Introduction
The incidence of oropharyngeal squamous cell carcinoma (OPSCC) has substantially increased over the last 30 years, with up to 70% of new diagnosis testing positive for human papilloma virus (HPV). The rise in HPV positive OPSCC has resulted in a demographic shift of the typical head and neck population from older male smokers to younger, non-smoking, patients with no gender predilection. This “viral epidemic” within a generally otherwise fit and well cohort has led to a drive for oncological and surgical management strategies that avoid the long-term complications associated with traditional OPSCC management.
Current recommendations for early T1-2 OPSCC advise single modality treatment in the form of either radical radiotherapy, transoral laser microsurgery or transoral robotic surgery (TORS), with more advanced disease typically managed with organ sparing chemoradiotherapy regimes. However, data from the RTOG trials suggests up to 35% of patients with OPSCC can experience severe late toxicity including pain, xerostomia, dysphagia, and reliance on gastrostomy feeding following chemotherapy treatment. Systematic reviews of TORS in early OPSCC have demonstrated similar survival outcomes with reduced rates of dysphagia and gastrostomy dependence compared to radiotherapy, advocating its use it young patients who wish to avoid long term toxicity. Similarly, with almost 25% of patients with OPSCC treated with chemoradiotherapy experiencing recurrence regardless of HPV status, there is an increasing interest in the utilization of TORS to avoid the need for open resection techniques which can carry a very significant quality of life burden.
In our tertiary referral head and neck unit, we have recently adopted the combined technique of TORS oropharyngeal resection with robotic-assisted insertion of radial forearm free flap (RFFF) in select patients with recurrent and residual OPSCC. We present the oncological, functional, and quality of life outcomes in 3 patients managed with this innovative technique.
Methods
Three patients presenting with recurrent or residual OPSCC were identified from the NHS Imperial College Healthcare head and neck multi-disciplinary team meeting from 2018 to 2019. Outpatient clinical examination, assessment under anesthesia, mapping biopsies, and head and neck radiologist review of cross-sectional imaging were vital in determining tumor resectability using TORS.
Preoperatively, patients were assessed jointly in clinic by both head and neck and plastic surgical teams, with the risks and benefits of TORS surgery (including the potential complications associated with RFFF) explained. In the event of positive margins and as an alternative option to TORS oropharyngectomy, resection via an open approach was discussed. Patients were counseled on the need for nasogastric feeding and temporary tracheostomy with the specialist nursing, dietician, and speech and language therapist teams.
All patients underwent a selective neck dissection, TORS oropharyngeal resection, RFFF, and temporary tracheostomy. One patient with more advanced disease also received a pectoralis major flap with a split thickness skin graft. All operations were performed at St Mary’s hospital, London, by the same head and neck and plastic reconstructive surgical teams using the daVinci robot system.
Pre- and postoperative University of Washington Quality of Life (UWQoL) and MD Anderson Dysphagia Index (MDADI) questionnaires were supplied to assess functional outcomes. University of Washington Quality of Life contains questions on 12 indicators scored from 0 to 100, with 100 implying no impact on QOL. MD Anderson Dysphagia Index assesses swallow through 20 questions scored from 1 to 5 which are then summarized under 4 headings (global, physical, emotional, functional) in a range from 0 to 100. Higher scores denote better swallowing outcomes.
Methods
Patient Cohort
Patient 1 is a 68-year-old male previously treated with chemoradiotherapy in India for a T3N0M0 p16 positive tonsillar SCC. A positron emission tomography-computed tomography (PET-CT) in the United Kingdom at 5 months posttreatment revealed an intense focus of increased uptake within the right tonsil in keeping with residual disease.
Patient 2 is a 53-year-old man who presented with persistent throat pain 46 months after previous chemoradiotherapy for a T2N3M0 p16 positive tongue base SCC. Endoscopic examination and magnetic resonance imaging demonstrated a malignant-appearing erosion over his tonsil suggestive of recurrent disease.
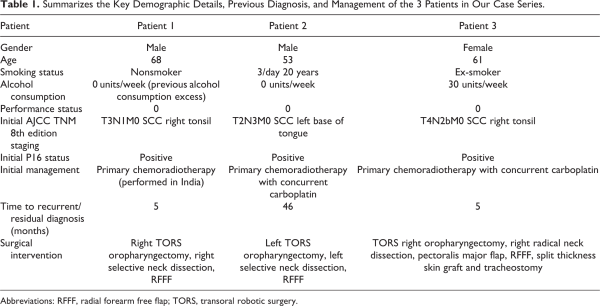
Patient 3 is a 63-year-old woman who was treated with induction chemotherapy followed by radical chemoradiotherapy for a T4N2bM0 tonsillar SCC. 4 months posttreatment a PET CT scan revealed metabolically active lesions within the right tonsil, glossotonsillar sulcus, and several right-sided neck lymph nodes. Patient demographic data is summarized in Table 1 and preoperative imaging is displayed in Figure 1.
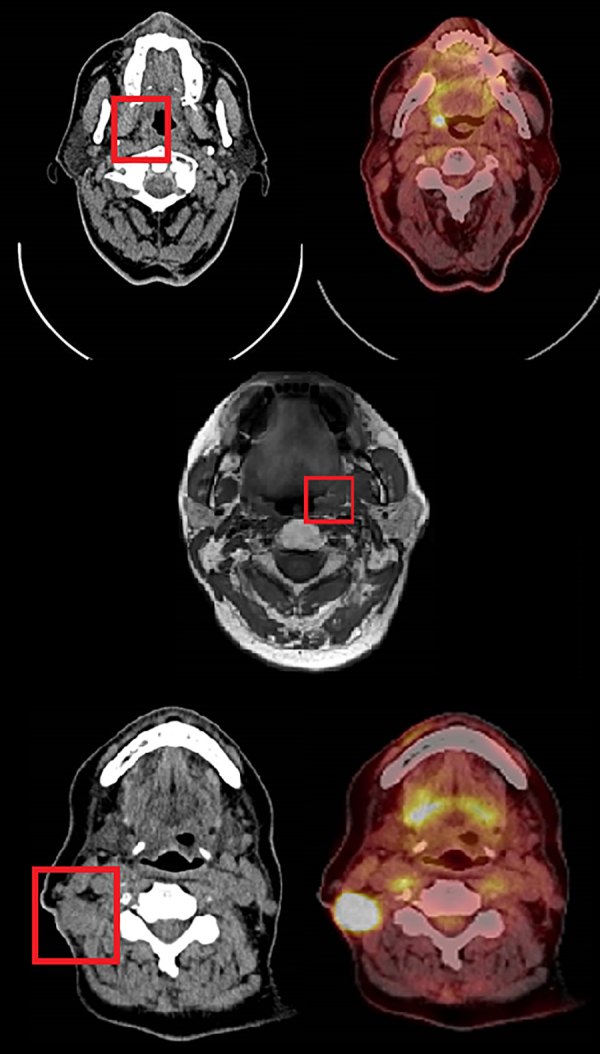
Figure 1
Summary of patient preoperative imaging. TOP (Patient 1). Left-axial view contrast enhanced CT showing lesion within right tonsil suggestive of residual disease (red box). Right-axial PET CT showing a strongly FDG avidity within the same tonsillar lesion. MIDDLE (Patient 2). T1 axial view MRI demonstrating a 2-cm mucosal irregularity with increased enhancement in the left tonsillar fossa (red box). BOTTOM (Patient 3). Left-axial view contrast enhanced CT showing malignant appearing changes in right tonsil and glossotonsillar sulcus and an enlarged abnormal right neck node (red box). Right-axial view PET CT showing intense FDG uptake within enlarged right neck lymph nodes. FDG indicates fluorodeoxyglucose; MRI, magnetic resonance imaging; PET-CT, positron emission tomography-computed tomography.
Methods
Surgical Technique
Patients initially underwent a selective neck dissection guided by nodal status on cross sectional imaging. Marginal mandibular, greater auricular, lingual, and accessory nerves were identified when necessary and preserved. Vessels for graft anastomosis were identified during this stage, with the facial artery and vein used in 2 patients and the transverse cervical artery and vein in the third. Other large vessels are not routinely ligated in order to maintain blood supply to the irradiated field and are later covered by the RFFF to reduce the risk of postoperative hemorrhage. A temporary tracheostomy is performed through a minimal access incision to protect the airway from potential postoperative edema and hemorrhage.
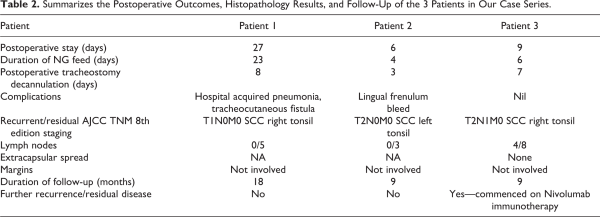
Access to the oropharynx is achieved with a Boyle-Davis gag and a silk stitch placed through the tip of the tongue to provide anterior retraction. The daVinci robot arms and camera are then introduced transorally with an assistant providing suction and retraction as required. The tumor is identified and excised with wide macroscopic margins. Hemostasis is achieved with floseal hemostatic matrix and bipolar diathermy. During this stage, the RFFF is harvested by the plastic surgical team. The graft is then introduced into the oral cavity and the vascular pedicle is tunneled under the digastric muscle to the external neck where a microvascular end-to-end anastomosis is performed to the previously identified donor vessels. The flap is inset within the oropharynx under robotic control with 3/0 sutures. The neck is then closed in layers with a penrose drain left in situ. Intraoperative clinical photographs are shown in Figure 2.
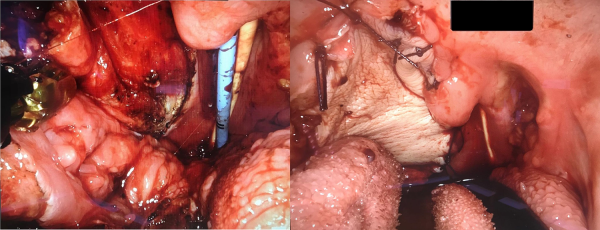
Figure 2
Intraoperative clinical photographs. LEFT, a right-sided oropharyngeal defect can be seen following transoral robotic excision of recurrent oropharyngeal cancer. The tongue base is seen inferiorly and the uvula superiorly. Nasogastric and endonasal tracheal tubes are seen centrally. RIGHT, the same right sided defect after primary closure with robotic-assisted radial forearm free flap.
Results
Mean postoperative stay was 14 (range 6-27 days) days with 2 patients discharged within 10 days of surgery. Two patients experienced postoperative complications. Patient 1 required a prolonged inpatient stay due to a persistent tracheocutaneous fistula following tracheostomy decannulation with a resultant hospital acquired pneumonia which was managed with first-line antibiotics. Patient 2 had a minor episode of hemorrhage from his lingual frenulum which was managed nonsurgically. Mean duration of enteral feeding was 11 days (4-23 days) with nasogastric tube removal and resumption oral diet occurring in all patients prior to discharge. All patients underwent early tracheostomy decannulation (mean postoperative interval 3 days, range 3-8) with no episodes of acute airway distress.
Histopathological examination demonstrated complete R0 clearance of the primary lesion in all cases with no margin involvement. All specimens demonstrated p16 positive SCC which was metastatic to 4/8 lymph nodes in one patient without extracapsular spread.
The mean duration of follow-up is 12 months with the first and second patients showing no signs of recurrence on clinical examination or cross-sectional imaging. A posttreatment CT in the third patient revealed likely new lymph node involvement in the right neck and mediastinum, and as a result, they have been commenced on Nivolumab immunotherapy as a third line treatment. Postoperative outcomes are summarized in Table 2.
Comparison of UWQOL scores did not show any considerable difference in QOL between the pre-and postoperative period; however, small improvements were noted in activity, chewing and anxiety scores, and no change or mild reduction seen in the remaining domains (Figure 3). Similarly, mean MDADI scores did not show any substantial difference across all domains, with global and emotional scores being identical pre- and postoperatively (G 66.7 vs 66.7, E72.2 vs 72.2) and functional and physical (F 58.7 vs 60, P 56.7 vs 57.54) scores demonstrating a slight improvement posttreatment (Figure 4).
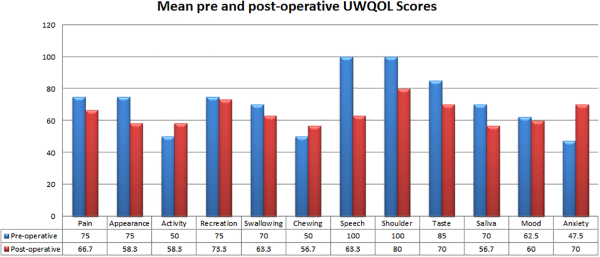
Figure 3
Graph and table summarizing mean preoperative (blue) and postoperative (red) University of Washington quality of life scores.
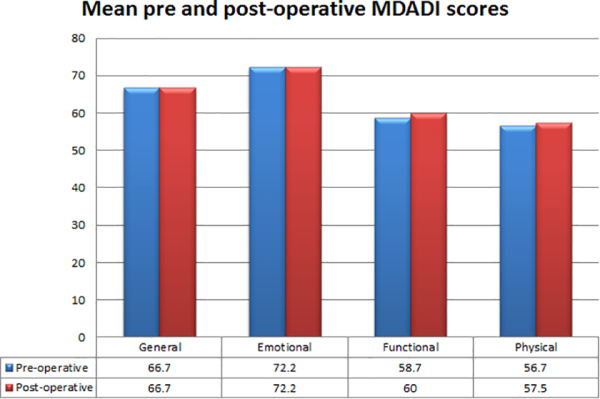
Figure 4
Graph and table summarizing mean preoperative (blue) and postoperative (red) MD Anderson dysphagia inventory scores.
Discussion
Chemoradiorecurrent oropharyngeal cancers have traditionally required extensive surgical resection to achieve disease clearance. These tumors often necessitate transcervical or lip-split mandibulotomy approaches to facilitate access to the oropharynx and deep neck spaces, resulting in considerable postoperative morbidity and poor functional recovery. Over 50% of patients undergoing conventional surgery experience significant postoperative complications including mandibular malunion, temporomandibular joint dysfunction, fistula, and dysphagia. The promising functional outcomes TORS has demonstrated in treating primary oropharyngeal tumors has therefore led to the emergent use of robotic surgery to treat recurrent and residual disease.
Two retrospective series have compared the functional and quality of life outcomes between TORS and conventional salvage surgery. In 2 cohorts of 64 patients, White et al reported statistically significant improvements in mean operative blood loss, operation time, presence of negative margins, shorter hospital stay, 2-year survival, and tracheostomy and gastrostomy dependence in the TORS group. Similarly, Dean et al demonstrated reduced length of hospital stay and tracheostomy and gastrostomy use in a comparison of 15 open and 7 TORs patients. However, these series highlight an important selection bias in that the limitations of robotic surgery in the context of advanced T stage disease and bony invasion means patients in the conventional surgical groups often have more advanced disease; a factor that is associated with an overall poorer prognosis regardless of treatment. Additionally, these differ from our series by avoidance of routine tracheostomy and free flap insertion; however, White reported a 20% incidence of airway compromise necessitating intervention in their TORs group. Dean et al only experienced a single episode of airway compromise necessitating reintubation; however, they resultantly altered their routine practice to keep patients intubated for 24 to 48 hours postoperatively. In our experience, tracheostomy may therefore reduce the incidence of postoperative airway emergency and avoid the complications associated with prolonged intensive care unit stay and intubation.
The use of a TORS and robotic assisted RFFF in OPSCC has not been extensively reported. Paleri et al have previously described use of RFFF and medial sural artery perforator flaps in 3 patients within a larger case series, limiting its use to patients with clear defects or exposed vessels. Despite reporting overall favorable swallowing and survival outcomes, the authors do not make any direct comparison between free flap and non-free flap patients. Our case series has demonstrated the method is technically feasible with minimal postoperative complications and clear surgical margins. All 3 patients have exhibited excellent functional outcomes with each undergoing tracheostomy decannulation, removal of nasogastric tube, and resumption of oral diet within 1 month post-procedure. Moreover, UWQOL and MDADI scores reveals similar pre- and postoperative swallowing and symptom outcomes, suggesting swallow function and QOL are not significantly negatively impacted by TORs with RFFF.
Advantages of Surgical Technique
Robotic surgery has distinct ergonomic advantages that make it ideal for operating in the confined areas of the oropharynx. Its 3-dimensional, high-definition camera and multi-jointed instruments allow for clear visualization and tissue handling without direct line of sight. It therefore facilitates safe and precise dissection of oropharyngeal tumors without the need for traumatic access techniques such as mandibular osteotomy. Patients can thus make a swifter postoperative recovery and avoid the need for long-term enteral feeding and tracheostomy.
Radial forearm free flap in patients with recurrent and residual disease confers a number of advantages over those left to heal by secondary intention. A previously irradiated surgical field can result in poor-quality, firm pharyngeal tissue with a compromised blood supply that can impede wound healing, thus putting patients at risk of postoperative complications such as bleeding, dysphagia, wound breakdown, and fistula. The RFFF covers the oropharyngeal defect without significantly altering the surrounding anatomy, conveying a dedicated arterial blood supply to promote wound healing and reducing the risk of postoperative complications.
Limitations
Our article presents only a small case series with a short duration of follow-up and no direct comparison to outcomes from open procedures or TORS without an RFFF. Additionally, it does not examine certain procedural details such as operating time and intraoperative blood loss which may increase when performing a large flap procedure. Transoral robotic surgery also presents issues that make adoption outside tertiary centers impractical including lack of widespread availability of robotic systems and local expertise, a steep learning curve, and the considerable expense associated with establishing and maintaining a da Vinci system. Nevertheless, these costs can be somewhat offset by reduced hospital stay, improved safety with reduced complication rates and improved functional outcomes. Transoral robotic surgery may also be limited by tumor staging and mouth opening, as large tumors with significant trismus are often not amenable to transoral excision.
Routine use of RFFF also presents additional costs as it requires prolonged operating theatre time and 2 surgical teams with expertise in robotic surgery and head and neck reconstruction. Furthermore, the RFFF exposes patients to additional complications including flap failure and pain, weakness, and altered sensation at the donor site although these issues were not demonstrated in our case series.
Conclusions
Transoral robotic surgery oropharyngectomy with robotic-assisted insertion of an RFFF is an innovative surgical technique that could help address the increasing problem of chemoradiorecurrent and residual OPSCC. Our limited case series has demonstrated the procedure can be performed with good oncological and functional outcomes, minimal reliance on tracheostomy and nasogastric feeding, and no significant immediate- or long-term complications. Future work comparing outcomes of TORS with RFFF against open approach resections and TORS without free flaps will help determine the true impact our technique on swallowing function and quality of life.
Authors’ Note Mr Andrew Williamson contributed to data collection, surgical assistant in cases, and primary author of manuscript. Mr Matthew Haywood contributed to editing of manuscript and surgical assistant in cases. Mr Zaid Awad contributed to senior author, editing of final draft of manuscript, operating surgeon responsible for patients.
Declaration of Conflicting Interests The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Mr Simon Wood worked as plastic and reconstructive consultant surgeon, Charing Cross Hospital. NHS Imperial College Healthcare head and neck oncology multidisciplinary team for their involvement in diagnosis and management of these patients.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Chaturvedi AK, Anderson WF, Lortet-Tieulent J, et al. Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers. J Clin Oncol. 2013;31(36):4550–4559.
- 2. Mehanna H, Beech T, Nicholson T, et al. Prevalence of human papillomavirus in oropharyngeal and nonoropharyngeal head and neck cancer—systematic review and meta-analysis of trends by time and region. Head Neck. 2013;35(5):747–755.
- 3. Machtay M, Moughan J, Trotti A, et al. Factors associated with severe late toxicity after concurrent chemoradiation for locally advanced head and neck cancer: an RTOG analysis. J Clin Oncol. 2008;26(21):3582–3589.
- 4. de Almeida JR, Byrd JK, Wu R, et al. A systematic review of transoral robotic surgery and radiotherapy for early oropharynx cancer: a systematic review. Laryngoscope. 2014;124(9):2096–2102.
- 5. Fakhry C, Zhang Q, Nguyen - Tan, et al. Human papillomavirus and overall survival after progression of oropharyngeal squamous cell carcinoma. J Clin Oncol. 2014;32(30):3365–3373.
- 6. Zadereo ME, Hanasono MM, Rosenthal DI, et al. The role of salvage surgery in patients with recurrent squamous cell carcinoma of the oropharynx. Cancer. 2009;115(24):5723–33.
- 7. Hutcheson K, Holsinger F, Kupferman M, Lewin JS. Functional outcomes after TORS for oropharyngeal cancer: a systematic review. Eur Arch Otorhinolaryngol. 2015;272(2):463–471.
- 8. White H, Ford S, Bush B, et al. Salvage surgery for recurrent cancers of the oropharynx: comparing TORS with standard open surgical approaches. JAMA Otolaryngol Head Neck Surg. 2013;139(8):773–778.
- 9. Dean NR, Rosenthal EL, Carroll WR, et al. Robotic-assisted surgery for primary or recurrent oropharyngeal carcinoma. Arch Otolaryngol Head Neck Surg. 2010;136(4):380–384.
- 10. Paleri V, Fox H, Coward S, et al. Transoral robotic surgery for residual and recurrent oropharyngeal cancers: exploratory study of surgical innovation using the IDEAL framework for early-phase surgical studies. Head Neck. 2018;40(3):512–525.