Key Messages:
Coping skills are likely to determine relapse in alcohol dependence. Empowering individuals with better coping strategies can help improve outcomes in persons suffering from alcohol-related problems.
The National Mental Health Survey of India 2015–2016 shows that the prevalence of Alcohol use disorders in adult men in India is 9%. High relapse rates and difficulty in maintaining abstinence are the core characteristics of alcohol dependence. Therefore, during the course of this psychiatric illness some patients with alcohol dependence relapse while others do not. Coping is a way of striving to manage the demands placed on a person by stressful circumstances that are seen to be exhausting or surpassing a person’s resources. Coping may also be understood as an action-oriented psychic effort made by an individual in an attempt to overcome a life event perceived as stressful. In an alcohol-dependent individual, coping would also refer to what the person thinks or does in a particular situation in an effort to overcome the risk of using alcohol again and again. Several Western studies have established a strong relationship between coping and relapse prevention in alcohol dependence. Research has also found that alcohol-dependent persons who may not have adequate coping strategies are more likely to have a relapse. Coping strategies are theoretically divided into those that are approach-oriented and those that are problem-oriented. Research in the past has shown that, while avoidance coping is associated with psychological adjustment, active coping leads to better psychological adaptation. Coping skills training helps patients to feel less overwhelmed by urge-provoking stimuli and therefore are less likely to relapse. Based on the relapse prevention paradigm, coping, self-efficacy, positive expectations, and the abstinence violation effect were all observed as risk factors for recurrence. The only substantial independent predictor of relapse was abstinence violation. The coping skills of alcohol-dependent subjects are inferior to the coping skills of non-alcoholics, particularly in situations that commonly pose a risk of relapse. Understanding the ways of handling coping would help mental health professionals to individualize successful strategies for relapse prevention. This research, therefore, aims to systematically understand the coping strategies of alcohol-dependent persons during a follow-up period of six months and to compare the coping styles of relapsed and non-relapsed persons.
Methods
This cross-sectional research was performed in the outpatient de-addiction services of the Department of Psychiatry at Chengalpattu Medical College which is a tertiary care, teaching institution situated in Tamil Nadu, South India. We employed the ICD 10 criteria for making a diagnosis of alcohol dependence in our participants.
Participants
One hundred and twenty-seven consecutive individuals were recruited over 14 months from April 2019 to June 2020. The majority of our study participants had completed their six-month follow-up period well before the Covid lockdown on 25 March 2020. Only a few participants who resided in areas near our hospital were followed up during the strict Covid lockdown period, from April 2020 to June 2020. We included individuals above 18 years attending our outpatient de-addiction services, who qualified for a diagnosis of Alcohol Dependence and were also abstinent from alcohol for one month. We excluded individuals with a history of major psychiatric illness, co-morbid substance use other than tobacco, if they have had in-patient treatment in the past, and those who currently require in-patient treatment.
All the participants and their spouses/caregivers were explained in detail about the importance and potential benefits of taking part in this research. We also made meticulous efforts to make our participants understand that their personal information would be kept strictly confidential. A comprehensive clinical psychiatric interview was conducted by the second author in a comfortable environment. The average duration of the interview including the administration of assessment scales was about one hour per participant, at baseline. All trial participants were requested to come for a regular follow-up at monthly intervals. During the follow-up visit, we elicited a detailed psychiatric history, including alcohol use history during the past 30 days. Becker, defines relapse as the restart of alcohol use after a prolonged period of abstinence. Considering the paucity of research on the exact time frame of relapse, we have only included individuals with a history of 30 days of abstinence from alcohol at baseline. Those who reported having consumed alcohol during this period were categorized as relapsed. We made every effort to corroborate the alcohol use information provided by the participants, by interviewing the spouses and/or close relatives who were living with them. Motivation Enhancement Therapy (MET) was administered by the second author to all the trial participants during their monthly follow-up visits. Each MET session lasting for an hour focused on helping our participants gain greater awareness of their behavior, exploring coping strategies, resolving ambivalence, and encouraging their commitment to remain abstinent from alcohol. Figure 1 summarizes the procedure and recruitment of the final sample. Twenty-four persons failed to complete the six-month follow-up period. We contacted all 24 individuals over the phone to convince them about the benefits of continuing to participate in this study. While 14 refused to come back citing some personal reasons, 10 persons returned for the second follow-up only to drop out in the third month. Institutional Ethical Committee at Chengalpattu Medical College granted the approval for performing this research. Written informed consent was obtained from all the individuals who were willing to be a part of this research. The sample size was estimated according to a previous study by Suresh Kumar et al. To detect a two-sided significant difference between groups with a power of 80% and a significance level of 5%, the required sample size was estimated to be 96 participants. Since we anticipated a 30% dropout rate, we adjusted our sample size to 125.
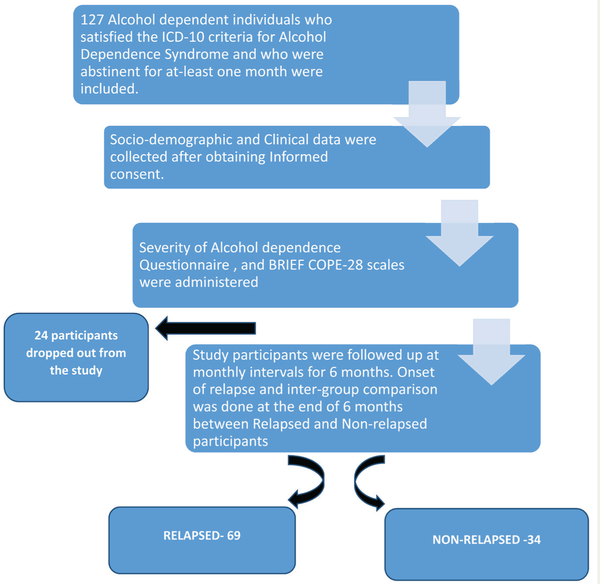
Flow Chart Depicting the Procedure.
Materials
Semi-structured Questionnaire
We used a semi-structured proforma which was designed by us to elicit data such as age, sex, educational qualifications, occupation, socio-economic status, marital status, and family history of any substance use.
Severity of Alcohol Dependence Questionnaire (SADQ)
The SADQ was used to assess the degree of alcohol dependence. It consists of 20 questions encompassing physical and affective withdrawal symptoms, relief drinking, frequency of alcohol intake, and the beginning of withdrawal symptoms. Each question’s response is graded on a 4-point scale. A score of 31 or greater suggests severe, 16–30 indicates moderate, and less than 16 shows mild alcohol dependence.
Coping Orientation to Problems Experienced Inventory (Brief-COPE)
We used the Brief-COPE to measure coping in our participants. It is a 28-item self-reportquestionnaire with three sub-scales: problem-focused coping, emotion-focused coping, and avoidant coping. In addition, the following facets of coping are reported: Self-distraction, Active coping, Denial, Substance use, Use of emotional support, Use of instrumental support, Behavioral disengagement, Venting, Positive reframing, Planning, Humor, Acceptance, Religion, & Self-blame. Average scores are obtained by dividing the sum of item scores and the number of items.
Statistical Analysis
We carefully recorded the data collected in a Microsoft Excel spreadsheet. This data was then subjected to statistical evaluation using the Statistical Product and Service Solutions (SPSS; Version 20.0 IBM Corp., Armonk, NY). Continuous variables have been presented in the form of Mean and Standard deviation. Comparison of means of continuous variables between groups was done by a t-test, to examine the potential differences between the two groups. Categorical variables have been shown in the form of frequency distributions and percentages. We used the chi-squared test to examine the potential associations between the categorical variables. To understand the correlation between the severity of alcohol dependence and the type of coping strategies we used Spearman’s correlation statistics. In our statistical analysis, the probability value of p < .05 was considered significant.
Results
We followed 103 male participants for a period of six months. At the end of the follow-up period, 69 out of the total 103 (66%) patients relapsed.
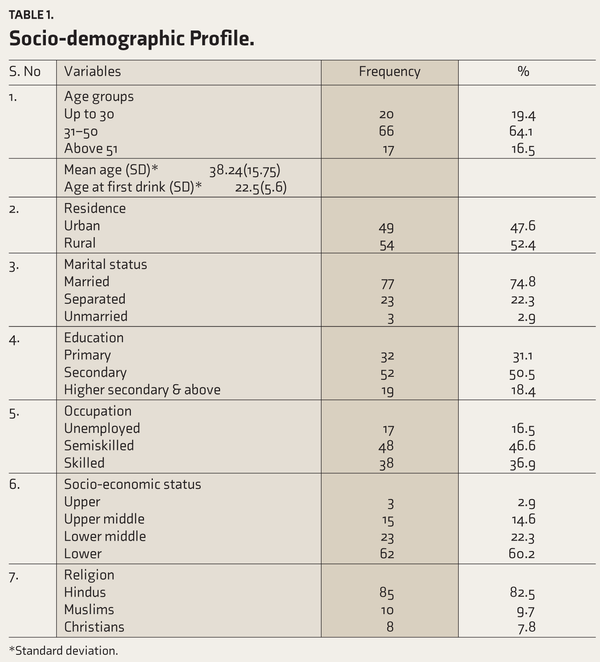
Table 1 shows the socio-demographic profile of our study sample. The mean age of our research subjects was 38.24 ± 15.75 years. Participants’ age at first drink was 22.5 ± 5.6 years. Sixty-six out of 103 (64.1%) study participants belonged to the age group of 31 and 50 years. More than half of our participants hailed from rural areas. Fifty-two (50.5%) of our subjects had completed secondary school education. While 49 persons (46.6%) were involved in semi-skilled jobs, 17 (16.5%) of them were unemployed. Sixty-two (60.2%) participants belonged to the lower socio-economic class. Eighty-five (82.5%) of our study subjects were Hindus. While 10 (9.7%) were Muslims, eight (7.8%) practiced Christianity.
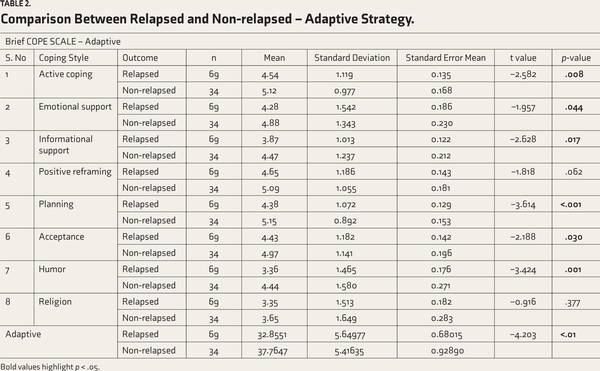
Table 2 indicates the results of the comparison between individuals who have relapsed versus non-relapsed on the adaptive sub-scale of Brief-COPE. Non-relapsed persons were practicing coping styles like active coping (p = .008), informational support (p = .017), emotional support (p = .044), planning (p < .001), acceptance (p = .03) and humor (p = .001) significantly greater than the relapsed subjects. Non-relapsed subjects were found to be practicing adaptive coping styles significantly (p < .01) more than the relapsed subjects. No statistically significant differences were found between the two groups in practicing coping styles like positive reframing and religion.
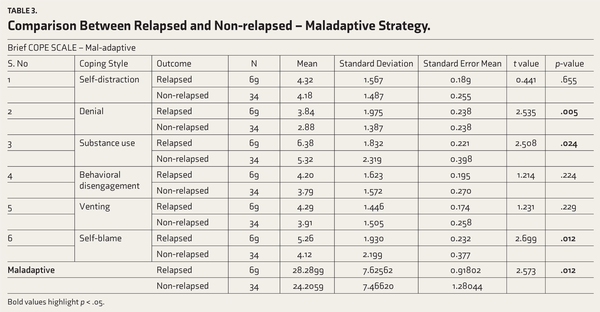
Table 3 summarizes the comparisons between relapsed and non-relapsed subjects on the maladaptive sub-scale of Brief-COPE. Relapsed individuals were practicing styles like denial (p = .005), substance abuse (p = .024), and self-blame (p = .012) more than the Non-relapsed persons and these differences were statistically significant. Relapsed persons were practicing maladaptive coping strategies significantly more (p = .012) than those who did not relapse. No statistically significant differences were found between the two groups of participants in practicing coping styles like self-distraction, behavioral disengagement, and venting.
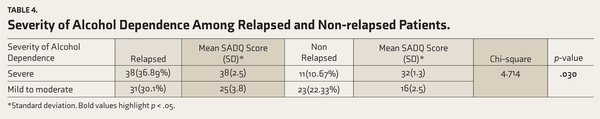
Table 4 summarizes the results of the severity of alcohol dependence among relapsed and non-relapsed patients on the SADQ. Thirty-eight (36.89%) relapsed patients had severe alcohol dependence compared to 11 (10.67%) non-relapsed patients. A statistically significant (p = .03) severe alcohol dependence was found among the relapsed individuals. There were, however, no significant differences among relapsed versus non-relapsed with mild to moderate severity of alcohol dependence. Relapsed participants with severe alcohol dependence had a mean SADQ score of 38 ± 2.5, while non-relapsed participants had a mean score of 32 ± 1.3, at baseline. In participants with mild to moderate alcohol dependence, the mean SADQ scores of relapsed and non-relapsed persons were 25 ± 3.8 and 16 ± 2.5, respectively.
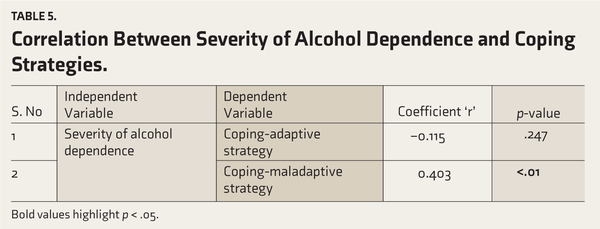
Table 5 shows the correlation between coping strategies and the severity of alcohol dependence. We found a weak, statistically non-significant negative correlation (r = -0.115) between the severity of alcohol dependence and adaptive coping strategies. We also observed a moderate positive correlation (r = 0.403) between the severity of alcohol dependence and maladaptive coping strategies. This was statistically significant (p < .01).
Discussion
It is critical to analyse and comprehend coping mechanisms in order to elucidate the association between exposure to high-risk life conditions for alcohol use and relapse. Past literature has clearly established the seminal role played by coping behaviors not only in repeated abuse of alcohol, but also in the prevention of relapse. Similarly, studies on coping with regard to specific relapse crises have consistently shown that persons who do not utilize any coping response are more vulnerable to relapse. Litt et al. who have a more quantitative approach to the concept of coping found that increased coping skills, during treatment, were a significant predictor for abstinence. We examined the baseline coping strategies of our participants at the time of recruitment into the study. During their monthly follow-up visits, we encouraged the individuals to identify triggers and make them understand their coping resources and strategies. Thus, we tried to equip each of our subjects with the greatest number of relapse-prevention coping strategies during their MET sessions. To our knowledge, there are very few Indian studies that attempt to enhance the coping strategies of persons dependent on alcohol and then to understand the differences between relapsed versus non-relapsed after a six-month follow-up period. This study is therefore an attempt to provide an enhancement of coping skills and strategies that would help individuals to remain abstinent from alcohol within the safe environment of a treatment setting.
The mean age of our participants was 38.24 ± 15.75 years. Sarkar et al., in a study conducted at a tertiary care center, have reported a similar finding of the highest prevalence of alcohol dependence among the 30 to 40-year age group. In their first study that documented national estimates of continual consumption of alcohol in India, Neufeld et al., observed that regular alcohol usage peaked (15%) in India in the fifth decade of life, relative to the second decade of life (71%; 21–28 years) in the United States. Our study findings correlate well with the above-mentioned reports. Our participants’ age at first drink was 22.5 ± 5.6 years. In their research with improved methods and a general hospital sample of problem drinkers, Johnson et al., determined that the age of onset is a more reliable indicator of the extent of alcoholism than a family history of alcoholism alone; the average age of commencement of alcohol drinking was reported as 21.39 ± 5.34 years. Among the individuals serving in the Indian Armed Forces, Chatterjee et al., observed no link between the age at first consumption and severity of alcohol dependence at detection. Similar to these reports, we observed that participants up to the age of 30 had statistically non-significant higher scores on the SADQ. Three-fourths of our study participants had their first use of Alcohol before 25 years of age. The easy availability of alcohol through government-controlled outlets and the availability of higher disposable income could explain the greater abuse and younger age of first-time users of alcohol in rural areas of Tamil Nadu.
We observed that 66% of our participants had relapsed at the end of the six-month follow-up period. Past Western studies have shown a remission rate of 20%–50% typically in treated samples., In a study that investigated the rates and predictors of three-year remission and subsequent 16-year relapse among initially untreated patients with alcohol use disorders who were not seeking help or who participated in treatment and/or Alcoholics Anonymous in the first year after acknowledging their need for help, Moos et al. indicated a 43% remission rate. A non-relapse/remission rate of 34% in our sample is consistent with the findings of the above studies. Our subjects sought professional help around 16 years after their first drink. This delay in seeking help could have contributed to a higher relapse rate in our sample. The majority of our participants were from a lower socioeconomic class and a rural background. This could also have contributed to a delay not only in recognizing an alcohol-related problem but also in seeking professional help. In a similar vein, Moos et al. have found that people who acknowledge that they have an alcohol use problem and initiate the process of seeking help but do not get help quickly are at a double disadvantage: they are far less likely to attain remission and, following remission, they are at a greater risk of relapse. Lower socioeconomic status could either trigger substance abuse or be a result of social disruption caused by the onset of dependence at an early age. Unemployment combined with economic challenges is well known to increase the likelihood of a relapse.,
Similar to the above-mentioned reports, we found that 85% of our subjects belonged to a lower socio-economic class and a majority of these individuals had relapsed. We also observed that more than half of our unemployed participants had relapsed. One-third of our participants had completed primary education and the rest had completed secondary school and above. We did not find any statistically significant differences between our primary versus secondary school-educated participants. Conversely, Rampure et al. found that those with no formal education or who just completed elementary school had a much greater relapse rate than those who received education (68.5% vs. 43.1%). Twenty-two percent of our participants had separated from their spouses. A greater number of relapsed participants had separated when compared to those who did not relapse. This difference was, however, not statistically significant. Contrary to our findings, Pilowsky et al., have reported that people who were divorced/separated or had a breakup of a steady relationship in the 12 months before Wave 1 were over two times as likely (OR = 2.32; 95% CI: 1.01–5.34; p = .05) to relapse compared to those who did not experience such an event.
Even though we did not objectively assess for stressful life events, we did observe that a majority of our participants with relapse had shared the details of both positive and negative life stress during their monthly follow-up visits. Christina et al., observed, identical to our results, that unpleasant life experiences predicted relapse in all participants. Positive life experiences predicted alcohol relapse in persons who had a history of an alcohol use disorder before entering the study. We found non-relapsed individuals to have significantly higher active coping and information support. These skills could have helped them deal with stressful life situations and also overcome those situations in which they felt tempted to use alcohol. A higher acceptance coping style in non-relapsed persons could have helped them accept or confront life problems due to alcohol than due to their environment or family. Such approach-oriented positive coping styles found in our non-relapsed persons could mean that they assumed greater responsibility for their actions including a relapse.
Higher emotional support in our non-relapsed subjects could indicate positive family behaviors and better social support. These are important predictors of long-term abstinence from alcohol. In contrast, relapsed persons shared with us during their follow-up sessions a higher degree of poor social support in the form of interpersonal conflicts and also negative family behaviors like avoiding alcohol-dependent persons. Our relapsed patients reported increased anger, loneliness, boredom, and negative affect due to avoidance by close family members. Similar to our study, Shanmugham et al., found that relapsed patients have observed considerably higher expressed emotions from family members than abstinent patients. Patients who relapsed experienced high criticism, irritability, excessive interference, and a lack of required emotional assistance. Chauhan VS et al. had reported that emotional support is an important factor in determining abstinence from alcohol. McKay has similarly reported how sad negative mood states increased the risk of relapse during and after treatment for alcohol dependence. Cooney et al. have documented how the display of alcoholic beverages and negative affect imagery led to an enhanced self-reported urge to drink and forecasted the time to relapse following discharge from the hospital.
Relapsed individuals showed significantly higher negative coping styles like denial, self-blame, and substance abuse. Self-distraction and venting were higher but not statistically significant among relapsed individuals. Higher denial could contribute to rationalization and a desire for immediate gratification. These in turn contribute as the precursors of an increased risk of relapse. In contrast, our non-relapsed subjects showed significantly higher adaptive coping strategies like active coping, informational support, planning, acceptance, and humor. Our non-relapsed participants reported during their follow-up visits that they had an improvement in their emotional reactivity and negative mood states. A significant acceptance of coping could have contributed to this. In their preliminary findings, Vieten et al. stated that acceptance-based relapse prevention offers the potential for preventing alcohol relapse and enhancing mood, emotional reactivity, craving, negative affect, positive affect, and mindfulness and that more research is essential. Mindfulness- and acceptance-based treatments challenge traditional notions of affect regulation in that they focus on allowing distressing cognitions and affective states to remain as they are, rather than working to alter or change their content.
In our study, no statistically significant difference was found between relapsed and non-relapsed participants in practicing coping styles like positive reframing and religion. The majority of our study participants practiced the Hindu religion. Even though relapse was numerically higher among our Hindu participants, it was not statistically significant. All our participants, irrespective of their religion revealed during their interviews that faith in their holy texts did help them to overcome urges to consume alcohol in certain specific situations. Belief in religious rituals and spirituality is found to be beneficial to many males with Alcohol Use Disorder (AUD). Most of our participants revealed during their follow-up sessions that activities like chanting the holy names of God, studying religious scriptures, participating in religious activities such as listening to discourses by eminent spiritual persons and singing/listening religious songs were very helpful for them in giving greater inner strength and peace of mind. Regardless of religious origin, carers viewed prayer and religious rituals as a source of optimism and a means of improving their family members’ drinking behaviors. A Lebanese study reported that among ever-drinkers, the chances of alcohol use disorders were equal across religious groups. Belief in God and practicing one’s religion were linked inversely to alcohol dependence in all religious groups, even among drinkers (belief in God only). The associations were occasionally stronger for Muslims, indicating that, as proposed by ‘reference group theory’, religiosity may play a more significant part in a more proscriptive religion.
We observed that persons with a maladaptive coping strategy had a significantly greater severity of alcohol dependence. Even though non-significant, we did observe that participants having adaptive coping strategies also had less severe alcohol dependence. We also observed a weak negative correlation between the severity of alcohol dependence and adaptive coping styles. This suggests that increasing adaptive coping strategies in a person is likely to lead to a decrease in the severity of alcohol dependence which may, in turn, reduce the chances of a relapse.
Coping strategies were found to be a significant predictor of alcohol consumption in a study of young adult social drinkers. Using alcohol to avoid contemplating a problem, that is, as a coping method, correlated with greater consumption of alcohol per drinking episode and more recurrent alcohol usage. In addition, in a study of problem drinkers, coping with difficulties without the use of alcohol was related to decreased levels of drinking. Another research on alcohol consumption among university students discovered that those who used alcohol to cope with stressful events consumed more alcohol than those who did not use alcohol to cope. Our findings are similar to those of the previous researchers.
Coping strategies and styles are the most critical predictors of relapse in alcohol-dependent persons. The most consistent finding in research investigations looking at predictors of relapse in alcoholism is a link between self-efficacy and alcohol relapse., Self-efficacy refers to an individual’s inner expectations about the probable effectiveness of specific coping strategies. Effective coping strategies and positive coping styles enhance an alcohol-dependent person’s inner strength to deal with certain ‘high-risk’ life situations. A high-risk situation is a typical life circumstance during which the alcohol-dependent person feels a highly irresistible urge and temptation to consume alcohol. During the follow-up visits, we provided motivational enhancement therapy to all our study subjects, focusing on problem-solving coping styles and strategies to effectively deal with high-risk situations. Specifically, we taught all our participants to ident-ify, avoid, and remove stimuli that are likely to induce craving. We also demonstrated how to alter their cognitive ideation when they were confronted with high-risk situations. We consistently observed that our relapsed participants with a greater maladaptive coping style often failed to think of various possible solutions, when confronted with a problem. We also observed that our non-relapsed participants with positive coping styles could be easily taught to identify, avoid, or adapt to high-risk situations. Our non-relapsed subjects who shared their experience of having coped successfully with high-risk situations using adaptive coping strategies were assumed to experience a heightened sense of self-efficacy. Our observations were similar to the findings reported by Turkish authors who looked at ways of problem-solving among relapsed individuals. They observed that persons who relapsed examined their current life situation to find alternate problem-solving strategies before acting, but if the solution is unsuccessful, they fail to do a retrospective appraisal and tend to ignore the problem. As a result, it is possible that relapsers fail to improve their problem-solving techniques. Limited problem-solving options promote the activation of previously learnt drinking behavior, which has taken on an automatic nature, and therefore increases the likelihood of relapse. It may be said that individuals who are remitters place a greater emphasis on finding alternatives to probable solutions in a problematic life scenario and are therefore more successful in remaining abstinent for a prolonged period. Individuals who utilize an avoidant approach are less likely to be engaged in problem-solving and are more prone to relapse.
The findings of our study cannot be generalized. Our findings should be interpreted as preliminary because they are limited by several factors like the study sample being hospital-based, lack of a control group, small sample size, shorter duration of follow-up period, and the presence of confounding factors. We have also not assessed the impact of personality factors on coping styles. We have not objectively assessed stressful life events, childhood trauma, and social support in our participants.
Conclusions
Alcohol dependence is common in the fourth decade of life. Subjects who were unemployed and belonging to a lower socioeconomic class had a greater relapse. Maladaptive coping strategies were associated with a greater severity of alcohol dependence. Non-relapsed persons with alcohol dependence had significantly higher positive and adaptive coping strategies. Relapsed persons, in contrast, had significantly higher negative and maladaptive coping strategies.
Declaration of Conflicting Interests The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Eashwar VA, Umadevi R, Gopalakrishnan S. Alcohol consumption in India–an epidemiological review. J Fam Med Pri Care Rev. 2020; 9(1): 49.
- 2. Folkman S, Lazarus RS. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J Pers Soc Psychol. 1985; 48(1): 150.
- 3. Moser AE, Annis HM. The role of coping in relapse crisis outcome: a prospective study of treated alcoholics. Addiction, 1996; 91(8): 1101–1114.
- 4. Miller PM, Book SW, Stewart SH. Medical treatment of alcohol dependence: a systematic review. Int J Psychiatry Med, 2011; 42(3): 227–266.
- 5. Monti PM, Rohsenow DJ. Coping-skills training and cue-exposure therapy in the treatment of alcoholism. Alcohol Res Health, 1999; 23(2): 107.
- 6. Becker HC. Alcohol dependence, withdrawal, and relapse. Alcohol Res Health, 2008; 31(4): 348–361
- 7. Sureshkumar K, Kailash S, Dalal PK, . Psychosocial factors associated with relapse in patients with alcohol dependence. Indian J Psychol Med, 2017; 39(3): 312–315.
- 8. Stockwell T, Murphy D, Hodgson R. The severity of alcohol dependence questionnaire: its use, reliability and validity. Br J Addict, 1983; 78(2): 145–155.
- 9. Carver CS. You want to measure coping but your protocol’too long: consider the brief cope. Int J Behav Med, 1997; 4(1): 92–100.
- 10. Shiffman S. Coping with temptations to smoke. J Consult Clin Psychol, 1984; 52(2): 261.
- 11. Litt MD, Kadden RM, Cooney NL, . Coping skills and treatment outcomes in cognitive-behavioral and interactional group therapy for alcoholism. J Consult Clin Psychol, 2003; 71: 118–128.
- 12. Sarkar AP, Sen S, Mondal S, . A study on socio-demographic characteristics of alcoholics attending the de-addiction center at Burdwan medical college and hospital in West Bengal. Indian J Public Health, 2013; 57(1): 33–35.
- 13. Neufeld KJ, Peters DH, Rani M, . Regular use of alcohol and tobacco in India and its association with age, gender, and poverty. Drug Alcohol Depend, 2005; 77(3): 283–291.
- 14. Johnson PR, Banu S, Ashok MV. Severity of alcoholism in Indian males: correlation with age of onset and family history of alcoholism. Indian J Psychiatry, 2010; 52(3): 243.
- 15. Chatterjee K, Dwivedi AK, Singh R. Age at first drink and severity of alcohol dependence. Med J Armed Forces India, 2021; 77(1): 70–74.
- 16. Miller WR, Walters ST, Bennett ME. How effective is alcoholism treatment in the United States? J Stud Alcohol, 2001; 62(2): 211–220.
- 17. Monahan SC, Finney JW. Explaining abstinence rates following treatment for alcohol abuse: a quantitative synthesis of patient, research design and treatment effects. Addiction, 1996; 91(6): 787–805.
- 18. Moos RH, Moos BS. Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction, 2006; 101(2): 212–222.
- 19. Veilleux JC, Colvin PJ, Anderson J, . A review of opioid dependence treatment: pharmacological and psychosocial interventions to treat opioid addiction. Clin Psychol Rev, 2010; 30(2): 155–166.
- 20. Kadam M, Sinha A, Nimkar S, . A comparative study of factors associated with relapse in alcohol dependence and opioid dependence. Indian J Psychol Med, 2017; 39(5): 627–633.
- 21. Rampure R, Inbaraj LR, Elizabeth CG, . Factors contributing to alcohol relapse in a rural population: lessons from a camp-based de-addiction model from rural Karnataka. Indian J Community Med, 2019; 44(4): 307.
- 22. Pilowsky DJ, Keyes KM, Geier TJ, . Stressful life events and relapse among formerly alcohol dependent adults. Socwork Ment Health, 2013; 11(2): 184–197.
- 23. Reyes CD, Pagano ME, Ronis RJ. The impact of stressful life events on alcohol use relapse: findings from the collaborative longitudinal personality disorders study. J Dual Diagn, 2009; 5(2): 226–232.
- 24. Shanmugam B, Das B, Bhattacharjee D, . Expressed emotions and coping among relapsed persons with alcohol dependence syndrome: a comparative study. Indian J Mental Health, 2021; 8(4): 429.
- 25. Chauhan VS, Nautiyal S, Garg R, . To identify predictors of relapse in cases of alcohol dependence syndrome in relation to life events. Ind Psychiatry J, 2018; 27(1): 73.
- 26. McKay JR. Negative mood, craving, and alcohol relapse: can treatment interrupt the process? Curr Psychiatry Rep, 2011; 13: 431–433.
- 27. Cooney NL, Litt MD, Morse PA, . Alcohol cue reactivity, negative-mood reactivity, and relapse in treated alcoholic men. J Abnorm Psychol, 1997; 106(2): 243.
- 28. Vieten C, Astin JA, Buscemi R, . Development of an acceptance-based coping intervention for alcohol dependence relapse prevention. Subst Abus, 2010; 31(2): 108–116.
- 29. Nadkarni A, Dabholkar H, McCambridge J, . The explanatory models and coping strategies for alcohol use disorders: an exploratory qualitative study from India. Asian J Psychiatr, 2013; 6(6): 521–527.
- 30. Ghandour LA, Karam EG, Maalouf WE. Lifetime alcohol use, abuse and dependence among university students in Lebanon: exploring the role of religiosity in different religious faiths. Addiction, 2009; 104(6): 940–948.
- 31. Mckee SA, Hinson RE, Wall A, . Alcohol outcome expectancies and coping styles as predictors of alcohol use in young adults. Addict Behav, 1998; 23: 17–22.
- 32. Davila R, Sanchez-Craig M, Wilkinson DA. Effects of using recommended coping strategies on drinking outcome following a brief intervention. Addiction, 2000; 95: 115–122.
- 33. Williams A, Clark D. Alcohol consumption in university students: the role of reasons for drinking, coping strategies, expectancies, and personality traits. Addict Behav, 1998; 23: 371–378.
- 34. Allsop S, Saunders B, Phillips M. The process of relapse in severely dependent male problem drinkers. Addiction, 2000; 95: 95–106.
- 35. Greenfield SF, Hufford MR, Vagge LM, . The relationship of self-efficacy expectancies to relapse among alcohol dependent men and women: a prospective study. J Stud Alcohol, 2000; 61: 345–351.
- 36. Demirbas H, Ilhan IO, Dogan YB. Ways of problem solving as predictors of relapse in alcohol dependent male inpatients. Addict Behav, 2012; 37(1): 131–134.