Introduction
The coronavirus disease 2019 (COVID-19) infection was first identified and reported in the year 2019 in a cluster of cases, caused by a newly identified Betacoronavirus. Reported at Wuhan, the capital of China’s Hubei province, , the virus was initially named as 2019 novel coronavirus (2019-nCoV) by the World Health Organization (WHO) on January 12, 2020. Later, a Coronavirus Study Group (CSG) of International Committee proposed a new name for the virus as severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) on February 11, 2020. SARS-CoV-2 virus is very closely related to the original SARS-CoV virus and is thought to be zoonotic in origin. The genomic analysis of SARS-CoV-2 virus has revealed the genetic similarity in the coronavirus (COV) clusters with the genus Betacoronavirus, of the subgenus Sarbecovirus (lineage B). SARS-CoV-2 virus is 96% identical at the entire genome level with other bat COV samples, that is, BatCovRaTG13.
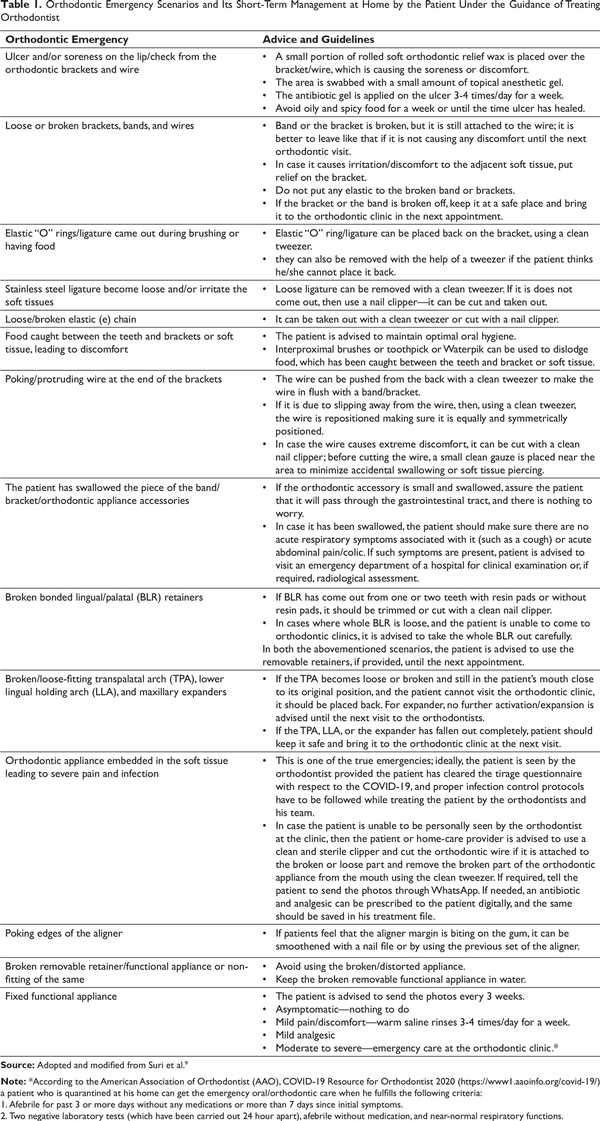
The COVID-19 has spread very rapidly to all the provinces in China. At present, more than 188 countries around the world have been affected (Figure 1)., The Director-General of WHO declared the condition a “Public Health Emergency of International Concern” on January 30, 2020. On March 11, 2020, the WHO declared the ensuing condition a pandemic. As of August 18, 2020, more than 220 million cases have been reported across the globe, resulting in more than 779,557 deaths. The rapid spread of the COVID-19 resulted in major health, financial, and humanitarian crises in an unprecedented manner at a time when the world was unprepared, which ultimately led to profound chaos and uncertainty. This has led to the enforcement of rules for very limited human movement by the respective federal agencies in various countries, leading to national emergencies and lockdowns.
The present scenario has caused orthodontic care providers to abruptly suspend active orthodontic treatment. At present, limited information and guidelines for clinical orthodontic care and the management of patients are available., This article aims to provide a comprehensive guideline for managing the emergency orthodontic condition and the patients at a clinical setup, using the currently available guidelines.
Etiology and Pandemic
The 2019-nCoV/SARS-CoV-2 Virus
SARS-CoV-2 is a non-segmented positive-sense RNA virus encapsulated by a lipid bilayer envelope, ranging from 60 nm to 140 nm in diameter with spike-like glycoprotein projections on its surface, giving it a crown-like appearance under the electron microscope; hence, the name coronavirus (Figure 2). The COVs are divided into four genera, identified as alpha, beta, gamma, and delta COVs. The SARS-CoV-2 is a member of the Betavirus genera.,
The COV genome has 96.2% similarity to a bat SARS-related COV (SARS-CoV; RaTG13) collected in Yunnan province, China, but it is not very similar to the genomes of the SARS-CoV (about 79%) or the MERS-CoV (about 50%). Both the SARS-CoV and the SARS-CoV-2 bind to angiotensin-converting enzyme II (ACE2) through the receptor-binding domain (RBD) of spike protein to initiate membrane fusion and enter human cells.- Five out of the six critical amino acid residues in the RBD were different between SARS CoV-2 and SARS-CoV (Figure 2), and a three-dimensional (3D) structural analysis indicated that the spike of the SARS-CoV-2 has a higher binding affinity to ACE2 than the SARS-CoV.,
A Snapshot of the COVID-19 Map of the Global Cases
Source: Center for System Science and Engineering at Johns Hopkins University, accessed at https://coronavirus.jhu.edu/map.html (accessed August 18, 2020).
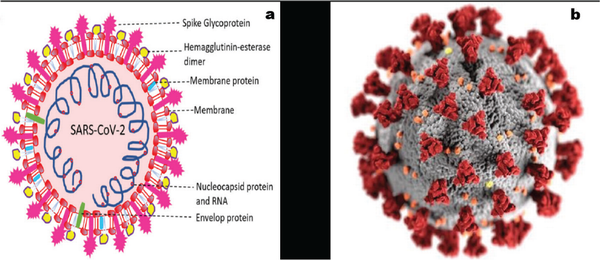
(a) The viral surface proteins, spike, envelope, and membrane, are embedded in a lipid bilayer. The single-stranded positive-sense viral RNA is associated with nucleocapsid protein. (b) The illustration, created at the Centers for Disease Control and Prevention (CDC), reveals ultrastructural morphology exhibited by coronaviruses
Source: 2a. Adapted with permission from Boopathi et al.; 2b. Image open source. CDC; Eckert and Higgins. https://cdc.gov/media/subtopic/images.htm.
Routes of Transmission
Epidemiological and genetic studies have highlighted the zoonotic origin of the COVID-19; its outbreak could have been initiated from animal to human transmission, followed by the human-to-human transmission., How and when this virus moved from animal to human populations is yet to be established. It has been suggested that the initial epidemiological outbreak began at the Wuhan seafood market in China, and the samples that were obtained from around the live section of the market were found to be positive for SARS-CoV-2 virus.
SARS-CoV-2 virus contains the ACE2 as a cell receptor, which is also present in horseshoe bat, pangolins, and humans. Molecular modeling studies reported that the binding affinity of SARS-CoV-2 virus to ACE2 receptors was high, thus affecting the human cells considerably. Cells of nasopharyngeal, alveolar, and gastrointestinal regions were the major targets because of the higher number of the ACE2 receptors., The strong association between the ACE2 receptor and the virus protein indicated that the population having more expression of ACE2 receptors could be more prone to the COVID-19 infection.
Human-to-human transmission of SARS-CoV-2 virus has been observed in health care, family, and community settings. The predominant mode of transmission was from the respiratory tract via droplets or indirectly through fomites and, to a lesser extent, via aerosols (Figure 3).,, The seeding of the virus to the mucous membranes of nose, oral cavity, and eyes is possible through contaminated fingers or objects following contact.A recent study under experimental conditions noted that the human COV remained infectious on inanimate surfaces at room temperature for up to 9 days. The virulence of the SARS-CoV-2 virus decreases with increasing temperature., At 30°C and above, veterinary COV persisted for 28 days. SARS-CoV-2 virus could specifically survive for a longer duration of up to 72 hours on surfaces of stainless steel and plastic in comparison to 4 hours on copper, and up to 24 hours on cardboard. SARS-CoV-2 virus was detected up to 3 hours in aerosol form or in dust, which creates a main concern in orthodontic and general clinical practice.
The basic reproductive number (Ro) for SARS-CoV-2 virus outbreak in Wuhan as on January 25, 2020, was estimated to be between 2.0 and 2.8. The mean incubation period appeared to be between 4 days and 7 days,- but it can be as short as 3 days or as long as up to 11 to 14 days (Figure 4). Studies have suggested that transmission can occur during incubation period and from asymptomatic or mildly infected people.- The convalescent patient has shown a near-normal body temperature for more than 3 days, near-normal respiratory symptoms, and the oropharyngeal to test swab the reverse transcriptase polymerase chain reactions (9RT-PCR) on two occasions were negative (taken at least 24 hours apart)., However, there is no risk of vertical transmission from mother to fetus. Studies demonstrated a strong presence of the virus in saliva; therefore, it can be considered as a potential source of infection., The virus was also isolated from blood and fecal swabs, but its presence in tear and urine has not been confirmed, suggesting the possibility of additional transmission routes. All secretions (except perspiration) and excretions, including diarrheal stools from patients with known or possible COVID-19, should be considered as potentially infectious.
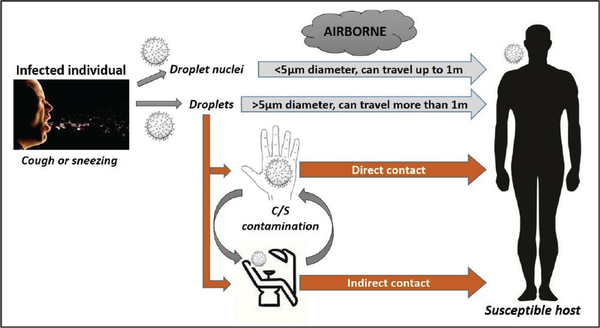
SARS-CoV-2 Virus Route of Transmission in Dental/Orthodontic Care Setup
Source: Adapted and modified with permission from Giudice et al.
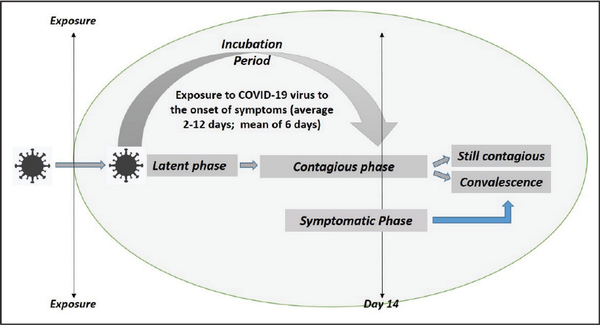
Various Phases Associated with COVID-19 Infection
Source: Adapted and modified with permission from Suri et.al.
Symptoms and Clinical Manifestation
Clinical symptoms of COVID-19 are nonspecific, while the clinical manifestations are very broad and can be classified as mild, moderate, and severe forms. The COVID-19 infection in the milder form is usually asymptomatic or present with very mild symptoms without signs of respiratory distress or radiological changes in a chest X-ray film. The moderate form is associated with increased body temperature (>37.4°C), dry cough, shortness of the breath, and nonspecific gastrointestinal symptoms such as diarrhea, respiratory symptoms, and signs of pneumonia on chest X-ray. Severe to a very severe form usually occurs 7 to 10 days after the infection, is characterized by difficulty in breathing and hypoxia with rapid progression to acute respiratory distress syndrome, septic shock, and multiple organ failure. Studies have suggested that 80% of the patients usually get a mild presentation of the symptoms, followed by 15% of moderate symptoms, and the remaining 5% present with severe to very severe clinical manifestations. Laboratory evaluation suggested that most patients have normal to decreased white blood cell counts and lymphocytopenia. In patients with severe complications, there is derangement of the neutrophil count, blood urea, and creatinine levels along with a continuous decrease in the lymphocyte count.
All age groups have shown sensitivity to the COVID-19 infection. However, it has been observed that the elderly population with associated medical risk factors are more prone for developing a severe risk of illness once infected. Studies show that younger individuals possess a better prognosis than individuals belonging to age groups above 60 years with or without associated risk factors. Any age groups with persistent comorbidity can exaggerate the severity and associated complications of the COVID-19 infection.
Implications for Orthodontic Management During and After the Pandemic
Telescreening and Triaging
A trained clinical staff member should perform an initial telephone triage or telescreen procedure before the dental appointment to assess the vulnerability of patients and the potential threat they may pose to members of the professional team, other patients, and accompanying people. Elderly patients, over 60 years of age, with medically debilitating conditions, especially those with cardiorespiratory disease and immunocompromised states, and pregnant patients in the third trimester, are more vulnerable and identified as susceptible to severe consequences of disease.,
The three most pertinent questions to be asked for initial screening should include the presence of any symptoms of febrile respiratory illness such as fever or cough, any recent travel history to an area with a high incidence of the COVID-19, or exposure to a person with known or suspected COVID-19 symptoms.-
Importantly, to identify high-risk areas, live global tracking of reported cases can be carried out by using the dashboard made accessible by the Center for Systems Science and Engineering at Johns Hopkins University (Figure 1). Similarly, National Informatics Centre, Government of India, has developed a COVID-19 tracking mobile app, Aarogya Setu (Figure 5). The COVID-19 patient triage plan can be considered for all patients (Figure 6). A positive response to either of the three questions should raise initial concern, and the elective dental care should be deferred for at least 2 weeks. The patients should be encouraged to engage in self-quarantine and contact their primary health-care physician by telephone or email.
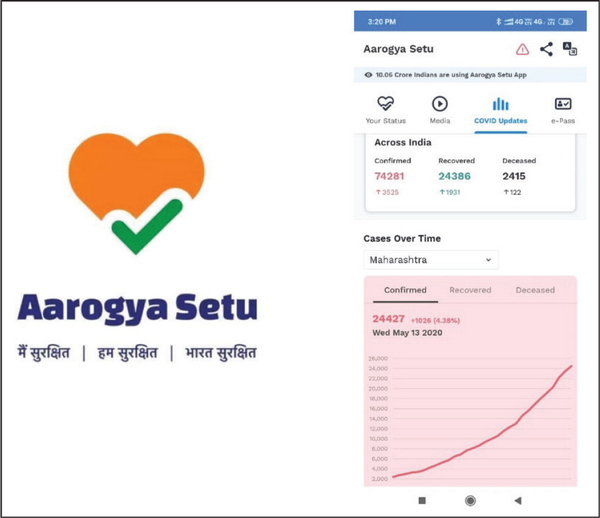
Arogya Setu, an Indian COVID-19 Tracking Mobile Application
Source:http://aarogyasetu.gov.in.
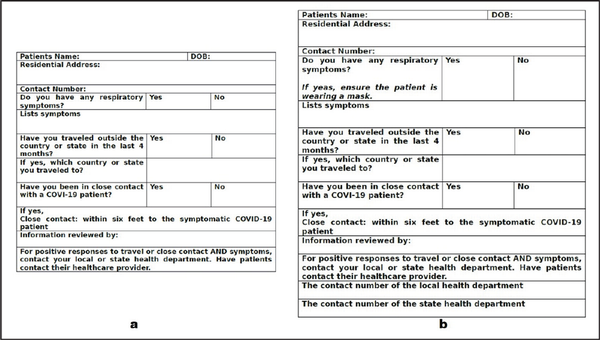
COVID-19 Patient Triage Forms (a) Patient Screening Form Before a Dental Visit, (b) Patient Screening Before the Elective or Emergency Procedure
Source: Adopted and modified from Coronavirus Disease (COVID-19) Patient Triage Plan, American Association of Orthodontists, https://www1.aaoinfo.org/covid-19/
Virtual Assistance
A virtual triage by using photos, videos, and video-calling can be of great help to differentiate and prioritize the actual orthodontic emergency that needs immediate attention in the clinics from the problem that can be self-aided by a home remedy and deferred without reporting to the clinic. A true dental emergency is the one that deals with swelling, uncontrollable pain, bleeding, infection, and trauma to teeth or bones. As far as orthodontic emergencies are concerned, severe pain or infection that arises due to the embedment of an orthodontic appliance into the gingiva or oral mucosa, circumstances related to dental trauma, or a condition in which a lack of management that leads to patient harm should be attended.,
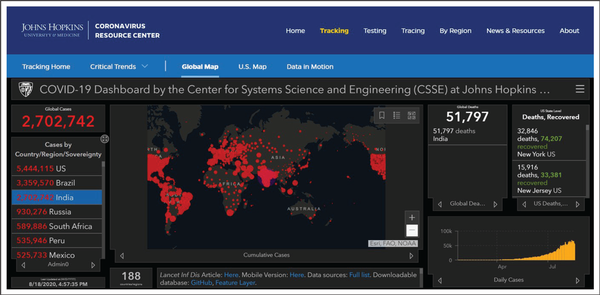
Many messenger apps and video-calling apps are available at present. Such a mobile messenger with a video-calling facility can be used by a hospital or dental clinic to communicate with patients. If an orthodontic emergency arises when the patient is at home, it is recommended that consultation occurs over the phone or through a video-calling app with the treating orthodontist. All the active orthodontic cases need to be contacted by the treating orthodontic office personnel and assurance provided. It is always advisable to obtain an electronically signed or verbal consent to provide the advice in this way and saved as a record. It is a professional duty to advise and guide the patient on managing minor orthodontic emergencies at home. Some of the frequent orthodontic emergencies, which may be faced by the patients, and their management strategies can be shared to all the active orthodontic patients by email or any other electronic means (Table 1).
History Recording and Patient Evaluation
A detailed and in-depth COVID-19 screening questionnaire, including medical history, social history gatherings, meetings, and travel history to assess the true emergency, is taken as soon as a patient reports to the clinic. The trained dental staff should measure the patient’s body temperature, using a noncontact forehead infrared thermal sensor., As per the Center for Disease Control and Prevention (CDC) guidelines, individuals exposed to a person with COVID-19 or a patient presenting with fever (99.32°F/37.4°C or higher), and any high-risk patient suspected as per the questionnaire should wear a mask or use a tissue to cover a cough and be offered separate space to wait.,
Suspected patients are informed about self-quarantining and checking their health regularly and recording it daily. Based on the assessment of the nature of the emergency, clinicians should decide the true extent of the severity of the dental condition, which may be helpful by either accepting the patient or deferring immediate dental care., Further, the patient should be encouraged to make a payment related to orthodontic services and consultation through online mode only, as the exchange of currency notes might act as a potential source for the spread of SARS-CoV-2 virus.
Personal Protecting Equipment and Infection Control in the Orthodontic Setup
The COVID-19 is a biological risk to which orthodontists, dental surgeons, dental hygienists, dental assistants, and other staff may be exposed and be infected if guidelines and protocols are not followed. SARS-CoV-2 virus is mainly transmitted through the oronasal route, as the viral load is maximum in the nasopharyngeal region of the infected person. Therefore, it is necessary to take measures to prevent diffusion of infection from one patient to another, to the dental devices, and the equipment; it is highly recommended to add a layer of airborne contact precautions to the routine orthodontic practice, minimizing the risk of virus transmission.
In orthodontic and dental practices, the prevention, reduction, and control of COVID-19 infection transmission can be achieved to a great extent by the use of the following:
appropriate personal protective equipment (PPE) and
appropriate decontamination, disinfection, and sterilization steps.
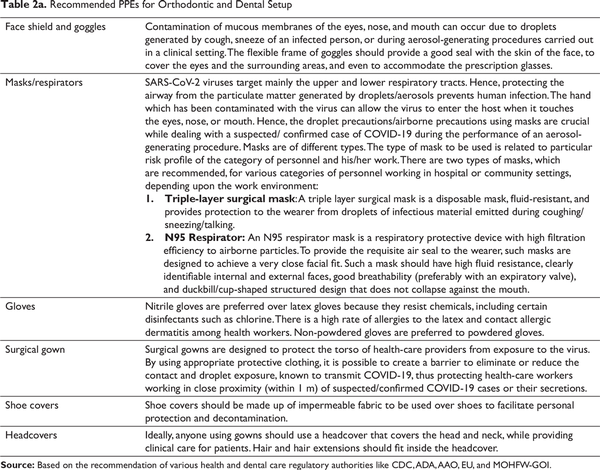
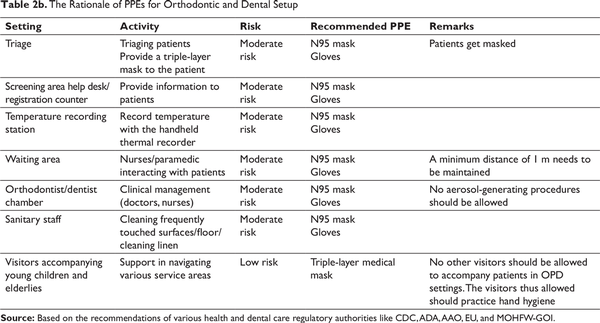
Details about each component of PPEs and rationale of its use have been highlighted in Tables 2a and 2b.
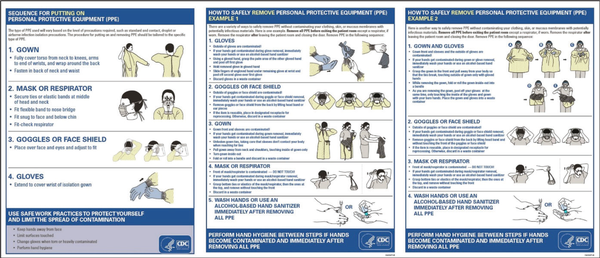
Sequence for Putting on and Removal of PPEs
Source:https://www.cdc.gov/hai/pdfs/ppe/PPE-Sequence.pdf
After the completion of clinical procedures, it is equally important to remove and dispose of the PPEs in an appropriate way to prevent cross- and environmental contamination. In this regard, the CDC has provided clear guidelines that should be strictly followed (Figure 7).
Orthodontic Emergency Management in the Clinic
After telescreening and virtual assistance, if the patient is required to be seen for a true clinical emergency, a standard protocol should be followed, which starts from the entry area to the operatory room. The orthodontic practice/office must maintain a very high standard of sterilization, infection prevention, and control protocol.,
Clinic Entrance Recommendation
At the point of entry to the clinic, the patient and an accompanying person should use an alcohol-based hand rub with at least 60% ethanol, or 75% 2-propanol to disinfect the hands. The patient should preferably visit the clinic alone or in company with a maximum of one attendant, who should not be at high risk for the COVID-19 infection (eg, medically compromised). A staff member with appropriate PPE (fit-tested N95 masks/respirators, double gloving, over the gown, and face/eye protection.) should record the temperature of every person using an infrared sensor thermometer to rule out fever before entering the registration area., A screening questionnaire should be completed verbally for each entrant and a distance of 6 feet between people should be maintained., This questionnaire should reconfirm the triage questions that were asked over the phone, and a consent signature is taken before any procedure (Figure 8).
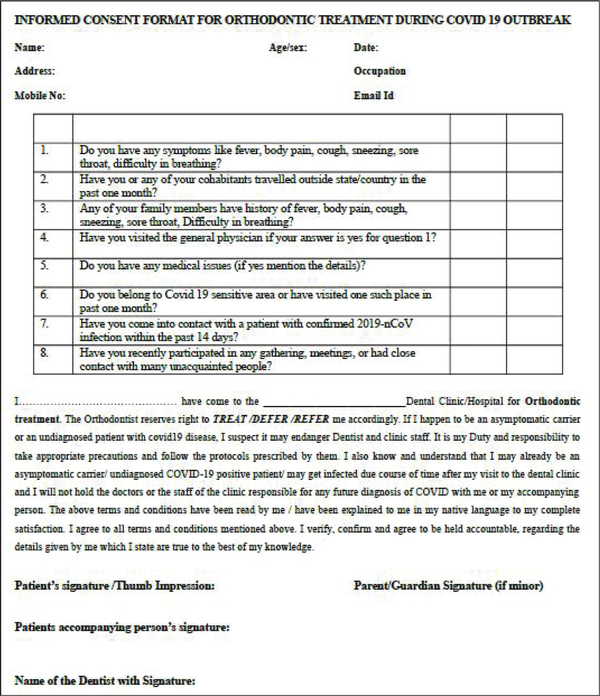
Informed Consent Form for Orthodontic Treatment During and Post-COVID-19 Outbreak
Source: Reproduced with permission from the Indian Orthodontic Society. https://iosweb.net/BulkFileUpload.aspx
Waiting Room Arrangements
Following the government’s “social distancing” policy, chairs should be positioned and separated by a safe distance and not facing each other. To avoid contact of people with magazines or other materials that cannot be disinfected should be removed. When more than one patient needs to be seen for an emergency, appointments should be staggered as much as possible. Once the patient enters the waiting room, the patient and accompanying person (in case the patient is minor) are advised to not touch the switches or any surfaces. They are advised to leave electronic devices and bags in the waiting room, and provision for the same should be made. Before the patient enters the orthodontic operatory, he/ she is reminded that in case of necessity, it is compulsory to cough or sneeze by covering the mouth and nose with tissue paper or a piece of cloth. The tissue paper is immediately disposed in a bin with lid, and the patient is advised to disinfect his/her hands with a sanitizer. The air-conditioning system should not be used in the waiting area as well as the orthodontic operatory room as it will recirculate, which can help in the spread of virus particles throughout the clinic.
Operatory Room
Only the patient should be allowed entry into the clinical/operatory area. The dental chair unit and the instruments, pliers, and accessories to be used should be well disinfected and sterilized. The orthodontist and the assistant must be well protected with recommended PPE and practice the proper procedural sequence for placement and removal of PPE. If the orthodontic procedure involves the use of rotary instruments such as air rotor and water, then the operatory should have regulated negative pressure; this will minimize the spread of aerosol. Structural changes in the dental operatory are advisable, whenever permitted. There is a mad rush for installing the air purifier before knowing about the exact requirements. It is advisable to take the opinion of an expert before venturing for the same. Further, air change per hour should be kept at least 8 to 10 times for effective removal and improve the quality of air in the operatory; also, it minimizes the hazard exposure to the dental surgeon and supporting team. In the case regulated negative pressure operatory is not possible, air purifiers with high-efficiency particulate air (HEPA) filters should be considered. Along with this, the adequate humidity level should be maintained, that is, in the range of 40% to 60%. Low-volume and high-volume evacuators (HVEs) should be judiciously used during dental procedures. HVEs ideally reduce the aerosol in the dental operatory by approximately 90%., If space is not a constraint, then it is advisable to have a close space/room for the aerosol-generating procedure with negative pressure airflow, high airflow rate, and with optional Ultraviolet-C (UV-C) lamps for irradiation after each procedure to keep the operatory safe for the next procedure.
Treatment Considerations
The orthodontic patient is asked to perform an oral rinse for 30 seconds with 1% solution of H2O2 (1 part of 10 vol 30% and 2 parts of water) or with 0.2% povidone iodine for at least 30 seconds before the orthodontic procedure to reduce the viral load in the patient’s saliva as viruses are sensitive to oxidation and structural lysis by these agents., The SARS-CoV-2 virus is not sensitive to routinely used oral chlorhexidine rinse.
Orthodontic and dental practitioners should refrain from performing any procedures that lead to the generation of aerosols, by avoiding air-water syringes, high-speed handpieces, and ultrasonic scalers. This is because long-distance transmission is possible when viral particles become suspended in the air, and they may remain in aerosols for up to 3 hours. The CDC has recommended that N95 masks, eye protection, gloves, and a gown should be used for any aerosol-generating procedures, as asymptomatic individuals can transmit the SARS-CoV-2 virus. Intraoral imaging (IOPA) should be restricted and extraoral radiographs like the excessive salivation orthopantomogram (OPG) should be utilized to reduce the excessive salivation and gag reflex associated with intraoral radiographs., If a local anesthesia application is required, the gel form of local anesthetics is preferred over spray type as it might generate the aerosol; this might cause the potential spread of the virus in the air. Disposable and single-use instruments and devices should be used whenever possible to reduce the cross-infection risks.
Various hands-free intraoral lower vacuum evacuator along with HVE and external mobile suction units with appropriate face mask and PPEs can be used during the aerosol-generating procedures like bonding and debonding of orthodontic brackets. Before the initial bonding is carried out, the patient may be asked to rinse his/his mouth with 1% H2O2 or 0.2% povidone iodine. Tooth surfaces should be cleaned with pumice and rinsed with water, followed by blot drying with the cotton roll. The etchant used should have increased viscosity so that it should not spread to the nearby area, thus putting more effort into cleaning it. After 30 seconds, it should be cleaned with water and dried, followed by the application of primer and bonding resin on the tooth and bracket. Before curing the resin, excess flash of it should be removed using the hand instruments. During debonding, extreme care should be taken to minimize the generation of aerosol. The tungsten carbide burs should be used to remove the composite resin with HVE and adequate water spray. The handpieces used during the procedures should have anti-retraction valves to prevent the backflow of water, thus minimizing the risk of contaminations. Along with this, external mobile aerosol suction units, which can be positioned near to the area of operation during the dental procedure, can be used to further minimize the aerosol in the dental operatory.
The COVID-19 pandemic has brought various challenges to the orthodontist and changes the view regarding the various aspects of treatment planning and its execution. The aligner treatment for mild-to-moderate malocclusion can be considered as an alternate option., The treatment outcome for aligner treatment is comparable to the contemporary fixed orthodontic treatment for mild-to-moderate malocclusion with acceptable clinical outcomes. They reduce the number of follow-up visits for patients and parents to the orthodontist. Such treatments can enhance the practice of social distancing in these challenging situations.
Post-treatment Consideration
Orthodontic practices must follow rigorous disinfection protocols, following the completion of an emergency or elective treatment, to minimize spread through fomites. Natural fresh air is always allowed between two patients in the operatory area and frequently in the waiting room. There are two means to achieve this: first, by opening a window, which allows the influx of fresh air (if there is provision for window) and, second, by using a medical-grade purifier with appropriate air filters.
Steel wires and appliance parts that are cut or removed should be treated as highly infected medical waste and disposed as a medical hazard. All surfaces should be thoroughly disinfected using hospital-grade disinfectants like sodium hypochlorite. For COV disinfection, bleach/sodium hypochlorite should be used for 1 minute at a higher concentration of 0.1% to 0.2%, compared to a standard 0.05% concentration, which was in routine disinfection use before the COVID-19 pandemic., Various studies have suggested that sodium hypochlorite at 0.1% to 0.2% concentration is an effective disinfectant against the SARS-CoV-2 virus when the time of contact is kept at 1 minute compared to the quaternary ammonium compounds.- Sodium hypochlorite is widely used in the dental operatory as a disinfectant because of its broad-spectrum activity against capsulated and non-capsulated viruses, bacteria, and other microorganisms; they are prepared, and they have the ability to dissolve the organic materials that come into their contact.- However, its main drawback is its smell and corrosion of the carbon steel part of the orthodontic appliance after regular use. Quaternary ammonium compounds are also considered to be a potential disinfectant, but their potency for SARS-CoV-2 virus is less than sodium hypochlorite., They are relatively expensive and need more time compared to the sodium hypochlorite for disinfecting the inanimate surfaces. Post-procedure decontamination of the operatory room can be done effectively with hydrogen peroxide vapor.
Dental waterlines remain a concern for microbial colonization and a potential source of contamination. Modern waterline systems have a valve to prevent the backflow of water containing the microorganisms. Nevertheless, they can be a potential source and spread of infection in the operatory. Therefore, following the use, the waterline system should be adequately purged to prevent a backflow of pathogens, which can reside in the plastic tubing. All instruments should be appropriately disinfected and sterilized immediately, and all used, as well as unused, disposables that were within the exposed area of the operatory should be presumed to be infected and disposed as infected medical waste. An earlier study demonstrated that SARS-CoV-2 virus might become resuspended in the air during the removal of contaminated PPE or from the floor, by the movement of health-care providers. Therefore, the treating clinician should remove the PPE in a well-demarcated sealed room.
Once all the clinical procedures have been completed for the day, all surfaces should be wiped with a 0.1% to 0.2% bleach solution. If any surface is visibly soiled, then it is first cleaned with detergent and water, dried, and wiped with 1,000 ppm of bleach solution. Further, if the operatory has any high-efficiency filter for air purification, regular checks are required. Peroxyacetic acid is used for the fumigation of the clinic at the end of the working day, and the area should be closed for at least 2 h. The next day’s operation should be commenced after thorough air ventilation.
Dental office waste should be routinely disposed of as standard regulated medical waste (RMW) with color-coded bins/bags/containers. The CDC RMW Guidelines should be adhered and followed and states that:
A single, leak-resistant biohazard bag is usually adequate for the containment of RMW wastes, provided the bag is sturdy, and the waste can be discarded without contaminating the bag’s exterior.
Puncturing or contamination of the bag requires placement into a second biohazard bag.
All bags should be securely closed for disposal.
Dental waste generated from the treatment of a true emergency of confirmed or suspected COVID-19 patients are considered medically infectious waste and must maintain proper segregation and should be strictly disposed of. This requires the use of double-layer medical waste package bags, ensuring adequate strength without leaks. Mandatory labeling of “COVID-19” to store COVID-19 waste and separating them in the temporary storage room are carried out before handing them over to the authorized staff of the common biological waste (CBW) treatment facilities’ collection vans.,
Of all the PPEs, N95 filtering facepiece respirators (FFRs) can be used for an extended time up to 8 hours and limited re-use up to five times under acceptable circumstances as per the CDC guidelines, following their appropriate decontamination.,
Discussion
The dental practice and orthodontic care during the pandemic and future practice will require precautionary and selective case evaluation based on the practitioner’s judgment to reduce cross-contamination and prevent new outbreaks.
The clinician should follow the guidelines provided by the concerned health regulatory authorities. Modification and redesign of the dental clinic might be required to maintain efficient air circulation and ventilation and appropriate standard PPE. Effective telescreens and triaging should be part of a routine clinical screening protocol until the uncertainty of the COVID-19 pandemic subsides. Any suspected patient with signs and symptoms of COVID-19 should require deferred orthodontic care and a referral to the COVID-19 screening unit as a priority. The dental treatment should be minimally invasive, of minimal contact, and avoid aerosols generation.
The COVID-19 pandemic has markedly influenced all dental health professionals and orthodontists. There is increased requirement and demand for clinical inventory leading to increased practice costs. Nevertheless, orthodontists and dental practitioners should maintain a balance between a level of care and the cost involved. Patients should be well informed with the changed norms of infection control measures and the cost factors.
The clinic disinfection protocols during pre-treatment, during treatment, and posttreatment should be strictly followed. The staff and patients’ well-being should be given maximum priority. The proposed workflow and guidelines collected from various health regulatory authorities in the article will provide appropriate and effective management of dental and orthodontic care during the COVID-19 pandemic and post-COVID practice.
Conclusions
The COVID-19 outbreak has affected human existence in many ways, with uncertainty faced globally. The orthodontists need to redesign the clinical practices into a need-based dentistry with the sole purpose of removing the risk of cross-contamination of the SARS-CoV-2 virus to dental staff and patients. During a pandemic emergency, orthodontic treatment should ensure only the management of a true emergency with the appropriate PPE, following the guidelines and protocols provided by the WHO and local authorities after effective telescreening and triage. Orthodontic practice and patient management must adapt to changes and maintain a balance between service and social needs.
- 1. Guo YR, Cao QD, Hong ZS The origin, transmission, and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak—an update on the status. Military Med Res. 2020;7:11. doi:10.1186/s40779-020-00240-.
- 2. Lu H, Stratton CW, Tang YW. The outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J Med Virol. 2020; 92:401–402.
- 3. WHO. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). WHO. https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf. Accessed May 12, 2020.
- 4. Wang C, Horby PW, Hayden FG A novel coronavirus outbreak of global health concern. Lancet. 2020; 395:470–473.
- 5. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real-time. Lancet Infect Dis. 2020. doi:10.1016/S1473-3099(20)30120-.
- 6. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–160.
- 7. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE). Johns Hopkins University. https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6. Accessed August 18, 2020.
- 8. Caprioglio A, Pizzetti GB, Zecca PA Management of orthodontic emergencies during 2019-nCoV. Prog Orthod. 2020;21:10. doi:10.1186/s40510-020-00310-.
- 9. Suri S, Vandersluis YR, Kochhar AS Clinical orthodontic management during the COVID-19 pandemic. Angle Orthod. 2020. doi:10.2319/033120-236..
- 10. Zhu N, Zhang D, Wang W A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382:727–733.
- 11. Richman DD, Whitley RJ, Hayden FG. Clinical Virology, 4th ed. Washington: ASM Press; 2016.
- 12. Zhou P, Yang XL, Wang XG A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020. doi:10.1038/s41586-020-2012-.
- 13. Paraskevis D, Kostaki EG, Magiorkinis G Full-genome evolutionary analysis of the novel coronavirus (2019-nCoV) rejects the hypothesis of emergence as a result of a recent recombination event. Infect Genet Evol. 2020;79:104212. doi:10.1016/j.meegid.2020.10421.
- 14. Lu R, Zhao X, Li J Genomic characterization and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020. doi:10.1016/S0140-6736(20)30251-.
- 15. Wrapp D, Wang N, Corbett KS Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. bioRxiv. 2020. doi: 10.1101/2020.02.11.944462
- 16. Peng X, Xu X, Li Y Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020; 12:1–6.
- 17. Giudice RL. The severe acute respiratory syndrome coronavirus-2 (SARS CoV-2) in dentistry. Management of biological risk in dental practice. Int J Environ Res Public Health. 2020;17:3067.doi:10.3390/ijerph17093067
- Organization. 18. World Health Novel coronavirus (2019-nCoV). Situation Report 11. January 31, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200131-sitrep-11-ncov.pdf?sfvrsn=de7c0f7_4. Accessed May 11, 2020.
- 19. Li Q, Guan X, Wu P Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020; 382:1199–1207.
- 20. Chen Y, Guo Y, Pan Y Structure analysis of the receptor binding of 2019-nCoV. Biochem Biophys Res Commun. 2020; 525:135–140.
- 21. Kampf G, Todt D, Pfaender S Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020; 104:246–251.
- 22. World Health Organization. Considerations for the provision of essential oral health services in the context of COVID-19. Interim guidance, August 3, 2020. https://who.int/publications/i/item/who-2019-ncov-oral-health-2020-1. Accesses August 4, 2020.
- 23. van Doremalen N, Bushmaker T, Morris D Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. N Engl J Med. 2020. doi:10.1056/NEJMc200497.
- 24. Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modeling study. Lancet. 2020; 395:689–697.
- 25. Ryu S, Chun BC. An interim review of the epidemiological characteristics of 2019 novel coronavirus. Epidemiol Health. 2020;42:e2020006. doi:10.4178/epih.e2020006e202000.
- 26. Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travelers from Wuhan, China, January 20–28, 2020. Euro Surveill. 2020;25(5):pii=2000062. doi:10.2807/1560-7917.ES.2020.25.5.200006.
- 27. Zou L, Ruan F, Huang M SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020. doi:10.1056/NEJMc20017.
- 28. Pan Y, Zhang D, Yang P, Moon LLM, Wang Q. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect Dis. 2020:24. doi:10.1016/S1473-3099(20)30113-.
- 29. Hoehl S, Rabenau H, Berger A Evidence of SARS-CoV-2 infection in returning travelers from Wuhan, China. N Engl J Med. 2020; 382:1278–1280.
- 30. Lan L, Xu D, Ye G Positive RT-PCR test results in patients recovered from COVID-19. J Am Med Assoc. 2020. doi:10.1001/jama.2020.278.
- 31. Ling Y, Xu SB, Lin YX Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin Med J (Engl). 2020. doi:10.1097/CM9.000000000000077.
- 32. To KKW, Tsang OTY, Yip CCY Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020. doi:10.1093/cid/ciaa14.
- 33. Wang WK, Chen SY, Liu IJ Detection of SARS-associated coronavirus in throat wash and saliva in early diagnosis. Emerg Infect Dis. 2004; 10:1213–1219.
- 34. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. J Am Med Assoc. 2020; 323:1239–1242.
- 35. Guan WJ, Ni ZY, Hu Y Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020. doi:10.1056/NEJMoa200203.
- 36. Verity R, Okell LC, Dorigatti I Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020. doi:10.1016/S1473-3099(20)30243-.
- 37. Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. J Am Med Assoc. 2020. doi:10.1001/jama.2020.4683.
- 38. Dawish S. COVID-19 considerations in dental care. Dent Update. 2020;47:4. doi.10.12968/denu.2020.47.4.287
- 39. Alharbi A, Alharbi S, Alqaidi S. Guidelines for dental care provision during the COVID-19 pandemic. Saudi Dent J. 2020; 32:181–186.
- 40. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real-time. Lancet Infect Dis. 2020. doi:10.1016/S1473-3099(20)30120-.
- 41. Bhoopathi S, Pom AB, Kolandaivel P. Novel 2019 Corona virus structure, mechanism of action, antiviral drug promises, and rule out against its treatment. J Biomol Struct. Dyn. 2020. doi:10.1080/07391102.2020.1758788.
- 42. Khanna RC, Cicinelli MV, Gilbert SS, al. et COVID-19 pandemic: lessons learned and future directions. Indian J Ophthalmol. 2020;68:703–710.
- 43. Peng X, Xu X, Li Y Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi:10.1038/s41368-020-0075-.
- 44. Centers for Disease Control and Prevention. Infection control: severe acute respiratory syndrome, coronavirus 2 (SARS-CoV-2). https://www.cdc.gov/coronavirus/2019-ncov/infection-control/controlrecommendations.html. Accessed July 30, 2020.
- 45. WHO. Coronavirus Situation Report-83. https://www.whi.int/emergencies/siseases/novel_coronavirus-2019/situation-reports/>. Accessed July 30, 2020.
- 46. Centers for Disease Control and Prevention (CDC). Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings. 2020. https://www.cdc.gov/coronavirus/2019-ncov/infectioncontro/control-recommendations.html?CDC_AA_refVal¼https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhcp%2Finfection-control.html#manage_access. Accessed May 14, 2020.
- 47. Ti LK, Ang LS, Foong TW What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Can J Anaesth. 2020; 67:756–758.
- 48. American Dental Association. Coronavirus frequently asked questions. 2020. https://success.ada.org/en/practice-management/patientcoronavirusfrequentlyaskedquestions. Accessed July 30, 2020.
- 49. Kim HJ, Ko JS, Kim TY. Recommendations for anesthesia in patients suspected of coronavirus 2019-nCoV infection. Korean J Anesthesiol. 2020; 73:89–91.
- 50. Xu K, Lai K, Liu Z. Suggestions on the prevention of COVID-19 for health care workers in the department of otorhinolaryngology head and neck surgery. World J Otorhinolaryngol Head Neck Surg. 2020. doi:10.1016/j.wjorl.2020.03.00.
- 51. Xie X, Li Y, Sun H Exhaled droplets due to talking and coughing. J R Soc Interface. 2009;6(Suppl 6): S703–S714.
- 52. Ather A, Nikita B, Ruparel NB Coronavirus disease 19 (COVID-19): implications for clinical dental care. J Endod. 2020; 46:584–595.
- 53. Mengng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020. doi:10.1177/002203452091424.
- 54. Harrel SK. Contaminated dental aerosols. Dimens Dent Hyg. 2003; 1:16–20.
- 55. Devker NR, Mohitey J, Vibhute A A study to evaluate and compare the efficacy of preprocedural mouth rinsing and high-volume evacuator attachment alone and in combination in reducing the amount of viable aerosols produced during ultrasonic scaling procedure. J Contemp Dent Pract. 2012; 13:681–689.
- 56. World Health Organization. Infection prevention and control of epidemic- and pandemic-prone acute respiratory infections in health care. Annex G, use of disinfectants: alcohol and bleach. 2014. https://www.ncbi.nlm.nih.gov/books/NBK214356/. Accessed July 30, 2020.
- 57. Dong Y, Mo X, Hu Y Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020. doi:10.1542/peds.2020-070.
- 58. Liu Y, Ning Z, Chen Y Aerodynamic characteristics and RNA concentration of SARS-CoV-2 aerosol in Wuhan hospitals during COVID-19 outbreak. bioRxiv. 2020. doi:10.1101/2020.03.08.98263.
- 59. Tao KX, Zhang BX, Zhang P General surgery branch of Hubei Medical Association, general surgery branch of Wuhan Medical Association recommendations for general surgery clinical practice in 2019 coronavirus disease situation. Zhonghua Wai Ke Za Zhi. 2020; 58:170–177.
- 60. World Health Organization. Infection prevention and control during health care when COVID-19 is suspected: interim guidance 2020. World Health Organization. https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125. Accessed July 27, 2020.
- 61. Eliades T, Koletsi D. Minimizing the aerosol-generating procedures in orthodontics in the ear of a pandemic: current evidence on the reduction of hazardous effects for the treatment team and patients. Am J Orthod Dentofacial Orthop. 2020. doi.10.1016/j.ajodo.2020.06.002
- 62. Srirengalaksmi M, Venugopal A, Pangilinan PJP The way forward. Part 1. Office environmental and infection control. J Clin Orthod. 2020. https://www.jco-online.com/archive/2020/06/340-orthodontics-in-the-covid-19-era-the-way-forward-part-1-office-environmental-and-infection-control/. Accessed August 16, 2020.
- 63. Chaudhary P, Sharan J, Amerco KKA. COVID-19. Precautions and recommendations. Am J Orthod Dentofacial Orthop. 2020;158:312.
- 64. Eliades T, Koletsi D. Minimizing the aerosol-generating procedures in orthodontics in the ear of a pandemic: current evidence on the reduction of hazardous effects for the treatment team and patients. Am J Orthod Dentofacial Orthop. 2020. doi:10.1016/j.ajodo.2020.06.00.
- 65. Infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in health-care settings. March 19, 2020. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/infectioncontrol/controlrecommendations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhcp%2Finfection-control.html. Accessed July 27, 2020.
- 66. ECRI. Disinfectant concentrations and contact time for EPA’s list of products effective against novel coronavirus SARS-CoV-2, the cause of COVID-19 (2020). May 13, 2020. https://www.ecri.org/components/HDJournal/Pages/Disinfectant-Concentrations-for-EPA-list-N-COVID-19.aspx?tab=2. Accessed May 14, 2020.
- 67. Samara F, Bardan R Are disinfectant for the prevention and control of COVID-19 safe? Health Secu. 2020; 18:1–3.
- 68. Kanf G. Potential role of inanimate surfaces for the spread of coronaviruses and their inactivation with disinfectant agents. Inf Prevnt Prac. 2020. doi:10.1016/j.infpip.2020.10004.
- 69. Ansaldi F, Banfi F, Morelli P SARS-CoV, influenza A and syncytial respiratory virus resistance against common disinfectants and ultraviolet irradiation. J Prevent Med Hyg. 2004; 45:5–8.
- 70. Oliet S, Sorin SM. Inhibition of the corrosive effect of sodium hypochlorite on carbon steel endodontic instruments. J Endodontol. 1978; 4:12–16.
- 71. Centers for Disease Control and Prevention (CDC). Regulated medical waste, chapter I, part 1 of guidelines for environmental infection control in health-care facilities (2003). July 2019. https://www.cdc.gov/infectioncontrol/guidelines/environmental/background/medical-waste.html. Accessed July 27, 2020.
- 72. Centers for Disease Control and Prevention (CDC). 2020a. Recommended guidance for extended use and limited re-use of N95 filtering facepiece respirators in health care settings. https://www.cdc.gov/niosh/topics/jcwcontrols/recommendedguidanceextuse.html. Accessed April 19, 2020.
- 73. Jena AK, Sharan J. Decontamination strategies for filtering facepiece respirators (FFRs) in health care organizations: a comprehensive review. Ann Work Expo Health. 2020. doi.10.1093/annweh/wxaa090