INTRODUCTION
Heart rate variability (HRV) is an objective marker of autonomic balance and cardiovascular health. It represents the changes in the cardiac inter-beat intervals (IBIs) in response to the sympathetic and parasympathetic nervous systems’ output over time. In the general population, lower HRV has been linked to increased all-cause mortality and a myriad of adverse outcomes such as multiple organ dysfunction syndrome, sepsis, and cardiovascular diseases, as well as increased systemic inflammation.
According to the guidelines of the HRV Task Force, short-term HRV recordings are traditionally acquired over a recording period of 5-10 minutes. However, with the miniaturization and advancement of HRV measuring devices, recordings of <5 minutes have also been used and are known as ultra-short-term HRV (HRVUST). With a recording of 10-20 seconds, HRVUST offers feasibility under standard conditions with minimum burden on the patients and has shown validity with its short-term counterparts, making it a valuable resource.
Combat injury has been considered “the most visible and arresting toll of war on the human body”. Thousands of casualties have been reported in the U.S. and U.K. military as a result of combat-related traumatic injuries (CRTIs)., However, the impact of CRTI on HRV is limitedly researched. A recently published systematic review reported lower levels of HRV in relation to non-acute traumatic injuries—albeit with low strength of evidence. The authors further highlighted that there is a paucity of HRV research in relation to traumatic injuries, especially in military populations, where the use of HRV has predominantly been limited as a triage tool in acute trauma settings. It was not until recently that the impact of long-term CRTI on HRVUST was studied for the first time in a sample of British servicemen. In this study, the authors reported an inverse relationship between CRTI and HRVUST. Notably, the striking impact of CRTI on HRVUST was persistent 8 years after injury. Injury severity and blast injuries were also reported to be independently associated with lower HRVUST.
To date, little is known about the underlying mechanism to explain the observed lower HRV associated with CRTI. It is well known that depression, anxiety, and poor physical health (e.g., lower physical functioning and relative obesity), are linked to lower HRV. Along with the obvious adverse physical sequelae, CRTI has also been linked to poorer mental health outcomes including increased levels of anxiety, depression, and post-traumatic stress disorder. Good mental and physical health (physical fitness and maintenance of normal body mass index [BMI]) are of vital importance to deployed military personnel to ensure optimal performance and resilience to injury.
To date, no study has explored the impact of these physical and mental health mediators on the long-term relationship between CRTI and HRV. Consequently, in this study, we sought to examine the influence of objective markers of physical and mental health on the relationship between CRTI, its severity, and HRV in a sample of male British combat personnel. We hypothesized that both physical and mental health would mediate the relationship between combat injury, its severity and HRV.
METHODS
Study Design and Setting
This study involved the baseline analysis of the ArmeD SerVices TrAuma and RehabilitatioN OutComE (ADVANCE) Cohort Study. In this study, combat veterans with CRTI were frequency-matched to uninjured deployed servicemen by age, rank, role, deployment (Afghanistan, 2003-2014), and time of deployment. All participants voluntarily took part in the study and provided written informed consent after reading the participant information sheet. The data for this study were collected at Headley Court (March 2016-August 2018) and Stanford Hall (August 2018 onward). The ADVANCE study has full ethical approval from the Ministry of Defence Research Ethics Committee (protocol no.: 357/PPE/12).
Study Population
The study population has been described previously. All participants were male British military personnel, and the detailed inclusion/exclusion criteria have been previously reported. The injured group consisted of servicemen who experienced physical CRTI during their deployment that required aeromedical evacuation for their injuries. Among the injured group, the most common mechanism of injury was blast followed by gunshot wounds and others. The uninjured group consisted of servicemen deployed to the same conflict at a similar time and in a similar role but was uninjured.
Sample Size
The sample size in the current study was a subset consisting of 862 participants (75.3%) from the full ADVANCE cohort (n = 1144). This subset represented the total number of participants from the full ADVANCE cohort who had full arterial waveform data available that could be used to measure HRVUST. The current dataset was similar to the full ADVANCE cohort in terms of key demographics and military characteristics (data not shown but available from the authors).
Study Variables
CRTI (yes or no) was the primary exposure variable. The secondary exposure variable was the New Injury Severity Score (NISS) used as a measure of injury severity. The NISS were calculated from the Abbreviated Injury Score (2008 update), which was provided by the U.K. Joint Theatre Trauma Registry. The NISS was categorized as severe (NISS ≥ 25) and less severe (NISS < 25) based on NISS’ predictive cut-off for all-cause mortality with the uninjured as the reference category.
The primary outcome variable in this study was the time domain HRV measure of root mean square of successive differences (RMSSD). RMSSD was calculated using consecutive IBI data over a 16-second recording of femoral arterial waveform data during the measurement of pulse wave velocity using the Vicorder device. The detailed methods have been described and published elsewhere., Overall, RMSSD was chosen given the length of arterial waveform recording and its established reliability and validity in HRVUST analysis.,
For mediators, the 6-minute walk test (6MWT) and BMI adjusted for amputation (hereafter referred to as BMI) were used as measures of physical health and fitness. The 6MWT has been used as a valid test of physical function for able bodies and amputees. The participants were asked to walk back and forth over a 20-m flat hard surface for a total of 6 minutes at their own maximal pace. The distance (meters) covered by each participant was noted and used for this test. Height (meters) and weight (kilograms) required for BMI calculation were measured using a stadiometer and electronic scale, respectively. In the case of an amputation, height recorded before injury was used from the medical record for BMI calculation. BMI was adjusted for amputation.
The scores of depressive and anxiety symptoms were used to measure mental health. The data on depression was captured using the Patient Health Questionnaire (PHQ-9)., It is a nine-item self-reported questionnaire to screen the presence of depression and its severity with the scores ranging from 0 to 27. Anxiety was measured using the Generalized Anxiety Disorder (GAD-7)., In this seven-item questionnaire, the participants were asked to recall anxiety symptoms over the preceding 2 weeks. The total score ranged from 0 to 21.
Rank at sampling was used as a proxy for the socioeconomic status of the participants according to the National Statistics Socio-Economic Classification.,,
The ranks were classified as lower (junior non-commissioned officers and other lower ranks), middle (senior non-commissioned officers), and senior (commissioned officers).,, Ethnicity was defined into two categories: White and other ethnic groups (Black, Asian, and Mixed).
Statistical Analysis
Descriptive statistics
The results are presented as mean ± standard deviation (SD) for normally distributed data or median and interquartile range (IQR) for skewed continuous data. The normality of continuous data was visually inspected through the histograms and Q–Q plots. Appropriate parametric or non-parametric tests were used to test the baseline differences between the injured and uninjured groups. The number of missing values was negligible (GAD-7, n = 2; PHQ-9, n = 3; 6MWT, n = 10), and therefore, no data were imputed and were handled by default complete case analysis. A P-value of <.05 was considered to indicate statistical significance. All tests were conducted in Stata 17 (StataCorp LLC, College Station, TX, USA).
Structural equation modeling
The effect of mediators on the exposure–outcome relationship was quantified using structural equation modeling (SEM). It is a statistical technique that is used to study the causal relationships among variables. The eligibility of included mediators was guided by the criteria recommended by Chmura, Kiernan, Essex, and Kupfer. SEM was used to construct the pathway between exposure and outcome variables in the presence of mediators (BMI, 6MWT, depression, and anxiety) using the maximum likelihood estimation. The SEM models were adjusted for a priori confounders: time from injury, rank, ethnicity, and age at assessment. These were not shown on the path diagrams for clarity purposes.
Two hypothesized pathway models were specified: One with CRTI as the exposure variable (Figure S1) and the other with injury severity (uninjured, NISS < 25, NISS ≥ 25) as the exposure variable (Figure S2). These models consisted of the direct effect of CRTI/injury severity on RMSSD mediated by the physical and mental health mediators. The covariances between depression and anxiety, BMI and 6MWT, BMI and depression, and BMI and anxiety were added based on the literature.
The direct effect (exposure → outcome) was calculated. The indirect effect was calculated as the product of two coefficients: (exposure → mediator) and (mediator → outcome). The unstandardized coefficients were reported for both direct and indirect effects. The proportion of mediation (%) was also reported. The chi-squared value (χ2), the comparative fit index (CFI), the Tucker–Lewis index (TLI), and the root mean square error of approximation (RMSEA) were used to assess the goodness of fit. A low χ2 value with an insignificant P-value represents an adequate fit. A value of.95 for CFI and TLI is deemed to represent a good fit, whereas a value of close to .06 for RMSEA is considered an acceptable fit. The model was further inspected for the Heywood case—no variances over 1 or negative were found (standardized coefficients). The total, direct, and indirect effects were reported using a bias-corrected bootstrapped CI with 1,000 resamples as recommended.
RESULTS
Of the 862 participants, 428 (49.6%) were injured (including 133 [31.1%] amputees) and 434 (50.3%) were uninjured. The overall mean age at assessment was 33.9 ± 5.4 years. The mean time from injury/deployment to assessment was 7.9 ± 2.1 years. No significant differences were noted between injured and uninjured servicemen in terms of age at assessment, ethnicity, and time from injury/deployment (Table S1). Stratified by injury status, only the difference in time from injury/deployment and the 6MWT was found to be statistically significant (Table S2).
The median RMSSD was significantly lower in injured vs. uninjured participants (39.4 ms [IQR: 27.77-59.77] vs. 46.2 ms [IQR: 31.14-67.84]; P < .001). Servicemen with NISS ≥ 25 had non-significantly lower RMSSD compared with those with NISS < 25 (36.3 ms [IQR: 24.18, 58.54] vs. 40.1 ms [IQR: 29.57, 59.77]; P = .08). The median scores of self-reported depression and anxiety symptoms were significantly higher in injured servicemen than in the uninjured servicemen. Injured servicemen covered a significantly lower distance on the 6MWT than uninjured counterparts and were also more likely to be overweight with a higher BMI than uninjured servicemen (Table S1).
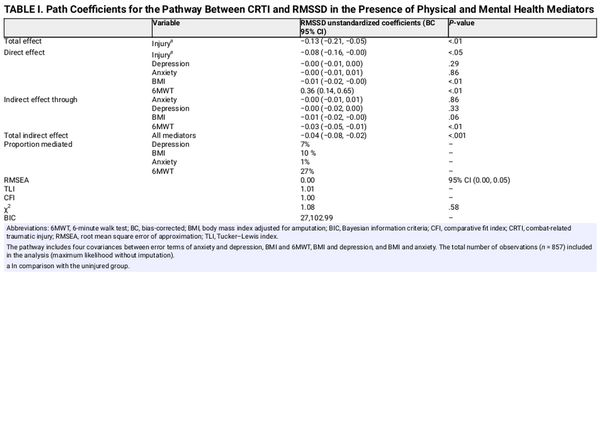
Figure 1 presents the unstandardized estimates for the adjusted CRTI model. The fit indices demonstrated a good fit model (Table I). A significant total effect of CRTI on RMSSD in the presence of mediators was −0.13 (95% CI: −0.21, −0.05). The direct effects of 6MWT and BMI on RMSSD were 0.36 (95% CI: 0.14, 0.65) and −0.01 (95% CI: −0.02, −0.00), respectively. Mental health mediators (depression and anxiety) had no significant direct effect on RMSSD.
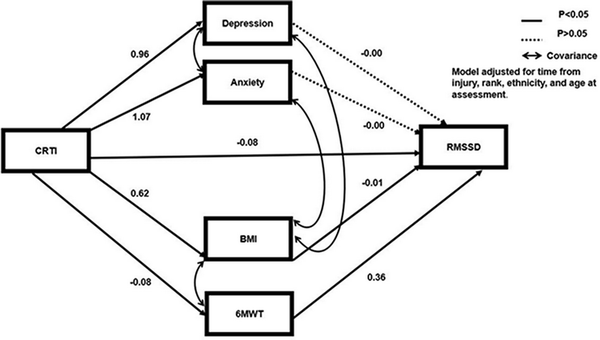
FIGURE 1
Path coefficients of adjusted mediation model on the CRTI–HRVUST pathway. Abbreviations: 6MWT, 6-minute walk test; BMI, body mass index adjusted for amputation; CRTI; combat-related traumatic injury; HRVUST ultra-short-term heart rate variability; RMSSD, root mean square of successive differences. The pathway includes four covariances between error terms of anxiety and depression, BMI and 6MWT, BMI and depression, and BMI and anxiety. Depression, anxiety, BMI, 6MWT, and RMSSD have been included in the SEM model as continuous variables. Model adjusted for age at assessment, rank, ethnicity, and time from injury with uninjured as the reference category.
A significant total indirect effect of all mediators on the association between CRTI and RMSSD was −0.04 (95% CI: −0.08, −0.02). However, only one significant indirect pathway was identified: CRTI → 6MWT → RMSSD with an estimate of −0.03 (95% CI: −0.05, −0.01). The ratio of indirect effect/total effects (a measure of effect size) was 0.27, reflecting that 27% of the effect of CRTI on RMSSD was mediated by the 6MWT after accounting for the other mediators. BMI, depression, and anxiety were not significant mediators of the relationship. The direct effect of CRTI on RMSSD was −0.08 (95% CI: −0.16, −0.00) and was still significant even after accounting for the mediators.
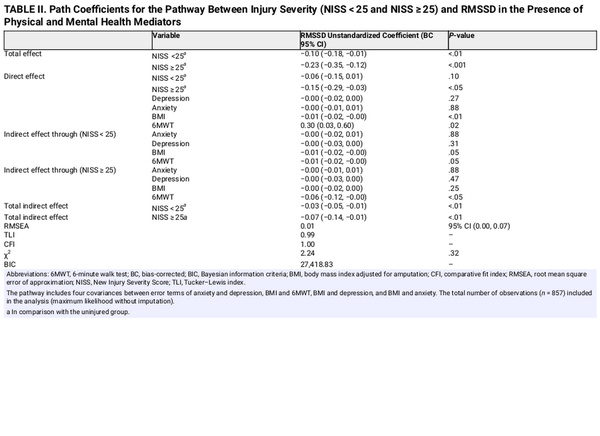
The unstandardized estimates for the adjusted injury severity model can be seen in Figure 2. A good model fit was observed for the injury severity and RMSSD model (Table II). The model showed a significant total effect of injury severity on RMSSD (Table II). For lower injury severity, an insignificant direct effect on RMSSD was observed. The indirect effect of lower injury severity on RMSSD through mental health factors was insignificant, whereas a borderline significant effect was observed for physical health factors (Table II).
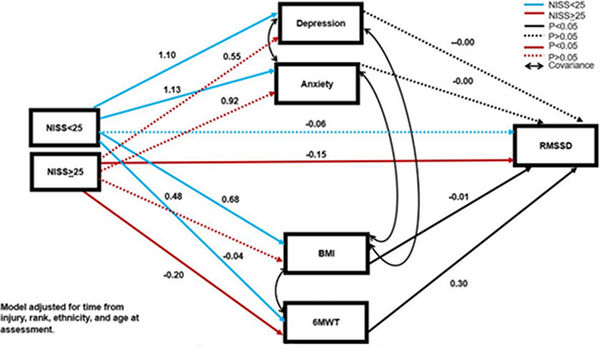
FIGURE 2
Path coefficients of adjusted mediation model on the Injury Severity- HRVUST pathway. Abbreviations: 6MWT, 6-minute walk test; BMI, body mass index adjusted for amputation; HRVUST ultra-short-term heart rate variability; NISS, New Injury Severity Score; RMSSD, root mean square of successive differences. The pathway includes four covariances between error terms of anxiety and depression, BMI and 6MWT, BMI and depression, and BMI and anxiety. Depression, anxiety, BMI, 6MWT, and RMSSD have been included in the SEM model as continuous variables. Model adjusted for age at assessment, rank, ethnicity, and time from injury with uninjured as the reference category.
Only the 6MWT significantly mediated the relationship between injury severity (NISS ≥ 25 vs. uninjured) and RMSSD with an estimate of −0.06 (95% CI: −0.12, −0.00). BMI, depression, and anxiety showed no significant mediation. A significant direct effect of NISS ≥ 25 on RMSSD was −0.15 (95% CI: −0.29, −0.03) and was still observed in the presence of mediators.
DISCUSSION
This study investigated the mediating effect of mental and physical health on the relationship between CRTI, its severity and HRV in male British military combat personnel. We found that depression, anxiety, and BMI did not mediate the relationship between injury, its severity and HRV. The only significant mediating pathway was observed through the 6MWT.
The present mediation analyses suggest that the association between CRTI and higher injury severity (NISS ≥ 25) and RMSSD is mediated by the 6MWT; however, a direct effect of CRTI and higher injury severity on RMSSD remained. The 6MWT was used as a proxy of physical function and exercise in the present study. The potential mechanism of action for this pathway could be explained by the role of physical exercise that has been evidenced to improve homeostasis and promote anti-inflammatory processes, indicating the neurological and cardioprotective role of physical exercise. This might explain the mediating role of physical function on HRV levels in our study sample. Furthermore, as servicemen are encouraged to be physically fit to be able to perform their military duties, our findings emphasize the importance of physical functioning, especially following CRTI as physical functioning is strongly associated with the increased vagal tone, HRV, and overall health and well-being. More importantly, our findings are free of “learning effect” bias—this may be observed when participants take the 6MWT in multiple trials and cover longer distances as a result—this was not the case in the present study. We also observed that those with severe injuries covered significantly lesser distance on the 6MWT as compared to those with less severe injuries (Table S2) and uninjured (Table S1). The mediation analysis also suggests that the servicemen with higher injury severity are more likely to benefit from the mediating effect of physical function on elevating RMSSD than those who are less severely injured. However, our findings are limited in direct comparison with other studies because of a lack of evidence on the CRTI-HRV mediating pathway.
Our hypothesis on the potential mediating effect of mental health mediators (depression and anxiety) was not supported by our findings. The finding of the insignificant effect of depression and anxiety on the CRTI–RMSSD relationship is unexpected given the increased mental health burden in our sample as previously reported and the association between lower HRV in relation to depression and anxiety. However, this may be explained by an insignificant direct effect of depression and anxiety on RMSSD individually in the present study, rendering the total indirect effect insignificant. Furthermore, depression and anxiety were used as continuous variables rather than binary (yes/no) in this study, which might have under-represented their effect. Another plausible explanation could be the higher physical activity levels of the cohort, which might have reduced anxiety and depression and were not accounted for in the present mediation analyses. However, it is uncertain whether it is the pre-injury or post-injury level of physical activity that seems to buffer the effect.
To the authors’ knowledge, this is the first study to explore the influence of physical and mental health mediators on the relationship between CRTI, its severity, and HRV. Other strengths include comparison with frequency-matched uninjured servicemen who shared a similar experience as the injured group except for their injury. The use of advanced SEM and reporting of bias-corrected bootstrapped CI represents the statistical rigor of the mediation analyses presented in this study.
The findings of this study should be interpreted under the context of a few limitations. First, only selected measures (6MWT and BMI; SC-PHQ9 and GAD-7) were included to represent mental and physical health in the current study. This might have limited the view of physical and mental health. It is suggested to include other measures of physical and mental health in future studies to fully capture their effects on HRV. Second, the cardiac IBIs used to derive HRV were sourced via the femoral arterial pulse wave data— contrary to the gold-standard ECG data. Only a subset of RMSSD data from the full ADVANCE dataset was used because of the unavailability of arterial waveforms. Nevertheless, this study did represent about 75% of the entire ADVANCE baseline cohort. Our findings are only applicable to White, male military personnel (with and without combat trauma) until results are replicated in other populations. Moreover, mediators included in this study were likely to be interrelated with each other, which might have masked or enhanced the effect of other mediators. However, to counter this, the covariances were added among the mediators to minimize and account for the interaction between them. It was also assumed that there were no unmeasured confounders—if this assumption was violated, this may have biased the results. Depression and anxiety scores were included in the causal pathways as continuous variables instead of dichotomous variables (yes/no). This might have under-represented their effect on RMSSD. Conversely, the cut-off score for the diagnosis of depression, anxiety, and its worsening severity is debatable. Furthermore, mental health measures (mediators) and RMSSD (outcome) were measured at the same time point, which may have introduced temporal order bias in our results. Lastly, the presented mediation pathways are limited by their cross-sectional and exploratory nature, for which longitudinal studies are warranted to validate these findings.
The findings offer implications for research, practice, and policy. From a primary healthcare perspective, physical function should be promoted to enhance RMSSD (parasympathetic tone) for the management and rehabilitation of people with traumatic injuries. Policymakers may also consider our findings to design policies targeted at promoting physical function following combat trauma. While this study focused on male British military personnel, it would be interesting to replicate this study in other groups such as female combatants and to explore the influence of sex on the presented causal pathway. Furthermore, keeping the limitations in mind, future research on HRV intervention may also consider our findings to guide and design interventions for people with traumatic injuries.
CONCLUSION
This study investigated the role of mental and physical health mediators in the relationship between combat injury, its severity and HRV in a sample of British servicemen. Our findings suggest that the 6MWT as a measure of physical function partially mediates the relationship between CRTI, its severity and HRV. Greater physical function may enhance HRV levels in populations with traumatic injuries. These findings have implications for the development of interventions and inform rehabilitation programs for the injured population.
ACKNOWLEDGMENTS
We wish to thank all the research staff at both Headley Court and Stanford Hall who helped with the ADVANCE study, including Dan Dyball, Eleanor Miller, Stefan Sprinckmoller, Maria-Benedicta Edwards, Helen Blackman, Melanie Chesnokov, Emma Coady, Sarah Evans, Guy Fraser, Meliha Kaya-Barge, Maija Maskuniitty, David Pernet, Helen Prentice, Urszula Pucilowska, Lajli Varsani, Anna Verey, Molly Waldron, Danny Weston, Tass White, Seamus Wilson, and Louise Young.
REFERENCES
- 1. Malik M: Heart rate variability: standards of measurement, physiological interpretation, and clinical use: Task Force of the European Society of Cardiology and the North American Society for Pacing and Electrophysiology. Ann Noninvasive Electrocardiol 1996; 1(2): 151–81.doi: .
- 2. Johnston BW, Barrett-Jolley R, Krige A, Welters ID: Heart rate variability: measurement and emerging use in critical care medicine. J Intensive Care Soc 2020; 21(2): 148–57.doi: .
- 3. Pecchia L, Castaldo R, Montesinos L, Melillo P: Are ultra‐short heart rate variability features good surrogates of short‐term ones? State‐of‐the‐art review and recommendations. Healthc Technol Lett 2018; 5(3): 94–100.doi: .
- 4. Munoz ML, Van Roon A, Riese H, et al: Validity of (ultra-) short recordings for heart rate variability measurements. PLoS One 2015; 10(9): e0138921.doi: .
- 5. Champion HR, Bellamy RF, Roberts CP, Leppaniemi A: A profile of combat injury. J Trauma Acute Care Surg 2003; 54(5): S13–9.doi: .
- 6. Keene DD, Penn-Barwell JG, Wood PR, et al: Died of wounds: a mortality review. BMJ Mil Health 2016; 162(5): 355–60.doi: .
- 7. Stewart IJ, Poltavskiy E, Howard JT, et al: The enduring health consequences of combat trauma: a legacy of chronic disease. J Gen Intern Med 2021; 36(3): 713–21.doi: .
- 8. Maqsood R, Khattab A, Bennett AN, Boos CJ, Siddiqi TJ: Association between non-acute traumatic injury (TI) and heart rate variability (HRV) in adults: a systematic review and meta-analysis. PLoS One 2023; 18(1): e0280718.doi: .
- 9. Ryan ML, Thorson CM, Otero CA, Vu T, Proctor KG: Clinical applications of heart rate variability in the triage and assessment of traumatically injured patients. Anesthesiol Res Pract 2011; 2011: 1–8.doi: .
- 10. Maqsood R, Schofield S, Bennett AN, et al: Relationship between combat-related traumatic injury and ultrashort term heart rate variability in a UK military cohort: findings from the ADVANCE study. BMJ Mil Health 2023; 1–6.doi: .
- 11. Koch C, Wilhelm M, Salzmann S, Rief W, Euteneuer F: A meta-analysis of heart rate variability in major depression. Psychol Med 2019; 49(12): 1948–57.doi: .
- 12. Chalmers JA, Quintana DS, Abbott MJA, Kemp AH: Anxiety disorders are associated with reduced heart rate variability: a meta-analysis. Front Psychiatry 2014; 5: 80.doi: .
- 13. Koenig J, Jarczok MN, Warth M, et al: Body mass index is related to autonomic nervous system activity as measured by heart rate variability—a replication using short term measurements. J Nutr Health Aging 2014; 18(3): 300–2.doi: .
- 14. Strüven A, Holzapfel C, Stremmel C, Brunner S: Obesity, nutrition, and heart rate variability. Int J Mol Sci 2021; 22(8): 4215.doi: .
- 15. Bhatnagar V, Richard E, Melcer T, Walker J, Galarneau M: Retrospective study of cardiovascular disease risk factors among a cohort of combat veterans with lower limb amputation. Vasc Health Risk Manag 2019; 15: 409–18.doi: .
- 16. Tavares KB, Russell DM, Conrad RJ, et al: Time to weigh in on obesity and associated comorbidities in combat-wounded amputees. J Trauma Acute Care Surg 2021; 90(2): 325–30.doi: .
- 17. Boos CJ, Schofield S, Cullinan P, et al: Association between combat-related traumatic injury and cardiovascular risk. Heart 2022; 108(5): 367–74.doi:doi: .
- 18. Linberg AA, Roach KE, Campbell SM, et al: Comparison of 6-minute walk test performance between male Active Duty soldiers and servicemens with and without traumatic lower-limb loss. J Rehab Res Dev 2013; 50(7): 931–40.doi: .
- 19. Littman AJ, Thompson ML, Arterburn DE, et al: Lower-limb amputation and body weight changes in men. J Rehab Res Dev 2015; 52(2): 159–70.doi: .
- 20. Dyball D, Bennett AN, Schofield S, et al: Mental health outcomes of male UK military personnel deployed to Afghanistan and the role of combat injury: analysis of baseline data from the ADVANCE cohort study. Lancet Psychiat 2022; 9(7): 547–54.doi: .
- 21. Rappole C, Grier T, Anderson MK, Hauschild V, Jones BH: Associations of age, aerobic fitness, and body mass index with injury in an operational Army brigade. J Sci Med Spot 2017; 20: S45–S50.doi: .
- 22. Bennett AN, Dyball DM, Boos CJ, et al: Study protocol for a prospective, longitudinal cohort study investigating the medical and psychosocial outcomes of UK combat casualties from the Afghanistan war: the ADVANCE study. BMJ Open 2020; 10(10): e037850.doi: .
- 23. Li H, Ma YF: New injury severity score (NISS) outperforms injury severity score (ISS) in the evaluation of severe blunt trauma patients. Chinese J Traumatol 2021; 24(05): 261–5.doi: .
- 24. Nussinovitch U, Elishkevitz KP, Katz K, et al: Reliability of ultra-short ECG indices for heart rate variability. Ann Noninvasive Electrocardiol 2011; 16(2): 117–22.doi: .
- 25. Lin SJ, Bose NH: Six-minute walk test in persons with transtibial amputation. Arch Phys Med Rehab 2008; 89(12): 2354–9.doi: .
- 26. Kroenke K, Spitzer RL, Williams JB: The PHQ‐9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16(9): 606–13.doi: .
- 27. Spitzer RL, Kroenke K, Williams JB, Löwe B: A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166(10): 1092–7.doi: .
- 28. Fairchild AJ, McDaniel HL: Best (but oft-forgotten) practices: mediation analysis. Am J Clin Nutr 2017; 105(6): 1259–71.doi: .
- 29. Chmura Kraemer H, Kiernan M, Essex M, Kupfer DJ: How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychol 2008; 27(2 Suppl): S101–8.doi: .
- 30. Cosci F, Fava GA: When anxiety and depression coexist: the role of differential diagnosis using clinimetric criteria. Psychother Psychosom 2021; 90(5): 308–17.doi: .
- 31. Larsson UE, Reynisdottir S: The six-minute walk test in outpatients with obesity: reproducibility and known group validity. Physiother Res Int 2008; 13(2): 84–93.doi: .
- 32. Luppino FS, de Wit LM, Bouvy PF, et al: Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 2010; 67(3): 220–9.doi: .
- 33. Amiri S, Behnezhad S: Obesity and anxiety symptoms: a systematic review and meta-analysis. Neuropsychiatrie: Klinik, Diagnostik, Therapie Und Rehabilitation: Organ der Gesellschaft Osterreichischer Nervenarzte und Psychiater 2019; 33(2): 72–89.doi: .
- 34. Hu L-T, Bentler PM: Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modell 1999; 6(1): 1–55.doi: .
- 35. MacKinnon DP, Lockwood CM, Williams J: Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivar Behav Res 2004; 39(1): 99–128.doi: .
- 36. Du H, Newton PJ, Salamonson Y, Carrieri-Kohlman VL, Davidson PM: A review of the six-minute walk test: its implication as a self-administered assessment tool. Eur J Cardiovasc Nurs 2009; 8(1): 2–8.doi: .
- 37. Mahalakshmi B, Maurya N, Lee SD, Bharath Kumar V: Possible neuroprotective mechanisms of physical exercise in neurodegeneration. Int J Mol Sci 2020; 21(16): 5895.doi: .
- 38. Kemp AH, Quintana DS: The relationship between mental and physical health: insights from the study of heart rate variability. Int J Psychophysiol 2013; 89(3): 288–96.doi: .
- 39. Gibbons WJ, Fruchter N, Sloan S, Levy RD: Reference values for a multiple repetition 6-minute walk test in healthy adults older than 20 years. J Cardiopulm Rehabil 2001; 21(2): 87–93.doi: .
- 40. Vo -T-T, Superchi C, Boutron I, Vansteelandt S: The conduct and reporting of mediation analysis in recently published randomized controlled trials: results from a methodological systematic review. J Clin Epidemiol 2020; 117: 78–88.doi: .