Introduction
Diagnoses of sexually transmitted infections (STIs) have been steadily increasing in England since 2016. Public Health England (PHE) recorded 423,100 STI diagnoses in 2016, which increased by 0.3% in 2017, 5% in 2018, and 5% in 2019 before a 32% decrease in 2020 owing to the COVID-19 pandemic. Current public health guidelines by the National Institute for Health and Care Excellence (NICE) for HIV and STI management emphasize frequent sexual health screening in conjunction with condom use. For the periods 2015 to 2019, there was an overall 23% increase in the number of sexual health consultations and a 31% increase in sexual health screens in England. Despite the consistent increase in demand for consultations and screening, sexual health services (SHS) have continued to operate with reduced budgets since 2016, leading to a reduction of services offered at clinics, staffing, and outreach activities. Additionally, PHE reported approximately 2 million sexual health screens were conducted from a total of 3.3 million attendances in 2017. Although the nature of the remaining 1.3 million visits is unclear, research has shown that high anxiety around sexual health prompts individuals to access repeat testing despite low-risk behavior and previous negative results.
Consultations between 2019 and 2020 reflected a unique situation due in part to the COVID-19 pandemic and lockdowns faced across the United Kingdom. During this period consultations decreased by 10% (from 3,853,387 to 3,482,700). Face-to-face consultations decreased by 35% but remained the most common method of contact between patients and SHS. However, stemming from the need for innovation in delivering services, telehealth and e-health methods became much more popular with telephone consultations increasing fivefold and internet consultations increasing twofold.,
Sexual Health Anxiety
Health anxiety refers to a range of illness-related anxiety characterized by a general worry about illness or pain persisting for less than 6 months and ranges from mild concern and worry to clinical hypochondriasis. A review of 12 studies estimated that health anxiety is found in approximately 2.1% to 13.1% of the population and is commonly treated using cognitive behavioral therapy (CBT).- Additionally, a recent systematic review of students in Western countries between 1985 and 2017 noted an increase in reported health anxiety.
Early research around sexual health anxiety (SHA) began in response to the psychological impact of the HIV/AIDS epidemic and was then referred to as “AIDS anxiety.”, AIDS anxiety was characterized by beliefs that one is dying of AIDS, obsessional thinking about AIDS, requests for repeated HIV testing despite low-risk behavior and previous negative results, and psychological symptoms including acute panic attacks, generalized anxiety, hypochondriasis, and somatic presentation. On the basis of the existing research at the time, Finney and Snell developed the Multidimensional AIDS Anxiety Questionnaire (MAAQ) to assess AIDS anxiety and were able to isolate 5 subscales at the physiological, cognitive, and behavioral levels. Since then, both the MAAQ and its isolated subscales have been used to measure AIDS anxiety- and the perceived fear of AIDS,- as well as more recently being adapted to measure the fear of COVID-19.- The physiological level was made up of the physiological arousal and fear of AIDS subscales; the emotional level consisted of cognitive worry, and the behavioral level consisted of sexual inhibition and discussion inhibition.
On the basis of the lack of current research on the topic, we decided to repurpose the term AIDS anxiety into SHA with a focus on STIs instead of AIDS. Among those who suffer from SHA are the “worried well”—individuals who believed themselves to have symptoms of HIV infection despite repeated serological testing confirming their negative status. Miller et al distinguished the worried well from those with general anxiety because of the increased HIV-related media by the reduction in anxiety in the latter group upon negative clinical and laboratory findings. As levels of anxiety and the number of worried well patients increased, healthcare professionals began experiencing increased levels of burnout and emotional distress, as well as a lack of available resources and funds required to address the concerns of their patients., Existing research has supported this claim and found that severe cases of health anxiety can require as much as 80% more resources than defined medical conditions.-
Digital Sexual Health Services
Digital sexual health services (DSHS) refer to any service delivered via technologies, such as smartphones, websites, and text messages. Some studies focus on the use of DSHS in children and young adults, but studies with adult samples are less common. Despite this gap in knowledge, a recent study by Nadarzynski et al found that acceptability for webchat and video consultations sexual health advice was moderate to high among a sample of adults in Hampshire, United Kingdom. Additionally, Burns et al reviewed 10 randomized controlled trials with samples ranging from 16 to 70 years using SMS messages and videos and identified an increased uptake of SHS and promising increases in condom use from 1 trial. More recently, Karim et al reviewed 9 studies focusing on adults with chronic diseases and found that mobile health applications had a positive effect on sexual health outcomes, such as sexual functioning and satisfaction.
The increasing number of STI diagnoses in the years before COVID-19 and the increase in SHS use placed a burden on healthcare professionals. As COVID-19 pushed services online, sexual healthcare professionals noted that DSHS increased patient access, service quality, facilitated more time with service users presenting with symptoms, and improved managing demand and clinical workflow. SHA and increased repeat testing have been known to contribute to this burden on healthcare workers., Previous research has linked health anxiety with age,- a more conscientious personality, a recent experience of illness (eg, HIV and myocardial infarction),,- poor mental health or obsessive-compulsive thoughts,- a history of alcohol or drug use,, high-risk perception of disease (eg, STIs),,, or engaging in high-risk behavior, such as having multiple casual partners or unprotected sex., Therefore, this study aimed to investigate the level of SHA among internet users in England and examine its predictors, as well as to identify preferences for DSHS. The findings of the survey will inform the guidelines around the provision of DSHS for people with increased levels of SHA.
Method
Design
The study used an exploratory cross-sectional design, incorporating an online survey engine to assess the level of SHA in a sample of internet users and to understand their preferences for DSHS. Ethical approval for the study was obtained from the University of Westminster.
Participants and Recruitment
Data collection took place between May 2019 and January 2020. All individuals aged 18 years and above living in England were eligible to take part in the survey. There were no specific exclusion criteria. The survey was voluntary, and participants had the right to withdraw at any time.
The study was advertised on social media websites (ie., Facebook, Twitter, Tumblr, and Reddit) using convenience and snowball sampling approaches with a focus on internet users. The study advertisement invited participants to complete the survey on anxiety about STIs and views about developing digital resources to help reduce this anxiety via a Qualtrics link in the advertisement. Participants were offered an entry to a prize draw worth £75 as an incentive. Because of the snowball sampling approach, we were unable to estimate a response rate.
Procedure
Upon accessing the survey on the social media advertisement, participants were directed to a page that described the study, including its target population (18 years and older living in England), and were asked to tick a box agreeing that they met the criteria of the study and consented to participate in the study. Data were collected using an online Qualtrics survey that took no more than 15 minutes. At the end of the survey, participants were presented with a debriefing page that explained the study and given the option to submit their email addresses for a chance to be included in a raffle giveaway.
Measures
The survey consisted of 6 sections and collected demographic information, recent contact with healthcare services, sexual health, personality, mental health, and substance use. Demographic data consisted of age, gender identity, preference of sexual partner, highest educational qualification, and ethnicity. Recent exposure to healthcare services consisted of 2 questions that asked how many times the participant had visited healthcare services, such as a general practitioner and sexual healthcare services, respectively, in the last 12 months.
The second section collected data on sexual health. Items included asked participants about who they usually had sex with, condom use, SHS use in the last 12 months, how many sexual partners they had had in the last 12 months, whether they had previously been diagnosed with an STI, their risk perception of STIs, how often they worried about STIs, SHA, and data around DSHS and their preferences for use. SHA was measured using an adjusted version of the MAAQ,, where all references to HIV were changed to STIs to reflect the nature of the current study. The modified MAAQ consisted of 48 items and measured 5 dimensions of SHA that corresponded to physiological (physiological arousal and fear of STIs), cognitive (cognitive worry), and behavioral (sexual inhibition and discussion inhibition) aspects of anxiety. Items were measured on a 5-point scale, where 1 was “not at all characteristic of me” and 5 was “very characteristic of me.” The Cronbach alpha for the composite MAAQ was 0.97, and values for the subscales were 0.96 (physiological arousal), 0.89 (fear of STIs), 0.94 (cognitive worry), 0.92 (sexual inhibition), and 0.9 (discussion inhibition).
DSHS included items on the digital services they were most likely and least likely to use to learn about sexual health, preferences for intervention, how important it was to talk to a health professional about their health, how important it was to talk to a friend or family member about their health, and how important it was to discuss their health with a health professional face to face. Preferences for intervention were measured by 11-items developed by the authors on a 5-point scale from 1 (strongly agree) to 5 (strongly disagree). Some examples included “I always prefer to talk face-to-face about my sexual health,” and “I would use an online/home-testing kit if recommended by a sexual health advisor.” All 3 items measuring the importance of discussing with a health professional, friend or family member, and discussing face-to-face were measured on a 5-point scale from 1 (very important) to 5 (not important).
Personality was measured using the Ten-Item Personality Inventory (TIPI). The TIPI measures 5 domains of personality according to the Big Five Inventory using a 7-point scale, where 1 denotes “strongly disagree” and 7 denotes “strongly agree.” However, only data for conscientiousness were included in the analysis based on the previous research. The Cronbach alpha for the conscientiousness subscale was 0.59.
The measured mental health constructs were depression, anxiety, and obsessive-compulsive behavior (OCB). The 21-item Depression, Anxiety, Stress Scale (DASS-21) was used to measure depression and anxiety using their respective subscales. The 14 items used a 4-point scale, where 0 indicated “did not apply to me at all” and 3 denoted “applied to me very much or most of the time.” The Cronbach alphas for depression and anxiety were 0.94 and 0.86, respectively. OCB was measured using the Obsessive-Compulsive Inventory-Revised (OCI-R) and the Cronbach alpha was 0.92. The OCI-R consists of 18 items on a 5-point scale that ranged from 0 (not at all) to 4 (extremely).
Finally, substance use was measured using the Brief Substance Use Screening Questionnaire (BSUSQ). The BSUSQ consists of 5 items that measured tobacco use, alcohol use, illegal drug use, nonmedical prescription drug use, and recreational prescription drug use in the past year on a 4-point scale ranging from 1 (never) to 4 (frequently).
Data Screening and Analysis
Data were processed and analyzed using IBM SPSS version 24. Responses on the MAAQ were screened to preserve data quality before analysis. The number of missing responses was calculated for each participant. Two participants were removed for having omitted 31 (65%) and 43 items (90%) of the MAAQ. Straight-lining was investigated by calculating the variance for each participant’s responses, with a score of 0 indicating possible straight-lining. Four participants were found to have a score of 0. One participant scored a variance of 0.02 and was found to have answered 1 item before potentially straight-lining the remaining items. All 5 participants were removed. Following these checks, 138 responses remained of the initial 145 recorded indicating a completion rate of 95%.
SHA was calculated as a composite score of all MAAQ items, as well as individual scores for each subscale as outlined by. A previous STI diagnosis was dichotomized (yes or no), and responses of “I don’t know” were coded as missing. Risk perception scores were also recoded into “below average,” “average,” and “above average.”
A multiple regression analysis with general SHA as the outcome was run using age, recent exposure to SHS, depression, anxiety, OCB, conscientiousness, previous STI diagnosis, alcohol use, illegal drug use, risk perception, number of sexual partners, and condom use as predictors. Multicollinearity analyses were run simultaneously, and variance inflation factor (VIF) scores equal to or greater than 3 were considered to have violated this assumption. Further multiple regression analyses were carried out using the same set of predictor variables and each SHA subscale to determine significant predictors.
Results
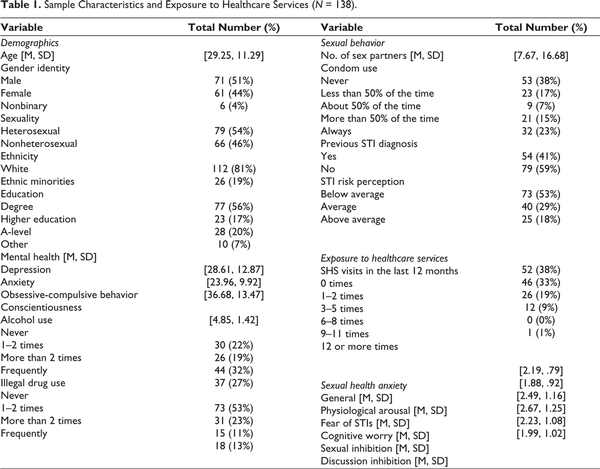
There were 138 complete responses to the survey. Descriptive data were presented in Table 1. The sample ranged from ages 18 to 67 (M = 29.25, SD = 11.29) and was mostly male (51%), White (81%), and educated to the degree level or higher (56%). Mean levels of both depression (M = 28.61, SD = 12.87) and anxiety (M = 23.96, SD = 9.92) scored within the severe category on the DASS-21 and the mean score for OCB in the sample was 36.68 (SD = 13.47). The majority of the sample had never done illegal drugs in the past year (53%); however, one-third of the sample (32%) had consumed more than 4 to 5 drinks a day on more than 2 occasions within the same period.
Participants had an average of 8 sex partners in the past year (M = 7.67, SD = 16.68), with 59% of the sample never having been previously diagnosed with an STI. More than half of the sample (53%) perceived their risk of STIs as below average but worried about their sexual health several times a year (29%). The average overall SHA in the sample was mild (M = 2.19, SD = 0.79), with average scores in the subscales ranging from low to moderate. In order of most anxious to least anxious, mean scores for the subscales were cognitive worry (M = 2.67, SD = 1.25), fear of STIs (M = 2.49, SD = 1.16), sexual inhibition (M = 2.23, SD = 1.08), discussion inhibition (M = 1.99, SD = 1.02), and physiological arousal (M = 1.88, SD = 0.92).
Predictors of Sexual Health Anxiety
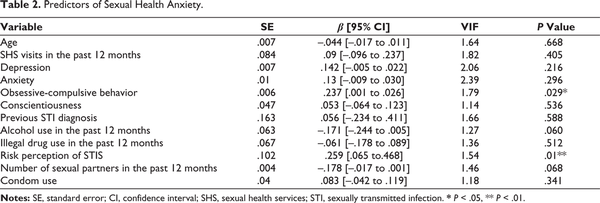
A multiple regression analysis was carried out using age, recent exposure to SHS, depression, anxiety, OCB, conscientiousness, a previous STI diagnosis, alcohol use, illegal drug use, risk perception, number of sexual partners, and condom use and general SHA scores. Correlates and their beta weights are reported in Table 2. The model predicting general SHA was significant (R2 = 0.29, F(12, 112) = 3.76, P≤.001) and predicted 29% of the variance. Higher general SHA was predicted by a higher frequency of OCB and a greater risk perception of STIs.
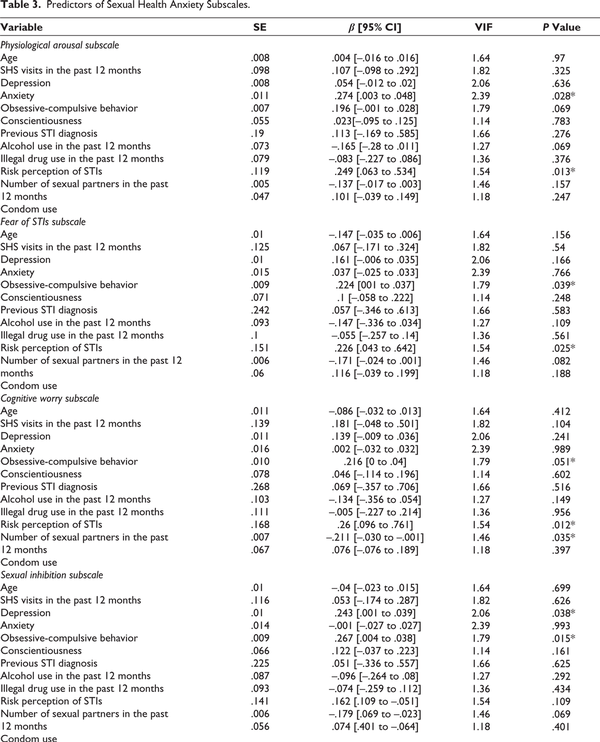
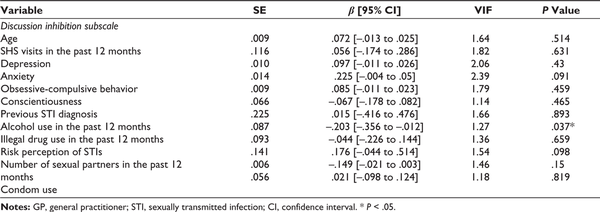
When considering the subscales of SHA, multiple regression models were conducted using the previously identified predictors and SHA subscales. Findings are reported in Table 3. All 5 regression models were significant (P ≤ .001). The model predicted 29% of the variance for physiological arousal (R2 = 0.29, F[12, 112] = 3.74, P ≤ .001), and higher scores were significantly predicted by higher scores in anxiety and a greater risk perception of STIs. Twenty-eight percent of the variance for fear of STIs was predicted by the model (R2 = 0.28, F[12, 112] = 3.54, P = .000). Like general SHA, fear of STIs was predicted by OCB and a greater risk perception of STIs. Twenty-five percent of the variance for cognitive worry was predicted (R2 = 0.25, F[12, 112] = 3.07, P = .001). Both greater risk perception and fewer sex partners in the past year predicted cognitive worry. The model predicted 27% of the variance for sexual inhibition (R2 = 0.27, F[12, 112] = 3.45, P = .000), and high scores were significantly predicted by high scores in depression and a higher frequency of OCB. Finally, the model predicted 19% of the variance for discussion inhibition (R2 = 0.19, F[12, 112] = 2.12, P = .021). Less frequent alcohol use was the only significant predictor of high scores in discussion inhibition.
Opinions on Digital Sexual Health Services
Figure 1 outlines preferences for digital advice platforms for sexual health information with the least preferred being Skype/video consultations (N = 70), social media (N = 64), chatbots or virtual assistants (N = 56), and email groups (N = 55). However, National Health Service websites were the most popular choice for information (N = 100), followed by other websites (N = 62) and online/home-testing kits (N = 48).
Opinions on DSHS were positive (see Figure 2). Seventy-five percent of the sample agreed that DSHS were useful and 86% would use an online/home-testing kit if recommended by a sexual health advisor. Acceptability of online forms for appropriate SHS and the need for STI screening were also positive (77% and 73%, respectively). However, more than half of the sample still preferred to talk to someone about their sexual health (55%) and have face-to-face conversations about their sexual health (52%). Finally, 34% of participants disagreed with the statement that “Only doctors at the clinic can make me feel less anxious about my sexual health” compared with 36% who agreed.
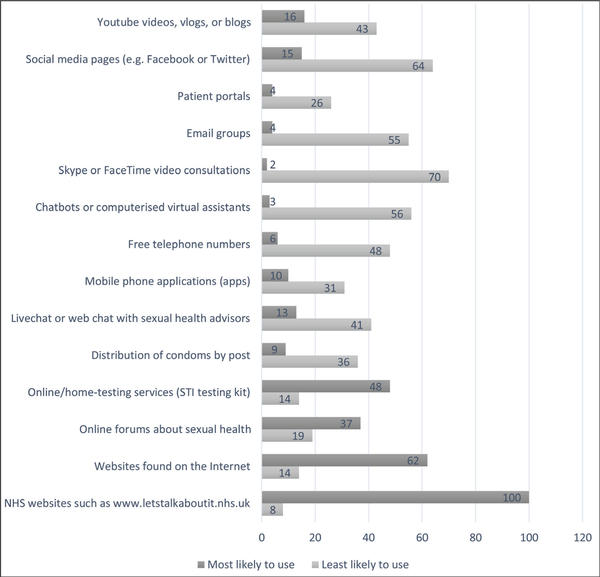
Preferred Digital Sources of Sexual Health Information.
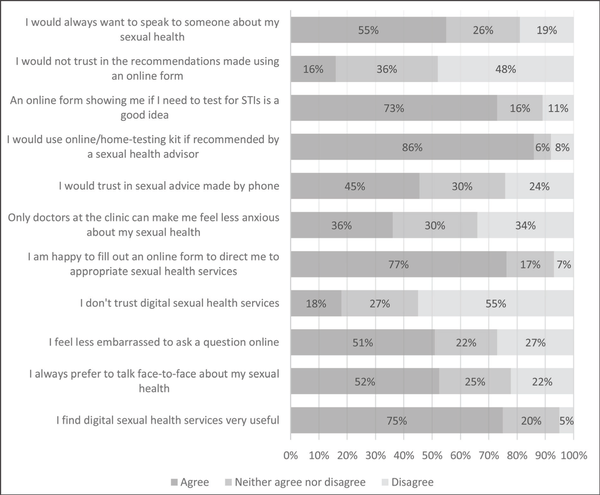
Preferences for Digital Sexual Health Interventions.
Discussion
To our knowledge, this was the first study to investigate SHA in the English population. Cognitive worry about STIs carried the greatest anxiety followed by fear of STIs. Avoiding sexual contact, avoiding discussions around STIs, and physiological arousal around STIs followed in that order. As such, this study began a body of research on SHA in the contemporary sexual health climate where the rate of STIs has been steadily increasing. In addition, this study further adds to the existing body of research on the “worried well” and has the potential to inform staff in sexual and reproductive health services about this under-researched population. The findings may inform patient-healthcare professional communication around sexual health and the associated anxiety as a large number of consultations because the COVID-19 pandemic are conducted digitally.
To our knowledge, this was the first study to investigate SHA using the adapted MAAQ, and therefore, investigated the 5 subtypes of AIDS anxiety in relation to STIs. We found that cognitive worry was highest followed by fear of STIs, sexual inhibition, discussion inhibition, and physiological arousal. This suggests that SHA may have had the greatest impact on the sample cognitively, and future interventions aimed at reducing SHA should focus on changing patterns of maladaptive beliefs, cognitions, and attitudes. Currently, CBT is the most common treatment for health anxiety. Our findings suggest that it may be helpful in also treating SHA, but further research is required.
Our findings demonstrated that participants who perceived themselves at a greater risk of STIs and experienced more severe symptoms of OCB were more likely to have higher SHA. These findings are consistent with previous studies that have focused on HIV or general health,,- and indicate that additional screening may be necessary to identify sexual health patients within these groups as they may require specific attention and education around STIs. Psychoeducation in particular is key to promoting positive sexual health in these populations.-
In addressing SHA, and moving beyond CBT, it may be useful to explore ways in which OCB and cognitive worry are the result of deeper underlying scripts or linked to issues triggered by external factors. Sexual scripts, for example, tend to be shaped by sociocultural norms (eg, religion), which inform what is considered normal and what is not. Future research could investigate whether sexual scripts may contribute to the way individuals perceive their risk of STIs and, ultimately, influence their levels of SHA. We propose applying the biopsychosocial model to the study of SHA. The model is readily used in health-related settings (eg, Friedman & Adler) and aligns with Finney and Snell’s classification of SHA into physiological, cognitive, and behavioral components.
There were two overlapping predictors among the MAAQ subscales. Like general SHA, more severe OCB significantly predicted greater fear of STIs and sexual inhibition. OCB has been associated with health anxiety in the past,- but a study by Abramowitz et al found that patients with obsessive-compulsive disorder did not score particularly high on health anxiety. This discrepancy could be an issue with measurement as Abramowitz et al measured health anxiety using a different instrument to the MAAQ. Therefore, we suggest further research into SHA using the MAAQ to build a knowledge base for comparison. Secondly, a greater risk perception of STIs significantly predicted higher scores in physiological arousal, fear of STIs, and cognitive worry. A systematic review of psychological and behavioral correlates of HIV risk perception found that psychological factors were rarely assessed, but cases where they were included found them to be related to participants’ risk perception. For example, a study by Price et al found that adolescent girls and young women in sub-Saharan Africa were more likely to worry about HIV when they reported higher risk factors such as having more sexual partners.
Digital Sexual Health Services
Our findings around DSHS indicate that the sample agreed that DSHS were a useful method of service delivery. This is because of the majority of positive responses to questions such as “An online form showing me if I need to test for STIs is a good idea,” “I am happy to fill out an online form to direct me to appropriate sexual health services,” and “I find digital health services very useful.” However, responses for the item “Only doctors at the clinic can make me feel less anxious about my sexual health” were equally distributed among those who agreed, disagreed, and were neutral, while the majority of responses to items such as “I would always want to speak to someone about my sexual health” and “I always prefer to talk face-to-face about my sexual health” were also positive. These findings demonstrate that despite the acceptance of DSHS, participants show a strong preference for face-to-face interactions around sexual health. As such, future research should develop a screening questionnaire that will identify individuals who require face-to-face intervention.
Limitations
There are a few limitations to this study. First, data were collected before the COVID-19 pandemic, and hence participants’ responses may have changed since the pandemic forced SHS online. Second, the study adapted the MAAQ, a scale used to measure AIDS anxiety, to measure the level of anxiety toward STIs. As a result, the scale may not be an accurate measure of SHA owing to the difference between the way people think about HIV and STIs. Finally, there are some limitations around the external validity of the sample, such as its size and demographic representation of the wider population. Our sample was recruited via a self-referred internet-based survey on sexual health that was prone to low response rates as noted over the last few decades and may have attracted individuals who are invested in or already have existing beliefs of SHS. It is also possible that these individuals may have differing opinions when compared to clinical or general populations. Additionally, mean scores on each of the mental health measures were high compared to what is expected of the general population, further limiting the external validity of the sample. It is not clear whether these high scores reflect genuine problems experienced by participants, or whether they arise because scores derived from online questionnaires may appear elevated when compared to norms derived from paper-and-pencil questionnaires.
In conclusion, SHA was predicted by participants’ STI risk perceptions and higher frequencies of OCB. There was some overlap between the predictors of subtypes of SHA, but further research is needed. Despite mild levels of SHA in the sample, the acceptance of DSHS was high; however, preferences for SHS leaned heavily toward face-to-face and in-person interactions.
Declaration of Conflicting Interests The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical Approval Ethical approval for the study was obtained from the University of Westminster Ethics Committee.
Funding The authors received no financial support for the research, authorship and/or publication of this article.
Informed Consent The participants have consented to the submission of the article to the journal.
References
- 1. Public Health England. National STI surveillance data tables 2020 – Table 1. Public Health England. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1056729/2020_Table_1_New_STI_diagnoses_and_rates_in_England_by_gender_updated.ods
- 2. Public Health England. Sexually transmitted infections and screening for chlamydia in England 2020. Public Health England; 2020. https://webarchive.nationalarchives.gov.uk/ukgwa/20220913171016mp_/https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1015176/STI_NCSP_report_2020.pdf
- 3. National Institute for Health and Care Excellence. Sexual health. https://www.nice.org.uk/guidance/qs178
- 4. Public Health England. Sexually transmitted infections and screening for chlamydia in England 2019. Public Health England; 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/914249/STI_NCSP_report_2019.pdf
- 5. Iacobucci G, Torjesen I. Cuts to sexual health services are putting patients at risk, says King’s Fund. BMJ. 2017;356:j1328. doi: 10.1136/bmj.j1328.
- 6. Public Health England. Sexually transmitted infections and screening for chlamydia in England, 2017. Public Health England; 2017. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/713944/hpr2018_AA-STIs_v5.pdf
- 7. Morin SF, Batchelor WF. Responding to the psychological crisis of AIDS. Public Health Rep. 1984;99(1):4–9.
- 8. Lunt A, Llewellyn C, Bayley J, Nadarzynski T. Sexual healthcare professionals’ views on the rapid provision of remote services at the beginning of COVID-19 pandemic: a mixed-methods study. Int J StD AIDS. 2021;32(12):1138–1148. doi: 10.1177/09564624211023018
- 9. Public Health England. The impact of the COVID-19 pandemic on prevention, testing, diagnosis and care for sexually transmitted infections, HIV, and viral hepatitis in England. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/943657/Impact_of_COVID-19_Report_2020.pdf
- 10. Weck F, Richtberg S, Neng J. Epidemiology of hypochondriasis and health anxiety: comparison of different diagnostic criteria. Curr Psychiatry Rev. 2014;10(1):14–23. doi: 10.2174/1573400509666131119004444
- 11. Cooper K, Gregory JD, Walker I, Lambe S, Salkovskis PM. Cognitive behaviour therapy for health anxiety: a systematic review and meta-analysis. Behav Cogn Psychother. 2017;45(2):110–123. doi: 10.1017/S1352465816000527
- 12. Kosic A, Lindholm P, Järvholm K, Hedman-Lagerlöf E, Axelsson E. Three decades of increase in health anxiety: systematic review and meta-analysis of birth cohort changes in university student samples from 1985 to 2017. J Anxiety Disord. 2020;71:102208. doi: 10.1016/j.janxdis.2020.102208
- 13. Sonnex C, Petherick A, Adler MW, Miller D. HIV infection: increase in public awareness and anxiety. BMJ. 1987;295(6591):193–195. doi: 10.1136/bmj.295.6591.193
- 14. Finney PD, Snell WE. The AIDS anxiety scale: components and correlates. Paper presented at: Annual Meeting of the Southwestern Psychological Association; July 23, 1993; Houston, TX. Accessed , . https://www.researchgate.net/profile/William-Snell-4/publication/284306199_The_Multidimensional_AIDS_Anxiety_Questionnaire/links/570527ef08ae13eb88b93f9a/The-Multidimensional-AIDS-Anxiety-Questionnaire
- 15. Falaye O, Afolayan JA. Psychotherapy and disclosure of sero status. Sky J Med Med Sci. 2015;3(5):56–62. http://www.skyjournals.org/sjmms/pdf/2015pdf/Jul/Falaye%20and%20Afolayan%20pdf.pdf
- 16. Afolayan JA, Ajibola OF. Use of self-management techniques and transactional analysis to enhance self disclosure of HIV positive status in Kwara State, Nigeria. J Psychol. 2010;1(1):55–63. doi: 10.1080/09764224.2010.11885446
- 17. Lefkowitz ES, Boone TL, Shearer CL. Communication with best friends about sex-related topics during emerging adulthood. J Youth Adolesc. 2004;33(4):339–351. doi: 10.1023/B:JOYO.0000032642.27242.c1
- 18. Espinosa-Hernández G, Lefkowitz ES. Sexual behaviors and attitudes and ethnic identity during college. J Sex Res. 2009;46(5):471–482. doi: 10.1080/00224490902829616
- 19. Lam CB, Lefkowitz ES. Risky sexual behaviors in emerging adults: longitudinal changes and within-person variations. Arch Sex Behav. 2013;42(4):523–532. doi: 10.1007/s10508-012-9959-x
- 20. Boone TL, Duran A. Sexual prejudice among heterosexual college men as a predictor of condom attitudes. Sex Roles. 2009;61(3-4):167–177. doi: 10.1007/s11199-009-9626-4
- 21. Ojedokun O, Idemudia ES, Kute VO. Burnout and fear of contagion as factors in aggressive tendency of health-care workers treating people with Aids. Soc Behav Pers. 2013;41(10):1625–1634. doi: 10.2224/sbp.2013.41.10.1625
- 22. Bolatov AK, Seisembekov TZ, Askarova AZh, Baikanova RK, Smailova DS, Fabbro E. Online-learning due to COVID-19 improved mental health among medical students. Med Sci Educ. 2021;31(1):183–192. doi: 10.1007/s40670-020-01165-y
- 23. Zammitti A, Imbrogliera C, Russo A, Zarbo R, Magnano P. The psychological impact of Coronavirus pandemic restrictions in Italy. The mediating role of the fear of COVID-19 in the relationship between positive and negative affect with positive and negative outcomes. Eur J Invest Health Psychol Educ. 2021;11(3):697–710. doi: 10.3390/ejihpe11030050
- 24. Miller D, Acton TM, Hedge B. The worried well: their identification and management. J R Coll Physicians Lond. 1988;22(3):158–165.
- 25. Wagner PJ, Curran P. Health beliefs and physician identified “worried well.” Health Psychol. 1984;3(5):459–474. doi: 10.1037/0278-6133.3.5.459
- 26. Barsky AJ, Orav EJ, Bates DW. Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Arch Gen Psychiatry. 2005;62(8):903. doi: 10.1001/archpsyc.62.8.903
- 27. Fink P, Ørnbøl E, Christensen KS. The outcome of health anxiety in primary care. A two-year follow-up study on health care costs and self-rated health. PLoS One. 2010;5(3):e9873. doi: 10.1371/journal.pone.0009873
- 28. Tyrer P. Recent advances in the understanding and treatment of health anxiety. Curr Psychiatry Rep. 2018;20(7):49. doi: 10.1007/s11920-018-0912-0
- 29. Murray E, Hekler EB, Andersson G, . Evaluating digital health interventions. Am J Prev Med. 2016;51(5):843–851. doi: 10.1016/j.amepre.2016.06.008
- 30. Nadarzynski T, Bayley J, Llewellyn C, Kidsley S, Graham CA. Acceptability of artificial intelligence (AI)-enabled chatbots, video consultations and live webchats as online platforms for sexual health advice. BMJ Sex Reprod Health. 2020;46(3):210–217. doi: 10.1136/bmjsrh-2018-200271
- 31. Burns K, Keating P, Free C. A systematic review of randomised control trials of sexual health interventions delivered by mobile technologies. BMC Public Health. 2016;16(1):778. doi: 10.1186/s12889-016-3408-z
- 32. Karim H, Choobineh H, Kheradbin N, Ravandi MH, Naserpor A, Safdari R. Mobile health applications for improving the sexual health outcomes among adults with chronic diseases: a systematic review. Digital Health. 2020;6:205520762090695. doi: 10.1177/2055207620906956
- 33. Fisher JD, Del Gado BP, Melchreit R, Spurlock-McLendon J. The dynamics of repeat HIV testing, and interventions for repeat HIV testers. AIDS Behav. 2002;6(2):183–191. doi: 10.1023/A:1015405416826
- 34. Gerolimatos LA, Edelstein BA. Predictors of health anxiety among older and young adults. Int Psychogeriatr. 2012;24(12):1998–2008. doi: 10.1017/S1041610212001329
- 35. Norton J, Elford J, Sherr L, Miller R, Johnson MA. Repeat HIV testers at a London same-day testing clinic. AIDS. 1997;11(6):773–781. https://europepmc.org/article/med/9143610
- 36. Salkovskis PM, Warwick HMC. Morbid preoccupations, health anxiety and reassurance: a cognitive-behavioural approach to hypochondriasis. Behav Res Ther. 1986;24(5):597–602. doi: 10.1016/0005-7967(86)90041-0
- 37. López-Solà C, Bui M, Hopper JL, . Predictors and consequences of health anxiety symptoms: a novel twin modeling study. Acta Psychiatr Scand. 2018;137(3):241–251. doi: 10.1111/acps.12850
- 38. Marinho M, Covelo V, Marques J, Bragança M. HIV/AIDS “worried well”—When the “virus” leads to a significant illness, even in its absence. Eur Psychiatr. 2017;41(S1):S237. doi: 10.1016/j.eurpsy.2017.01.2256
- 39. Phillips KA, Paul J, Kegeles S, Stall R, Hoff C, Coates TJ. Predictors of repeat HIV testing among gay and bisexual men. AIDS. 1995;9(7):769–776. doi: 10.1097/00002030-199507000-00015
- 40. Snell WE, Finney PD. Multidimensional AIDS Anxiety Questionnaire. In Fishers TD, Davis CM, Yarber WL, Davis SL, eds. Handbook of Sexuality-Related Measures. 3rd ed. Routledge; 2011:378–380.
- 41. Gosling SD, Rentfrow PJ, Swann WB. A very brief measure of the Big-Five personality domains. J Res Pers. 2003;37(6):504–528. doi: 10.1016/S0092-6566(03)00046-1
- 42. John OP, Srivastava S. The Big-Five trait taxonomy: history, measurement, and theoretical perspectives. In: Pervin LA, John OP, eds. Handbook of Personality: Theory and Research. 2nd ed. Guilford Press; 1999:102-138.
- 43. Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the depression anxiety stress scales in clinical groups and a community sample. Psychol Assess. 1998;10(2):176–181. doi: 10.1037/1040-3590.10.2.176
- 44. Foa EB, Huppert JD, Leiberg S, . Obsessive–compulsive inventory—revised. Published online , 2011. doi: 10.1037/t01258-000
- 45. McNeely J, Halkitis PN, Horton A, Khan R, Gourevitch MN. Brief substance use screening questionnaire. Published online , 2016. doi: 10.1037/t45179-000
- 46. Higgins A, Barker P, Begley CM. Sexual health education for people with mental health problems: what can we learn from the literature? J Psychiatr Ment Health Nurs. 2006;13(6):687–697. doi: 10.1111/j.1365-2850.2006.01016.x
- 47. Pandor A, Kaltenthaler E, Higgins A, . Sexual health risk reduction interventions for people with severe mental illness: a systematic review. BMC Public Health. 2015;15(1):138. doi: 10.1186/s12889-015-1448-4
- 48. Simon W, Gagnon JH. Sexual scripts. In Aggleton P, Parker R, eds. Culture, Society and Sexuality. Routledge; 2007:47–56. doi: 10.4324/9780203966105-13
- 49. Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129–136. doi: 10.1126/science.847460
- 50. Friedman HS, Adler NE. The history and background of health psychology. In Friedman HS, Silver RC, eds. Foundations of Health Psychology. Oxford University Press; 2007:3–18.
- 51. Abramowitz JS, Olatunji BO, Deacon BJ. Health anxiety, hypochondriasis, and the anxiety disorders. Behav Ther. 2007;38(1):86–94. doi: 10.1016/j.beth.2006.05.001
- 52. Evangeli M, Baker LLE, Pady K, Jones B, Wroe AL. What leads some people to think they are HIV-positive before knowing their diagnosis? A systematic review of psychological and behavioural correlates of HIV-risk perception. AIDS Care. 2016;28(8):943–953. doi: 10.1080/09540121.2016.1139040
- 53. Price JT, Rosenberg NE, Vansia D, . Predictors of HIV, HIV risk perception, and HIV worry among adolescent girls and young women in Lilongwe, Malawi. J Acquir Immune Defic Syndr. 2018;77(1):53–63. doi: 10.1097/QAI.0000000000001567
- 54. Sammut R, Griscti O, Norman IJ. Strategies to improve response rates to web surveys: a literature review. Int J Nurs Stud. 2021;123:104058. doi: 10.1016/j.ijnurstu.2021.104058
- 55. Buchanan T. Personality testing on the Internet: what we know and what we do not. In Joinson AN, KcKenna KYA, Postmes T, Reips UD, eds. The Oxford Handbook of Internet Psychology. Oxford University Press; 2007:447–459.