Introduction
In civilian environments, terrorist attacks are a new phenomenon of threat against people living in urban areas that have spread around the globe. They can cause catastrophic haemorrhage similar to the military trauma paradigm. Global terrorist attacks have taken place in several locations, including Madrid in 2004, London in 2005 and 2017, Boston in 2013 and Paris in 2015. These have resulted in civilian experiences akin to war phenomena, with civilians likely to be exposed to explosive device and gunshot wounds. Open space explosions have resulted in increased numbers of injuries and statistically high volumes of amputations. Between 1970 and 2014, the average number of terrorist incidents was 2000 per year and, not surprisingly, the majority occurred in the Middle East and South Asia. Western Europe had 13.2% of all terrorist incidents, ranking fourth overall. Apart from mass casualties from terrorist events, natural disasters and shark attacks in Australia have often been associated with exsanguination from isolated extremity injuries., Australia has the second‐highest number of reported shark attacks in the world after North America, and limb loss (at least one arm or leg) occurred in 7% of all reported injuries. In life‐threatening massive haemorrhage, tourniquet applications could be beneficial when limb haemorrhage is uncontrollable by simple methods (e.g. direct pressure, limb elevation and wound packing), where there are multiple casualties with extremity haemorrhage, or mangled limbs with multiple bleeding locations (as in shark bite).
Effective tourniquet applications on battlefields
Tourniquets have been used for many decades as a first aid tool to limit major bleeding on the battlefield, but their use has remained controversial because of adverse effects., For instance, tourniquet applications may cause ischaemia by preventing arterial blood flow, permanent nerve injury and muscle injury (including contractures, rhabdomyolysis and compartment syndrome) when applied for over 2 h and vascular injury and skin necrosis., For such reasons, tourniquet use might be discouraged in prehospital services. Nevertheless, military personnel has been at the forefront of reintroducing tourniquet use on the battlefield and developing military trauma practice for controlling catastrophic haemorrhage. Kragh and colleagues summarised a series of empirical reports of successful tourniquet use for saving lives on battlefields in the Middle East. For instance, in a prospective observational survey carried out on 232 patients from seven nationalities admitted to a combat support hospital, effectiveness was shown as 76% when tourniquets were applied in prehospital environments compared with 86% in Emergency Departments. Similarly, in a 1‐year prospective study in a military hospital in Iraq, with 499 patients from 13 nationalities, there was a survival rate of 90% when tourniquets were applied prior to onset of shock, compared with a survival rate of 18% when applied after onset of shock. These prospective studies from combat grounds have clearly shown benefits of prehospital tourniquet use to control massive bleeding from injured limbs and reduce mortality in military personnel.
Prehospital tourniquet applications in civilian settings
In civilian settings, mass casualties are seen in deliberate terrorist attacks, mass shootings or occupational/industrial disasters. Tourniquets are efficient tools to stem blood flow and have proved successful in combat environments, and their use is now being considered for first responders and paramedics in prehospital environments. Studies have been conducted in the United States, United Kingdom and Canada, but there has been only one Australian report, a case study in Queensland.
In the United States, a large dataset was derived from retrospective medical records related to tourniquet use from nine urban Level 1 trauma centres from 2010 to 2013. Findings clearly demonstrated that prehospital tourniquets were effective in controlling haemorrhage, with 56.5% of patients showing increased systolic blood pressure (SBP). Overall mortality was 3% and 28.9% underwent amputations because limbs were not salvageable, which reflected the severity and pattern of injuries rather than tourniquet application. A retrospective cohort study design to collect data on trauma patients from the Trauma Registry of the American College of Surgeons database was carried out between 2008 and 2016. All‐cause mortality was lower in patients with indicated tourniquet placement than those with no indication. After controlling for confounding factors (years, mechanism of injury and SBP), patients with delayed tourniquet application showed a 4.5‐fold increased risk of death from haemorrhagic shock (Odds Ratio = 4.5, 95% confidence interval (CI) = 1.23–16.4, p = 0.02). Interestingly, patients with tourniquet application in prehospital settings had significantly higher GCS (Glasgow Coma Scale) scores and blood pressure upon arrival than those with tourniquets applied at trauma centres. In a retrospective review, use of non‐commercial tourniquets (latex surgical tubing) in Boston prehospital settings between 2005 and 2012 was examined and there were 10.5% of fatalities when prehospital tourniquets were applied. Retrospective data from NEMSIS, the largest Emergency Medical Services (EMS) database in the United States, were drawn between 2011 and 2014. Prevalence of using tourniquets in prehospital settings was 0.2 per 1000 EMS activations and injuries where tourniquets were used were mainly stabbing/accidental cutting. Unfortunately, no findings relating tourniquet application to mortality/morbidity rates were mentioned.
In Canada, a 10‐year retrospective study conducted at two large Level I trauma centres, 186 patients arrived at centres without tourniquet applications while four patients had improvised tourniquets (e.g. neck tie, belt, handkerchief) applied prehospital by police and bystanders. All tourniquet patients survived without developing compartment syndrome but two of them (50%) underwent limb amputation because of severe limb damage or near amputation. People without tourniquet application received significantly more blood products than those with early tourniquet applications, and 3.2% died from exsanguination.
The articles cited above were retrospective studies, but the findings clearly demonstrate the effectiveness of tourniquet application in prehospital settings in saving lives and this outweighed the risks of tourniquet application. European countries (including the United Kingdom) and the United States have well‐established guidelines for prehospital tourniquet uses in the event of threatening extremity haemorrhage, but the tourniquet endorsement does not extend to other developed nations, including Australia, where prehospital tourniquet applications are not mandatory in every State or Territory.
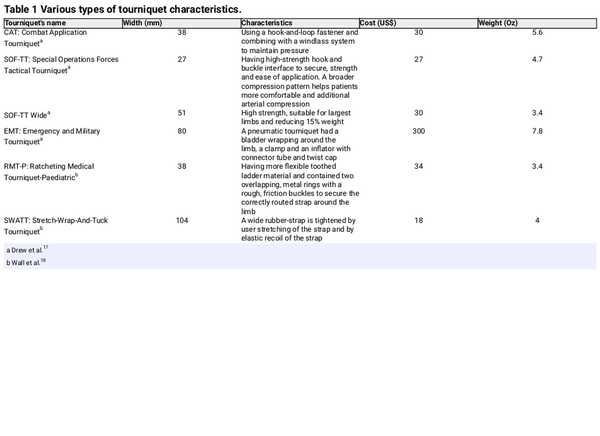
When considering the most effective types of prehospital/emergency tourniquet to control arterial blood flow from systematic circulation, several commercial tourniquets have been mentioned, including the Combat Application Tourniquet (CAT), Stretch‐Wrap‐And‐Tuck Tourniquet (SWATT), SOF‐Tactical Tourniquet‐Wide (SOFTT‐W) and the Ratcheting Medical Tourniquet‐Paediatric (RMT‐P). Characteristics of these tourniquets are outlined in Table 1. Apart from commercially available tourniquets, there is the Improvised Russian Tourniquet (IRT), the Emergency and Military Tourniquet (EMT) and improvised tourniquets. Unfortunately, only one systematic review has been conducted comparing types of commercial tourniquet used in civilian trauma, but the effectiveness of each tourniquet type was not compared and there was no distinction between tourniquet applications in prehospital or other emergency settings. There are systematic review articles examining tourniquet use for limb and trauma surgery but most examined hospital procedures (operation theatre or Emergency Department). Little has been written about the use of tourniquets in prehospital settings and there is little information about benefits and complications for specific commercial tourniquet types in prehospital settings.
This systematic review was designed to evaluate effectiveness and complications of prehospital tourniquets and compare efficacy of commercial tourniquet applications that could be used in prehospital settings.
Methods
Studies up to March 2018 reporting tourniquet use by emergency services were included in the review. Six databases (ScienceDirect, PubMed, Ovid, SAGE, SpringerLink, Taylor & Francis) were searched using the search terms ‘emergency services’ and ‘tourniquet’ to identify published articles about tourniquet applications, with no date limits but only including articles written in English. After a first screening that examined title and abstract, the author and a research assistant independently carried out the second screening to identify articles meeting eligibility criteria for inclusion. These were studies of adults (aged 18 years and over), not including animal models/simulations/mannequins and not using abdominal and junctional tourniquets. Abstracts, conference papers and case reports were excluded, together with studies set solely in hospitals and operating theatres. Full‐text articles were obtained after application of selection criteria. The two researchers compared the number of eligible full‐text articles; they had identified in each database, and where there were discrepancies, they jointly reassessed the articles until reaching agreement on inclusion/exclusion – see Table 2.
All full‐text articles from the six databases were checked for duplication, and 14 articles remained for inclusion in the systematic review. The studies were compared by examining the research design (prospective randomised, prospective comparative, prospective cross‐sectional and retrospective studies) and participant characteristics and numbers to allow a quality assessment of each study. In addition, data extraction was focused on comparing tourniquet type and positive and negative outcomes from tourniquet applications.
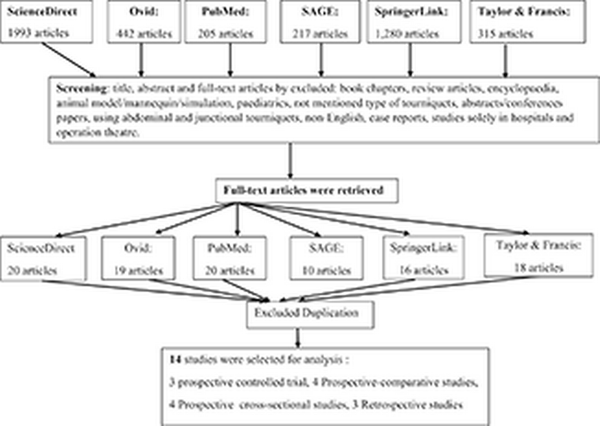
Table 2
A flow diagram of articles selection.
Study quality and bias assessment
The Effective Public Health Practice Project (EPHPP) Quality Assessment Tool for Quantitative Studies was selected to assess methodological strength of each study. The EPHPP tool was chosen to evaluate effectiveness of studies because it contains an appropriate quality assessment for examining a variety of research designs in public health. EPHPP quality assessment involves rating each of six components on a three‐point scale (strong, moderate and weak): selection bias, study design, confounders, blinding, data collection methods and attrition. A global rating for each study is determined by summation of the six component scores, resulting in an overall rating of strong, moderate or weak for each article. A strong rating indicates that no component had a weak rating, a moderate rating indicates one component had a weak rating and a weak rating indicates two or more components had weak ratings. Two evaluators examined each domain independently and discrepancies were resolved by discussing the rationale until agreement was reached.
Results
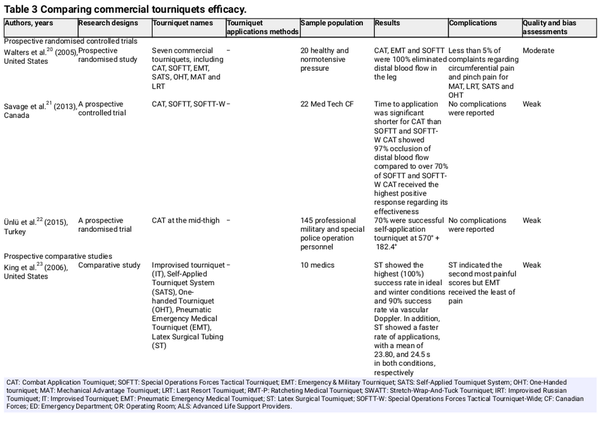
The 14 full‐text articles retrieved from six databases included eight articles from the United States, two from the United Kingdom, two from Israeli and one each from Turkey and Canada. In total, there were three prospective randomised controlled trials, four articles reporting prospective comparative studies, four papers reporting prospective cross‐sectional studies and three articles reporting retrospective studies, as shown in Table 3. The quality assessment of each study is shown in Table 3.
Prospective randomised studies
Prospective randomised studies from the United States, Canada and Turkey all concluded that CAT was an effective tourniquet application for occluding distal blood flow ranging from nearly 70% to 100%, as detailed below.
Walters et al. performed a prospective randomised trial comparing seven types of tourniquet: CAT, SATS, Mechanical Advantage Tourniquet (MAT), SOFTT, H‐Dyne One‐Handed Tourniquet (OHT), Last Resort Tourniquet (LRT) and EMT, with 20 healthy normotensive participants. Three tourniquets (CAT, EMT and SOFTT) completely occluded distal blood flow in the leg in all participants but the remaining tourniquets were below 80% success rate. Failure of tourniquet application included pain, slipping and physical limitation. The study was identified as having moderate quality assessment because of a weak rating in confounding bias.
In a Canadian study, three types of tourniquet were compared, CAT, SOFTT and SOFTT‐W, with 22 Med Tech CF (Medical Technician in the Canadian Forces) in a prospective controlled design. Tourniquet application times were significantly shorter for CAT, which was also significantly more effective in preventing blood flow (97%) than SOFTT (72.70%) or SOFTT‐W (73.80%). The study displayed several limitations in study design, confounders and blinding processes and was therefore of weak quality.
In a study of CAT self‐application in Turkey, a randomised trial design was used with 145 professional military and special police operations personnel. There was no significant difference in success rate of CAT self‐application between left and right lower extremities. Overall success rate of applied CAT was 66% at 630°. This study had some issues of mitigating confounding bias and blinding, so it was rated weak in terms of quality assessment.
Prospective comparative studies
Four prospective comparative studies were identified, from the United States, Canada and two from the United Kingdom., The Canadian study identified ST (Latex Surgical Tube) as having high success rate of occlusion similar to a CAT study in the United States. Two studies from the United Kingdom demonstrated that EMT and pneumatic tourniquets were better than CAT in relation to occlusion of popliteal flow. All studies were rated weak in the assessment of quality and bias, as detailed below.
In the Canadian study, five types of tourniquet, IT, SATS, OHT, pneumatic EMT and latex Surgical Tubing (ST), were tested with 10 medics with less than 10 years of experience. EMT and ST tourniquets produced the two highest successful rates of occlusion by palpable pulse check (80% vs 100%) and vascular Doppler method (80% vs 90%) under ideal and winter conditions. Fastest rate of tourniquet application was for ST, which also had slightly higher scores for being very easy to apply. EMT was rated the least painful when applied. This study had weak quality in relation to confounders and blinding for assessment criteria.
In the US study, four different thigh tourniquets (CAT, SOFTT‐W, RMT‐P and SWATT) were compared on calf and forearm with 16 voluntary participants (8 men and 8 women). Highest calf friction pressure was obtained with CAT while highest forearm friction pressure was obtained with RMT‐P. Even though RMT‐P and CAT were the same width (38 mm), occlusion pressure was higher with CAT than RMT‐P. All tourniquets were able to reach occlusion. CAT, SOFTT‐W and RMT‐P applications failed to maintain 120‐s pressure after complete occlusion but SWATT could hold 120‐s occlusion pressure. SOFTT‐W was the least easy to use and was given the highest discomfort ratings. This study was ranked weak because of confounders and blinding procedures.
In a study from the United Kingdom, the effectiveness of a windlass system (CAT) was compared with EMT when applied at the mid‐thigh level in 24 volunteers who were serving military personnel. CAT self‐application gave occlusion of popliteal flow in 16.6% cases compared with 75% when using EMT, which was a significant difference (p = 0.001). Weak study design, confounding bias and blinding were identified in the study.
In the United Kingdom, 12 healthy serving soldiers were recruited for an experiment comparing effectiveness of CAT and Tactical Pneumatic Tourniquet in stopping blood flow at the mid‐thigh level (half‐way point between the greater trochanter and the superior pole of the patella). Complete occlusion of the popliteal artery was achieved in a median time of 16 s (range 12–20) with CAT compared with 11 s (range 7–12) for pneumatic tourniquet. There was no significant difference in pain scores after application between the two tourniquets. Three weak domains of quality assessment were identified: study design, confounding bias and blinding.
Prospective cross‐sectional studies
Four articles were selected reporting prospective cross‐sectional studies, with three from the United States and one study from Israel. All studies used CAT to stop arterial occlusion as detailed below. Nearly all studies displayed weak quality and bias in the assessment.
A prospective observation survey was conducted from March to October 2006 at the combat support hospital in Baghdad, Iraq, with 232 patients who had 428 tourniquet applications on 309 limbs. The most common tourniquet used was CAT but this was rated second in effectiveness (79%) behind EMT (92%). EMT was the widest tourniquet, followed by CAT, but EMT was not designed for prehospital use and required a high level of care. This study was ranked weak on quality assessment because of study design, confounders and blinding.
A 3‐month cross‐sectional study was carried out at Forward Operating Base Shank, Afghanistan (Level II). In 90% of cases, CATs were applied before arrival at the centre, while SOFTT, ratchet‐type tourniquets and improvised tourniquets were used for 5% of cases. In over 80% of limbs, a distal pulse was still present. For pulseless limbs with tourniquet application, 50% returned a distal pulse upon tourniquet release. Four components of quality assessment were ranked as weak including selection bias, study design, confounding issues and blinding.
In the United States, a prospective study was used to compare efficacy of tourniquet application for SWATT, CAT and pneumatic tourniquets with 17 undergraduate students. For occlusion pressure, CAT was significantly higher than SWATT and pneumatic tourniquets with pressure greater than 500 mmHg. There were significant differences in pressure decrease and loss occlusion over 1 min between the three types of tourniquet (e.g. pressure decrease, CAT: 44 ± 33 mmHg; SWATT: 6 ± 8 mmHg; Cuff: 14 ± 19 mmHg, p = 0.0001). The rating of quality assessment was weak because of selection bias, study design and blinding procedures.
A prospective observational study was carried out at the Israeli Naval Special Warfare Unit base with 23 healthy combat personnel. Participants applied CAT more quickly than SOFTT to the thigh, while CAT and SOFTT applications were much quicker than for IRT which required nearly double the time to apply, resulting in high fail rates for IRT. Failure rates for self‐application were lower in CAT than in SOFTT but the difference was not significant (14% vs 20%, p = 0.50). This was the only prospective cross‐sectional study with a moderate rating in quality assessment, which was due to weak blinding.
Retrospective studies
Three journal articles reporting retrospective studies were retrieved, two of which were US studies and one from Israel. The success rate of prehospital CAT was shown to be quite high for saving lives with fewer adverse effects, but the quality of all studies was weak because of the nature of retrospective studies.
In one retrospective study, researchers reviewed medical charts of all trauma patients with tourniquets applied from the Trauma Registry of the Los Angeles County and University of Southern California Hospital between 2007 and 2014. Over 50% of trauma patients were injured from stab wounds and tourniquets were used in prehospital settings. Injuries were 2.5 times more frequent on upper extremities than lower extremities. The type of tourniquet most often used in prehospital settings was CAT. There were 15.15% amputations (15 of 99 operations), of which nine were partial or full amputations at the scene and five had severe tissue damage from their injuries. Researchers concluded that amputations were not caused by tourniquet use, and no mortality rate was reported. Four components were rated weak in quality assessment: selection bias, study design, confounders and blinding.
A retrospective cohort study was conducted in the United States between 2008 and 2013 with 105 patients who had traumatic injury, with CAT applied either prehospital or in the Emergency Department at The Texas Trauma Institute – Memorial Hermann Hospital. Of the tourniquets applied, 78% were placed by prehospital staff and major causes of injury were limb laceration (40%) followed by traumatic amputation (29%). Over 80% of patients showed no complications associated with tourniquet use. Almost 30% of patients who had tourniquets applied underwent amputation because of the direct consequences of injuries, including traumatic amputation, non‐salvageable limbs or completion or partial amputation. Mortality rate with tourniquet use was 14%. Five components were rated weak in quality assessment, namely selection bias, study design, confounders, blinding and data collection.
Analysis of retrospective data from the Israel Defence Force Trauma Registry collected during July and August 2014 showed that 119 tourniquets were applied to 90 casualties. The major mechanism of injury was penetrating wounds caused by improvised explosive devices and shrapnel injuries. Nearly 90% of tourniquet applications used CAT and a success rate at first attempt was 70%, regardless of caregiver skills, tourniquet type or limb characteristics. The survival rate was nearly 90% with a complication rate of just over 11%, and three patients underwent amputations. This study was rated weak for study design, confounders and blinding.
Adverse effects of tourniquet applications
Three prospective randomised studies demonstrated no complications of tourniquet application with pain complaints in fewer than 5% of cases. Similarly, discomfort and minor pain were reported in three studies of prospective comparative studies,, while there were no reports of complications in one study. Discomfort and minor pain after tourniquet applications were reported in two prospective cross‐sectional studies carried out on healthy volunteers, but in the study by Kragh et al. at a combat support hospital, nearly 90% cases required surgery to amputate or shorten limbs when tourniquets were applied for 2 h or more. In the retrospective studies, approximately 2% of cases developed compartment syndrome and other complications in one study, Scerbo et al. found over 80% had no complications related to tourniquet application and Shlaifer et al. found nearly 12% of complications.
When assessing adverse effects of tourniquet application reported in the 14 articles in this review, use of commercial tourniquets, especially CAT, resulted in fewer complications such as compartment syndrome and neurological deficits but induced pain could not be avoided. Amputations associated with tourniquet use occurred because of the primary injury itself and were not directly associated with tourniquet application.
Discussion
While the use of tourniquets was once controversial because of complications attributed to their use, research and development over many years means that tourniquets are now suitable for saving lives while minimising adverse effects. After examining 14 articles about the efficacy of commercial tourniquets, one conclusion is that CAT might be a good option in prehospital settings for preventing massive haemorrhage and exsanguination death and with a low risk of complications. Considering tourniquet characteristics, wider tourniquets seemed to be more suitable for the occlusion of arterial blood flow at a lower pressure. Although CAT (38 mm) is narrower than SWATT (104 mm) and EMT (80 mm) (see Table 1), it showed superior efficacy in terms of blood flow occlusion than SWATT but not EMT. However, EMT was not developed for use in prehospital environments. Furthermore, when CAT was applied adequately and correctly with three turns of the windlass, it was effective in occluding arterial flow in over 90% of cases. Using band routing through the buckle on CAT, which can be performed once or twice, makes it easier and faster to apply and the double‐routing also prevents the band from slipping when more torque is required, thereby controlling haemorrhage and the overall volume of blood lost. Results are inconclusive about whether CAT is superior to other commercial tourniquet devices for prehospital exsanguination treatment because of research design, sample size and confounding factors. However, a commercial tourniquet, especially CAT, might be a suitable medical device in the first instance as a potential limb tourniquet to stop uncontrolled haemorrhage. CAT does require several modifications to improve its efficacy and effectiveness to stop haemorrhaging in trauma victims, especially a wider band and increased tightening capacity to stop arterial blood flow in a short period of time with fewer adverse effects. However, as first responders and prehospital personnel, we need to start using tourniquet application as a first‐line treatment for life‐threatening limb haemorrhage in patients facing prolonged transport periods and limited resources, particularly in rural areas. Haemorrhage control is critical in saving people's lives and this takes precedence over doubts about the efficacy of tourniquets.
As with other medical treatment devices, there have been complications associated with tourniquet application, with concerns about use contributing to amputation, severe ischemic and neurologic injury. Such apprehension is appropriate when improvised tourniquets are used, while commercial prehospital tourniquets that have been researched and developed over time have contributed to positive outcomes and minimised adverse effects. A primary adverse event noted from nearly all 14 studies was minor pain and discomfort related to tourniquet application because of compression tissue injury or damage, which can be resolved promptly after deflating tourniquet devices. Studies have shown that the pain from tourniquet application was relieved within a few seconds and this contributed to a sensation of wellbeing. Nevertheless, an aching sensation appeared in less than 1 min and reached a peak after 2 min before sensation returned to normal. Only one of the 14 studies reviewed identified that tourniquet application contributed to almost 90% of limb shortening because of prolonged tourniquet application for 2 h, but in 75% of cases this was related to the injuries sustained. In orthopaedic surgery in hospitals, a 2‐h time period is generally accepted as the safe limit because longer periods of tourniquet application could lead to progressive neuromuscular injury. Hospitals are more likely to use pneumatic devices (e.g. EMT) rather windlass tourniquets (e.g. CAT). The argument has been raised that to reduce or prevent neurological complications, the maximum safe time for tourniquet application should be 78 min. Prehospital transportation can be completed within this time in most rural or regional locations. Apart from terrorist attacks in urban areas, various forms of trauma incidents have been found in regional/remote areas, including interpersonal violence, shootings, workplace injuries from mining/farm equipment, and road and traffic crashes. Many of these have resulted in life‐threatening limb haemorrhage in which tourniquet use might prevent limb exsanguination and save lives.,
Ambulance personnel as first responders need to stop limb haemorrhage and they should not hesitate to use tourniquets for short periods to limit blood loss while expediting transport to the nearest trauma/hospital setting. This action is more beneficial to patient survival than not applying tourniquets because of concerns about possible complications. In severely injured patients, the time taken to apply direct pressure dressings could accelerate onset of haemorrhagic shock from uncontrolled haemorrhage, with limited prospects for survival.
Implications
No new information has emerged from this systematic review, but it has confirmed that commercial tourniquet applications are useful devices with benefits that outweigh adverse complications, and these findings should be endorsed by ambulance officers and first responders when organising haemorrhage control. Furthermore, international organisations have recommended using limb tourniquets in civilian first aid, and the use of commercial tourniquet devices should be advocated, particularly CAT which has been proved successful for battle and non‐battle injuries in some studies. While availably commercial tourniquets seem to offer greater benefits than improvised tourniquets, education and training in tourniquet applications for first responders is essential because the key to tourniquet effectiveness depends upon stopping arterial blood flow with limited pressure‐gradient force on nerves. Adequate knowledge of tourniquet application and proper training of users will improve care for trauma victims and save many human lives.
Limitations of the study
In this study, the journal articles reviewed included prospective randomised controlled trials, prospective comparative and cross‐sectional studies but none of them received the highest ‘strong’ ranking in quality and bias assessments. Features that affected quality included using healthy volunteers as subjects who might not be representative of the target population, non‐randomised trials and uncontrolled confounding. Furthermore, most studies had small sample sizes of around 20 participants, which gave low statistical power and undermined internal and external validity. Apart from these limitations, the strengths of this study included the use of two evaluators, the extensive and comprehensive search of six databases with no limit on year of publication, and the application of an appropriate assessment tool for quality assessment of observational and clinical studies based on populations.
Authorship
The author conducted a literature search, analysed, drafted and revised a whole article.
Availability of data and materials
Data sharing was not available because no dataset was generated as a systematic review study.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed consent
Written informed consent was not necessary because no patient data have been included in the manuscript.
ORCID iD
Nualnong Wongtongkam
https://orcid.org/0000‐0001‐7623‐6608
Acknowledgements
The author would like to express gratitude to a research assistant in assisting literature search.
References
- 1. Beaucreux C, Vivien B, Miles E, et al. Application of tourniquet in civilian trauma: systematic review of the literature. Anaesth Crit Care Pain Med 2018; 5: S2352–S5568.
- 2. Edwards DS, McMenemy L, Stapley SA, et al. 40 years of terrorist bombings – a meta‐analysis of the casualty and injury profile. Injury 2016; 47(3): 646–652.
- 3. Khan F, Amatya B, Gosney J, et al. Medical rehabilitation in natural disasters: a review. Arch Phys Med Rehabil 2015; 96(9): 1709–1727.
- 4. Rtshiladze MA, Andersen SP, Nguyen DQ, et al. The 2009 Sydney shark attacks: case series and literature review. ANZ J Surg 2011; 81(5): 345–351.
- 5. Ricci JA, Vargas CR, Singhal D, et al. Shark attack‐related injuries: epidemiology and implications for plastic surgeons. J Plast Reconstr Aesthet Surg 2016; 69(1): 108–114.
- 6. Lee C, Porter KM. Tourniquet use in the civilian prehospital setting. Emerg Med J 2007; 24(8): 584–587.
- 7. Dayan L, Zinmann C, Stahl S, et al. Complications associated with prolonged tourniquet application on the battlefield. Mil Med 2008; 173(1): 63–66.
- 8. Richey SL. Tourniquets for the control of traumatic hemorrhage: a review of the literature. World J Emerg Surg 2007; 2: 28.
- 9. Wakai A, Winter DC, Street JT, et al. Pneumatic tourniquets in extremity surgery. J Am Acad Orthop Surg 2001; 9(5): 345–351.
- 10. Kragh JF Jr, Walters TJ, Baer DG, et al. Practical use of emergency tourniquets to stop bleeding in major limb trauma. J Trauma 2008; 64(Suppl. 2): S38–S49; discussion S49–S50.
- 11. Kragh JF Jr, Littrel ML, Jones JA, et al. Battle casualty survival with emergency tourniquet use to stop limb bleeding. J Emerg Med 2011; 41(6): 590–597.
- 12. Schroll R, Smith A, McSwain NE Jr, et al. A multi‐institutional analysis of prehospital tourniquet use. J Trauma Acute Care Surg 2015; 79(1): 10–14; discussion 14.
- 13. Scerbo MH, Holcomb JB, Taub E, et al. The trauma center is too late: major limb trauma without a pre‐hospital tourniquet has increased death from hemorrhagic shock. J Trauma Acute Care Surg 2017; 83(6): 1165–1172.
- 14. Kue RC, Temin ES, Weiner SG, et al. Tourniquet use in a civilian emergency medical services setting: a descriptive analysis of the Boston EMS experience. Prehosp Emerg Care 2015; 19(3): 399–404.
- 15. El Sayed MJ, Tamim H, Mailhac A, et al. Trends and predictors of limb tourniquet use by civilian emergency medical services in the United States. Prehosp Emerg Care 2017; 21(1): 54–62.
- 16. Passos E, Dingley B, Smith A, et al. Tourniquet use for peripheral vascular injuries in the civilian setting. Injury 2014; 45(3): 573–577.
- 17. Drew B, Bennett BL, Littlejohn L. Application of current hemorrhage control techniques for backcountry care: part one, tourniquets and hemorrhage control adjuncts. Wilderness Environ Med 2015; 26(2): 236–245.
- 18. Wall PL, Sahr SM, Buising CM. Different width and tightening system: emergency tourniquets on distal limb segments. J Spec Oper Med 2015; 15(4): 28–38.
- 19. Thomas BH, Ciliska D, Dobbins M, et al. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs 2004; 1(3): 176–184.
- 20. Walters TJ, Wenke JC, Kauvar DS, et al. Effectiveness of self‐applied tourniquets in human volunteers. Prehosp Emerg Care 2005; 9(4): 416–422.
- 21. Savage E, Pannell D, Payne E, et al. Re‐evaluating the field tourniquet for the Canadian forces. Mil Med 2013; 178(6): 669–675.
- 22. Ünlü A, Petrone P, Guvenc I, et al. Combat application tourniquet (CAT) eradicates popliteal pulses effectively by correcting the windlass turn degrees: a trial on 145 participants. Eur J Trauma Emerg Surg 2015; 43: 605–609.
- 23. King RB, Filips D, Blitz S, et al. Evaluation of possible tourniquet systems for use in the Canadian forces. J Trauma 2006; 60(5): 1061–1071.
- 24. Taylor DM, Vater GM, Parker PJ. An evaluation of two tourniquet systems for the control of prehospital lower limb hemorrhage. J Trauma 2011; 71(3): 591–595.
- 25. Beaven A, Briard R, Ballard M, et al. Two new effective tourniquets for potential use in the military environment: a serving soldier study. Mil Med 2017; 182(7): e1929–e1932.
- 26. Wall PL, Duevel DC, Hassan MB, et al. Tourniquets and occlusion: the pressure of design. Mil Med 2013; 178(5): 578–587.
- 27. Heldenberg E, Aharony S, Wolf T, et al. Evaluating new types of tourniquets by the Israeli naval special warfare unit. Disaster Mil Med 2015; 1: 1.
- 28. King DR, van der Wilden G, Kragh JF Jr, et al. Forward assessment of 79 prehospital battlefield tourniquets used in the current war. J Spec Oper Med 2012; 12(4): 33–38.
- 29. Inaba K, Siboni S, Resnick S, et al. Tourniquet use for civilian extremity trauma. J Trauma Acute Care Surg 2015; 79(2): 232–237; quiz 332–333.
- 30. Scerbo MH, Mumm JP, Gates K, et al. Safety and appropriateness of tourniquets in 105 civilians. Prehosp Emerg Care 2016; 20(6): 712–722.
- 31. Shlaifer A, Yitzhak A, Baruch EN, et al. Point of injury tourniquet application during operation protective edge‐what do we learn? J Trauma Acute Care Surg 2017; 83(2): 278–283.
- 32. Doyle GS, Taillac PP. Tourniquets: a review of current use with proposals for expanded prehospital use. Prehosp Emerg Care 2008; 12(2): 241–256.
- 33. Weppner J, Lang M, Sunday R, et al. Efficacy of tourniquets exposed to the Afghanistan combat environment stored in individual first aid kits versus on the exterior of plate carriers. Mil Med 2013; 178(3): 334–337.
- 34. Clumpner BR, Polston RW, Kragh JF Jr, et al. Single versus double routing of the band in the combat application tourniquet. J Spec Oper Med 2013; 13(1): 34–41.
- 35. Estebe JP, Le Naoures A, Chemaly L, et al. Tourniquet pain in a volunteer study: effect of changes in cuff width and pressure. Anaesthesia 2000; 55(1): 21–26.
- 36. Lakstein D, Blumenfeld A, Sokolov T, et al. Tourniquets for hemorrhage control on the battlefield: a 4‐year accumulated experience. J Trauma 2003; 54(Suppl. 5): S221–S225.
- 37. McDonell AC, Veitch C, Aitken P, et al. The organisation of trauma services for rural Australia. J Emerg Prim Health Care 2009; 7(2): 990308.
- 38. Singletary EM, Charlton NP, Epstein JL, et al. Part 15: first aid: 2015 American heart association and American red cross guidelines update for first aid. Circulation 2015; 132(18 Suppl. 2): S574–S589.
- 39. Zideman DA, De Buck ED, Singletary EM, et al. European resuscitation council guidelines for resuscitation 2015 section 9. Resuscitation 2015; 95: 278–287.