Introduction
Class II malocclusion is a major reason for patients to seek orthodontic treatment. Combinations of dental and skeletal factors ranging from mild to severe are among the multiple characteristics of this discrepancy. The treatment protocols for class II malocclusion can vary widely depending on the time of treatment, the severity of the malocclusion, and patient compliance.
One of the recommended therapeutic approaches to class II malocclusion in growing patients is functional jaw orthopedics for mandibular advancement. Fixed devices for mandibular advancement can also be used along with fixed mechanotherapy. The effects of several compliance-free fixed functional appliances for mandibular advancement have been studied.- One of the popular fixed functional appliances is the Forsus Fatigue Resistant Device (FFRD).,
FFRD is a semirigid telescoping system incorporating a superelastic nickel–titanium (NiTi) coil spring that can be incorporated into the preexisting fixed orthodontic appliances. The Forsus device is attached to the maxillary molar headgear tube and mandibular archwire, creating a mesial force on the mandibular arch and a distal force on the maxillary arch.
A headgear is used in class II malocclusion patients to restrict the growth of the maxilla. Teuscher suggested that forward and downward growth of the maxilla could be altered using a headgear, and the mandible could also change its growth direction to a forward and upward position with condylar adaptation.
A combination of an FFRD and a headgear can bring about dramatic changes in the correction of severe class II malocclusions. This case report describes the management of skeletal class II malocclusion in a growing patient with the desired results.
Pretreatment Assessment
History and Clinical Examination
SP, a 13-year-old female patient, reported to the orthodontic clinic with the chief complaint of forwardly placed upper front teeth. There was no relevant medical history.
Extraoral examination revealed that she had a convex profile, incompetent lips, a lip trap, a deep mentolabial sulcus, an everted lower lip, posterior divergence, and a clinically positive visual treatment objective (VTO) (Figure 1).
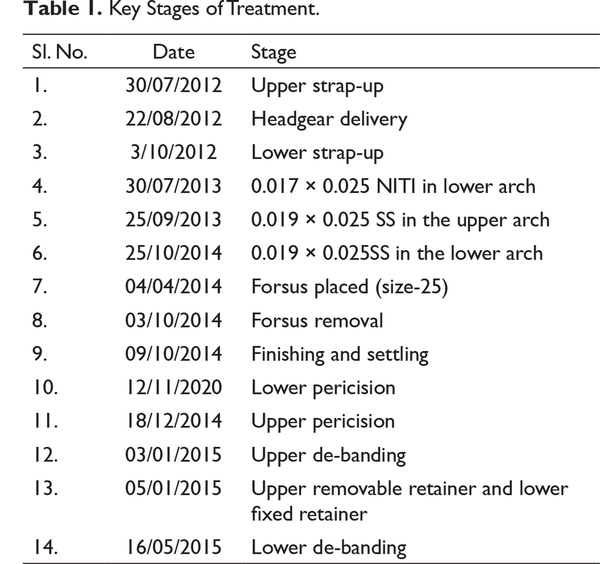
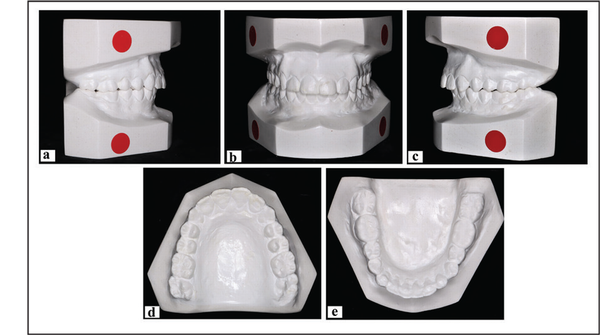
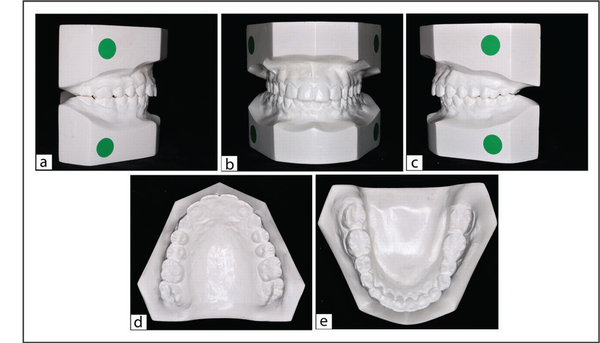
Intraoral examination revealed that the patient had permanent dentition in three quadrants, and in the upper right quadrant the patient had 54 and 55 and unerupted 14 and 15. She presented with a normal gingiva and frenal attachment with narrow upper and lower arches with moderate crowding. Patient had restorations wrt teeth 16, 17, 36, and 46. Second molars were unerupted in the oral cavity.
The left buccal segment showed class I molar and half unit class II canine relation and the right buccal segment showed class II molar and class II canine relation (Figures 2 and 3). The patient exhibited a deep bite and an exaggerated Curve of Spee. The incisor relationship was class II division 1, with an overjet of 12 mm and overbite of 6 mm. Midlines were not coinciding with the facial midlines, with the upper midline shifted towards the left side by 4 mm and the lower midline shifted to the right by 2 mm.

Pretreatment Extraoral Photographs. (a) Frontal, (b) frontal smiling, (c) oblique, (d) oblique smiling, (e) profile, and (f) VTO.

Pretreatment Intraoral Photographs. (a) Right buccal, (b) frontal, (c) left buccal, (d) upper occlusal, and (e) lower occlusal.
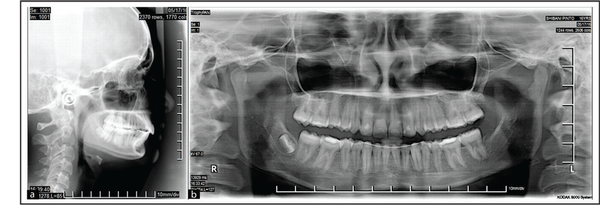
General Radiographic Examination
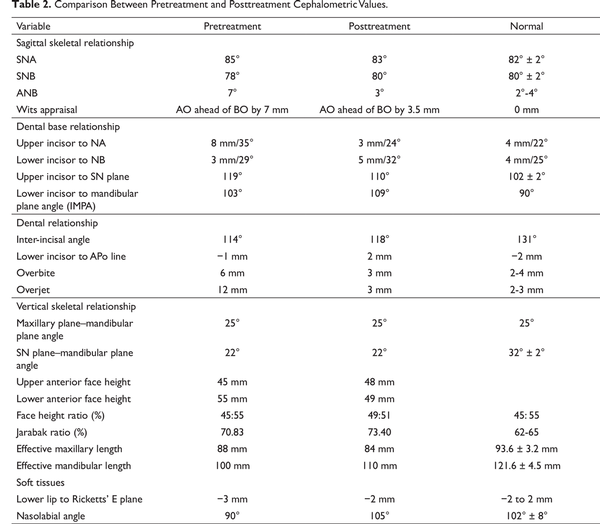
The pretreatment radiographs taken were a lateral cephalogram and an orthopantomogram (OPG) (Figure 4). The OPG showed the absence of third-molar tooth buds. The cervical vertebrae maturation index (CVMI) showed that the patient was in stage 3 (transition, 25% to 65% growth remaining).
Pretreatment cephalometric analysis showed a skeletal class II relation, with a forwardly placed maxilla and backwardly placed mandible, shorter mandibular length in relation to the maxillary length, proclined upper and lower anteriors, and a horizontal growth pattern (Table 2).
Pretreatment Study Model. (a) Right buccal, (b) frontal, (c) left buccal, (d) upper occlusal, and (e) lower occlusal.
Pretreatment Radiographs. (a) Lateral cephalogram and (b) orthopantomogram.
Model Analysis
Permanent dentition analysis was carried out even though there were decidous 54 and 55 (the references for mesiodistal [MD] width of unerupted premolars were taken considering the MD of the contralateral premolar teeth). Ashley Howe’s analysis indicated that it was a borderline case, and expansion was indicated in both arches. Bolton’s analysis showed an overall mandibular tooth material excess of 0.74 mm and anterior mandibular tooth material excess of 2.55 mm.
The “Index of Orthodontic Treatment Need” (IOTN) was 5.a (overjet greater than 9 mm), indicated a great need of treatment (5a).
Diagnostic Summary
Angle’s class II division 1 subdivision with a class II skeletal relationship due to a prognathic maxilla and a retrognathic mandible, a horizontal growth pattern, bidental proclination, an exaggerated Curve of Spee, a large overjet, an increased overbite, and a normal nasolabial angle.
Problem List
Skeletal class II relation with a prognathic maxilla and retrognathic mandible;
Decreased mandibular length (deficient by 11 mm);
V-shaped upper and lower arches;
Increased overjet (12 mm) and overbite (6 mm);
Non-coinciding midline;
Half unit class II molar relation on the right side and class I on the left side;
Class II canine relation on the right side and half unit class II the left side;
Exaggerated Curve of Spee (7 mm);
Moderate crowding in the upper and lower arches;
Proclined upper anteriors;
Deep mentolabial sulcus;
Incompetent lips; and
Lip trap.
Aims and Objectives of Treatment
Correction of skeletal pattern;
Restriction of maxillary growth and promotion of mandibular growth;
Correction of molar relation on the right side and canine relation on both sides;
Establishment of an ideal overjet and overbite;
Correction of the Curve of Spee;
Correction of midline discrepancy; and
Correction of crowding.
Treatment Plan
The treatment plan suggested was a two-phase therapy using a twin block with a headgear. Neither parents nor the patient were ready for a removable appliance.
The treatment plan included a headgear with fixed mechanotherapy and fixed functional appliance (Forsus). The headgear was to restrict the growth and also to distalize the maxilla. The Forsus would advance the mandible for sagittal correction. The treatment sequence would be: extraction of the 54 and 55, fixed mechanotherapy with the headgear, leveling and alignment of both the arches, reevaluation of the case for therapeutic extraction, or class II correction for mandibular advancement.
Proposed Retention Strategy
A lower fixed retainer would be retained in the mouth until the cessation of growth. An upper Begg’s wraparound retainer with an anterior bite plane would be worn at least for 2 years posttreatment. The patient would be instructed to reduce the duration of the upper retainer gradually.
Treatment Progress
The patient was treated with a preadjusted edgewise appliance, MBT prescription (Gemini, 3M Unitek) with slot dimensions 0.022″ × 0.028″. Initial leveling and aligning was done on the upper arch using a 2×4 appliance (Figures 5a-c; Table 1). Headgear therapy was started along with fixed mechanotherapy (Figure 6).
The lower arch was bonded 3 months after the upper strap-up (Figures 5d-f). The 0.016″ round Nickel Titanium (NiTi) were then followed by 0.017″ × 0.025″ NiTi wires and 0.019″ × 0.025″ rectangular NiTi wires. Then, 0.019″ × 0.025″ rectangular stainless steel (SS) wires were placed in the upper and lower arches. The Forsus was placed once the SS wires were placed in both the arches (Figures 5g-i). The patient was recalled at monthly intervals for monitoring the progress. Reactivation of the Forsus was done placing a split crimp on the push rod. The Forsus was removed when a class I molar and canine relation was achieved.
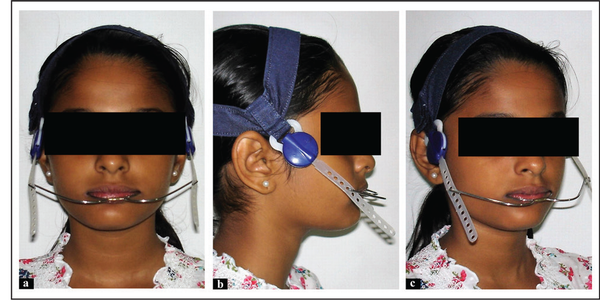
Headgear with fixed appliance. (a) Frontal, (b) profile, (c) oblique.
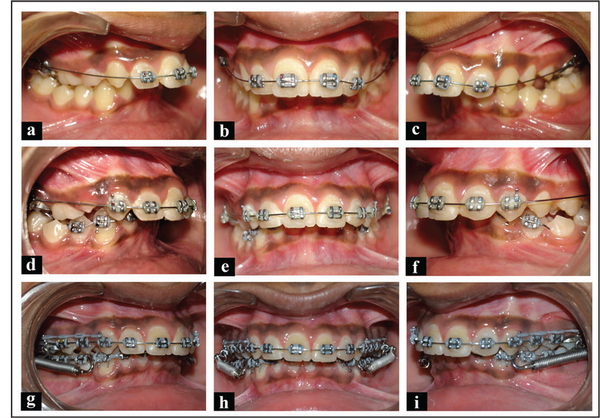
Mid-treatment Photographs. Upper strap-up using a 2×4 appliance (a to c), lower strap-up (d to f), forsus placement after levelling the lower arch (g to i).
Posttreatment Assessment
Posttreatment Results
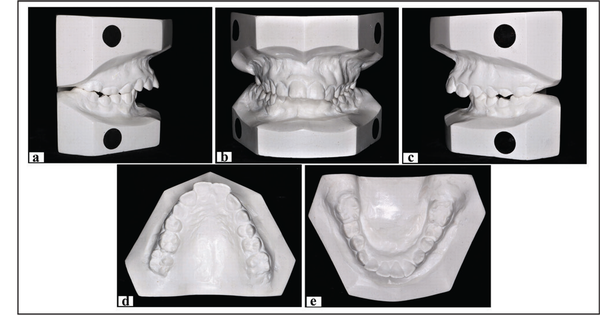
The profile was changed from convex to straight (Figure 7). The nasolabial angle improved. The lips were competent. The molar and canine relationships were corrected. The overjet and overbite was greatly improved (Figures 8 and 9). The midlines were coinciding. Good intercuspations were achieved. A fixed retainer was bonded in the lower arch, and a removable retainer with an anterior bite plane was placed in the upper arch (Figure 8). The weighted peer assessment rating (PAR) score revealed that the treatment results were greatly improved (the score changed from 43 to 2).
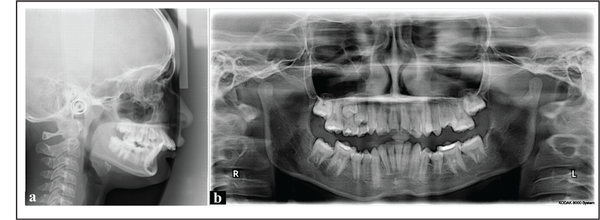
The OPG showed good root parallelism (Figure 10). Superimposition showed that the maxillary growth had been redirected clockwise and the mandible moved forward (Figure 11). Occlusion remained stable 3 years after the orthodontic treatment (Figures 12-14).
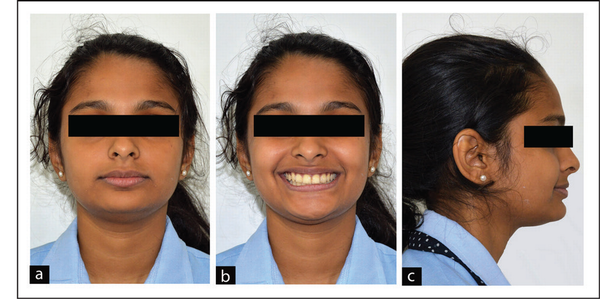
Posttreatment Extraoral Photographs. (a) Frontal, (b) frontal smiling, and (c) profile.
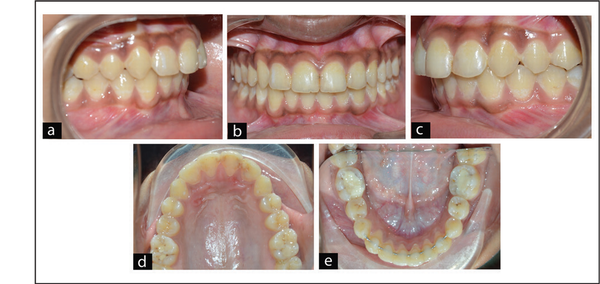
Posttreatment Intraoral Photographs. (a) Right buccal (b) frontal, (c) left buccal, (d) upper occlusal, and (e) lower occlusal.
Posttreatment Study Model. (a) Right buccal, (b) frontal, (c) left buccal, (d) upper occlusal, and (e) lower occlusal.
Posttreatment Radiographs. (a) Lateral cephalogram and (b) orthopantomogram.
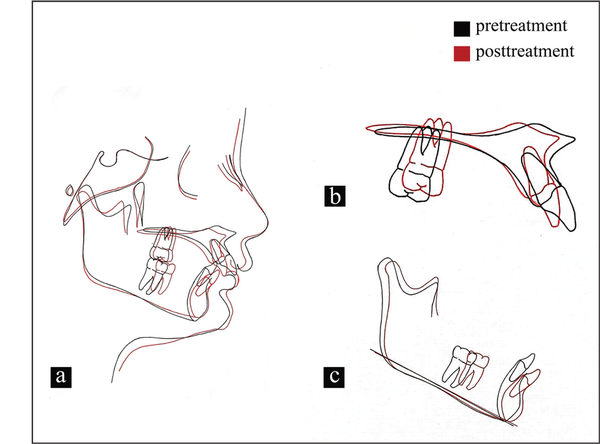
Pretreatment and Posttreatment Tracing Superimposition, (a) Overall, (b) maxilla, and (c) mandible.
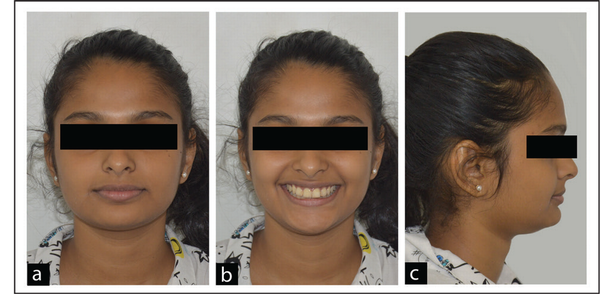
Post-retention Extraoral Photographs. (a) Frontal, (b) frontal smiling, and (c) profile.

Post-retention Intraoral Photographs. (a) Right buccal, (b) frontal, (c) left buccal, (d) upper occlusal, and (e) lower occlusal.
Posttreatment Study Model. (a) Right buccal, (b) frontal, (c) left buccal, (d) upper occlusal, and (e) lower occlusal.
Posttreatment Cephalometric Assessment (Table 2)
There is an improvement in the skeletal relation.
Upper anterior proclination is reduced.
There is a reduction in the overjet and overbite.
The nasolabial angle is improved.
Soft-tissue balance is achieved.
Complications Encountered During the Treatment
Though there were no severe complications during therapy, a mild degree of orthodontic scars (white spot lesions) were seen around the teeth. Repeated oral hygiene instructions were given to the patient, as well as her parents, during therapy, to avoid white spot lesions. Throughout the treatment, usage of a fluoridated mouth rinse and tooth paste was advised, and the patient was instructed to continue them after the de-banding.
Critical Appraisal
SP, 13-year-old female patient, was treated according to the aim and objectives stated. The posttreatment results show that most of the objectives stated were achieved. The overjet was greatly improved. The overbite was reduced. The midlines were corrected. Root parallelism was achieved in all teeth except for 31. The skeletal relationships were improved considerably. The Curve of Spee was corrected. The lower anteriors were slightly proclined. Root parallelism was achieved. The mandibular length was increased. Lips were competent. Chin prominence was improved. Good soft-tissue balance was achieved. There was a slight increase in the overjet and overbite during the third year of the follow-up. The patient was advised to wear an upper Begg’s wraparound appliance with an anterior bite plane and to be seen every month for a slight amount of interproximal reduction (IPR) and overbite correction. However, posterior occlusion remained stable 3 years after the treatment.
Conclusions
This case report demonstrates the efficiency of the combined clinical use of a headgear and a fixed Forsus appliance in distalizing the maxillary molar and advancing the mandible.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Shahistha Parveen
https://orcid.org/0000-0002-5984-6719
Rohan Mascarenhas
https://orcid.org/0000-0002-8803-7224
- 1. Pancherz H. The Herbst appliance: Its biologic effects and clinical use. Am J Orthod. 1985; 87:1–20.
- 2. O’Brien K, Wright J, Conboy F Effectiveness of early orthodontic treatment with the twin-block appliance: a multicenter, randomized, controlled trial. Part 1: dental and skeletal effects. Am J Orthod Dentofacial Orthop. 2003;124 (3):234–243.
- 3. Pangrazio-Kulbersh V, Berger JL, Chermak DS, Kaczynski R, Simon ES, Haerian A. Treatment effects of the mandibular anterior repositioning appliance on patients with Class II malocclusion. Am J Orthod Dentofacial Orthop. 2003; 123:286–295.
- 4. Karacay S, Akin E, Olmez H, Gurton AU, Sagdic D. Forsus nitinol flat spring and jasper jumper corrections of Class II division 1malocclusions. Angle Orthod. 2006;76(4):666–672.
- 5. Sood S. The Forsus fatigue resistant device as a fixed functional appliance. J Clin Orthod. 2011;45(8):463–466.
- 6. Vogt W. The Forsus fatigue resistant device. J Clin Orthod. 2006;40(6):368–377.
- 7. Forsus. Forsus™ fatigue resistant device. https://multimedia.3m.com/mws/media/823065O/forsus-fatigue-resistant-device-treatment-guide.pdf. Accessed November 2, 2020.
- 8. Teuscher U. A growth-related concept for skeletal Class II treatment. Am J Orthod. 1978;74(3):258–275.