Figure
No caption available.
INTRODUCTION
Myopic astigmatism is a refractive error that affects a significant portion of the world's population. It is a type of visual impairment that occurs when the eye is both near-sighted and has astigmatism, a condition where the cornea or lens of the eye is irregularly shaped. This causes light to be focused unevenly on the retina, resulting in distorted or blurred vision. Myopic astigmatism can have a significant impact on a person's quality of life, but there are various treatment options available to manage it.
The prevalence of myopic astigmatism varies among different populations, but it is most common in younger individuals. While myopia and astigmatism are both distinct conditions, they often occur together, and myopic astigmatism is estimated to affect around 30% of those with myopia.[]
Myopia occurs when the eyeball is too long or the cornea is too steep, causing light to focus in front of the retina instead of directly on it. This makes distant objects appear blurry, while close objects remain clear. Myopia is often hereditary, but it can also develop as a result of environmental factors such as excessive reading or computer use. Astigmatism occurs when the cornea or lens of the eye is irregularly shaped, causing light to be focused unevenly on the retina. This results in distorted or blurred vision, both at a distance and up close. Astigmatism can also be hereditary or caused by eye injury or disease.
When myopia and astigmatism occur together, they can cause significant visual impairment and affect a person's quality of life.
SYMPTOMS
Myopic astigmatism can cause a range of symptoms, including blurred vision, eye strain, headaches, and difficulty with depth perception. People with myopic astigmatism may have trouble seeing objects both up close and at a distance, and may find it challenging to read or drive a car. The condition can also cause eye fatigue, which can affect daily activities such as studying or working on a computer.
Higher preoperative myopic astigmatism is associated with a higher probability of retreatment due to patient dissatisfaction as a result of residual cylindrical error.
DIAGNOSIS
Diagnosis of a refractive error is usually done based on a simple refraction which may be aided by a cycloplegic agent. This is usually followed by a post cycloplegic refraction. Myopic astigmatism may easily be diagnosed following a refraction.
Other diagnostic modalities which aid in planning the management include a topographical analysis using various methods like pentacam or corvis. Aberratometry can also help in distinguishing corneal versus lenticular astigmatism including any higher order abberations.
MANAGEMENT
The treatment options for myopic astigmatism include corrective lenses and refractive surgery. Corrective lenses can be prescribed in the form of eyeglasses or contact lenses, which work by altering the way light enters the eye, thus correcting the focusing problem. Eyeglasses and contact lenses can be used for both myopia and astigmatism, and they are often effective in improving vision.
CONTACT LENSES
Various types of contact lenses may be used for the correction of myopic astigmatism. These include-
Soft toric lenses-indicated in early keratoconus, intolerance/discomfort to RGP lenses. These are conventional hydrogel or silicon hydrogel lenses. They have a single laser marking at 6 o'clock to assess rotation.
RGP lenses- Rigid gas permeable lenses are the first lens of choice for visual improvement. These can be traditional or customised Rose K lenses, especially for use in keratoconus patients.
Rose K lenses- These are best suited in case of central nipple cone in keratoconus patients, however may be individually customised based on the location of the nipple. These are multi-curved lenses with a small optical zone which snugly fits the cone.
Intralimbal lenses- These are large diameter lenses ranging between 10.5-12 mm and used in patients with moderate keratoconus. The large diameter helps in improving the lens centration and reduces the lens movements.
Piggyback contact lenses- In this, the RGP lens is placed on a soft contact lens. This arrangement improves the contact lens fit and is indicated in advanced keratoconus, pellucid marginal degeneration or post LASIK ectasia.
Scleral contact lens- These lenses rest on the sclera and do not touch the cornea or the limbus, thus leaving some space between the contact lens and the cornea. Indicated in higher astigmatism or advanced ectasias.
Hybrid lenses- These have a rigid lens in the center and a soft skirt in the periphery. These also help improve the fit and reduce discomfort.
REFRACTIVE SURGERY
Refractive surgery is another treatment option for myopic astigmatism. This type of surgery involves reshaping the cornea to correct the focusing problem, and it can be performed using different methods such as PRK, LASIK, SMILE, or ICL implantation. Cornea based refractive procedures reshape the cornea to correct the refractive error and can provide long-term vision improvement. These procedures are often effective in correcting vision and reducing the need for corrective lenses, but they do carry some risks and may not be suitable for everyone.
On comparing SMILE with LASIK, studies showed that SMILE has slightly worse results in correcting low-to-moderate astigmatism.[, ] A study showed comparable results between SMILE and LASIK in cases with correction of high astigmatism (>3 D).[] Undercorrection was noted in both SMILE and LASIK for high astigmatism correction, but better outcome was noted in LASIK for low-to-moderate astigmatism correction.[, ]
SCREENING GUIDELINES IN MYOPIC REFRACTIVE SURGERY
The various available options for the treatment of myopic astigmatism are cornea based or lens based procedures. Cornea based procedures practised commonly these days include photorefractive keratectomy (PRK), Laser assisted keratomileusis (LASIK) or Small incision lenticule extraction (SMILE). Lens based procedures include phakic IOLs and Refractive lens exchange (RLE).
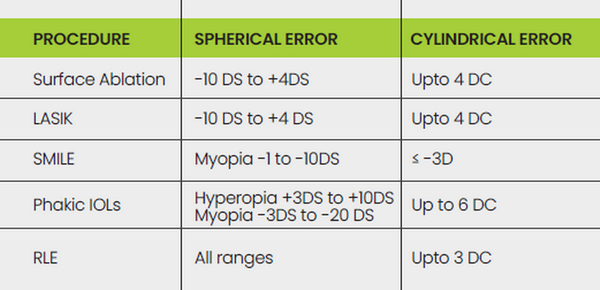
A combination of these procedures may also be tried. FDA approved range of refractive correction is given in the following table 1-
Ideal candidate for refractive surgery-
Age > 18 yrs
Stable refractive error > 1 yr
Not pregnant / nursing or planning to conceive for 1 yr
No systemic or auto-immune disease
Adequately counselled and has realistic expectations
Contraindications for refractive surgery-
Age < 18 years
Unstable refraction
Severe dry eyes
One eyed
Known case of progressive corneal ectatic disorders
History of eye inflammation/herpetic eye disease
Large pupil size (>7mm)
Known case of glaucoma
Known Systemic and Autoimmune illness
Drugs : Systemic corticosteroids, Amiodarone, Sumatriptan, Antihistaminics, Isotretinoin
Presence of nystagmus/amblyopia/squint
Pre-operative workup-
Off Contact Lenses (> 2 wks-Soft CL & >4 wk-Rigid CL)
Manifest Refractive Spherical Equivalent (MRSE)
Keratometry (Automated, Topolyzer)
Corneal Topography (Orbscan, Pentacam)
Pupillometry (Orbscan, Pentacam)
Corneal Pachymetry (Ultrasonic, Orbscan, Pentacam)
Anterior chamber depth (ACD) and White to White (WTW) measurement (for Phakic IOL): Orbscan, IOL master, Digital Calipers .
CORNEAL TOPOGRAPHY SCREENING PARAMETERS
Sagittal Map
Kmax > 48.7 D
Km b/w both eyes > 2 D
Kmax-K2 > 1 D
SRAX > 21°
I-S > 1.4 D
Anterior Elevation Map
Anterior Elevation > 12μm
Pachymetry Map
S-I >30 μm
CCT <470 μm with normal topography
CCT <500 μm with abnormal topography
Pachy apex - TL > 10 μm
Y- coordinate TL > -500 μm
TL b/w both eyes > 30 μm
Posterior Elevation Map
Posterior Elevation >17 μm
Corneal topography screening parameters on Belin/Ambrosio Enhanced Ectasia display
On Difference map,
> 5 μm for the front elevation
>12 μm difference for the back elevation was suspicious
The cut-off criteria for Ambrosio relational thickness[] -ART-Max was 339 μm
Thickness profile - Average Progression > 1.1 -Curves : CTSP, PTI
BAD-D
> 1.6 suggestive FFKC
> 2.6 suggestive of KC
CUT OFF PARAMETERS FOR LASIK/SMILE
RSBT = CCT - [FT + AD]
RSBT-Residual stromal bed thickness CCT-Central corneal thickness FT-Flap thickness AD-Depth of ablation
Ablation depth in μm (Munnerlyn formula) =
(Ref Error × (OZ)[]) / 3
RSBT > 250 μm for LASIK/SMILE/Surface ablation*
Percentage Tissue Altered (PTA) = (FT + AD)/CCT
PTA < 40% for LASIK*
Post-operative keratometry - >34 and <48
CAUSES OF UNFAVOURABLE OUTCOMES IN LASIK OR SMILE
Undercorrection can be attributable to the lack of cyclotorsion control, which has been a major issue in astigmatism correction. Causes of cyclotorsion include ocular torsion caused by the vestibular system, movement of the head and body under laser, and unmasking of cyclophoria.[] As high as 82% of patients are expected to have cyclotorsion when they lie flat, which has been reported as the main contributing factor to postoperative undercorrection.[] Cyclotorsion induces misalignment and can lead to inaccuracy in treatment orientations. Static cyclotorsion occurs when a patient changes from an upright position to a supine one. Dynamic cyclotorsion occurs when there is a torsional eye movement during laser application intraoperatively.
To compensate for cyclotorsion, manual compensation was suggested during SMILE. Preoperatively, limbal marks at 0 and 180° can be made while patient is sitting in an upright position. Upon supine positioning, the limbal markings can serve as a guide to detect any cyclotorsion. Head adjustment can be performed according to the alignment between the limbal markings and reticule on the screen of the SMILE platform. Some surgeons prefer to rotate the treatment cone after docking. In this technique, corneal markings are needed to enable visualization of the markings and cyclotorsion compensation is done by gentle rotation of the contact glass. A recent study evaluated manual cyclotorsion compensation by preoperative corneal marking and rotation of the treatment cone.[]
Achieving accurate centration is also very important in laser based refractive surgeries. Unable to achieve accurate centration may increase the risk of decentered treatment and lead to unfavorable visual outcome.[]
Another important consideration in planning any refractive surgery is angle kappa which is the angle between the visual axis and the pupillary axis. The measurement is important in refractive surgery, as it affects proper centration.[] In optical zone centration, centration using the pupil tracking has been widely adopted. However, the pupillary axis is different from the visual axis. The pupillary axis is the line passing through the pupillary center perpendicular to the cornea. The visual axis is the line connecting the fovea with the fixation point; this lineline passes through the nodal point of the eye.
However, the centration on the pupil will create new aberrations in myopic astigmatism cases with a large angle kappa. This will lead to decentered ablation and will induce symptoms of halo and glare.[]
The correction of moderate-to-high myopia or myopic astigmatism by implanation of an implantable collamer lens is an effective, relative safe and predictable method. It has an important place in the modern refractive surgery, especially in patients, who are not able to undergo the photorefractive corneal surgery to correct their refractive errors.[] ICL surgery is simple with the ease of reversibility. Currently, FDA approves correction of myopic refractive error in patients with spherical equivalent ranging from -3.0 D to -20.0 D and cylinder of 1.0 to 4.0 D.
CONCLUSIONS
Myopic astigmatism is a common refractive error that affects a significant portion of the population. It can have a significant impact on a person's quality of life, causing symptoms such as blurred vision, eye strain, and headaches. However, there are various treatment options available to manage the condition, including corrective lenses and refractive surgery.
Financial disclosure
None
Conflict of Interest
None
Acknowledgements
Nil
REFERENCES
- 1. Chow SSW, Chow LLW, Lee CZ, Chan TCY. Astigmatism Correction Using SMILE. Asia-Pac J Ophthalmol Phila Pa. 2019;8(5):391–6.
- 2. Khalifa MA, Ghoneim AM, Shaheen MS, Piñero DP. Vector analysis of astigmatic changes after small-incision lenticule extraction andwavefront-guided laser in situ keratomileusis. J Cataract Refract Surg. 2017 ;43(6):819–24.
- 3. Chan TCY, Ng ALK, Cheng GPM, Wang Z, Ye C, Woo VCP, et al. Vector analysis of astigmatic correction after small-incision lenticule extraction and femtosecond-assisted LASIK for low to moderate myopic astigmatism. Br J Ophthalmol. 2016 ;100(4):553–9
- 4. Chan TCY, Ng ALK, Cheng GPM, Wang Z, Ye C, Woo VCP, et al. Vector analysis of astigmatic correction after small-incision lenticule extraction and femtosecond-assisted LASIK for low to moderate myopic astigmatism. Br J Ophthalmol. 2016 ;100(4):553–9
- 5. Zhang J, Wang Y, Chen X. Comparison of Moderate- to High-Astigmatism Corrections Using Wave-Front-Guided Laser In Situ Keratomileusis and Small-Incision Lenticule Extraction. Cornea. 2016 ;35(4):523–30.
- 6. Taneri S, Kieβler S, Rost A, Schultz T, Dick HB. Small-incision lenticule extraction for the correction of myopic astigmatism. J Cataract Refract Surg. 2019 ;45(l):62–71.
- 7. Alió Del Barrio JL, Vargas V, Al-Shymali O, Alió JL. Small incision lenticule extraction (SMILE) in the correction of myopic astigmatism: outcomes and limitations - an update. Eye Vis Lond Engl. 2017;4:26.
- 8. Ganesh S, Brar S, Pawar A. Results of Intraoperative Manual Cyclotorsion Compensation for Myopic Astigmatism in Patients Undergoing Small Incision Lenticule Extraction (SMILE). J Refract Surg Thorofare NJ 1995. 2017 ;33(8):506–12.
- 9. Park CY, Oh SY, Chuck RS. Measurement of angle kappa and centration in refractive surgery. Curr Opin Ophthalmol. 2012 ;23(4):269–75.
- 10. Park CY, Oh SY, Chuck RS. Measurement of angle kappa and centration in refractive surgery. Curr Opin Ophthalmol. 2012 ;23(4):269–75.
- 11. Řeháková T, Veliká V, Rozsíval P, Jirásková N. Correction of Myopia and Myopic Astigmatism by Implantation of a Phakic Posterior Chamber Implantable Collamer Lens. Ceska Slov Oftalmol Cas Ceske Oftalmol Spolecnosti Slov Oftalmol Spolecnosti. 2019;74(4):147–52..