Introduction
The COVID-19 pandemic was a major global health crisis, significantly affecting healthcare sectors worldwide, with those in developing countries facing particularly acute challenges (; ). These regions were especially susceptible to the effects of the pandemic because of their limited healthcare resources. This scarcity was most evident in the shortfall in healthcare professionals, including physicians, nurses and allied health workers, which led to detrimental outcomes, such as high staff turnover (; ). Turnover not only affected the quality of patient care but also increased training costs and placed additional burdens on the remaining workforce (). There were also inequalities in healthcare provision and access, as rural areas often had fewer and poorly equipped facilities compared with urban areas (; ).
These long-standing issues were exacerbated by the pandemic, which highlighted the vulnerabilities inherent in the healthcare systems of developing nations. In these countries, hospitals struggled to provide health care to both COVID-19 patients and people afflicted with other medical conditions (). The strain on resources underlined critical gaps in infrastructure and the urgent need to foster the systemic resilience necessary to withstand global health emergencies. In this research study, the term “developing countries” is used, with the understanding that no globally standardised alternative currently exists ().
In response to the COVID-19 pandemic, many countries, including Saudi Arabia, implemented a range of strategies for combatting the virus, such as enforcing lockdowns, suspending flights and promoting social distancing protocols (). These measures, mainly intended to minimise physical contact, transformed daily life and posed significant challenges to the continuity of essential services, including health care. Amid this landscape, the integration of mobile health applications (m-health apps) into healthcare provision emerged as a crucial intervention.
Mobile health applications refer to smartphone-based software programmes designed to deliver, support and enhance healthcare services (; ). The m-health apps used in developing countries played a fundamental role in the management of the COVID-19 crisis, making it possible for practitioners to adeptly address the unique challenges that these regions were facing (). These applications enabled the remote provision of healthcare services, allowing for ongoing patient care and monitoring while following social distancing protocols (; ). M-health applications also contributed to the identification of COVID-19 cases by providing geographical information on infected individuals who were tracked by the applications, which helped mitigate the further spread of infections (; ). With these advantages, m-health technologies had the potential to significantly improve access to healthcare resources and services, decrease healthcare costs and reduce health inequalities (). During the COVID-19 period, various m-health apps were developed globally to meet the needs and demands of the period. Notable examples include the COVID Symptom Tracker, Corona Checker, Relief Central and Test Yourself Goa ().
In the Saudi Arabian setting, which is the focus of the study, the government provides free healthcare services to all citizens (). Saudi Arabia launched “Saudi Vision 2030,” with the Health Sector Transformation Programme as a key element aimed at reforming the healthcare system into a comprehensive, value-based model focused on public health, prevention and financial sustainability (). A central enabler of this transformation, mobile health applications, is expected to enhance healthcare productivity, integrate services, and improve patient experiences. For example, applications such as Sehhaty, Tawakkalna and Tabaud were launched and updated to enhance healthcare accessibility across the country during the pandemic (). Sehhaty provides services ranging from online consultations to e-prescriptions and booking COVID-19 tests (). Tawakkalna uses global positioning system to manage movement during curfew hours and issues special permits (; ). Tabaud aids in COVID-19 contact tracing by transmitting anonymous data to those near confirmed cases (; ).
Acceptance and adoption of m-health applications
Despite the significant benefits that m-health apps have offered, their acceptance and use among physicians in developing countries, such as Saudi Arabia, have been notably low (; ). This limitation has prompted researchers to examine the potential deterrents to the adoption of such technologies. For example, several studies have explored the factors influencing physicians’ usage of mobile health services (; ; ; ). One such factor is performance expectancy, which has been found to be critical in encouraging physicians to use m-health technologies (; ; ; ). Other factors that have been highlighted as significant in successful m-health adoption by physicians are effort expectancy, social influence (; ) and facilitating conditions (; ). Furthermore, and highlighted self-efficacy as a crucial factor in physicians’ adoption of m-health technologies, while pinpointed personal innovativeness as an important determinant. Researchers have also identified a number of major barriers to widespread m-health adoption, including technology anxiety (; ), and concerns about data security, financial incentives and patient engagement ().
While existing research has provided considerable insights into the factors affecting physicians’ behavioural intention to use m-health apps, important gaps have remained unaddressed. For example, most previous studies have predominantly employed quantitative methodologies to examine physicians’ perceptions about and acceptance of m-health apps (; ; ). Although quantitative research is valuable for probing into predefined variables and their relationships, it may not delve deeply into the nuanced factors that influence adoption, potentially overlooking unforeseen variables or emerging phenomena (; ). A quantitative approach might also fail to fully capture the complexities underlying the individual attitudes, beliefs and social contexts that are critical for comprehensively understanding m-health acceptance (). Therefore, there is a compelling case for incorporating qualitative research into investigations. Such a methodology is aimed at deriving deeper insights as well as uncovering the underlying motives, patterns and broader social and cultural dynamics at play, thereby offering a richer, more nuanced perspective on the factors influencing m-health app adoption among physicians (; ). Moreover, understanding is lacking as to how the demands emerging due to global health emergencies, such as the COVID-19 pandemic, influence healthcare professionals’ attitudes and usage of digital health technologies in these settings (). The current crisis has highlighted opportunities and obstacles related to the use of m-health applications in emergency situations, emphasising the importance of understanding professionals’ motivations and barriers with respect to using these technologies. Illuminating these issues is crucial, as it can offer invaluable guidance on improving m-health adoption and thereby better prepare healthcare systems for future health crises.
In the Saudi Arabian setting, which is the focus of the current research, most existing studies have explored patients’ behavioural intention to adopt m-health technologies (; ). For example, investigated the factors influencing patients’ adoption of mobile health applications. The authors found that key determinants, such as effort expectancy, social influence and healthcare authority enforcement, significantly affect patients’ intention to use these technologies. However, limited attention has been paid to the perspectives of physicians, despite these professionals being a vital link in treatment pathways for patients (). Physicians considerably influence m-health adoption, with patients more likely to use apps recommended by their healthcare providers ().
Technology acceptance frameworks
Theories and models of technology acceptance are conceptual frameworks developed to understand and predict the adoption and use of new technologies by individuals and organisations (). In the rapidly evolving world of technology, it is crucial to comprehend why some innovations are embraced enthusiastically, while others are met with resistance or indifference (). Using theories and models for this purpose enables stakeholders to design more user-centric technologies, tailor implementation strategies, and address barriers to adoption, ultimately increasing acceptance and successful technology integration ().
One of the most comprehensive and widely recognised models in the field is the Unified Theory of Acceptance and Use of Technology (UTAUT), proposed by . The UTAUT integrates elements from various technology acceptance theories, aiming to offer a unified framework for understanding the factors influencing individuals’ acceptance and use of technology in organisational settings (). This model identifies four key determinants of technology acceptance: performance expectancy, effort expectancy, social influence and facilitating conditions. Additionally, it considers moderating factors such as gender, age, experience and voluntariness of use.
In contrast to previous theories and models that primarily focus on individual attitudes and perceptions, the UTAUT model considers wider organisational and sociocultural determinants of decisions regarding technology adoption, making it highly relevant for studies involving employees, such as physicians (; ; ). Though there are other acceptance models such as Theory of Reasoned Action, Technology Acceptance Model (TAM), Theory of Planned Behaviour (TPB), Combined model of TAM and TPB (C-TAM-TPB), Motivational Model, model of Personal Computer Utilisation, Social Cognitive Theory and Innovation Diffusion Theory, but established that UTAUT outperformed these models by explaining as much as 70% of the variance in behavioural intention and 50% in technology use. This makes the UTAUT model standout justifying its robust explanatory power.
The study aimed to extend the original UTAUT by exploring additional factors specific to the Saudi Arabia context. By incorporating qualitative methods alongside the main determinants of UTAUT, the research seeks to identify context-specific influences on physicians’ acceptance and use of m-health technologies, offering a more comprehensive framework for understanding technology adoption in health care (Figure 1).
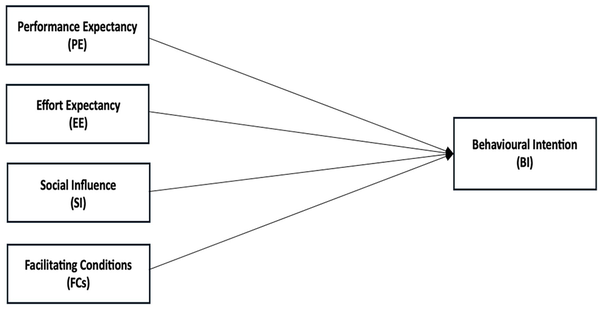
Figure 1
The conceptual model, adapted from the UTAUT ().
UTAUT: Unified Theory of Acceptance and Use of Technology.
Prevalent technology acceptance theories and models, including the UTAUT, are predominantly created and validated in developed countries (). However, emphasised that it is necessary to incorporate qualitative methodologies into UTAUT-based quantitative studies on developing regions. Prior research has highlighted the comprehensiveness of the UTAUT model in predicting the behavioural intentions of users toward information technology in developing nations (; ; ). Similar to , these studies suggest including qualitative methods in explorations to uncover additional acceptance-related factors that the model may not capture on its own or factors that might not be as pronounced in Western settings. The insights derived can significantly enhance the applicability and effectiveness of the UTAUT model in diverse geographical and cultural contexts.
Aims
The current study aimed to explore the factors that influenced the acceptance and adoption of m-health apps by physicians in Saudi Arabia during the COVID-19 pandemic, across both public and private hospitals. This research seeks to identify the key facilitators and barriers of m-health adoption in Saudi Arabia, with the goal of informing strategies to enhance the use of these technologies in healthcare settings within the country.
Method
Research approach and design
The study employed a qualitative research method. It was guided by the UTAUT. The study collected data through semi-structured interviews with physicians to delve into the determinants of their readiness to adopt m-health technologies.
Sampling and data collection
As the study aimed to uncover additional factors influencing physicians’ behavioural intentions to accept and adopt m-health applications – factors not addressed by the UTAUT model – purposive sampling was employed. This approach specifically targeted physicians who were early adopters of m-health technology or have unique perspectives on its implementation. By focusing on these key participants, the study gathered rich, qualitative data, offering insights into the specific factors these physicians encounter in their practice. The inclusion criteria required participants to be licensed physicians practising in Saudi Arabia during the COVID-19 pandemic. The job description criteria for the physicians selected in this study were based on their active involvement in patient care, clinical decision-making and use of m-health applications. Their roles in prescribing treatments and managing patient health made them key stakeholders in m-health adoption. Focusing on licensed physicians in Saudi Arabia during the COVID-19 pandemic ensured that participants had practical experience with these technologies, making their insights critical to the aim of this study. On the other hand, non-Saudi physicians were excluded to focus on those fully integrated into Saudi Arabia’s healthcare system, culture and regulations. This ensures the data reflect local physicians’ experiences, making the findings more applicable to Saudi healthcare policies and decision-making.
In qualitative research, sample size is determined predominantly on the basis of data saturation, which means that data collection continues until no additional themes that affect the understanding of the pursued research question emerge (). Empirical studies suggest that data saturation is typically achieved within a range of 9–17 interviews, particularly when working with narrowly defined research objectives (). In this study, Saudi physicians were interviewed until data saturation was reached, with a total of 16 physicians participating. These physicians were drawn from various public and private healthcare institutions across Saudi Arabia, ensuring a diverse representation from different sectors of the healthcare delivery system. The reason for focusing solely on physicians is that the study aimed to explore the perspectives of medical practitioners who directly prescribe and manage patient care using m-health technologies, making their insights particularly relevant to m-health adoption. Informed consent was obtained electronically from all participating Saudi physicians before their interviews.
The development of the interview guide was informed by a literature review on m-health acceptance and adoption by physicians (). The interview guide was piloted with four physicians prior to the main data collection phase. Feedback from this pilot phase was used to adjust the questions for clarity and relevance, ensuring the final interview guide aligned with the research aim. This guide included an introduction that defined and described m-health apps to ensure that the participants were aware of the technologies being studied. The interview guide was initially developed in English and subsequently translated into Arabic, the official language of Saudi Arabia, to ensure full comprehension by all participants. The questions were divided into two main categories: those on demographic information (i.e. gender, age, specialisation), and those to be presented during the interview proper. The latter were subdivided into three questions, namely, general open-ended, in-depth and closing questions. In the general open-ended questions, participants were asked about their overall awareness of m-health, whether such applications had been used by them, and any barriers or facilitators encountered in using m-health technologies. Based on their responses, follow-up prompts were used to further explore these areas. The in-depth questions were focused on specific aspects, including data privacy and security concerns, financial incentives, patient involvement and the influence of organisational culture on the adoption of m-health apps. Finally, the closing questions allowed participants to mention any additional factors or concerns they felt were relevant but had not been discussed during the interview. This structure ensured that both general and context-specific factors influencing participants’ perspectives on m-health were comprehensively explored, with prompts used to facilitate deeper inquiry into key themes, thereby enhancing the richness of the qualitative data. All the interviews were scheduled and conducted using Zoom, and each lasted for 20–40 minutes. All interviews were conducted by the first author.
Data analysis
The interviews were audio-recorded and then transcribed prior to data analysis. The transcription was conducted using NVivo software Version 14, which facilitated the organisation and coding of the data. The transcribed data were then examined using template analysis, a systematic and flexible approach that has become increasingly popular for the management and examination of qualitative data (). A significant benefit of template analysis lies in its facilitation of both inductive and deductive methods, thereby allowing for an exhaustive and multifaceted approach to research (). This framework entails many steps: data familiarisation, preliminary coding, clustering, initial template development, template modification, final template definition and template use for data interpretation (). Researchers familiarise themselves with the data of interest by poring over raw data before beginning the coding process, ensuring a thorough grasp of each participant’s experience. Preliminary coding involves marking relevant text segments and using a priori themes based on theoretical constructs or previous studies. In this stage, the study employed the UTAUT model, along with the findings from the literature review, to define a priori themes (). These themes provided a structured basis for identifying relevant data segments but were subject to adjustment as the analysis progressed, reflecting the dynamic nature of qualitative template analysis. Clustering follows, which involves grouping coded segments to identify and refine the a priori themes into meaningful categories. The initial template is then developed by synthesising the defined clusters and their themes into an organised template, providing a clear framework for analysing the data. The template may be adjusted during the analysis by refining, combining or subdividing themes to accurately represent the nuances of the data. Finalising the template establishes a structure for interpreting the complete dataset, ensuring an in-depth analysis. The final step is applying the refined template to the dataset, facilitating a thorough and systematic exploration of the themes identified and thereby generating meaningful insights relevant to the research objectives.
Ethics approval
Ethical approval for the research was granted by the ethics committee of the University of Technology Sydney (UTS HREC REF NO. ETH21-6751).
Results
Participant characteristics
The participant group comprised 10 men and 6 women physicians. The physicians’ age distribution was as follows: One physician belonged to the age group of 25–30 years, the majority (11 physicians) belonged to the age group of 31–40 years, and four physicians belonged to the age group of 41–50 years. In terms of specialisation, most of the physicians (12) were general practitioners, three were in family medicine, and one was an urologist. With regard to work settings, four physicians were employed in the primary healthcare sector under the Ministry of Health, the majority (10 physicians) worked in hospitals also overseen by the Ministry of Health, and two were from the military sector.
Results of the template analysis
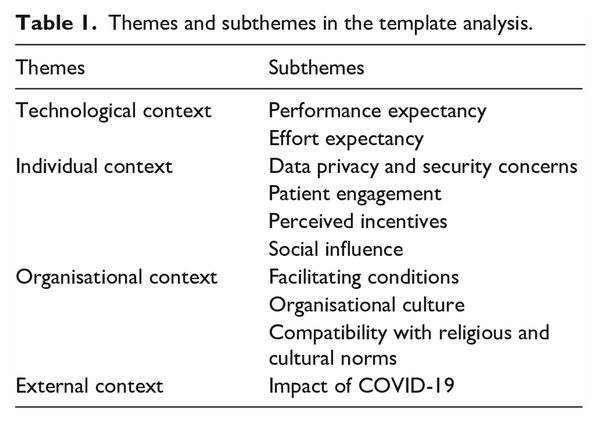
The final template included four themes: technological, individual, organisational and external contexts (Table 1). These themes and subthemes are described in detail in the following sections.
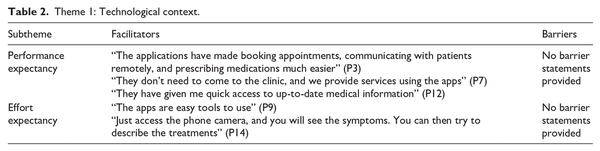
Theme 1: Technological context
Technological context was related to the technical aspects of m-health apps and encompassed two subthemes: performance expectancy and effort expectancy (see Table 2).
Performance expectancy
Performance expectancy refers to the degree to which physicians believe that using m-health apps will improve their job performance. The participating physicians acknowledged that m-health apps have significantly enhanced healthcare delivery in various respects. Specifically, they have transformed patient access to healthcare services by simplifying procedures such as booking appointments, prescribing medications and facilitating remote clinical consultations: “The applications have made booking appointments, communicating with patients remotely, and prescribing medications much easier” (P3). These apps have also considerably reduced the need for physical visits among patients who do not require face-to-face consultations: “They don’t need to come to the clinic, and we provide services using the apps” (P7). Finally, they have improved the physicians’ access to up-to-date information, thus supporting clinical decision-making: “They have given me quick access to up-to-date medical information” (P12).
Effort expectancy
Effort expectancy pertains to the ease with which m-health apps are used. The physicians found these applications user-friendly and effective, particularly in facilitating remote consultations: “The apps are easy tools to use” (P9) and “Just access the phone camera, and you will see the symptoms. You can then try to describe the treatments” (P14).
Theme 2: Individual context
This theme focused on the individual-level factors influencing physicians’ decision-making regarding using m-health apps. It was divided into four subthemes: data privacy and security concerns, patient engagement, perceived incentives and social influence (see Table 3).
Data privacy and security concerns
The physicians expressed varied perceptions regarding data privacy and security in m-health apps. On the one hand, some felt confident about the security measures provided in the apps, emphasising the robustness of current cybersecurity systems against major breaches or complaints: “Mobile health apps are in compliance with rigorous data protection laws. . . . I’m pretty sure about patient data confidentiality” (P2). On the other hand, others shared prevalent concerns about hacking, unauthorised access to patient information, and the management of data by third parties: “The most important problem is data hacking and access to patient information. . . . how these applications store and deal with data, especially when sharing this information with third parties” (P10).
Patient engagement
The level of patient involvement with m-health apps affected participants’ adoption of these technologies. They were motivated to incorporate the apps into their practice when their patients actively used these tools: “When patients are passionate about mobile health applications, it really motivates me” (P2). Positive patient feedback also encouraged the physicians to use the technologies more broadly: “One of my patients has been using this app . . . this discipline in the use of the app has helped us both monitor her condition better” (P11). However, challenges in patient engagement existed, particularly among elderly patients. The lack of comfort and familiarity with these technologies drove a preference for face-to-face consultations: “Patients, especially older people, are less comfortable with these apps and prefer to come to the hospital” (P13).
Perceived incentives
Financial incentives emerged as a crucial factor for adoption. The physicians recognised that such rewards can increase efficiency and motivation, especially when associated with improvements in patient care: “Financial rewards play a big role, especially when they’re associated with significant improvements in patient care . . . the doctor becomes more productive because of financial compensation, but it also helps improve patient outcomes” (P3). Some of them expressed the belief that offering financial incentives may effectively motivate older physicians, who tend to be hesitant about adopting new technologies: “If there is a financial incentive, the use of apps will increase, especially among older colleagues” (P1).
Social influence
The impact of colleagues and professional networks was key to the physicians’ decision to adopt m-health apps. They were more likely to use these solutions when they saw their peers using them successfully, which was a powerful motivational factor: “When I see other doctors using m-health apps successfully, it motivates me to use them too” (P5) and “I began using this app after a colleague suggested it at a conference” (P16).
Theme 3: Organisational context
Organisational context was related to the role of healthcare organisations in promoting m-health apps. This theme was divided into three subthemes: facilitating conditions, organisational culture and compatibility with religious and cultural norms (see Table 4).
Facilitating conditions
Facilitating conditions refer to the degree to which individuals believe that an existing organisational and technical infrastructure supports the use of m-health apps. The level of support provided by healthcare organisations, including technical assistance and training, substantially influenced the physicians’ attitudes towards using m-health apps. Several technical issues were a common concern among them. Some faced difficulties with system reliability, including account crashes, unstable applications and cumbersome database interfaces, which can disrupt healthcare delivery: “Sometimes having trouble in communication. . . . trouble with the Internet and the database, and technical issues, like account crashes and problems creating new accounts” (P10). Furthermore, issues of integrating m-health apps and current healthcare systems existed, which often led to increased workloads and inefficiencies: “The apps require doctors to work long hours to add patient data because there is no integration between applications and medical records” (P15). The absence of integration disrupted the smooth progression of patient care, as physicians faced difficulties in obtaining comprehensive patient histories: “When patient data is not connected to an entire health system. . . . I cannot provide complete care to patients, as I do not know their histories” (P8).
Organisational support facilitates the effective incorporation of m-health technologies into daily health practices, enhancing physicians’ confidence in and willingness to use these innovations: “Hospital support contributes positively to the effective incorporation of these technologies into our health practices” (P3). Thus, technical support was highly regarded by the respondents because it advances sustained operation and minimises interruptions resulting from technical complications, thereby reducing physician complaints: “If a technical team is available who can provide immediate support, that motivates me to use the apps” (P6). Training from healthcare organisations was also seen as a fundamental source of encouragement for the use of these apps. It effectively reduced the concerns of clinicians regarding the technologies, enhanced their comfort levels, and promoted wider implementation: “Training helps overcome any reservations or concerns that doctors may have about the technology, facilitating its wider adoption” (P11).
Organisational culture
The culture in healthcare organisations was another significant driver of adoption. The presence of a traditional culture that places value on conventional practices may engender resistance to new technologies and limit the utilisation of these applications. This impediment stems from the fact that decision-makers might not support the integration of these technologies into healthcare practices: “If the culture in a hospital favours traditional methods, with resistance against adopting modern technology, then surely I will not use the technology” (P8). In contrast, an organisational environment that promotes technological innovation can substantially enhance the acceptance of m-health apps. Physicians are more likely to adopt and effectively use these digital technologies when the workplace encourages the integration of new technologies: “When the culture in a hospital encourages innovation, accepts technology, and appreciates the need for continuous improvement, this motivates me to use applications effectively” (P11).
Compatibility with religious and cultural norms
Cultural norms and religious practices substantially affect the level of acceptability and utilisation of m-health applications. The physicians observed that enabling patients to choose the gender of their healthcare providers through the app significantly enhances user comfort and supports the use of the app. Many female patients prefer female doctors when seeking medical assistance for gynaecological difficulties or general health concerns given considerations of modesty. This feature not only corresponds with cultural and religious norms but also promotes a more open and trusting environment, improving the quality of physician–patient interactions: “Being able to choose a provider’s gender has really affected patient comfort. It is important for patients, especially women, to feel comfortable during medical consultations for cultural and religious reasons” (P3). In addition, applications should accommodate religious practices through features that, for example, automatically adjust medication reminders during Ramadan when patients are fasting “Features that cater to religious practices are important. It helps our patients keep up with their treatments while they fulfil their religious duties” (P7).
Theme 4. External context
The primary focus of external context was the effects of the COVID-19 pandemic on the adoption of m-health apps. It was intended to capture how the global outbreak has influenced Saudi physicians’ perceptions of m-health apps (see Table 5).
Impact of COVID-19
Before the COVID-19 pandemic, some of the physicians preferred face-to-face consultations, but the crisis has changed their perspectives, driving them to reconsider the use of mobile health technologies: “I’ve always preferred and liked to give advice face-to-face in my own office” (P4). The ensuing social distancing measures highlighted the crucial role and necessity of these innovations in maintaining continuous patient care: “The crisis necessitated a shift to telehealth. . . . This transformation has played a major role in maintaining patient care while adhering to social distancing guidelines” (P7).
Discussion
Summary of main findings
This research represents a pioneering qualitative investigation into determinants of the acceptance and adoption of m-health apps by physicians in developing countries during the COVID-19 pandemic, with a specific focus on Saudi Arabia. Unlike the majority of prior studies, which have adopted quantitative methodologies in combination with the UTAUT model (; ; ; ; ), the current research enhanced the existing framework by integrating both core and peripheral determinants that have been less emphasised in traditional models such as the UTAUT. By employing a qualitative approach, we examined how physicians in a developing country have perceived and prioritised these additional factors amid an unprecedented global health crisis. The results offer valuable insights that can guide the development of targeted strategies for enhancing m-health integration in Saudi Arabia and similar developing countries. They also contribute to the literature by validating known determinants, such as the UTAUT factors, within the unique context of Saudi Arabia. Additionally, they identify context-specific factors influencing m-health adoption, including compatibility with religious and cultural norms, data privacy and security concerns, patient engagement and organisational culture. This advancement emphasises the necessity of modifying and expanding traditional technology adoption frameworks to better align with the realities faced by healthcare professionals in Saudi Arabia and similar contexts (Figure 2).
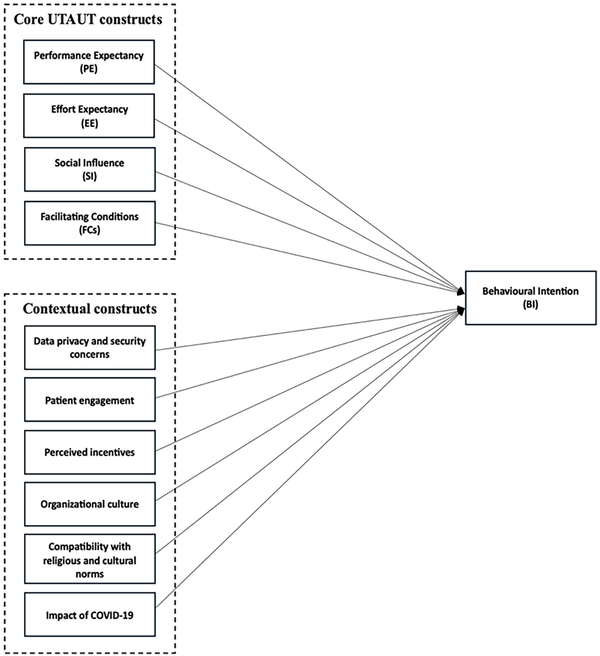
Figure 2
Extended UTAUT model for mHealth adoption in Saudi Arabia.
UTAUT: Unified Theory of Acceptance and Use of Technology.
Core constructs of the UTAUT model
This subsection presents our exploration of the fundamental components of the UTAUT model in relation to m-health adoption by Saudi physicians: performance expectancy, effort expectancy, social influence and facilitating conditions. By exploring how these core components are validated and manifested in the local context, we illuminated the fundamental drivers of technology adoption among healthcare professionals.
Performance expectancy and effort expectancy critically affected the adoption of m-health apps by the Saudi physicians. Such adoption was driven by the physicians’ recognition of the enhancement in healthcare services made possible by m-health, which aligns with prior research (; ; ; ). Perceived improvements in efficiency and patient care were central to their acceptance, underscoring the need for developers to enhance app functionality and reliability. The respondents also indicated the importance of user-friendly interfaces, consistent with earlier studies (; ; ). Thus, simplifying user interfaces and ensuring the intuitive use of these apps can increase their usage.
The study also established the importance of social influence in the adoption of m-health apps among Saudi physicians, again in line with the literature (; ). Physicians sometimes rely on their colleagues’ experiences and achievements as motivation for incorporating new technologies into their own practices. Therefore, leveraging social influence through ambassador programmes or peer endorsements can enhance the adoption of m-health apps among healthcare professionals. Facilitating conditions also exerted a significant impact on the adoption of new technologies. Our findings, in line with previous studies (; ), demonstrated that robust technical support and comprehensive training are crucial determinants of physicians’ attitudes towards m-health apps. Providing ongoing support and training may reduce the concerns that physicians may have about using these technologies, making it easier for them to incorporate these tools into their regular routines.
Extension of the UTAUT in Saudi Arabia and similar contexts
This subsection discusses our extension of the conventional UTAUT model to consider additional factors that significantly influence the adoption of m-health apps in settings such as Saudi Arabia. These factors are compatibility with religious and cultural norms, data privacy and security concerns, patient engagement, organisational culture and the impact of the COVID-19 pandemic. This analysis emphasises how adapting and expanding the model advances a more comprehensive understanding of technology adoption in diverse sociocultural landscapes.
We found that compatibility with religious and cultural norms is a vital factor for m-health acceptance and adoption in Saudi Arabia, where Islamic traditions strongly influence societal behaviours and everyday life (). This crucial determinant is disregarded in the original UTAUT model (), yet it is essential for the acceptance and utilisation of m-health applications in these regions. Features such as enabling patients to select the genders of their healthcare providers and modify medication reminders in line with religious observances cater to cultural sensitivities. These features not only enhance patient comfort but also improve the quality of physician–patient interactions, leading to more effective consultations, better diagnosis and treatment adherence, and ultimately higher patient satisfaction and health outcomes. Unlike the previous studies (; ; ), this study found that an organisational culture that embraces technological innovation can facilitate the adoption of new technologies. Healthcare organisations that promote ongoing education and a culture conducive to innovation are more likely to enjoy increased technology adoption rates among their personnel.
Data privacy and security concerns, patient engagement and perceived incentives likewise significantly influence the use of m-health technologies in Saudi Arabia. Conflicting attitudes towards data security highlight the necessity for rigorous data protection procedures in order to enhance trust among healthcare professionals, as noted in other studies (). Thus, the establishment of strong data protection measures is critical, as these not only foster confidence among healthcare professionals but also ensure the security of patient data and maintain the integrity of healthcare services, thereby enhancing m-health utilisation. The participants also reported that the active participation of patients plays a crucial role in motivating healthcare professionals to adopt new technologies, consistent with prior studies (). Ensuring that patient needs and preferences are met can enhance patient involvement, thereby encouraging professionals to integrate these technologies into their practice. Moreover, this study supports the findings of previous research that illustrated the value of financial incentives in encouraging the integration of technology into healthcare environments ().
Finally, the COVID-19 pandemic has accelerated significant transformations in healthcare industries worldwide, particularly in Saudi Arabia, where physicians have exhibited major changes in their perspectives on m-health apps. This shift aligns with findings from previous studies that suggested the pandemic accelerated the shift toward the use of m-health technologies and emphasised the significance of these innovations in maintaining continuous healthcare provision during crises (; ). Specifically, these technologies have been increasingly acknowledged as instrumental to maintaining healthcare service provision when conventional in-person consultations are rendered impossible by lockdowns and social distancing protocols.
Theoretical and practical implications
This study enhances the theoretical and practical understanding of the acceptance and adoption of m-health apps in developing countries, including Saudi Arabia, particularly amid global health emergencies, such as the COVID-19 pandemic. By integrating qualitative insights into the UTAUT framework and identifying additional context-specific factors, this research highlighted the need for technological acceptance theories to be adapted to the sociocultural and economic realities of developing nations to better reflect their unique circumstances. The aim of the study – to broaden the UTAUT model by incorporating factors such as cultural compatibility, data privacy concerns and organisational support – was successfully achieved. The insights derived also underscored the value of qualitative research methods in capturing the nuanced drivers of adoption, enabling a deeper grasp of the factors that influence m-health uptake among physicians in Saudi Arabia and similar contexts.
From a practical perspective, this study offers actionable recommendations for policymakers, healthcare managers and m-health app developers. These stakeholders should implement several key strategies. First, they should develop m-health apps underlain by respect for cultural and religious norms. For instance, these apps should allow patients to choose their providers’ genders and adjust reminders on the basis of religious practices. Second, policymakers should strengthen data privacy by enforcing stricter protection laws and conducting regular audits to build trust. Third, patient engagement should be enhanced by creating features (e.g. personalised health monitoring) that motivate healthcare professionals to adopt m-health technologies. Additionally, fostering a culture of innovation within healthcare organisations through training programmes and peer support will encourage greater technology use. Financial incentives, such as subsidies and rewards for m-health adoption, should also be considered. Finally, comprehensive ongoing training and technical support are essential to ensure the ease of use and successful integration of these technologies into daily practice. By integrating the abovementioned theoretical and practical implications, the study not only advances academic discourse but also provides concrete steps for improving the implementation and acceptance of m-health technologies in diverse healthcare environments.
Limitations and directions for future research
While this study shed light on the factors influencing the acceptance and adoption of m-health apps among physicians in Saudi Arabia, several limitations must be acknowledged. To begin with, the research focused primarily on the perspectives of physicians and did not include the valuable insights that can be gained from other healthcare professionals, such as nurses, allied health workers and healthcare administrators. Exploring these voices in future research would enable a more comprehensive understanding of the barriers and facilitators of m-health adoption across the entire healthcare workforce. Patients’ perspectives are also critical, as their engagement and satisfaction are essential to the successful integration of m-health technologies. By expanding the scope to include both healthcare providers and patients, future studies can offer a fuller picture of m-health adoption, helping to address a broader spectrum of needs and challenges. Additionally, this study is specific to Saudi Arabia, a country with unique cultural, religious and organisational characteristics. Although it derived insights relevant to similar developing countries, caution should be exercised when generalising the results to regions with different sociocultural and healthcare landscapes. Future research can examine m-health adoption in diverse settings to compare how different cultural and organisational contexts influence the success of these technologies.
Another limitation is the focus on the short-term adoption of m-health technologies during the COVID-19 pandemic. While this study illuminated how healthcare professionals respond to m-health issues during a crisis, it did not account for the long-term outcomes of using these applications. Other researchers should investigate the lasting effects of m-health app usage on healthcare delivery, patient outcomes and overall system efficiency. Longitudinal studies can explore whether the benefits observed during the pandemic persist and how these technologies evolve to meet ongoing healthcare needs.
Moreover, the current research employed a qualitative approach, concentrating on in-depth interviews with a select group of physicians. Although this method allows for a nuanced understanding of individual experiences, it may limit the generalisability of findings to broader healthcare populations. Future studies would benefit from using mixed methods or larger, more diverse quantitative surveys to capture a wider range of opinions and enhance generalisability. Addressing these limitations and broadening the scope of future research will not only facilitate the more effective integration of these technologies into healthcare systems globally but also ensure that solutions are adaptable to the unique needs of different healthcare environments.
Conclusion
This study explored the factors that influenced physicians’ acceptance and adoption of m-health in Saudi Arabia during the COVID-19 pandemic on the basis of the UTAUT model, which was enhanced through the incorporation of additional critical factors for m-health app adoption. Beyond encompassing the UTAUT’s focus on performance expectancy, effort expectancy, social influence and facilitating conditions, our study highlighted the critical roles of compatibility with religious and cultural norms, organisational culture, data privacy and security concerns, patient engagement, perceived incentives, organisational support and the impact of COVID-19 in adoption. It is important to address these factors to promote the successful integration of m-health apps into clinical practice. This study also emphasised the importance of a tailored approach to the use of technology adoption frameworks to better fit the cultural and organisational contexts of Saudi Arabia and similar developing countries.
The aim of this study was successfully achieved, as it not only validated traditional UTAUT factors but also identified critical context-specific determinants that influence m-health adoption in Saudi Arabia. This comprehensive approach clarified how m-health technologies can be better tailored to suit the unique sociocultural and organisational landscapes of developing nations, particularly those similar to Saudi Arabia. To apply the findings of this study, relevant stakeholders should address data privacy concerns, enhance patient engagement, provide financial incentives and ensure extensive training on m-health usage. Fostering a culture of technological innovation within healthcare institutions is equally essential. In developing countries, such strategies are critical for overcoming the barriers to m-health adoption, and they improve healthcare delivery and outcomes.
Accepted for publication November 1, 2024
Author note Sultan Alsahli was awarded a Doctor of Philosophy (PhD) scholarship by Umm Al-Qura University through the Saudi Arabian Cultural Mission in Australia. All authors have approved the final version of the manuscript.
Author contributions Sultan Alsahli, the first author: conceptualisation, methodology, investigation, writing – original draft. Mary Lam and Su-yin Hor: supervision, review – editing.
Declaration of conflicting interests The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding The authors received no financial support for the research, authorship and/or publication of this article: This work was supported by Umm Al-Qura University, facilitated through the Saudi Arabian Cultural Mission in Australia.
Sultan Alsahli, MSc
https://orcid.org/0009-0001-8549-8340
Su-yin Hor, PhD
https://orcid.org/0000-0002-6498-9722
Mary K Lam, PhD
https://orcid.org/0000-0001-9451-8203
References
- Addotey-Delove M, Scott RE, Mars M (2023) Healthcare workers’ perspectives of mHealth adoption factors in the developing world: Scoping review. International Journal of Environmental Research and Public Health 20(2): 1244.
- Adetunji CO, Olaniyan OT, Adeyomoye O, et al. (2022) eHealth, mHealth, and telemedicine for COVID-19 pandemic. In: Pani SK, Dash S, dos Santos WP, et al. (eds) Assessing COVID-19 and Other Pandemics and Epidemics using Computational Modelling and Data Analysis. Cham: Springer International Publishing, pp.157–168.
- Alanzi T (2021) A review of mobile applications available in the App and Google play stores used during the COVID-19 outbreak. Journal of Multidisciplinary Healthcare 14: 45–57.
- Al-Hanawi MK (2021) Socioeconomic determinants and inequalities in the prevalence of non-communicable diseases in Saudi Arabia. International Journal for Equity in Health 20(1): 174.
- Aljohani N, Chandran D (2021) Factors affecting the adoption of M-health applications in Saudi Arabia: Impact of healthcare authority enforcement. In Pacific Asia Conference on Information Systems. Dubai, UAE: Association for Information Systems.
- Alsahli S, Hor S-y (2024) The adoption of mobile health applications by physicians during the COVID-19 pandemic in developing countries: The case of Saudi Arabia. International Journal of Information Management Data Insights 4(2): 100289.
- Alsahli S, Hor S-Y, Lam M (2023) Factors influencing the acceptance and adoption of mobile health apps by physicians during the COVID-19 pandemic: Systematic review. Journal of Medical Internet Research mHealth and uHealth 11: e50419.
- Alsheddi A, Sharma D, Talukder M (2020) Impact of users’ socio-cultural and religious orientation on government resource planning (GRP) systems usage in Saudi Arabia. Institute of Electrical and Electronics Engineers Access 8: 122722–122735.
- Alsswey A, Al-Samarraie H, Bervell B (2021) mHealth technology utilization in the Arab world : A systematic review of systems, usage, and challenges. Health and Technology 11(4): 895–907.
- Alzahrani AI, Al-Samarraie H, Eldenfria A, et al. (2022) Users’ intention to continue using mHealth services: A DEMATEL approach during the COVID-19 pandemic. Technology in Society 68: 101862.
- Asadzadeh A, Kalankesh LR (2021) A scope of mobile health solutions in COVID-19 pandemics. Informatics in Medicine Unlocked 23: 100558.
- Azam M, Bin Naeem S, Kamel Boulos MN, et al. (2023) Modelling the predictors of mobile health (mHealth) adoption among healthcare professionals in low-resource environments. International Journal of Environmental Research and Public Health 20(23): 7112.
- Bawack RE, Kala Kamdjoug JR (2018) Adequacy of UTAUT in clinician adoption of health information systems in developing countries: The case of Cameroon. International Journal of Medical Informatics 109: 15–22.
- Bhatt V, Chakraborty S (2022) Intrinsic Antecedents to mHealth Adoption Intention. International Journal of Electronic Government Research 18(2): 1–17.
- Bolan N, Cowgill KD, Walker K, et al. (2021) Human resources for health-related challenges to ensuring quality newborn care in low- and middle-income countries: A scoping review. Global Health: Science and Practice 9(1): 160–176.
- Busetto L, Wick W, Gumbinger C (2020) How to use and assess qualitative research methods. Neurological Research and Practice 2(1): 14.
- Chahal S, Biln N, Clarke B (2021) Patient perspectives on a digital mobile health application for RA. Open Access Rheumatology: Research and Reviews 13: 63–71.
- Creswell JW, Creswell JD (2023) Research design : Qualitative, quantitative, and mixed methods approaches. Thousand Oaks, CA: Sage Publications, Inc.
- Della Vecchia C, Leroy T, Bauquier C, et al. (2022) Willingness of French general practitioners to prescribe mhealth apps and devices: Quantitative study. Journal of Medical Internet Research mHealth and uHealth 10(2): e28372.
- Diel S, Doctor E, Reith R, et al. (2023) Examining supporting and constraining factors of physicians’ acceptance of telemedical online consultations: A survey study. BioMed Central Health Services Research 23(1): 1128.
- Glass JE, Matson TE, Lim C, et al. (2021) Approaches for implementing app-based digital treatments for drug use disorders into primary care: A qualitative, user-centered design study of patient perspectives. Journal of Medical Internet Research 23(7): e25866.
- Hassounah M, Raheel H, Alhefzi M (2020) Digital response during the COVID-19 pandemic in Saudi Arabia. Journal of Medical Internet Research 22(9): e19338.
- Hennink M, Kaiser BN (2022) Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Social Science & Medicine 292: 114523.
- Holderried TA, Hecker K, Reh L, et al. (2023) The potential of eHealth for cancer patients–does COVID-19 pandemic change the attitude towards use of telemedicine services? Public Library of Science 18(2): e0280723.
- Jin X, Yuan Z, Zhou Z (2023) Understanding the antecedents and effects of mHealth app use in pandemics: A sequential mixed-method investigation. International Journal of Environmental Research and Public Health 20(1): 834.
- Khokhar T, Serajuddin U (2015) Is the Term ‘Developing World’ Outdated? Available at: https://www.weforum.org/agenda/2015/11/is-the-term-developing-world-outdated/ (accessed 22 September 2024).
- King N, Brooks J, Tabari S (2018) Template analysis in business and management research. In: Ciesielska M, Jemielniak D (eds) Qualitative Methodologies in Organization Studies: Volume II: Methods and Possibilities. Cham: Springer International Publishing, pp.179–206.
- Lee W-I, Fu H-P, Mendoza N, et al. (2021) Determinants impacting user behavior towards emergency use intentions of m-health services in Taiwan. Healthcare 9(5): 535.
- Levin AT, Owusu-Boaitey N, Pugh S, et al. (2022) Assessing the burden of COVID-19 in developing countries: Systematic review, meta-analysis and public policy implications. BMJ Global Health 7(5): e008477.
- Li S, Zhou Y, Kundu T, et al. (2021) Impact of entry restriction policies on international air transport connectivity during COVID-19 pandemic. Transportation Research Part E: Logistics and Transportation Review 152: 102411.
- Lim J (2021) Characteristics of elderly care work that influence care workers’ turnover intentions. Healthcare 9(3): 259.
- Mahendradhata Y, Andayani NLPE, Hasri ET, et al. (2021) The capacity of the Indonesian healthcare system to respond to COVID-19. Frontiers in Public Health 9:649819.
- Ming LC, Untong N, Aliudin NA, et al. (2020) Mobile health apps on COVID-19 launched in the early days of the pandemic: Content analysis and review. Journal of Medical Internet Research mHealth and uHealth 8(9): e19796.
- Momani A (2020) The unified theory of acceptance and use of technology: A new approach in technology acceptance. International Journal of Sociotechnology and Knowledge Development 12(3): 79–98.
- Saudi Vision (2020) Health Sector Transformation Program. Available at: https://www.vision2030.gov.sa/en/explore/programs/health-sector-transformation-program (accessed 10 April 2024).
- Shah A, Jhanjhi N, Humayun M, et al. (2022) Health Care Digital Revolution During COVID-19. In: Anandan R, Suseendran G, Chatterjee P, et al. (eds) How COVID-19 is accelerating the digital revolution. Cham: Springer International Publishing, , pp.17–30.
- Sharifian R, Askarian F, Nematolahi M, et al. (2014) Factors influencing nurses’ acceptance of hospital information systems in Iran: Application of the unified theory of acceptance and use of technology. Health Information Management Journal 43(3): 23–28.
- Shiferaw KB, Mengiste SA, Gullslett MK, et al. (2021) Healthcare providers’ acceptance of telemedicine and preference of modalities during COVID-19 pandemics in a low-resource setting: An extended UTAUT model. Public Library of Science 16(4): e0250220.
- Sohn K, Kwon O (2020) Technology acceptance theories and factors influencing artificial Intelligence-based intelligent products. Telematics and Informatics 47: 101324.
- Swidi AKA, Faaeq MK (2019) How robust is the UTAUT theory in explaining the usage intention of e-government services in an unstable security context?: A study in Iraq. Electronic Government, an International Journal 15(1): 37.
- Venkatesh V, Brown SA, Bala H (2013) Bridging the qualitative-quantitative divide: Guidelines for conducting mixed methods research in information systems. Management Information Systems Quarterly 37(1): 21–54.
- Venkatesh V, Morris MG, Davis GB, et al. (2003) User acceptance of information technology: Toward a unified view. MIS Quarterly 27(3): 425–478.
- Wang Y, Li Y, Qin S, et al. (2020) The disequilibrium in the distribution of the primary health workforce among eight economic regions and between rural and urban areas in China. International Journal for Equity in Health 19(1): 1–10.
- Wu P, Zhang R, Luan J, et al. (2022) Factors affecting physicians using mobile health applications: An empirical study. BioMed Central Health Services Research 22(1): 24.
- Yang S, Chen Y, Zhou L, et al. (2021) Willingness to adopt mHealth among Chinese parents during the COVID-19 outbreak: Cross-sectional questionnaire study. Journal of Medical Internet Research mHealth and uHealth 9(1): e23155.