Introduction
Class III skeletal problems are caused by a maxillary deficiency, a mandibular excess, or a combination of the two. Although maximum skeletal class III patients are present with elements of deformities in both the jaws, a study reported that maxillary deficiency is the primary problem in 40% of the cases, mandibular excess in 42%, and both jaws in 18% of the cases.
Although class III skeletal problems are fewer in comparison to class II problems, it is widely acknowledged that a significant proportion of class III patients are affected esthetically and psychologically by their condition. What compounds the fact is that class III problems are often not as amenable to growth modulation or camouflage treatment mechanics as compared to the class II counterparts that respond more readily and effectively to these measures. Existing data indicate that the worst one-third of class III patients require orthognathic surgery compared to just 5% of class II patients.
Class III skeletal patients often exhibit dental compensations in the form of proclined maxillary incisors and retroclined mandibular incisors. The goal of presurgical orthodontics remains to decompensate the dentition and place the incisors in alignment with their respective skeletal bases. Extractions in the maxillary arch are often required to relieve crowding and to correct the inclination of incisors. Extractions, however, are rarely carried out in the mandibular arch.
Although in the 1960s maximum skeletal class III problems were addressed with mandibular setbacks, there were certain drawbacks including, but not limited to, reduced stability, increased relapse, and airway compromise. As we enter the new century, almost 90% patients are addressed by maxillary surgery, about half performed alone, and the other half in conjunction with mandibular setback as a bijaw procedure.
Another useful adjunct in planning of orthosurgical cases is the advent of cone-beam computed tomography (CBCT) which provides useful information for diagnosis, treatment planning, and assessment of treatment outcomes for orthognathic surgery cases. Presurgical assessment of CBCT provides vital information about dental and skeletal structures that aid in orthodontic as well as surgical treatment planning.
This case report demonstrates the ideal orthosurgical management of a severe skeletal class III malocclusion with extreme dental compensations highlighting the pivotal and adjunctive role of CBCT in such cases.
Materials and Methods
An 18-year-old girl reported to our dental center the chief complaint of unaesthetic appearance with her upper front teeth positioned behind her lower teeth and thus difficulty in speech and mastication. Her past medical history and dental history were noncontributory. She presented with no familial history of class III malocclusion or any other genetic disorder.
Extra oral frontal examination revealed no gross facial asymmetry in vertical thirds and horizontal fifths of the face. Profile examination revealed a concave profile with midfacial deficiency, acute nasolabial angle, and a shallow mentolabial sulcus. Smile analysis revealed reduced maxillary incisal display at rest and on smiling (Figure 1).
Intraoral examination showed dental caries in relation to 36, 46, presence of class III molar, canine and incisal relationship bilaterally, severe crowding in the maxillary arch with buccally blocked out 13, bilateral posterior crossbite in relation to maxillary premolars, mandibular dental midline shift to left by 3 mm, mild crowding in mandibular arch, and reverse overjet of 5 mm (Figure 1). The panoramic radiograph showed no gross abnormality (Figure 2).
A thorough functional analysis of the patient revealed that the patient has difficulty in mastication, in particular with incising from the maxillary and mandibular anterior teeth. Analysis of speech revealed distortion in production of labiodental consonants “f” and “v”. A sample of the patient’s speech was recorded and archived in the pretreatment records.
Model analysis revealed tooth size arch length discrepancy of 8 mm in the maxillary arch and 3 mm in the mandibular arch with no bolt-on discrepancy.
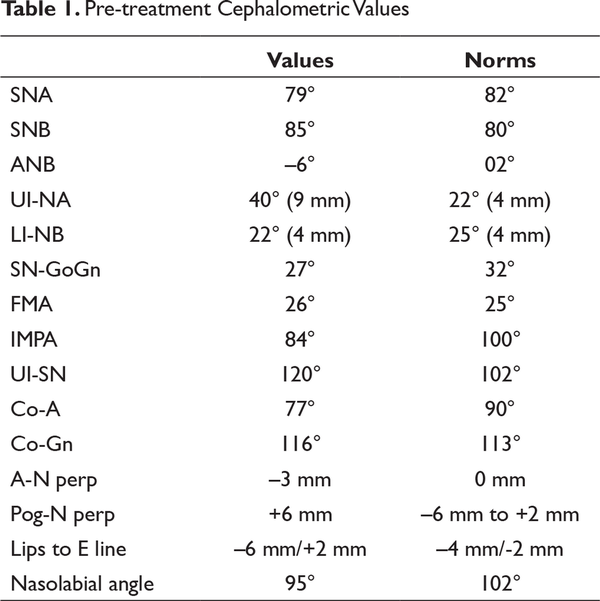
Pretreatment cephalometric analysis revealed that the patient had class III skeletal bases (SNA = 79°, SNB = 85°, ANB = –6°, maxillomandibular differential = 43 mm), retrognathic maxilla (SNA = 79°, Pt A to N perpendicular = –3 mm), prognathic mandible (SNB = 85°, Pog to N perpendicular = +6 mm), proclined upper incisors (UI to NA = 40°/9 mm, UI to SN = 120°), retroclined lower incisors (IMPA = 84°), and a reduced nasolabial angle (95°; Table 1, Figure 3).

Pre-treatment Extra Oral Frontal, Smile and Profile Photographs; Intra Oral Photographs
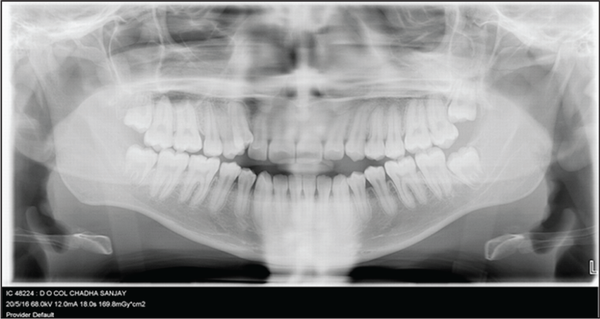
Pre-treatment Orthopantomogram
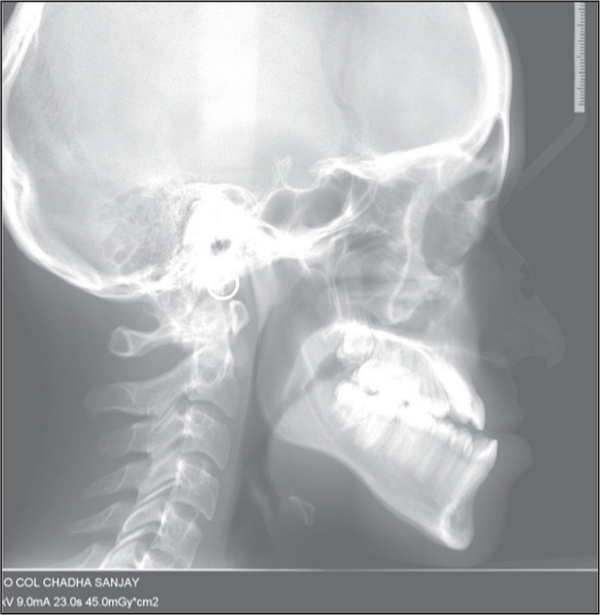
Pre-treatment Lateral Cephalogram
Treatment Objectives
The treatment objectives included improving speech and mastication, restoration of carious teeth, improvement of profile and smile esthetics, correction of midline discrepancy, leveling and alignment, optimizing overjet and overbite, achieving a stable functional occlusal relationship bilaterally, and correction of underlying skeletal discrepancy.
Treatment Plan
Based on the clinical, functional, and radiological findings, an orthosurgical treatment plan was formulated. Extraction of 14 was decided in the maxillary arch to alleviate the crowding and to decompensate the dentition. Archwire expansion and mandibular incisor proclination were deemed sufficient for the correction of crowding and to decompensate the dentition in the mandibular arch. A decision was made regarding the removal of third molars at the time of sagittal split osteotomy in line with recommendations proposed by Doucet.
High-level quadrangular Le Fort I osteotomy was planned for maxillary advancement and bilateral sagittal split osteotomy (BSSO) for mandibular setback to correct the skeletal discrepancy.
Treatment Progress
Presurgical orthodontics included banding and bonding with 0.022” Roth preadjusted edgewise appliance (PEA), extraction of 14 to alleviate maxillary crowding, leveling and alignment in both the arches and placement of a finishing archwire of 0.021” × 0.025” stainless steel to stabilize the arches.
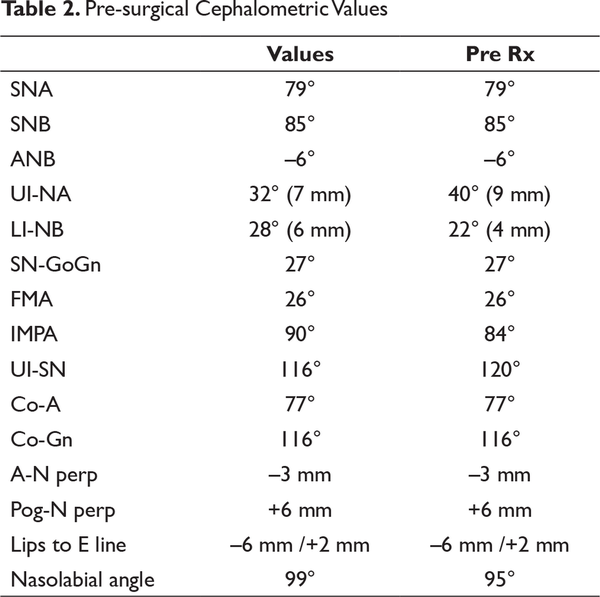
After 12 months of presurgical orthodontic treatment, the reverse overjet accentuated from 5 mm to 8 mm. Complete records including lateral cephalogram, intraoral, and extraoral photographs and study models were taken again (Figure 4). Presurgical cephalometric analysis revealed that decompensation of maxillary and mandibular incisors was achieved (Table 2). Cephalometric and prediction tracing was performed to analyze the outcome (Figure 5). Based on clinical and cephalometric prediction analysis as well as data gleamed from three-dimensional (3D) surgical simulation, a decision was made for 5 mm of maxillary advancement and 7 mm of mandibular setback. Facebow transfer was carried out (Figure 5) and this relationship was then transferred to a semiadjustable articulator (Stratos 2000, Ivoclar Vivadent, Schaan, Liechtenstein). Mock surgery was performed on the articulated models and two-stage surgical splints were fabricated (stage 1 splint in pink acrylic for maxillary advancement and stage 2 splint in clear acrylic for mandibular setback).

Pre-surgical Extra Oral Frontal, Smile and Profile Photographs; Intra Oral Photographs
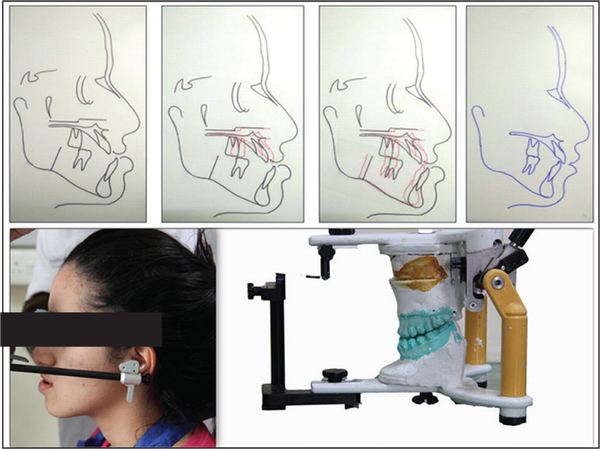
Pre-surgical Cephalometric Prediction with Maxillary Advancement of 5mm and Mandibular Setback of 7mm; Pre-surgical Face Bow Transfer, Semi-adjustable Articulator Mounting and Mock Surgery
Pre-surgical Assessment of IAN Course, Proximity and Position Using CBCT
3D Surgical Simulation with Facial Photographic Superimposition for Maxillary Advancement and Mandibular Setback
Presurgical CBCT Assessment
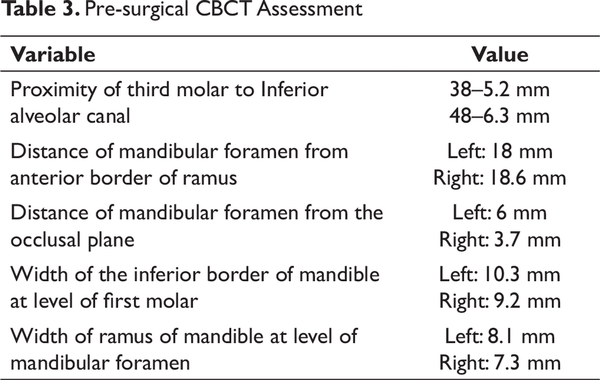
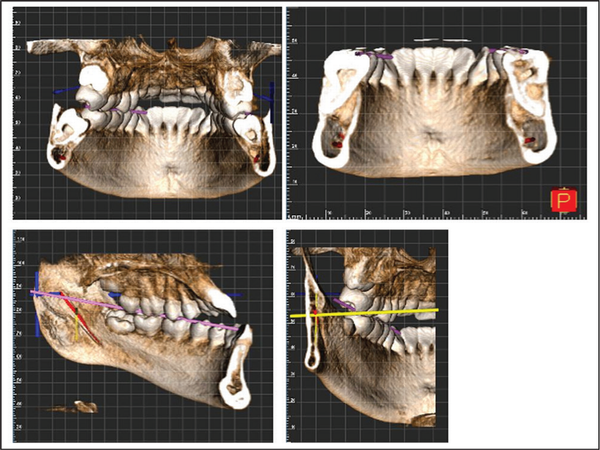
Prior to taking up the patient for surgery, an assessment of the pretreatment CBCT (NewTom Giano, Bologna, Italy) was carried out (FOV – 110 mm × 80 mm, Voxel size – 0.3 mm). The primary findings were in relation to the proximity of the mandibular third molar to the inferior alveolar nerve (IAN) canal as it was planned to remove them intraoperatively prior to BSSO. The distance of mandibular foramen from the anterior border of ramus and the occlusal table was calculated. The adequacy of the bone stock was also measured in form of the width of the inferior border of the mandible. The findings as assessed from the CBCT are reported in Table 3 and the same were communicated to the surgical team for preoperative planning (Figure 6).
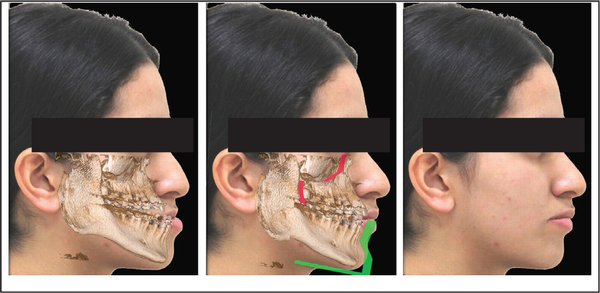
The assessment of the pre-surgical CBCT was carried out (FOV – 110 mm × 80 mm, Voxel size – 0.3 mm). 3D simulation (NNT Viewer (NewTom, Bologna, Italy), 3D Slicer (http://www.slicer.org), Adobe Photoshop CC (Adobe Inc, San Jose, California)) was done which provided information regarding the quantification of maxillary advancement and mandibular setback. Facial photographic superimposition allowed us to forecast the posttreatment results. The same was helpful in patient education and motivation (Figure 7).
The patient was taken up for surgery under general anesthesia and a high-level quadrangular Le Fort I osteotomy was done in maxilla. A maxillary advancement of 5 mm, as guided by the stage 1 splint, followed by rigid fixation using titanium plates and screws was carried out. Cinching of the Alar base was done to prevent nasal flaring due to maxillary advancement. After the maxillary fixation, bilateral intraoral vestibular incisions were given and osteotomy was carried out distal to mandibular second molars bilaterally. The mandible was then repositioned in relation to maxilla as guided by the stage 2 splint for a setback of 7 mm, and rigid fixation was carried out using titanium plates and screws (Figure 8).
Postsurgical healing was uneventful. The final splint was fixed intraorally for a period of 4 weeks to aid in neuromuscular adaptation along with guiding elastics. Postsurgical settling of occlusion was done and full interdigitation of buccal occlusion was achieved in four months. The complete orthosurgical procedure was completed in 16 months. A flexible spiral wire retainer was placed in maxillary and mandibular arches for retention and complete posttreatment records were taken.
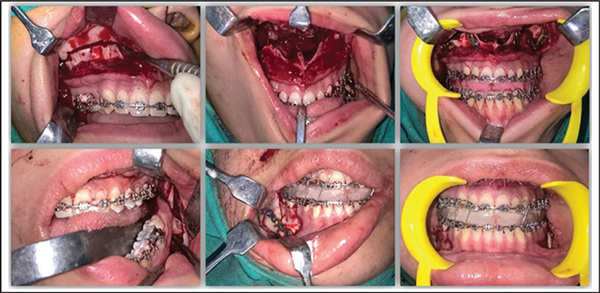
Intra Operative Photographs Illustrating Le-fort I Osteotomy for Maxillary Advancement Followed by Bilateral Sagittal Split Osteotomy for Mandibular Setback

Post-treatment Extra Oral Frontal, Smile and Profile Photographs; Intra Oral Photographs
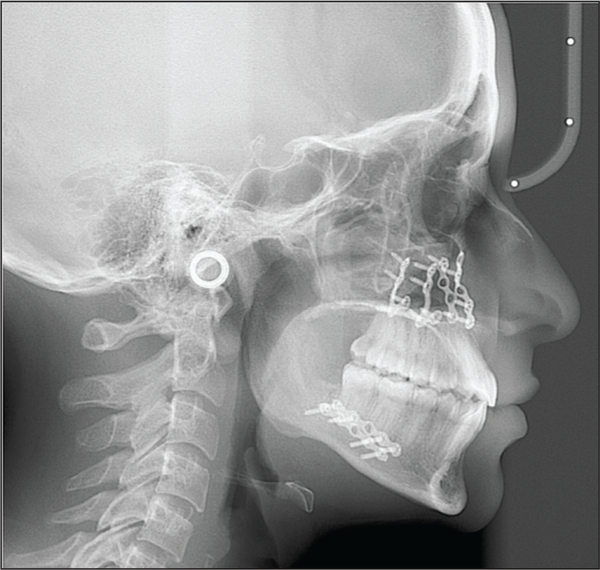
Post-treatment Lateral Cephalogram
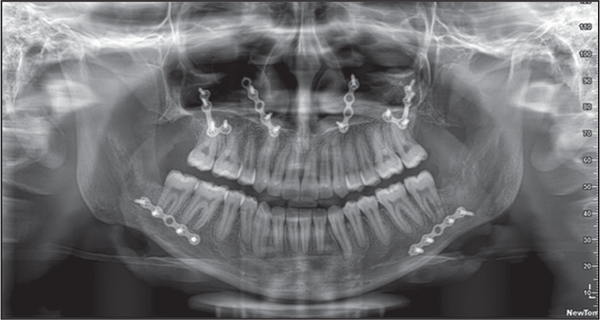
Post-treatment Orthopantomogram
Results
The posttreatment results show a significant and remarkable improvement in soft and hard tissue parameters. Extra oral frontal photographs reveal a marked improvement in facial and smile esthetics with an optimal smile arc and maxillary incisal display. Profile photograph reveals a substantial improvement in esthetics with optimization of nasolabial angle (Figure 9).
Posttreatment intraoral pictures reveal a well-settled functional occlusion with class I canine relationship bilaterally, coincident midlines, ideal overjet, and overbite (Figure 9).
Posttreatment functional analysis of speech and mastication revealed significant improvement in both parameters. Patient exhibited no difficulty in pronunciation of labiodental consonants. The speech was also compared with pretreatment archival voice recording to confirm the findings.
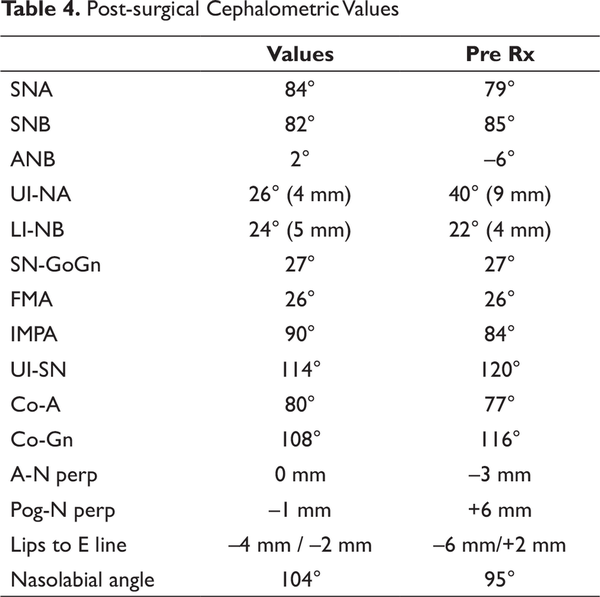
Posttreatment lateral cephalogram shows correction of skeletal bases (ANB = 2o, maxillomandibular differential = 34 mm), soft tissue analysis revealed that both upper and lower lips are on the esthetic E line with an ideal nasolabial angle (104o; Table 4, Figure 10).
The posttreatment panoramic radiograph showed that root parallelism had been achieved (Figure 11).
Posttreatment CBCT Assessment
A posttreatment CBCT was taken immediately after debonding to assess treatment results (FOV – 110 mm × 80 mm, Voxel size – 0.3 mm).
The presence or absence and the degree of apical root resorption in the CBCT images was evaluated using the scoring system of Levander and Malmgren that classifies it into 5 grades: 0, no root resorption; 1, mild resorption, with the root of normal length and only an irregular contour; 2, moderate resorption, with small areas of root loss and the apex having an almost straight contour; 3, severe resorption, with loss of almost one third of root length; and 4, extreme resorption, with loss of more than one-third of the root length. A total of 27 teeth were evaluated for the presence or absence of root resorption. 12 teeth showed no evidence of root resorption. 13 teeth showed mild resorption, while 2 teeth showed moderate resorption. This translated to a total prevalence of 55.6% (Figure 12).
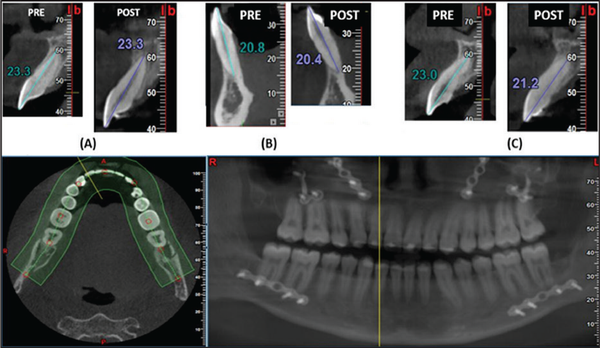
Use of CBCT to Assess Orthodontic Induced Apical Root Resorption. (A) Evaluation of 11 Showing No Root Resorption, (B) Evaluation of 41 Showing Mild Root Resorption, (C) Evaluation of 12 Showing Moderate Root Resorption; CBCT Panoramic Radiograph for Assessment of Post-treatment Root Angulation and Parallelism
The root angulations were assessed via CBCT-generated panoramic image using the multiplanar mode (Figure 12).
The absence of fenestrations and dehiscences indicated that the teeth are placed well within the alveolar housing with precise and judicious treatment biomechanics performed.
Discussion
By definition, class III skeletal problems are caused by maxillary deficiency, mandibular prognathism, or some combination of maxillary deficit and mandibular excess. It has also been recognized since long that a higher proportion of class III patients feel socially and psychologically handicapped with their condition as compared to class II patients. Functional deficits in speech and mastication show higher correlations with skeletal class III malocclusion. This also necessitates the fact that a significant majority of these cases require orthognathic surgery for optimal correction of dental and skeletal malocclusions.
It is believed that a reverse overjet of greater than 4 mm cannot be managed orthodontically alone. Our patient presented with a reverse overjet of 5 mm with severe dentoalveolar compensations. There was an element of maxillary hypoplasia as well as mandibular prognathism, thus necessitating orthosurgical line of management.
The goal of presurgical orthodontic treatment is to align the upper and lower teeth to their respective skeletal bases and remove all dentoalveolar compensations. This often necessitates premolar extractions in the maxillary arch to alleviate dental crowding, if any, and correct the maxillary incisor angulation. In the mandibular arch, it is often required to move the lower incisors facially, and thus extractions are rarely indicated in the mandibular arch. In our case, a single premolar extraction was done to fulfill the above-mentioned objectives as well as to plan for a postsurgical functional class II molar relationship unilaterally.
Another decision was made in our case to extract third molars during the time of surgery. Although traditionally third molars have been removed 9 to 12 months before orthosurgical treatment to avoid a “bad split” recent reports have stated that the removal of impacted third molar at least 6 months or 1 year before BSSO does not reduce the incidence of unwanted mandibular fractures., , In fact, it has been stated that the presence of third molars during sagittal split osteotomy minimizes postoperative neurosensory disturbance of the IAN.
SEDENTEXCT guidelines on the use of dental CBCT recognizes its invaluable role in orthosurgical planning. In our case the preoperative CBCT played a vital role in the assessment of third molars and location of IAN bundle. CBCT elucidated the 3D relationship of the third molar root to the mandibular canal; the coronal sections allowed a bucco-lingual appreciation of the mandibular canal. This is useful to identify cases in which a lingually placed IAN is at risk during surgery. This observation dictates the surgical approach of how to remove the third molar, so the IAN will not be subjected to pressure. In our case, CBCT assessment showed that the roots of the third molars were well clear of the IAN bundle, thus facilitating easy removal intraoperatively.
Previous studies have yielded a postoperative incidence of sensory deficits of the IAN immediately after surgery, ranging from 12.5% to 100%. It has been evaluated that a low corpus height and the location of the mandibular canal near the inferior border of the mandible may increase the risk of IAN injury. Another study has stated that lack of a bone marrow space on the buccal side, including a fusion-type anatomy with no buccal side cortical bone of the mandibular canal places the IAN at risk during BSSO and the osteotomy cut should be moved anteriorly in such cases. In our case, we were able to trace the course of the IAN from the mandibular foramen anteriorly, thus predicating risk of causeless manipulation intraoperatively.
CBCT was also used to assess the quantum of root resorption posttreatment. Histologic studies have reported greater than 90% occurrence of root resorption in orthodontically treated teeth., Lower percentages are reported when diagnostic radiographic techniques are used. Lupi et al reported that the incidence of external apical root resorption before treatment is 15% and after treatment, 73%. Radiographic techniques include mainly panoramic and periapical radiographs. Both techniques are two-dimensional (2D) representations of a 3D structure and are susceptible to dimensional inaccuracy, projection errors, and distortions. CBCT is a powerful tool to detect apical root resorption and overcomes the inherent limitations of the traditional radiographic aids., In our case, there was a low posttreatment prevalence of root resorption of 55.6% indicating both toward judicious treatment mechanics and a shortened duration of treatment.
Proper angulation of teeth is one of the objectives of orthodontic treatment. It is one of the 6 keys illustrated by Andrews. Ideal occlusion and proper articulation are difficult to obtain without adequate axial inclination of all teeth. Moreover, the proper angulation of roots of the maxillary and mandibular dentition is a prerequisite for the American Board of Orthodontics examination. Orthopantomograms (OPG) have been used traditionally to evaluate root angulations and positions before, during, and after orthodontic treatment. OPGs, being 2D representations of 3D structures, are dimensionally inaccurate and the same has been demonstrated through research., CBCT is a more powerful tool for the visualization and assessment of root angulation and the CBCT pan-like image is more accurate than a conventional pan radiograph.- The same was carried out in our case to reveal near-optimal root angulation and parallelism.
A new dimension to the use of CBCT in orthosurgical cases which is gaining traction in recent times is the incorporation of 3D surgical simulation. Soft tissue as well as skeletal surgical simulation improves the accuracy and reliability of the surgical procedure itself and also has a marked effect on patient motivation. In our case, an intuitive and cost-effective combination of NNT viewer, 3D Slicer, and Adobe Photoshop CC were used for 3D reconstruction, 3D slicing and quantification, and facial superimposition, respectively.
In the orthosurgical management of class III patients with significant skeletal dysplasia, more than 90% of the cases have maxillary surgery, out of which about half are performed as a single jaw procedure whereas 2 jaw procedures constitute the other half. Maxillary surgery is both more esthetic and more stable than isolated mandibular setback and 2 jaw procedures offer further advantages in esthetics compared with maxillary surgery alone. Moreover, isolated mandibular setback can reduce oral volume and cause reduction in the pharyngeal airway. It is also known that when performed alone, Le Fort maxillary advancement greater than 6 mm and bilateral sagittal split osteotomy mandibular setback greater than 10 mm are often associated with significant relapse., In view of all the above-mentioned factors the decision for 2 jaw procedures was taken in our case for optimal esthetic, functional, and stable results.
Conclusion
The present case report shows the successful management of severe skeletal class III dentofacial deformity with combined orthodontics and bijaw orthognathic surgery. There was a marked improvement in the facial esthetics and ideal functional occlusion was achieved. A multidisciplinary team approach is required in diagnosis and management of these cases. Adjunctive diagnostic aid in the form of CBCT was judiciously utilized to aid in treatment planning, improve the prognosis, and audit the results. It is recommended that meticulous evaluation of craniofacial complex with CBCT be done, to aid in diagnosis and treatment planning, to provide vital adjunctive information, to oral and maxillofacial surgeon in order to avoid intraoperative and postoperative complications and hence to achieve ideal desired treatment results.
Gaurav Pratap Singh
https://orcid.org/0000-0001-5748-6644
References
- 1. Proffit WR, Phillips C, Dann CT. Who seeks surgical-orthodontic treatment? Int J Adult Orthodon Orthognath Surg. 1990;5(3):153–160.
- 2. Proffit WR, Fields JH, Moray LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: Estimates from the NHANES III survey. Int J Adult Orthodon Orthognath Surg. 1998;13(2):97–106.
- 3. Proffit WR, White RP, Sarver DM. Contemporary Treatment of Dentofacial Deformity. St Louis, Missouri: C.V. Mosby; 2003.
- 4. Kapila SD, Nervina JM. CBCT in orthodontics: Assessment of treatment outcomes and indications for its use. Dentomaxillofac radiol. 2015;44(1):20140282.
- 5. Doucet JC, Morrison AD, Davis BR Concomitant removal of mandibular third molars during sagittal split osteotomy minimizes neurosensory dysfunction. J Oral Maxillofac Surg. 2012; 70:2153–2163.
- 6. Levander E, Malmgren O. Evaluation of the risk of root resorption during orthodontic treatment. A study of upper incisors. Eur J Orthod. 1988; 10:30–38.
- 7. Squire D, Best AM, Lindauer SJ, Laskin DM. Determining the limits of orthodontic treatment of overbite, overjet, and transverse discrepancy: a pilot study. Am J Orthod Dentofac Orthop. 2006;129(6):804–808.
- 8. Kessel SP. The rationale of maxillary premolar extraction only in Class II therapy. Am J Orthod. 1963; 49:276–293.
- 9. Fonseca RJ. Fonseca Oral and Maxillofacial Surgery. Vol 2. Philadelphia, PA: Sunders; 2000.
- 10. Precious DS, Lung KE, Pynn BR Presence of impacted teeth as a determining factor of unfavorable splits in 1256 sagittal-split osteotomies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998; 85:362–365.
- 11. Mehra P, Castro V, Frietas RZ Complications of the mandibular sagittal split ramus osteotomy associated with the presence or absence of third molars. J Oral Maxillofac Surg. 2001; 59:854–858.
- 12. Horner K, Islam M, Flygare L, Tsiklakis K, Whaites E. Basic principles for use of dental cone beam computed tomography: consensus guidelines of the European Academy of Dental and Maxillofacial Radiology. Dentomaxillofac Radiol. 2009;38(4):187–195.
- 13. Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, Bergé SJ. Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int J Oral Maxillofac Surg. 2009;38(9):964–971.
- 14. Ylikontiola L, Kinnunen J, Oikarinen K. Factors affecting neurosensory disturbance after mandibular bilateral sagittal split osteotomy. J Oral Maxillofac Surg. 2000;58(11):1234–1239.
- 15. Teerijoki-Oksa T, Jääskeläinen SK, Forssell K, Forssell H, Vähätalo K, Tammisalo T, Virtanen A. Risk factors of nerve injury during mandibular sagittal split osteotomy. Int J Oral Maxillofac Surg. 2002;31(1):33–39.
- 16. Tsuji Y, Muto T, Kawakami J, Takeda S. Computed tomographic analysis of the position and course of the mandibular canal: relevance to the sagittal split ramus osteotomy. Int J Oral Maxillofac Surg. 2005;34(3):243–246.
- 17. McLaughlin KD. Quantitative determination of root resorption during orthodontic treatment. Am J Orthod Dentofac Orthop. 1964;50(2):143.
- 18. Stevnik A, Mjor IA. Pulp and dentine reactions to experimental tooth intrusion. A histological study of the initial changes. Am J Orthod. 1970;57: 370–385.
- 19. Lupi JE, Handelman CS, Sadowsky C. Prevalence and severity of apical root resorption and alveolar bone loss in orthodontically treated adults. Am J Orthod Dentofacial Orthop. 1996;109(1):28–37.
- 20. Dudic A, Giannopoulou C, Leuzinger M, Kiliaridis S. Detection of apical root resorption after orthodontic treatment by using panoramic radiography and cone-beam computed tomography of super-high resolution. Am J Orthod Dentofacial Orthop. 2009;135(4):434–437.
- 21. Lund H, Gröndahl K, Hansen K, Gröndahl HG. Apical root resorption during orthodontic treatment: a prospective study using cone beam CT. Angle Orthod. 2011;82(3):480–487.
- 22. Andrews LF. The six keys to normal occlusion. Am J Orthod. 1972; 62:296–309.
- 23. American Board of Orthodontics. Information for candidates. St. Louis, MO: American Board of Orthodontics; 2001: 13.
- 24. Mckee IW, Glover KE, Williamson PC, Lam EW, Heo G, Major PW. The effect of vertical and horizontal head positioning in panoramic radiography on mesiodistal tooth angulations. Angle Orthod. 2001; 71:442–451.
- 25. Mckee IW, Williamson PC, Lam EW, Heo G, Glover KE, Major PW. The accuracy of 4 panoramic units in the projection of mesiodistal tooth angulations. Am J Orthod Dentofacial Orthop. 2002; 121:166–167.
- 26. Peck JL, Sameshima GT, Miller A, Worth P, Hatcher DC. Mesiodistal root angulation using panoramic and cone beam CT. Angle Orthod. 2007;77(2):206–213.
- 27. Van Elslande D, Heo G, Flores-Mir C, Carey J, Major PW. Accuracy of mesiodistal root angulation projected by cone-beam computed tomographic panoramic-like images. Am J Orthod Dentofacial Orthop. 2010;137(4):S94–S99.
- 28. Bouwens DG, Cevidanes L, Ludlow JB, Phillips C. Comparison of mesiodistal root angulation with posttreatment panoramic radiographs and cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2011;139(1):126–132.
- 29. Swennen G. 3D virtual treatment planning of orthognathic surgery. Berlin, Heidelberg: Springer; 2017.
- 30. Bailey LT, Cevidanes LH, Proffit WR. Stability and predictability of orthognathic surgery. Am J Orthod Dentofac Orthop. 2004;126(3):273–277.
- 31. Mobarak KA, Krogstad O, Espeland L, Lyberg T. Long-term stability of mandibular setback surgery: a follow-up of 80 bilateral sagittal split osteotomy patients. Int J Adult Orthodon Orthognath Surg. 2000;15(2):83–95.