Introduction
Otosclerosis is an underlying disease of the bony labyrinth. This disorder, occurring only within the area of a person’s temporal bone, is characterized by a progressive hearing loss and tinnitus. - The disease has a long-term course and can lead to severe hypoacusis and even deafness. ,
On the basis of histological examinations, it was concluded that the process of otosclerosis most often develops in the front part of the oval window in a spot referred to as “fistula ante fenestram.” In addition to the above location, the lesions may also include the round window, semicircular canals, the area around the cochlea, endings of nerve fibers of the upper ampulla branch, and lateral vestibular nerve. -
On the basis of the location of the otosclerosis outbreaks, 3 types of otosclerosis were distinguished:
The Bezold-Siebenmann type
The Manasse type
The Lermoyez type
Otosclerotic outbreaks most often cause immobilization of the stirrup in the oval window and the appearance of conductive hypoacusis (Bezold-Siebenmann type). In pure tone audiometry, threshold curves have an ascending character, the Cochlear reserve is maintained, often a refraction of the bone conduction curve with a depth of 10 to 20 dB at a frequency of 2000 Hz (the so-called Carhart notch) appears. At the initial stage of the disease, the hypoacusis may be one-sided, later bilateral, and usually unbalanced. Patients with otosclerosis who have conductive hypoacusis are characterized by quiet speech and often better hearing in noise (paracusis Willisi). As otosclerotic lesions spread to the niche area of the oval window, proteolytic enzymes are released in the outbreaks of otospongiosis. The enzymes penetrate into the fluid of the inner ear, resulting in a change in hypoacusis from conductive to mixed or even sensorineural hearing loss (Lermoyez type). Otosclerosis within the labyrinth, but without immobilizing the stapes base, leads to hypoacusis of the sensorineural type (Manasse type).
The advanced form of otosclerosis is defined clinically as mixed hypoacusis with bone conduction thresholds above 55 dB and air conduction above 95 dB. The most serious variant of this disease is the so-called malignant form of otosclerosis, in which the reconstruction concerns the whole labyrinth bone cover, ultimately leading to deafness. -
Material and Method
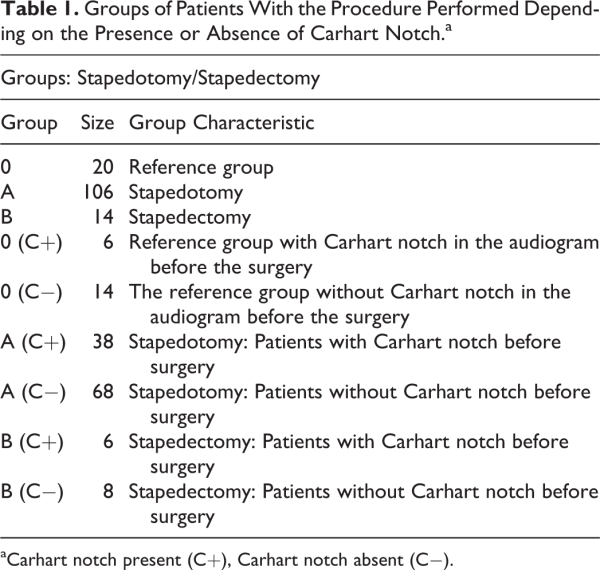
The analysis included 140 patients operated on for the first time due to otosclerosis at our department in 2010 to 2016. The youngest patient was 19 years old and the oldest was 62 years old. The average age was 39.31 years. The study group consisted of 107 women aged 19 to 62 years (average age: 40.33 years) and 33 men aged 27 to 59 years (average age: 38.23 years). The aim of the analysis was to divide patients into 2 groups depending on the surgery performed (stapedotomy [A], stapedectomy [B]). In addition, a reference group was isolated from the group whose members underwent stapedotomy. The reference group consisted of patients in whom, apart from complete immobilization of the stirrup base in the oval window, no other lesions were found in the middle ear and the osseous conduction of the ear operated in the presurgical tonal audiogram fell within the range of 0 to 20 dB. The reference group consisted of 20 patients, 16 women and 4 men (Table 1). In order to carry out a detailed analysis, patients in particular groups were divided into subgroups (0: Carhart notch present [C+], Carhart notch absent [C−], A: [C+], [C−], B: [C+], [C−]) depending on the occurrence of Carhart notch in the tonal audiogram before the surgery or lack thereof (Table 1). The study looked for the answer to the question of whether the presence or absence of Carhart notch in the presurgical tonal audiogram affects the final outcome of the otosclerosis surgery.
The audiometric tests were performed in a sound-proof cabin of the audiometric laboratory. In the cabin, the equivalent sound level corrected by the A characteristic did not exceed 25 dB A. The intensity of the stimulus for each of the tested frequencies was determined with an accuracy of 5 dB. The interior of the room was always occupied only by the examined person. Threshold values for air and bone conduction were determined by the MIDIMATE 622 audiometer (Midimate 622; Madsen, Budapest, Hungary) equipped with TDK 39 headphones (39 headphones; TDH, Tokyo, Japan). The audiometer met the ISO ISO0389-1985 standard and the ISO7566-1987 standard for air conduction and bone conduction, respectively.
The data obtained during the research were subjected to statistical analysis. The first test applied in order to analyze the improvement in hearing was the Fisher test, also known in the relevant literature as the analysis of variance test. The test analyzes the impact of the classification criterion on the results of the conducted study. In the work, the null hypothesis states that the mean values of given parameters are statistically equal. The alternative hypothesis is the inverse statement that the means are not equal. The statistical test conducted with the use of the analysis of variance consisted of finding the F0 function. The null hypothesis stating that all means are equal was rejected with the α risk of error when: F0 > αFN-kk-1. In the test verifying nonparametric hypotheses, the c2 test was applied—that of multicolumn contingency tables (cross tabulation). This test is used for nonmeasurable variables of qualitative nature. In this test, the Pearson χ2 test was applied as the method of calculating c2, which was confirmed by the χ2 goodness-of-fit test. This method allows to analyze whether the data representing variables contained in cross-tabulation provide sufficient proof for a correlation between these variables. The correlation significance is represented with the use of Cramér V, whose value always falls between 0 and 1. The greater the correlation between variables, the closer to 1 the value of the coefficient is. In the work, the sufficient significance level of 5% was defined (α = .05), which means that the risk of the error of rejecting the hypothesis in case of its validity equals 5%. Statistically significant results were reported for P < .05.
In the statistical analysis process, the Statistica software was used (Statistica, StatSoftPolska, Krakow, Poland). Informed consent was taken from each patient included in the study. Local ethics committee approved the study.
Results
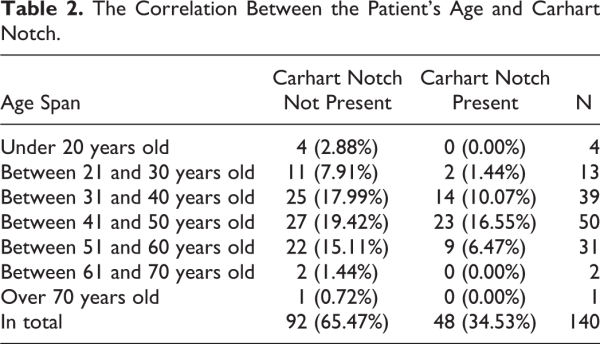
In the assessment of Carhart notch in the tonal audiogram prior to surgical treatment depending on the patient’s age, no statistically significant differences were found (χ2 = 7, 76, P = .08 and Cramér V = 0.22; Table 2).
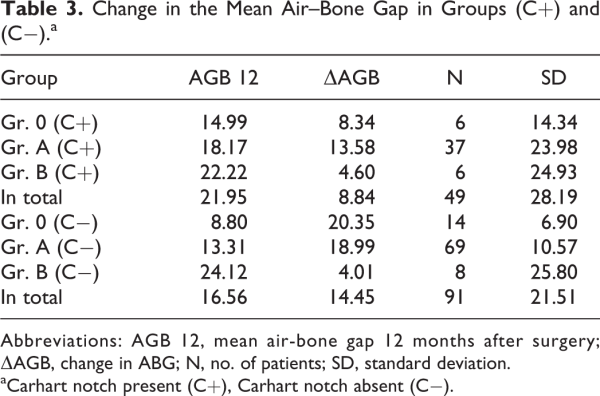
In the next stage of the analysis, the degree of hearing improvement was determined in terms of closing the air–bone gap (ABG) 12 months after the surgery, depending on the occurrence of Carhart notch in the presurgical audiogram. In the analysis of variance after the treatment, the following results of changes in the mean ABGs were obtained, P < .05 (Table 3).
Based on the obtained data, it was confirmed that the result of the surgery after stapedotomy is statistically better than that of the procedure performed with the stapedectomy method, regardless of the presence of the Carhart notch.
Analysis within the same procedure showed a statistically better result of stapedotomy in patients without the notch (Group [Gr.] A [C−], Gr.0 [C−]) than in the same procedure in patients with the notch present (Gr. A [C+]). The opposite situation occurred in the case of stapedectomy. In the assessment of this group of patients, statistically better results were obtained in patients with the notch (Gr. B [C+]).
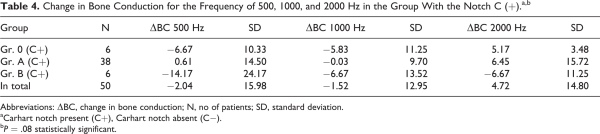
In the subsequent part of the study, the change in the value of the bone conduction threshold was analyzed depending on the surgical procedure and the presence or absence of Carhart notch in the presurgical tonal audiogram. The analysis was conducted for the frequencies of 500, 1000, and 2000 Hz. For the groups of patients created on the basis of the surgery performed with Carhart notch present in the presurgical tonal audiogram, the following results were obtained (Table 4).
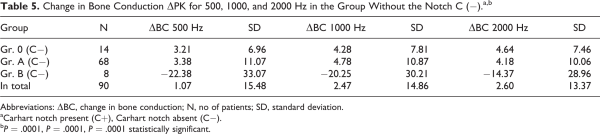
Within the analyzed groups, there were no statistically significant changes in the bone conduction threshold values in the studied frequencies after the surgery. In the analysis of groups of patients without the Carhart notch in the presurgical tonal audiogram, the following results were obtained (Table 5).
Based on the obtained data, it was concluded that after the period of 12 months from the surgery, the change in the mean threshold value of bone conduction between the groups formed at the frequencies tested was statistically significant (P < .05). The average values for groups A and 0 were significantly different from the group B average. In the population of patients without the Carhart notch and the stapedotomy surgery (Gr. 0, Gr. A), a statistically significant improvement in the mean threshold of bone conduction was found. In the postsurgical evaluation of patients without the Carhart notch who underwent stapedectomy, an increase in the mean threshold of bone conduction was noted. At the same time, there were no statistically significant differences between the mean threshold bone conduction values of groups A and 0.
Discussion
Otosclerosis is an osteodystrophic disease of the labyrinth bone shell, manifested by progressive hearing loss and tinnitus. According to the current state of knowledge, the only effective way to treat otosclerosis is to perform a surgery on the stirrup, whose aim is to restore the functions of the oval window and thus the proper mobility of the middle ear transmission system.
Considering the factors affecting the improvement of hearing in patients operated on due to otosclerosis, the occurrence of Carhart notch and its influence on the result of surgical treatment were analyzed. Carhart notch, described for the first time in 1950, involves a reduction in the bone curve by approximately 10 to 20 dB at a frequency of 2000 Hz. It arises as a result of mechanical immobilization of the stirrup base in the oval window and disturbances in the self-resonance of the ossicular chain. Immobilization of the stirrup in otosclerosis and the associated loss of ossicular resonance impairs the 3 bone conduction pathways described by Tondorf in 1968 (directly from the bones to the cochlea, from the bones to the middle ear and to the cochlea, and from the bones to the external auditory canal, then to the middle ear and to the cochlea). The largest contribution of the middle ear elements occurs for the resonant frequency. The improvement in bone conduction after a successful surgery (stapedotomy) changes the properties of the middle ear by changing the mass and stiffness of the osseous chain, causing a modification of the resonant frequency and improvement in the measured bone conduction thresholds. The change in bone conduction and disappearance of Carhart notch after successful surgery are complex and multicomponent phenomena, and according to numerous authors (Sheehy, Sellars, Hueb et al, and Lippy et al ), it is not possible to analyze and explain the obtained results using a single mechanism. In our observations, the lack of Carhart notch in the presurgical tonal audiogram is a favorable prognostic factor in terms of hearing improvement (closing the cochlear reserve and improving bone conduction) in the case of stapedotomy. ,
Conclusions
The presence of Carhart notch in the presurgical tonal audiogram is an unfavorable prognostic factor in relation to closing the cochlear reserve and improving bone conduction after the stapedotomy.
Regardless of the presence or absence of Carhart notch in the presurgical tonal audiogram, stapedotomy is the procedure with the highest efficiency in the treatment of otosclerosis.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by statutory funds of the Department of Otolaryngology, Jagiellonian University, Krakow, Poland.
Agnieszka Wiatr
https://orcid.org/0000-0002-1793-0744
Maciej Wiatr
https://orcid.org/0000-0003-0840-9268
References
- 1. Niemczyk K, Bruzgielewicz A, Bartoszewicz R, Pierchała K. Naturalny rozwój otosklerozy—od szumu do głuchoty. Pol Merkuriusz Lek. 2005;19(111):475–477.
- 2. Gersdorff M, Nouwen J, Gilain C, Decat M, Betsch C. Tinnitus and otosclerosis. Eur Arch Otorhinolaryngol. 2000;257(6):314–316.
- 3. Kaczmarek JP, Szymiec E, Dabrowski P, Szyfter W. Jednostronne szumy uszne—diagnostyka i leczenie. Otolaryngol Pol. 2002;56(3):361–364.
- 4. Quaranta N, Bartoli R, Lopriore A, Fernandez-Vega S, Giagnotti F, Quaranta A. Cochlear implantation in otosclerosis. Otol Neurotol. 2005;26(5):983–987.
- 5. Szymański M, Siwiec H, Gołąbek W. Zmiana obrazu otosklerozy w dwóch dziesięcioleciach. Otolaryngol Pol. 2002;56(5):557–560.
- 6. Quesnel AM, Ishai R, McKenna MJ. Otosclerosis: temporal bone pathology. Otolaryngol Clin North Am. 2018;51(2):291–303.
- 7. Schuknecht HF. Pathology of the Ear. 2. Vol. 4. New York, NY: Lea and Febiger;1993:365–379.
- 8. Nager GT. Pathology of the Ear and Temporal Bone. 1. Baltimore, MD: Williams &Wilkins; 1993:943–1010.
- 9. Szyfter W. Otoskleroza. Zarys audiologii klinicznej. Pruszewicz A (red). Wydawnictwo AM, Poznań. 2000:329–331.
- 10. Latkowski B. Moja przygoda z otosklerozą. Otolaryngol Pol. 1998;52(5):557–563.
- 11. Olszewski E, Reroń E. Otoskleroza. Nowa Med. 1996;3(7):18–20.
- 12. Cohen MM Jr. The new bone biology: pathologic, molecular and clinical correlates. Am J Med Genet. 2006;140(23):2646–2706.
- 13. Arnold W, Niedermeyer HP, Altermatt HJ, Neubert WJ. Zur Pathogenesse der Otosclerose. HNO. 1996;44(3):121–129.
- 14. Lander ES. Initial impact of the sequencing of the human genome. Nature. 2011;470(7333):187–203.
- 15. Menger DJ, Tange RA. The etiology of otosclerosis: a review of the literature. Clin Otolaryngol Allied Sci. 2003;28(2):112–120.
- 16. Paparella MM. Otolaryngology: Otology and Neuro-Otology. Philadelphia, PA: W.B. Saunders Company; 1991:1489–1512.
- 17. Danesh AA, Shahnaz N, Hall JW. The audiology of otosclerosis. Otolaryngol Clin North Am. 2018;51(2):327–342.
- 18. Kukuła K. Elementy statystyki w zadaniach. Warszawa, Poland: PWN; 1998.
- 19. Tondorf J. A new concept of bone conduction. Arch Otolaryngol. 1968,87(6):595–600.
- 20. Sheehy JL. Stapedectomy in the fenestrated ear. Ann Otol Rhinol Laryngol. 1962;71(12):1027–1038.
- 21. Sellars SL. Surgery of advanced otosclerosis. S Afr Med J. 1972;46(15):434–437.
- 22. Hueb MM, Goycoolea MV, Muchow D, Duvall AJ, Paparella MM, Sheridan C. In search of missing links in otology. III. Development of a new animal model for cholesteatoma. Laryngoscope. 1993;103(7):774–784.
- 23. Lippy WH, Battista RA, Schuring AG, Rizer FM. Far-advanced otosclerosis. Am J Otol. 1994;15(2):225–228.
- 24. Perez R, de Almeida J, Nedzelski JM, Chen JM. Variations in the “Carhart notch” and overclosure after laser-assisted stapedotomy in otosclerosis. Otol Neurotol. 2009;30(8):1033–1036.
- 25. Cheng HCS, Agrawal SK, Parnes LS. Stapedectomy versus stapedotomy. Otolaryngol Clin North Am. 2018;51(2):375–392.