Introduction
The demand for both primary and revision hip arthroplasty is increasing. Revision of a cemented femoral component can be technically demanding and risks femoral canal perforation, increased operating times and blood loss. To address this problem the extended trochanteric osteotomy (ETO) has been popularised., Despite the excellent exposure to the femoral canal, this technique may be associated with complications and morbidity, such as non-union, migration of the greater trochanter fragment leading to de-functioning of the hip abductors, subsidence of the revised femoral prosthesis and possible subsequent hip instability.
The proximal femoral anterior cortical window was first described by Zweymüller et al. The window allows access to the distal portion of the cement mantle. Following cement removal, a long stem femoral component is used to bypass the cortical window by at least double the canal diameter. The cortical window is replaced and secured with cables or wires. An advantage of this technique is that it does not compromise the greater trochanter and abductor mechanism. Radiographically such cortical windows tend to incorporate from 3 to 7 months., In this paper we describe the technique and its evolution initially using a cutting slot jig and progressing to a 3D-printed patient-specific instrumented (PSI) jig.
The aim of this study was primarily to describe the technique of creating the anterior cortical femoral window using a jig, either generic or PSI, to optimise window size and allow access to the femoral canal. Secondly, we sought to determine whether bony integration of a de-vascularised cortical window occurs using computed tomography (CT). Thirdly we evaluated functional outcomes allowing context with other studies.–
Methods
Approval from the local research ethics board was obtained. A retrospective review of records and imaging for patients undergoing anterior femoral cortical windowing during revision hip arthroplasty was undertaken. All procedures were performed by the Senior author surgeon in a district hospital between 2006 and 2021. Patient demographics, diagnosis requiring revision, and the revision stem implanted were recorded.
Surgical technique
Patients were positioned in the lateral decubitus position. Whilst the technique can be applied to other surgical approaches such as the posterior approach the Senior Author’s preference is for a modified Watson-Jones. This was performed whereby the interval between tensor fascia lata and gluteus medius was enlarged by detaching the anterior portion of the gluteus medius from the greater trochanter. The femoral stem was removed from the cement mantle with the use of a burr to the cement shoulder. Then cement was removed from the proximal femur using standard methods. The skin and fascial incisions were then extended distally. Vastus lateralis was split longitudinally to allow exposure of the anterior cortex of the femur.
The position of the window was predetermined radiologically based on the length of the extracted stem. It was planned to span the distal cement mantle from the level of the inferior portion of the lesser trochanter to the proximal part of the cement plug. A Dall-Miles cable was placed approximately 1 cm inferior to the planned window position to prevent possible distal fracture propagation.
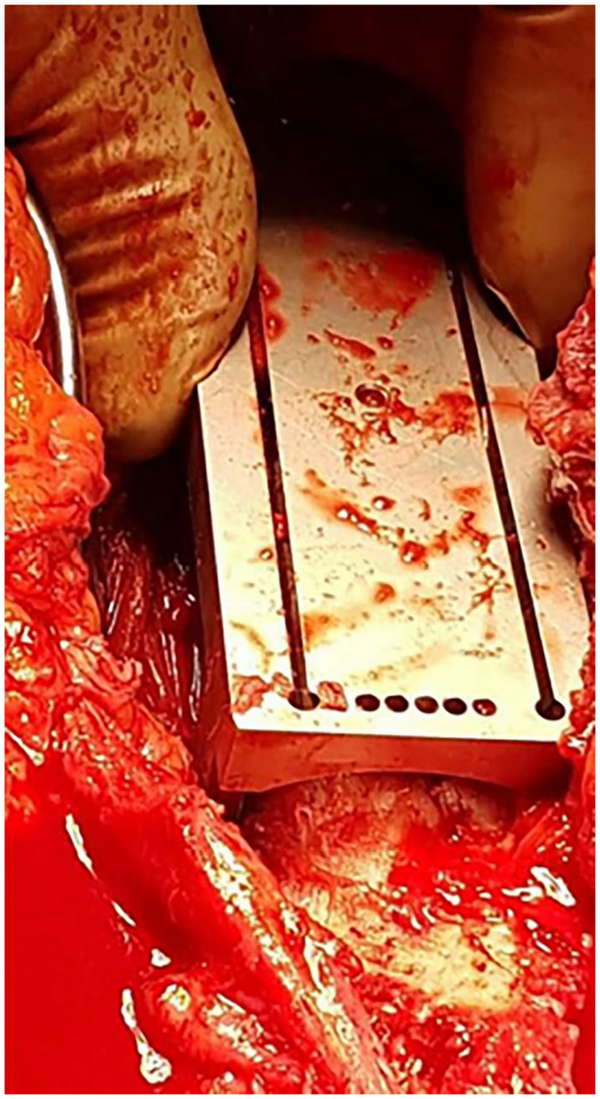
When creating the window, the earlier technique was to use an oscillating saw to cut medial and lateral longitudinal limbs with a single cutting guide jig (Figure 1). The surgeon determined the angle of the longitudinal cut at the operating table. The window was completed by making distal and proximal transverse cuts by predrilling and then using an osteotome to connect the multiple 2.5-mm drill holes.
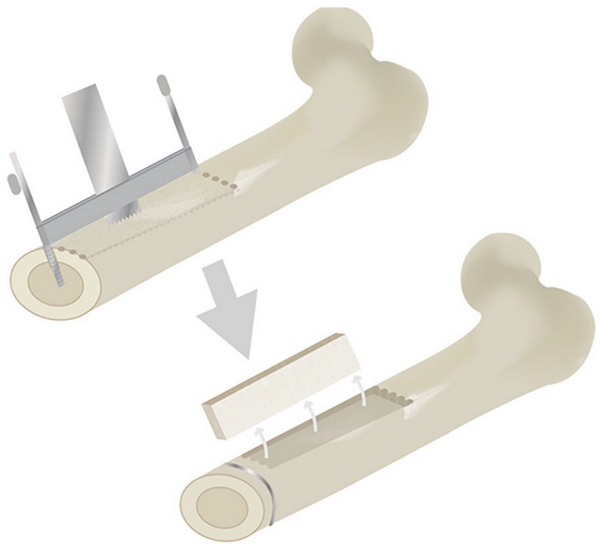
Figure 1
Cutting guide jig.
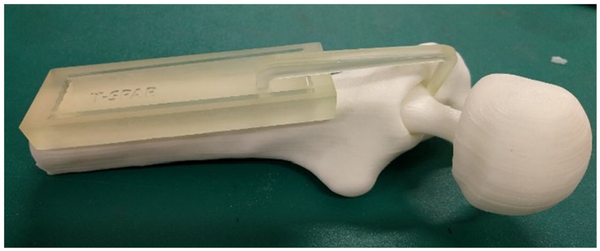
The technique evolved to using a 7.5 cm long block jig with longitudinal angled cutting guide and drill holes for the transverse limb to create the upper and lower limits of the window (Figure 2). More recently 3D-printed jigs, as shown in Figure 3, of varying length can now be used to extract secure cementless stems if removal through conventional means fails. Furthermore, these jigs can be used for extracting cement mantles.
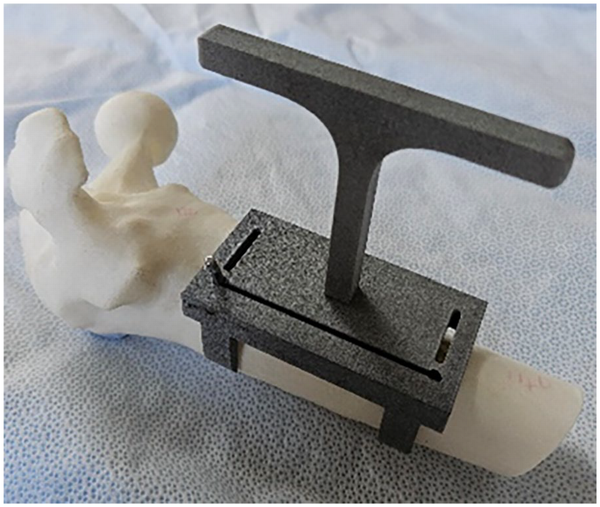
Figure 3
3D-printed jig.
For the last 6 cases from April 2018 a patient-specific instrumented (PSI) jig was used (Figures 4 and 5.) These patients had a preoperative CT scan of the proximal femur. Using software (Auckland Bioengineering Institute, New Zealand) and 3D-printing, a patient-specific jig, shaped as a rectangular rhomboid hard resin block complete with angled saw guide slots and drill holes was prepared. The PSI jig allowed less soft-tissue dissection and improved the accuracy of the application as it was contoured to the anterior femoral cortex shape and also when performing the osteotomy. The cutting block was applied with drill pins in the corners of the proposed cortical window thus preventing potential saw cut propagations. Saw cuts and drill holes were then made for an optimal-sized anterior cortical window using the jig.
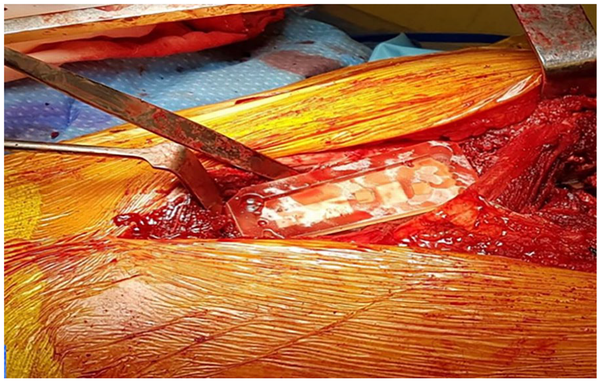
Figure 5
PSI screwed in-situ.
The femoral window was then removed and stored in sterile saline. The distal cement mantle and cement plug were removed using chisels, burrs, and long drill bits of varying diameters. The window allowed visualisation of the drill bit to be placed centrally in the canal and give confidence drilling distally through the cement plug, without the concern of perforating the cortex distal to the plug.
The canal was prepared by successive reaming for the long stem prosthesis, aiming to bypass the distal extent of the cortical window by at least twice the femoral diameter as recommended by Klein and Rubash. In aseptic cases, a modular, distal-fit uncemented ZMR stem was used (Zimmer) (Figure 6.) On occasion a cerclage wire would be applied to the proximal femur to prevent propagation of a fissure to the window when it became apparent whilst inserting the revision femoral stem (Figure 8.) In septic cases undergoing first-stage revision, either a Tecres Spacer G or a Biomet StageOne Select spacer was implanted, again bypassing the femoral window by at least twice the femoral diameter. The cortical window was replaced and secured with further Dall-Miles cables. In non-infected cases, cancellous bone graft from the femoral canal reamings was placed around the corticotomy.
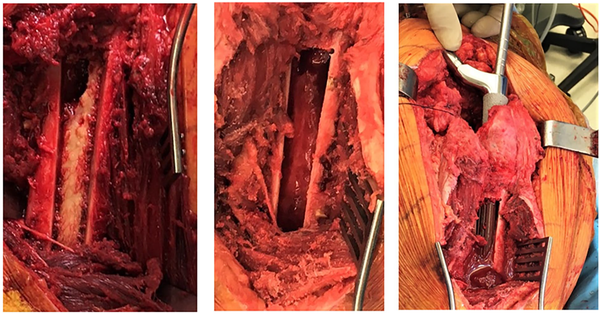
Figure 6
Photo on left shows cement mantle prior to removal, Photo in middle resected cement mantle and Photo on right ZMR stem being inserted.
Assessment of imaging
Patients had a limited CT scan of the proximal femur to assess integration of the femoral window from 5 months post-revision surgery. Bony integration of each window was assessed on axial imaging at 10-mm intervals along the length of the window. A scoring system was devised to quantify bony integration of the cortical windows. At each axial interval, complete integration was defined as bony union of both the medial and lateral corticotomy of the window; this was assigned a score of 1. Partial integration was defined as bony union of either the medial or lateral corticotomy; this was assigned a score of 0.5. Non-integration was defined as no bony union of either the medial or lateral corticotomy; this was assigned a score of 0 (Figure 7). The sum of the scores were divided by the number of axial slices assessed, to give an overall integration score ranging from 0 to 1, where 0 represents complete non-integration of the cortical window, and 1 represents complete integration. Assessment of CT imaging was performed by 2 authors plus a consultant radiologist from our institution. The same axial CT images were assessed by each author on 2 occasions, separated by a period of at least 2 weeks.
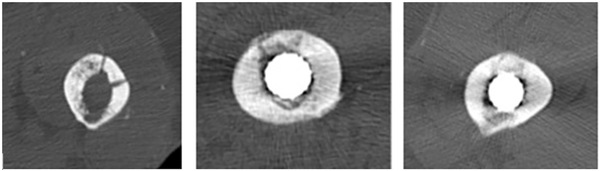
Figure 7
Axial CT slices demonstrating non-integration Score 0 (left), partial integration, score 0.5 (centre), and complete integration score 1 (right) of the femoral cortical window.
New Zealand Joint Registry review and functional outcomes
The New Zealand Joint Registry was reviewed to check that no revisions of our cases had been performed elsewhere. At 6 months post-surgery, the New Zealand Joint Registry (NZJR) sends patients the Oxford-12 questionnaire. Oxford scores were collected from the NZJR for our patient cohort. 10 scores were collected.
Statistical analysis
Intra- and inter-observer agreement of CT assessment was calculated using interclass correlation coefficient. Levene’s test for equality of variances analysis was used to compare overall integration scores in aseptic versus septic cases. All statistical analyses were performed using SPSS.
Results
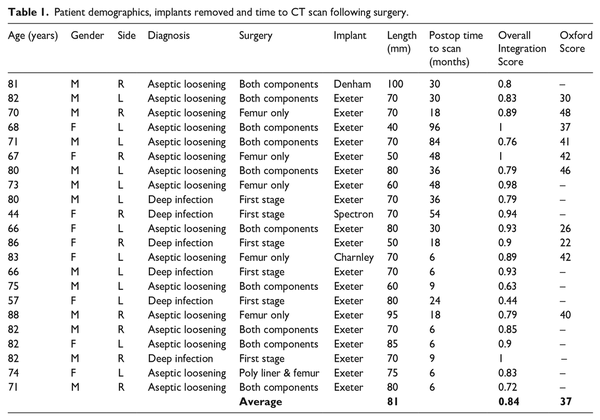
Between January 2006 and 2021, the senior author (JVD) performed 22 anterior cortical femoral windows during revision hip arthroplasty cases. There were 13 male and 9 female patients, with an average age of 74 years (range 44–88 years.) These cases are summarised in Table 1.
All 22 cases involved revision of a cemented femoral component. 16 single-stage revisions were performed for aseptic loosening, 10 of which included revision of both femoral and acetabular components, and 6 the femoral component only. 6 patients underwent first stage revision for deep infection (Table 1.) Of the 16 single-stage revisions performed, Zimmer ZMR taper stems (185 mm distal stem length) were implanted in all cases. Of the 6 first-stage revisions performed for infection, long cement spacers were implanted in all cases. 5 of these 6 patients went on to second-stage revision using the Zimmer ZMR (185 mm length) stem. In 2 patients the ZMR prosthesis subsided 1 cm.
No patient who underwent single-stage revision for aseptic loosening had further surgery either at our institution or elsewhere in New Zealand. 6 patients with sepsis went on to second-stage revision arthroplasty. 2 patients proceeded to second stage revision without complication. 1 patient required closed reduction of a dislocated cement spacer 1-week post first stage. 1 patient returned to theatre twice for wound debridement and closure following first-stage revision, before second-stage revision at 2 months. The final patient in this first-stage revision cohort, a 57-year-old female with severe rheumatoid arthritis, was ultimately treated with an excisional arthroplasty. This was following repeat first-stage revision and multiple washouts. Femoral stem survivorship was 100% in the rest of the series with a mean of 8 years follow-up (range 1–16 years).
Review of radiographs revealed full integration of the cortical window in 21 cases. The earliest time to integration was 4 months. The following plain radiographs of a patient revised for aseptic loosening at day-1 and at 12 months post-surgery, respectively (Figures 7 and 8).
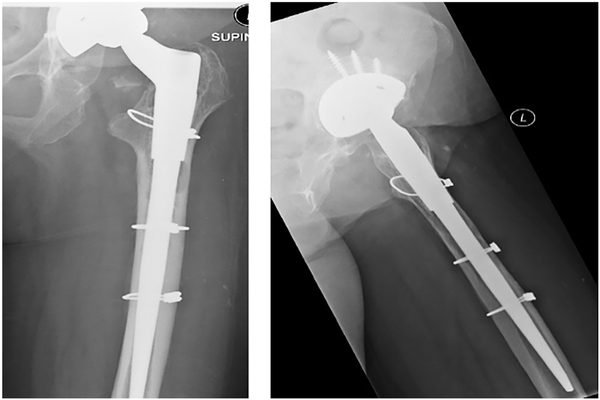
Figure 8
AP and lateral radiographs day-1 post-surgery. The femoral window cannot be appreciated on the AP view as it overlies the femoral component The superior and inferior transverse limbs of the cortical window are visible on the lateral view. Note proximal cerclage wire applied to prevent fracture propagating to the window whilst inserting the revision femoral stem.
Radiographs confirmed 2 cases of femoral stem subsidence of 1 cm. Both stems stabilised subsequently. CT scans were performed between 5 months and 9 years postoperatively (mean 30 months) (Table 1). The mean rectangular-shaped window size was 8 × 1.5 cm, with width variation of 1–2 cm. Average overall integration score was 0.84 (range scores 0.44–1). 3 patients demonstrated complete union of the cortical window. Using interclass correlation coefficient, inter-observer agreement was 0.86, and mean intra-observer agreement was 0.88 (0.79, 0.92, 0.92) for the first 16 cases. Values >0.8 are considered to show very good agreement, and >0.9 show excellent agreement.
Average overall integration score for aseptic cases was 0.85 (range 0.63 to 1, n = 16), and for septic cases was 0.77 (range 0.44–0.98, n = 6). Levene’s test for equality of variances analysis showed no statistically significant difference between integration scores (p = 0.324). Given the integration scores shown in Table 1 we suggest that most integration occurs within 6 months of surgery.
Oxford scores, provided through the New Zealand Joint Registry (NZJR) were available for 10 of the 22 patients (45%). The mean Oxford score was 37 (range 26–48) (Table 1). Focusing on the 16 patients who underwent single-stage revision for aseptic loosening, Oxford Hip Scores were available for 9 patients (56%). The mean score in this cohort was 39 (range 26–48).
Discussion
The proximal anterior femoral cortical window technique is an attractive alternative to the ETO. The exposure provided by an ETO remains superior to that provided by a cortical window. However, the femoral cortical window in this study provided adequate access to the distal cement mantle to allow complete extraction without compromise to the abductor mechanism. In addition, the cortical window technique has benefits for accessing and removing a well-fixed distal cement mantle by virtue of its simplicity of technique and low complication profile.
Replacement of the window is simple and the fixation required minimal. This is in contrast to an ETO where reduction and fixation of a greater trochanter segment after insertion of the definitive femoral component may be challenging. The anterior femoral window technique allows the proximal femur and abductor mechanism to remain undisturbed. This again contrasts with an ETO, where if a non-union should occur, it may lead to stem subsidence and to migration of the proximal segment, potentially de-functioning the abductor mechanism. In our study, however, stem subsidence did occur in 2 cases of 1 cm subsidence, but this was because of stem undersizing of the distal fit uncemented revision stem. The likelihood of subsidence is only compromised by a cortical window that extends past the isthmus. This does not occur with the standard-length femoral components that are removed as the tip of the prosthesis is either proximal or at the level of the isthmus.
The use of a PSI jig facilitates the technique of creating a cortical window. The virtue of a PSI jig is that it ensures, an optimally sized window and saves time, but is not mandatory. A generic 3D jig as in Figure 3 can also be used, however, our preference is for the PSI. The mean window size of 1.5 × 8 cm was adequate for removing the cement mantle in all cases in contrast to the shorter length, but wider width used by Patel K of 2.5 × 5 cm mean window size. Despite the length of the window, which was determined by the length of the prosthesis, there were no fractures in this study.
Using appropriate cement removal chisels and high-speed burrs allowed for removal of the cement mantle in the confines of the window size. The challenge of removing a distal cement plug distal to the window is facilitated by using long drills that are passed down centrally within the canal from above to drill through the plug with confidence not to perforate the cortex distally. The cement plug was then removed piecemeal. This study was focused on extraction of a distal cement mantle, but the technique might be used for extracting a secure cementless femoral component. In that context using a generic “off the shelf” 3D jig and not a PSI jig would be both more suitable and economical.
There were no cases of postoperative periprosthetic fractures in this series, however, minor proximal intraoperative fractures did appear from time to time whilst inserting the revision femoral stem. Propagation of the fissure to the window was prevented when a cerclage wire was applied proximally (Figure 8). As described by other authors, it is important to use a revision stem that bypasses the cortical window as reported by Klein and Rubash.
The assessment of radiographs for the presence or absence of osseous bridging along osteotomy sites can be difficult in the setting of a distal fit uncemented component. The use of CT resolves this issue as it allows better visualization particularly on the axial views. This is the first study to use CT to assess cortical window integration however we do not advocate postoperative CT scan as a requirement in routine practice. The score we devised to assess integration demonstrates very good intra- and inter-observer agreement and we proposed an acceptable integration score would be at least 0.75, that is, ¾ of the cortical window is incorporated into the femur. There was no relationship with window size and subsidence, nor for that matter with sepsis and asepsis in our series. The 2 cases of subsidence occurred because of under-sizing of the revision femoral component. The lowest overall integration score (0.44) was seen in the patient with advanced rheumatoid arthritis with sepsis ultimately requiring a Girdlestone procedure.
The CT scan confirmation of good to excellent bone incorporation indicates that the resected “de-vascularised” cortical window can be removed and replaced into the femoral cortex with confidence: non-union is unlikely. Application of autogenous bone graft from reamings to the corticotomy site as part of the technique in this study and reported by Klein and Rubash may have some bearing on the union rate. Using a vascularised cortical window was described by Sahemy et al. and may be an advantageous technique. However, our study shows that our de-vascularised cortical window does unite with the host bone within a 6-month period. The surgical technique described to obtain a vascularised cortical bone window may be more challenging compared to the technique described above which can be applied in a regional hospital setting.
Functional outcomes were only available for 45% of our patients. This is likely due to patients not receiving or not returning the Oxford score, which is sent by the NZJR to revision arthroplasty patients 6 months postoperatively. Outcomes of revision arthroplasty tend to be superior for aseptic pathology compared with septic pathology. Focusing on our single-stage revision cohort, Oxford scores were available for 56% of patients. The average score of 39, compares favourably to the mean Oxford score of 35.1 for revision hip arthroplasty in New Zealand between 1999 and 2016 NZJR.
This study has a number of imitations. It is a technique description and a retrospective review and the cohort is small. Functional results were not available for all patients. It is a single-surgeon series but despite this, the technique was successfully undertaken by attending and trainee surgeons alike. The other limitation is that the advantages of this technique compared to an ETO are not objectively determined although there is the perception that the morbidity is reduced and the technique less challenging.
Conclusion
This single-surgeon series shows that a proximal anterior femoral cortical window is a useful and safe adjunct to femoral cement removal. It can be performed by non-subspecialist arthroplasty surgeons using either a generic or PSI jig, to facilitate the technique ensuring it is reproducible and technically straightforward. It has a safe complication profile. CT imaging confirms that “de-vascularised” femoral cortical windows demonstrate integration in both aseptic and septic cases, and functional outcomes compare favourably with those reported in the NZJR.
We would like to acknowledge and thank P Roberts and J Zhang at the Auckland Bioengineering Institute, Auckland University, New Zealand.
Declaration of conflicting interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship and/or publication of this article.
Michael C Wyatt
https://orcid.org/0000-0001-5283-2608
References
- 1. Eftekhar NS. Rechannelization of cemented femur using a guide and drill system. Clin Orthop Relat Res 1977; 123: 29–31.
- 2. Younger T, Bradford M, Magnus R, et al. Extended proximal femoral osteotomy: A new technique for femoral revision arthroplasty. J Arthroplasty 1995; 10: 329–338.
- 3. Mardones R, Gonzalez C, Cabanela ME, et al. Extended femoral osteotomy for revision of hip arthroplasty. J Arthroplasty 2005; 20: 79–83.
- 4. Zweymüller KA, Steindl M, Melmer T. Anterior windowing of the femur diaphysis for cement removal in revision surgery. Clin Orthop Relat Res 2005; 441: 227–236.
- 5. Shepherd BD, Turnbull A. The fate of femoral windows in revision joint arthroplasty. J Bone Joint Surg Am 1989; 71: 716–718.
- 6. Sahemey R, Garala K, Chahal G, et al. Outcomes of revision total hip arthroplasty using a vascularised anterior femoral window. Eur J Orthop Surg Traumatol 2022; 32: 1325–1332.
- 7. Park C, Yeom J, Park J, et al. Anterior cortical window technique instead of extended trochanteric osteotomy in revision total hip arthroplasty: a minimum 10-year follow-up. Clin Orthop Surg 2019; 11: 396.
- 8. Klein AH, Rubash H. Femoral windows in revision total hip arthroplasty. Clin Orthop Relat Res 1993; 291: 164–170.
- 9. Singhai S, Gandavaram S, Herlekar D, et al. Effectiveness of cortical window technique for revision hip arthroplasty. Orthopaedic J MP Chapter 2019; 25: 3–7.
- 10. New Zealand Orthopaedic Joint Registry. nzoa.org.nz/nzoa-joint-registry (1999–2016).