Introduction
Chronic fatigue syndrome (CFS) is a medical condition of which the etiology and prognosis are not fully understood (). CFS is characterized by severe and medically unexplained fatigue of at least 6 months. Patients also experience a number of other symptoms like self-reported impairments in concentration and short-term memory, sleep disturbances, muscle pain, and headache (). Studies show that the course and duration of the illness vary with some people improving over time, but for many, CFS is a chronic condition (; ; ). When symptoms cannot be attributed to any known disease, the most used treatment forms for people with CFS are cognitive behavioral therapy (CBT) which attends to factors that may predispose and perpetuate symptoms and graded exercise therapy (GET) which is based on the concept of deconditioning (for a review, see ).
Having CFS has serious consequences for all domains in life (e.g. loss of employment, social isolation) and can be considered an important stressor. This may make people with CFS more vulnerable to feelings of depression, secondary to their illness. Studies indeed show that people with CFS report higher levels of depression and greater perceived distress (). As CFS puts a heavy burden on patients and is often long-lasting, it is important to find optimal ways of coping with the disease in order to lower levels of depression. This might help in achieving a better (emotional) quality of life.
A few studies have been performed on the way people cope with CFS and its relationship with emotional problems. Coping strategies such as problem-focused coping and seeking social support () have been found to be related to better mental health in people with CFS. Coping strategies such as cognitive avoidance () and behavioral disengagement () have been related to poorer mental health in this group. Various coping strategies have remained unstudied. Lately, cognitive coping strategies have been studied intensively. Studies among people from the general population showed significant relations between the following cognitive coping strategies and depressive symptoms: self-blame, rumination, positive reappraisal (inversely), positive refocusing (inversely), and catastrophizing (, , ). Whether these strategies are related to depressive symptoms in people with CFS remains to be studied.
To come to generalized conclusions, more research is needed on the relationships between a broad range of coping strategies and emotional problems. In this study, we will focus on a broad range of specific cognitive and behavioral coping strategies. First, we will examine the bivariate relationships between coping and depressive symptoms. Next, the multivariate relationships will be explored.
Methods
Sample
A total of 36 people with CFS filled in the questionnaire. Six of them did not complete the questionnaire. Of the remaining 30 participants, the majority was female (n = 28; 93%). The age of the participants ranged from 16 to 58 (mean (M) = 32.13, standard deviation (SD) = 10.65). Most participants were Dutch (n = 25; 83%), the remaining participants were from another European country. Over half (n = 17; 57%) were married or living together and 11 respondents (40%) had children. Eight respondents (27%) were higher educated (college or university) and the others attended higher general secondary education or pre-university education (20%), intermediate vocational education (27%), lower secondary education (17%), or primary education (3%). Seven participants (23%) had a paid part-time job, the remaining did not have a paid job (two participants did volunteer work). Half of the respondents (53%) reported to have CFS for over 5 years and 43 percent reported to use medication for their CFS. Symptoms mentioned were severe fatigue (100%), non-refreshing sleep (90%), concentration problems (90%), subjective memory impairment (77%), long during feelings of malaise after physical strain (73%), muscle pain (63%), pain in joints (60%), headache (47%), and a sore throat (23%).
Procedure
After obtaining permission from the Ethics Committee of the University, participants were recruited through a CFS forum. People with CFS were invited to fill in an online questionnaire through a secured website. All respondents were informed about the goal of the study at the beginning of the questionnaire. They were told that they were free to decide whether they wanted to participate and that they could stop at any time without giving a reason. They were also told that anonymity was guaranteed. After this information, participants had to fill in an informed consent form.
Measures
Cognitive coping
To measure cognitive coping strategies the Cognitive Emotion Regulation Questionnaire (CERQ) was used (, ). The CERQ consists of 36 items and 9 subscales, and assesses what people think at the time of or after the experience of threatening or stressful life events. In this study, respondents were asked which specific cognitive coping strategies they used in relation to having CFS. Each subscale consists of four items. Each of the items has a 5-point Likert scale, with values that range from 1 = (almost) never to 5 = (almost) always. A subscale score can be obtained by adding up the four items, indicating the extent to which a certain cognitive coping strategy is used (possible scores for each subscale ranged from 4 to 20). The CERQ subscales are as follows: self-blame, which refers to thoughts of blaming yourself for your CFS; acceptance, which refers to thoughts of accepting your CFS and resigning yourself to it; rumination, which refers to thinking about the feelings and thoughts associated with the CFS; positive refocusing, which refers to thinking about joyful and pleasant issues instead of thinking about the CFS; refocus on planning, which refers to thinking about what steps to take and how to handle the CFS; positive reappraisal, which refers to thoughts of attaching a positive meaning to the CFS in terms of personal growth; putting into perspective, which refers to thoughts of playing down the seriousness of the CFS or comparing it relative to other events that are worse; catastrophizing, which refers to thoughts of explicitly emphasizing the terror of the CFS; and other-blame, which refers to thoughts of putting the blame for the CFS on others. The psychometric properties of the CERQ were proven to be good (, ; ), with Cronbach’s alpha coefficients in most cases well over .70 and in many cases even over .80. Furthermore, the CERQ has been shown to have good factorial validity, good discriminative properties and good construct validity ().
Behavioral coping
To measure behavioral coping strategies two subscales of the COPE were used (), reflecting pure behavioral strategies: active coping and use of emotional social support (two items were slightly rephrased to emphasize the behavior). Each subscale consists of four items. Each of the items has a 4-point Likert scale, with values that range from 1 = rarelyor never to 4 = very often. A subscale score can be obtained by adding up the four items, indicating the extent to which a certain coping strategy is used (possible scores for each subscale range from 4 to 16). Good psychometric properties have been found ().
Depressive symptoms
Depressive symptoms were measured by the Depression Subscale of the Hospital Anxiety and Depression Scale (HADS: ; Dutch translation by ). All seven items have a 4-point scale (0–3). High scores on the Depression Subscale reflect increased levels of depression. The HADS is a reliable self-report instrument with sufficient internal validity ().
Statistical analyses
To study the relationships between cognitive coping, behavioral coping and depressive symptoms, Pearson correlations and multiple regression analysis (MRA) were used. Because the sample size was not large enough to include all variables in the MRA, only the coping strategies which had a significant correlation with depressive symptoms were included in the MRA to explore the possible model. In this MRA, “method stepwise” was used ().
Results
Preliminary analyses
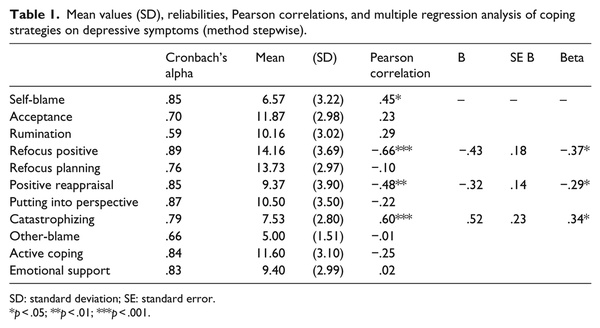
Prior to performing the main analyses, mean values, SDs, and alpha reliabilities of the variables were calculated (Table 1). The alpha reliabilities appeared to be acceptable to good. The mean depression score was 8.17 (SD = 4.24). When caseness of depression was defined by a score of 8 or above (), 53.3 percent of the respondents fulfilled this criteria. Furthermore, Pearson correlations among the study variables were computed. The correlations among the coping variables were not so high as to indicate that multicollinearity might be problematic for the MRA (see ).
Relationships between coping and depressive symptoms
To study the relationships between coping and depressive symptoms, Pearson correlations were calculated (Table 1). Various cognitive coping strategies were significantly related to depressive symptoms. Self-blame and catastrophizing were positively correlated with depressive symptoms, while refocus positive and positive reappraisal were negatively correlated with depressive symptoms. None of the behavioral coping strategies had a significant correlation with depressive symptoms.
Next, an exploratory MRA (method stepwise) was performed (Table 1). The four coping strategies which had a significant correlation with depressive symptoms were included. In the final solution, catastrophizing had a positive significant relationship with depressive symptoms, whereas refocus positive and positive reappraisal had a negative significant relationship with depressive symptoms. A total of 55% of the variance (adjusted R2) was explained (F(3,26) = 12.67; p < .001).
Discussion
Although people with CFS report heightened levels of depressive symptoms and may benefit from psychological interventions that help them to cope with the disease, only a limited number of studies have focused on which coping factors could be useful in shaping the specific content of such interventions. This study included a wide range of coping techniques. The aim was to study the relationships between cognitive coping, behavioral coping, and symptoms of depression in people with CFS, in order to find relevant, evidence-based, intervention targets.
First, the bivariate relationships were studied. Various coping techniques appeared to be related to depressive symptoms. When looking closer at the different forms of coping strategies, it is interesting to see that the cognitive coping strategies were especially important: self-blame, positive refocusing, positive reappraisal, and catastrophizing were all related to the level of depressive symptoms. These findings are in line with earlier studies among the general population (, , ). In contrast, none of the behavioral coping strategies were significantly related to depression. This is not in line with earlier research, where both problem-focused coping and seeking social support () were related to better mental health in people with CFS. However, one should keep in mind that in this study, the power is rather low. Active coping showed a (non-significant) small to moderate relationship with depressive symptoms. Finally, in the exploratory model, especially, positive refocusing, positive reappraisal, and catastrophizing were important. Together, they explained a large amount of the variance, indicating that they might be important intervention targets.
If our findings can be replicated, they suggest that cognitive coping strategies have a stronger influence than behavioral coping strategies on symptoms of depression in people with CFS. Possibly, this has to do with the fact that people with CFS experience severe fatigue, making it hard to successfully cope with the condition in a behavioral way. In addition, for many people, CFS is a chronic condition for which no physical cause has been found so far. Patients cannot take specific actions that will cure them from having CFS. Coping strategies such as thinking about joyful and pleasant issues instead of thinking about the CFS and attaching a positive meaning to the CFS in terms of personal growth may be more effective methods for successfully adjusting to living with this (often) chronic condition. In addition, catastrophizing and self-blaming thoughts about the CFS should be avoided. If the findings of this study can be confirmed, they would have important clinical implications. They suggest that these specific coping strategies are relevant for the development of new evidence-based psychological treatment programs for depression (e.g. coping skills training), specifically tailored for people with CFS. In addition, existing programs for people with CFS could be adapted in order to focus on these specific coping strategies.
This study has some methodological concerns. The first issue of concern is the small sample size and the representativeness of the group studied. The sample was obtained through a CFS forum and thus self-selected. Women were overrepresented. The second limitation of this study results from the cross-sectional design. No conclusions can be drawn regarding the causality or temporal order of the cognitive coping strategies and depressive symptoms. One might lead to the other or they might influence each other. However, in order to bring about change or break this cycle, one could well intervene on the coping strategies. Finally, a limitation was that all variables were measured by self-report, which may have caused bias.
Despite these shortcomings, several cognitive coping strategies seem to be related to symptoms of depression in people with CFS. Especially, the cognitive coping strategies refocus positive, positive reappraisal and catastrophizing seem to be important factors. If these findings can be confirmed, they could contribute to the focus and content of psychological programs for people with CFS to optimally cope with their disease and lower levels of depression.
Declaration of conflicting interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Ax S, Gregg VH, Jones D (2001) Coping and illness cognitions: Chronic Fatigue Syndrome. Clinical Psychology Review 21: 161–182.
- Bjelland I, Dahl AA, Tangen Haug T, et al. (2002) The validity of the Hospital Anxiety and Depression Scale: An updated literature review. Journal of Psychosomatic Research 52: 69–77.
- Carver CS, Scheier MF, Weintraub JK (1989) Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology 56: 267–283.
- Fernie BA, Murphy G, Wells A, et al. (2016) Treatment outcome and metacognitive change in CBT and GET for Chronic Fatigue Syndrome. Behavioural and Cognitive Psychotherapy 44: 397–409.
- Field A (2005) Discovering Statistics Using SPSS. London: SAGE.
- Fukuda K, Straus SE, Hickie I, et al. (1994) The chronic fatigue syndrome: A comprehensive approach to its definition and study. Annals of International Medicine 121: 953–959.
- Garnefski N, Kraaij V (2006) Relationships between cognitive emotion regulation strategies and depressive symptoms: A comparative study of five specific samples. Personality and Individual Differences 40: 1659–1669.
- Garnefski N, Kraaij V (2007) The Cognitive Emotion Regulation Questionnaire: Psychometric features and prospective relationships with depression and anxiety in adults. European Journal of Psychological Assessment 23: 141–149.
- Garnefski N, Kraaij V (2009) Cognitive coping and psychological adjustment in different types of stressful life events. Individual Differences Research 7: 168–181.
- Garnefski N, Kraaij V, Spinhoven P (2001) Negative life events, cognitive emotion regulation and emotional problems. Personality and Individual Differences 30: 1311–1327.
- Garnefski N, Kraaij V, Spinhoven P (2002) CERQ: Manual for the Use of the Cognitive Emotion Regulation Questionnaire: A Questionnaire for Measuring Cognitive Coping Strategies. Leiderdorp: DATEC V.O.F.
- Heijmans MJWM (1998) Coping and adaptive outcome in Chronic Fatigue Syndrome: Importance of illness cognitions. Journal of Psychosomatic Research 45: 39–51.
- McInnis OA, Matheson K, Anisman H (2014) Living with the unexplained: Coping, distress, and depression among women with chronic fatigue syndrome and/or fibromyalgia compared to an autoimmune disorder. Anxiety, Stress, & Coping 27: 601–618.
- Pinksterhuis I, Strand EB, Stormorken E, et al. (2015) From chaos and insecurity to understanding and coping: Experienced benefits of a group-based education programme for people with chronic fatigue syndrome. British Journal of Guidance & Counselling 43: 463–475.
- Ray C, Jefferies S, Weir WRC (1995) Coping with chronic fatigue syndrome: Illness responses and their relationship with fatigue, functional impairment and emotional status. Psychological Medicine 25: 937–945.
- Spinhoven P, Ormel J, Sloekers PPA, et al. (1997) A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychological Medicine 27: 363–370.
- Tabachnick BG, Fidell LS (1996) Using Multivariate Statistics (3rd edn). New York: HarperCollins Publishers.
- Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica 67: 361–370.