INTRODUCTION
The 21st Century Cures Act (Cures Act) was enacted on December 13, 2016, to launch research in the development of medical products by innovative advances in the science of novel treatments for hard-to-treat diseases, e.g. cancer, addiction, and mental disorders. In this ambitious framework, digital health (DH) plays a critical role.
DH entails using information and communication technologies (ICT) in medicine and other health professions. DH applications aim to advance population wellness, enhance medical management, mitigate health risks, allow better health-care access, lower costs, and provide a venue to individualize the medicine based on each patient's comorbidities.[] DH involves various technologies, including wearable monitoring devices, mobile health, telehealth, health information technology, and telemedicine. The World Health Organization (WHO) provided DH technology guidelines in 2019. The WHO considers DH to involve all ICTs needed for health-care incorporation. DH includes applying sensors, mobile apps, social media, and location-sensing technologies to obtain wellness, diagnosis, prevention, and disease management data. In addition, DH has the potential to provide information to monitor and intervene when and where acute or chronic medical conditions require. With improved DH technologies and observations indicating clinical benefits, their integration within health-care systems is inevitable. However, while health-care systems are adopting these technologies, some challenges remain to overcome, e.g. enhancing patients’ confidence regarding their health information privacy.
The WHO guidelines focus on the population's health-related issues, including DH availability, quality, utilization rates, efficiency, cost, and accountability. In addition, critical evaluations of emerging DH-based interventions are needed to assess their benefits, harms, feasibility, and resource utilization. Enhancing DH literacy by including training programs for current and future health-care workers, including physicians, researchers, and scientists, remains essential. DH is considered a multidisciplinary field in which content experts in health care collaborate with engineers, economists, ethicists, legal experts, and computer and social scientists. While DH continues to expand, it is not entirely clear how and when it will be fully incorporated into health care and its ultimate capabilities and functions. The ever-growing prevalence of comorbid conditions has resulted in a drastic increase in health-care spending. In addition, the widespread use of smartphones in the community provides an opportunity to explore the DH capacities in advancing health care.
COGNITIVE-BEHAVIOR THERAPY
In each society, the factors with profound effects on the community and individual health are (1) lifestyles in general, (2) the genetic compositions, (3) environmental factors, (4) economic status, (5) the education levels, and (6) health-care performance. The interplay between these factors determines the health level. Among factors that impact lifestyles are “nonfunctional attitudes (nonfunctional attitudes are negative beliefs or actions, resulting from communication with others and developed by the individual toward themselves, other people and the world in which they live).” These attitudes include depression, anxiety, smoking, drug addiction, phobias and panic attacks, chronic insomnia, attention-deficit hyperactivity disorder (ADHD), and behavioral changes related to chronic diseases such as diabetes mellitus or hypertension. It is not only the major life events that create and maintain the psychological, emotional, and behavioral issues, but these also could be influenced by the individual cognitive structures and constructions. These factors create a close relationship between thoughts, emotions, and behaviors.
Psychopathologists can assess and interpret these behavioral issues through cognitive and behavioral therapies. They can identify the recurrent thoughts and dysfunctional reasoning patterns to replace and/or integrate nonfunctional attitudes with more functional beliefs. Cognitive-behavior therapy (CBT) is a reliable and effective model for understanding and treating psychopathological disorders. In CBT, cognitive aspects, i.e. thinking, reasoning, attention, and memory, with implications on the state of consciousness or awareness, and behavioral manifestations of these nonfunctional attitudes are targeted.[] The role of DH in CBT requires further exploration.
DIGITAL HEALTH AND MOBILE HEALTH
Medical devices
The European Parliament defines medical devices as any instrument, apparatus, application, software, implant, reagent, material, or other items manufactured and used alone or in combination for specific human medical needs.[] These needs could include diagnosis, prevention, monitoring, prognosis, treatment, disease severity alleviation, or study, replace, or modify anatomy or pathophysiologic processes. Medical devices could also obtain information with in vitro testing of human specimens, including organs, blood, or donated tissues.
Smart wearable technology
The role of smart wearable technology is growing in clinical medicine, health care, health management, workplaces, education, and scientific research. These medical devices can collect real-time human activity and behavioral information. Unlike traditional wearables, e.g. wristwatches and clothes, smart wearables can collect information and carry the Internet of things (IoT) [Figure 1],[] through which interconnecting physical objects and computing data create domain-specific intelligence[] (Inside wearables: How the science of human behavior change offers the secret to long-term. Endeavour Partners, 2017, [https://medium.com/endeavourprtnrs/inside-wearable-how-the–science-of-human-behavior-change-offers-the-secret-to-long-term-engagement]). While smart wearables could provide important services, many consumers do not regularly use them, decreasing the device's capacity to collect and process information. Conversations with patients to set goals with clear plans to achieve them, accompanied by a joint review of the data, could improve their compliance.[] In a large-scale systematic review, Noah et al. found no significant improvement in body mass index (−0.73; 95% confidence interval [CI]: −1.84, 0.38), weight (−1.29; 95% CI: −3.06, 0.48), waist circumference (−2.41; 95% CI: −5.16, 0.34), body fat percentage (0.11; 95% CI: −1.56, 1.34), systolic blood pressure (−2.62; 95% CI: −5.31, 0.06), and diastolic blood pressure (−0.99; 95% CI: −2.73, 0.74) after using smart wearable devices.[] They also highlighted that health behavior models and personalized coaching were associated with the highest success. The authors highlight substantial knowledge gaps in the evidence-based science regarding smart wearable implementation.
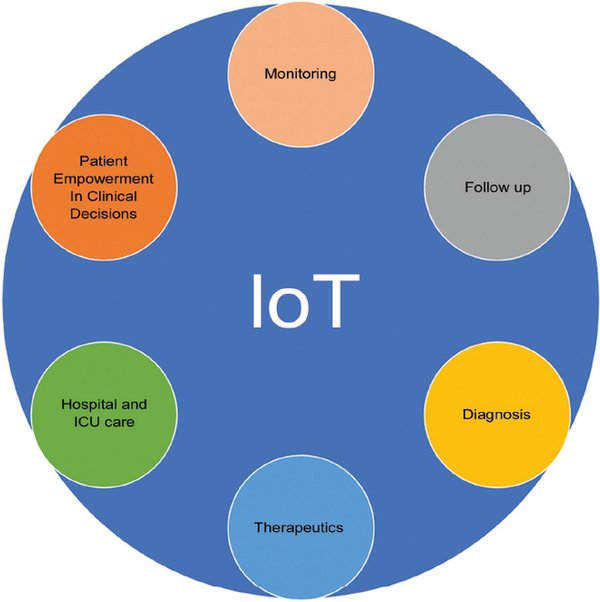
Figure 1.
The primary components of Internet of Things (IoT)
Internet of things
By measuring daily behaviors and other variables and communicating the information over the Internet, smartphones qualify for the definition IoT [Figure 1].[,] For example, smartphones and smartwatches can measure heart rate[] (Apple Watch Series 4 [https://www.apple.com/apple-watch-series-4/) and identify the presence of atrial fibrillation (AliveCor.KardiaMobile [https://www.alivecor.com/]). Several studies indicated these devices’ effectiveness in identifying atrial fibrillation.[,] Therefore, the food and drug administration (FDA) recognized this functionality, and in late March 2019, Europeans issued CE Marking for this application (CE marking indicates that a product has been assessed by the manufacturer and deemed to meet Europe safety, health and environmental protection requirements).
Another example of IoT [Figure 1] utilization in health care is the capsules taken by mouth to enter the stomach and emit signals[] to a wearable sensor patch. The FDA approved this technology in 2017 to monitor medication adherence. Specific sensors are also used to facilitate Parkinson's disease diagnosis and management at home.[]
Digital biomarkers
The digital biomarkers are physiological and behavioral measurements collected through portable, wearable, implantable, or digestible digital devices that characterize, influence, or predict health-related outcomes.[]
These biomarkers can be classified into those that indicate the possibility of development of a disease in a healthy individual (susceptibility), confirm the presence of a disease or suspected condition (diagnosis), measure the status of a disease or medical condition (monitoring), identify the possibility of a clinical event (prognostic), and assess the biological response of an individual receiving drug therapy (pharmacodynamic).[]
Digital diagnostics
Some medical conditions can be detected and managed with wearable and environmental sensors, mobile apps, social media, and location tracking technology.[] These devices provide early information regarding phases of disease development and progress.[,] Digital Diagnostics allow the collection of clinically relevant data to assess and assure patients’ physical well-being and improve diagnosis or early management of acute or chronic clinical conditions [Table 1]. The volume of the collected data is often substantial, and it can be used for machine learning and other artificial intelligence (AI) techniques to support medical decisions.[]
Table 1
Examples of digital diagnostics
| Examples |
|---|
| A smartphone app detects malaria utilizing blood from a finger stick |
| Using deep learning technology, one can interpret the retinal fundus images |
| Detection of depression and suicidal ideas |
| Detection of ASD in children |
| Smartphones and smart watches measure heart rate and identify the presence of atrial fibrillation |
| Capsules are taken by mouth to enter the stomach and emit signals to a wearable sensor patch |
| Facilitating Parkinson's disease diagnosis and management at home |
There are few fields in medicine using these devices for diagnostication. The research on Parkinson's disease using these devices focuses on early detection, tremor, body movement analysis, motor fluctuations (ON-OFF phases), and home and long-term monitoring. Another example is studies focused on children with autism spectrum disorder (ASD) with a lower social scenes preference than children without ASD. The eye-tracking and gaze measurement to assess social scenes is used for ASD screening. In an investigation on this topic, the authors demonstrated the ability of the algorithm to correctly differentiate visual preferences for social or abstract scenes (left or right side of the screen preference). The algorithm identified distractions and maintained high accuracy compared to manual assessment, with an error of only 1.52% compared with the gold standard.[] Another field benefiting from these devices is depression. Individuals’ voices contain features with useful information for the depression diagnosis. In a recent study, deep-learning tools based on neural networks were superior to handcrafted features in various areas.[]
Digital diagnostics are used for malaria as well. A simple smartphone app can detect malaria utilizing blood from a fingerstick. This diagnosis is made by a specific color only absorbed by malaria parasites. These smartphones use a small lens with 350-fold magnification power to capture cell count images using AI algorithms to identify different artifacts, including the malaria parasites within red blood cells. Then this information, along with the Global Positioning System-detected patient locations, is sent to healthcare centers to identify the malaria outbreak center. This can also generate a universal snapshot of malaria clusters globally.[]
Using deep learning technology to interpret the retinal fundus images is gaining momentum. For example, deep learning models to predict cardiovascular risk factors were trained and validated on retinal images of large cohorts of patients. These models used anatomical features, such as optic disc or blood vessels, to generate their prediction.[]
There are several challenges in the implementation of digital diagnostics. One of the major challenges in mobile health is the high rate of sensor and app usage abandonment.[] Several surveys indicate more than half of activity tracker users stop using their devices, and a third did so in the 1st 6 months (Inside wearables: how the science of human behavior change offers the secret to long-term. Endeavour Partners, 2017 [https://medium.com/@endeavourprtnrs]). Nevertheless, there are potential paths to improve device utilization. Enhancing patient communication to enhance patients’ understanding on the one hand and implementing shared decision-making strategies to change patients’ behaviors related to their diseases, on the other hand, could be considered effective strategies.
DIGITAL THERAPEUTICS
Behavioral and psychological factors can impact the efficacy of clinically validated medical care plans. Digital therapeutics are specialized software, e.g. apps, that can effectively and measurably guide a patient's progress toward improving outcomes [Table 2].[]
Table 2
Features of digital therapeutics and examples
| Features |
| They must be validated through randomized and controlled clinical trials |
| Algorithms compose the primary active ingredient of digital therapy |
| They must be subjected-when necessary for reimbursement-to assessments by HTA |
| They are reimbursed in some cases by public health services, e.g., in England and Germany |
| They can be prescribed by the doctor, although some therapies that meet all these criteria are offered to the patient directly by the manufacturer, similar to over-the-counter drugs |
| Examples |
| reSET-O® for treating addiction to substances such as alcohol, cannabis, and cocaine |
| Somryst™ for treating chronic insomnia |
| EndeavorRx™ is the first approved video game therapeutic option for ADHD treatment |
| Freespira is an innovative, clinically proven digital therapy to reduce or eliminate debilitating panic attacks |
| Kalmeda is developed to manage tinnitus |
| Velibra is used for anxiety disorders |
| Deprexis for the treatment of depression |
| Sleepio for the treatment of insomnia |
The international medical device regulators forum, a global group harmonizing regulatory requirements for medical products, defines medical software as “intended to be used for one or more medical purposes but performing without being part of a hardware medical device” (https://www.fda.gov/media/100714/download). Medical software can operate on generic computing platforms.
Software as a medical device ranges from those that allow a smartphone to display images obtained from magnetic resonance imaging for diagnostic purposes to computer-aided detection software that performs image postprocessing to help detect breast cancer. Medical software can be interfaced with other medical devices, including hardware. When software is connected to medical hardware but is a necessary component of its medical function is considered medical software.
DEVELOPMENTS IN DIGITAL THERAPEUTICS
Digital therapeutics development is a very complex process. In addition, following development, its clinical efficacy should be assessed in clinical trials. The digital drugs could be updated and evolve in the course of experimentation. Algorithms compose the primary active ingredient of digital therapy. Digital therapeutics require enrichment with digital excipients (an inactive substance that serves as the vehicle or medium for a drug or other active substance) to make them bioavailable. These include modules to remind complying with the digital treatments, connect physicians or healthcare providers with patients, generate dialogues with a virtual assistant, and achieve maximum digital bioavailability of the active ingredient, i.e. algorithms.
One of the first steps is to initiate the development of a digital therapy cognitive and behavioral literature review. This phase should result in ideas regarding therapeutic interventions to be tested and validated after digitalization. In this phase, patients can serve as users, testers, or partners involved in the experimentation. Medical software development, e.g. applications or video games, should include options for patients from different backgrounds, races, and ethnicities to interact with them. In addition, patient information security should be maintained. Finally, optimizing these digital therapies (DTx) to patients’ adherence to the physician's recommendations is essential. These steps often require close collaboration among multidisciplinary teams.
While a selected group of individuals can pilot the usability of the digital therapeutic tool, clinical trials in controlled conditions should be considered (equivalent to Phase I clinical trials). Finally, randomized controlled clinical trials with an intention-to-treat design (Phases II and III clinical trials) should be conducted to understand the benefits and disadvantages of these therapies and seek approval from the regulatory authorities. In these trials, the superiority and tolerability of digital therapeutic options could be compared with other treatment options or placebo. Placebos in these trials are simulated digital solutions for the disease of interest with no known clinical impact. For example, they should be in the form of similarly shaped applications to the digital therapeutic application.
Regulatory agencies often oversee digital therapeutics’ development, research, and trials. Approval of these trials by the ethics committees with specific content expertise is necessary. The outcomes considered for these therapeutic options could be similar to other drug trial outcomes. The need for different experimental designs should also be explored ([https://peartherapeutics.com/], [https://www.omadahealth.com/]).
An example of this process is the reSET treatment approval by the U. S. FDA in 2017. The reSET treatment is an application for treating addiction to substances such as alcohol, cannabis, and cocaine in a 3-month treatment plan. In 2018, reSET-O® for the treatment of opioid addiction was cleared by the FDA (https://www. fda. gov/news-events/press-announcements/fda-clears-mobile-medical-app-help-those-opioid-use-disorder-stay-recovery-programs). Another example of digital therapeutics with reasonable progress is insomnia treatment.[] Somryst™ for treating chronic insomnia was the first product submitted through the FDA's traditional 510(k) pathway. In addition, this software was reviewed through the FDA's software pre-certification pilot program and to be cleared in March 2020 (https://www.statnews. com/2018/07/25/phone-apps-digital-therapeutics/).
The FDA-approved ADHD pharmacological treatments[] include stimulants (amphetamines and methylphenidate) and nonstimulants (atomoxetine and guanfacine). Amphetamines are considered the most effective medications in reducing inattention, hyperactivity, and impulsivity in the short-term and possibly long term. As digital cognitive behavioral therapy is growing rapidly, using digital therapeutics in ADHD is considered. EndeavorRx™ is the first approved video game therapeutic option for ADHD treatment. In April 2020, The Lancet DigitalHealth[] published a study confirming the effectiveness of EndeavorRx™. The game's administration versus “placebo” included 25 min of activity per day, 5 days a week. Parents noted an improvement after 4 weeks in about half of 348 enrolled patients. This improvement rate exceeded 65% after another 30 days. The software treatment for actively reducing severity of ADHD clinical trial was a randomized, double-blinded, parallel-group controlled trial conducted at 20 research institutions in the United States between 2016 and 2017. The primary outcomes of this trial were changes in test of variables of attention (TOVA) and attention performance index (API) scores. The intervention was the digital therapy developed by Akili vs. a game without therapeutic effects on the control group. The mean change from baseline in the TOVA and API scores was significant in the AKL-T01 (intervention/game) group compared to the control group.
Recent studies support the hypothesis that virtual reality (VR) therapies can effectively distract patients suffering from chronic and acute pain. Patient immersion in interactive VR provides a distraction from painful stimuli and may decrease pain perception.[] As a result, the FDA has cleared Freespira® as a treatment option for patients with posttraumatic stress disorder. Freespira is an innovative, clinically proven digital therapy to reduce or eliminate debilitating panic attacks (A solution for panic attack treatment: FDA-cleared, drug-free [https://freespira.com/]).
The European Medicines Agency continues to assess approval processes for these therapeutic options. Germany, Belgium, France, and the United Kingdom have approved DTx covered by public health, and therefore, they can be prescribed by the respective health services. Kalmeda and Velibra are Germany's first two DTx approved and reimbursed. Kalmeda was developed to manage tinnitus, while Velibra is used for anxiety disorders. The application costs are covered by insurance after physicians prescribe them. No official assessment of Kalmeda's effectiveness was published; however, German laws indicate the evidence could be produced within a year after approval. In France, the High Health Authority approved the first software-based medical device to be reimbursed by the health services. Moovcare is a digital therapy based on a weekly questionnaire to detect lung cancer recurrence or complications. Finally, the UK National Health Service, through the national institute for health and care excellence, has so far conducted two evaluations of DTx, i.e. Deprexis for the treatment of depression and Sleepio for the treatment of insomnia.
DTx manage “nonfunctional attitudes”, including lifestyles and behavioral attitudes with relevant impacts on health status. However, digital treatments do not address the complexity of relationships surrounding us. Obesity and smoking are nonfunctional attitudes that could be modified using digital therapeutics.
Obesity and smoking affect the health of millions of citizens. Therefore, the network phenomenon plays a relevant role in the biological and behavioral traits of obesity and smoking.
One study in 2007, “The Spread of Obesity in a Large Social Network over 32 Years”,[] evaluated 12,067 individuals from 1971 to 2003 as a part of the Framingham Heart Study within a densely interconnected social network. Longitudinal statistical models were used to examine whether weight gain in one person was associated with weight gain in their friends, siblings, spouse, and neighbors. Distinct clusters of obese persons (body mass index ≥ 30 kg/m2) were found in the network at all time points. These clusters did not appear to be attributable solely to the formation of social ties among obese people. The chance of becoming obese increased by 57% if an individual had a friend who was obese in a given interval. Another study in 2008, “The Collective Dynamics of Smoking in a Large Social Network”,[] aimed to assess the impact of social ties in smoking habits on the same cohort and timeline. The investigators noted that smoking cessation by a spouse, sibling, or friend reduced a person's chance of smoking by 67%, 36%, and 25%, respectively. As smoking behavior spreads through close and distant social ties, the interconnected groups of people quit smoking in concert to marginalize the smokers socially. As knowledge of network ties is essential in treating smokers, and DTx can outline and manage these relationships, digital therapeutics could be considered a potentially effective path to increasing smoking cessation.
CONCLUSIONS
By leading to advances in DH, the digital revolution is opening new frontiers in medical knowledge, i.e. diagnosis and therapy. Like all new frontiers, standard rules, international regulatory bodies, and comparative studies are needed to confirm the promises of digital biomarkers, diagnostics, and therapies. More precise rules and policies are also required to ensure consistency between promises and expected clinical outcomes before their distribution by health services.
Conflicts of interest
Claudio Ronco is the Honorary Editor-in-Chief of the journal. Kianoush B. Kashani is an Editorial Board Member of the journal. The article was subject to the journal's standard procedures, with peer review handled independently of these members and their research groups.
How to cite this article: Barracca A, Ledda S, Mancosu G. et al. Digital Health: A New Frontier. J Transl Crit Care Med. 2023;5:e00018. doi: 10.1097/JTCCM-D-22-00018
REFERENCES
1.
Ronquillo Y, Meyers A, Korvek SJ. Digital Health, in StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.2.
Rachman S. The evolution of behaviour therapy and cognitive behaviour therapy. Behav Res Ther. 2015; 64:1–8.3.
Parliament TE. Europe Medical Device Regulation 2017/745. Regulation (EU) 2017/745 of the European Parliament And of the Council 2017. Accessed on April 4, 2022. https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32017R07454.
Xue Y. A review on intelligent wearables: Uses and risks. Hum Behav Emerg Technol. 2019; 1:287–294.5.
Whitney RL, Ward DH, Marois MT, Schmid CH, Sim I, Kravitz RL. Patient perceptions of their own data in mHealth technology-enabled N-of-1 trials for chronic pain: Qualitative study. JMIR Mhealth Uhealth. 2018; 6:e10291.6.
Noah B, Keller MS, Mosadeghi S, Stein L, Johl S, Delshad S, et al. Impact of remote patient monitoring on clinical outcomes: An updated meta-analysis of randomized controlled trials. NPJ Digit Med. 2018; 1:20172.7.
Simblett S, Greer B, Matcham F, Curtis H, Polhemus A, Ferrão J, et al. Barriers to and facilitators of engagement with remote measurement technology for managing health: Systematic review and content analysis of findings. J Med Internet Res. 2018; 20:e10480.8.
Coppetti T, Brauchlin A, Müggler S, Attinger-Toller A, Templin C, Schönrath F, et al. Accuracy of smartphone apps for heart rate measurement. Eur J Prev Cardiol. 2017; 24:1287–1293.9.
Torfs T, Smeets CJ, Geng D, Berset T, Van der Auwera J, Vandervoort P, et al. Clinical validation of a low-power and wearable ECG patch for long term full-disclosure monitoring. J Electrocardiol. 2014; 47:881–889.10.
Turakhia MP, Desai M, Hedlin H, Rajmane A, Talati N, Ferris T, et al. Rationale and design of a large-scale, app-based study to identify cardiac arrhythmias using a smartwatch: The apple heart study. Am Heart J. 2019; 207:66–75.11.
Hafezi H, Robertson TL, Moon GD, Au-Yeung KY, Zdeblick MJ, Savage GM. An ingestible sensor for measuring medication adherence. IEEE Trans Biomed Eng. 2015; 62:99–109.12.
Rovini E, Maremmani C, Cavallo F. Automated systems based on wearable sensors for the management of Parkinson's disease at home: A systematic review. Telemed J E Health. 2019; 25:167–183.13.
Coravos A, Khozin S, Mandl KD. Developing and adopting safe and effective digital biomarkers to improve patient outcomes. NPJ Digit Med. 2019; 2:14.14.
Shuren J, Patel B, Gottlieb S. FDA regulation of mobile medical apps. JAMA. 2018; 320:337–338.15.
Byrom B, Watson C, Doll H, Coons SJ, Eremenco S, Ballinger R, et al. Selection of and evidentiary considerations for wearable devices and their measurements for use in regulatory decision making: Recommendations from the ePRO consortium. Value Health. 2018; 21:631–639.16.
Izmailova ES, Wagner JA, Perakslis ED. Wearable devices in clinical trials: Hype and hypothesis. Clin Pharmacol Ther 2018; 104:42–52.17.
Rovini E, Maremmani C, Cavallo F. How wearable sensors can support Parkinson's disease diagnosis and treatment: A systematic review. Front Neurosci. 2017; 11:555.18.
Silva de Lima AL, Hahn T, de Vries NM, Cohen E, Bataille L, Little MA, et al. Large-scale wearable sensor deployment in Parkinson's patients: The Parkinson@home study protocol. JMIR Res Protoc. 2016; 5:e172.19.
Sim I. Mobile devices and health. N Engl J Med 2019; 381:956–68.20.
Vargas-Cuentas NI, Roman-Gonzalez A, Gilman RH, Barrientos F, Ting J, Hidalgo D, et al. Developing an eye-tracking algorithm as a potential tool for early diagnosis of autism spectrum disorder in children. PLoS One. 2017; 12:e0188826.21.
He L, Cao C. Automated depression analysis using convolutional neural networks from speech. J Biomed Inform. 2018; 83:103–111.22.
Pirnstill CW, Coté GL. Malaria diagnosis using a mobile phone polarized microscope. Sci Rep. 2015; 5:13368.23.
Poplin R, Varadarajan AV, Blumer K, Liu Y, McConnell MV, Corrado GS, et al. Prediction of cardiovascular risk factors from retinal fundus photographs via deep learning. Nat Biomed Eng. 2018; 2:158–164.24.
Moore RC, Swendsen J, Depp CA. Applications for self-administered mobile cognitive assessments in clinical research: A systematic review. Int J Methods Psychiatr Res. 2017; 26:e1562.25.
Luik AI, Kyle SD, Espie CA. Digital Cognitive Behavioral Therapy (dCBT) for Insomnia: A state-of-the-science review. Curr Sleep Med Rep. 2017; 3:48–56.26.
Cortese S. Pharmacologic treatment of attention deficit-hyperactivity disorder. N Engl J Med. 2020; 383:1050–1056.27.
Kollins SH, DeLoss DJ, Cañadas E, Lutz J, Findling RL, Keefe RSE, et al. A novel digital intervention for actively reducing severity of paediatric ADHD (STARS-ADHD): A randomised controlled trial. Lancet Digit Health. 2020; 2:e168–178.28.
Pourmand A, Davis S, Marchak A, Whiteside T, Sikka N. Virtual reality as a clinical tool for pain management. Curr Pain Headache Rep. 2018; 22:53.29.
Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007; 357:370–379.30.
Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008; 358:2249–2258.
