between the two psychological treatment groups only. Those with a history of psychological therapy; serious suicide attempt; inability to complete questionnaires; restricted mobility; or antidepressant drugs were excluded.
INTERVENTION
Usual GP care; 6-12 sessions of non-directive counselling from a specialist counsellor (mean = 6 sessions); or cognitive behavioural therapy with a psychologist (mean = 16.5 sessions).
OUTCOMES
Depressive symptoms (Beck depression inventory); health related quality of life; satisfaction with treatment; direct treatment and other costs - all measured after 4 and 12 months. Outcome assessment was not blind to treatment allocation.
ASSUMPTIONS
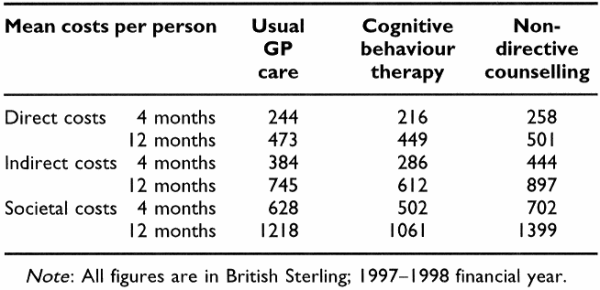
Societal cost-effectiveness perspective; cost data was collected from patient medical records and self-report. Unit costs for 1997-1998 financial year were calculated using the British National Formulary and Personal Social Services Research Unit and Chartered Institute of Public Finance and Accountancy databases. Means and decision rules were used in the case of missing values.
MAIN RESULTS
After 4 months, depressive symptoms were lower for those receiving specialist led interventions compared to usual GP care. This difference was not evident after 1 year. After 4 months both intervention groups were more satisfied than the usual GP care group, but after 1 year satisfaction was higher only in the non-directive counselling group. There were no differences between the three groups in direct, societal, or loss of production costs (see Table 1). Those receiving usual care had more consultations; use of antidepressant drugs; and psychiatric referrals. There were no differences in these trends for randomised and non-randomised participants.
AUTHORS' CONCLUSIONS
Psychological therapies based in a general practice setting have short-term clinical benefits over usual GP care, but these may not last. The lack of effect after 1 year may be due to under powering. Variation in treatment costs necessitates further research.