INTRODUCTION
The Military Health System (MHS) is the global health system of the Department of Defense (DoD) and includes over 50 military hospitals and 600 clinics. Its purpose, under the direction of the Defense Health Agency (DHA), is to support service members and their families. The primary objectives are to maintain a medically ready fighting force, as well as a ready medical force to care for the war fighter. Within this system is Brooke Army Medical Center (BAMC), the largest military hospital and the only level 1 trauma center in the DoD. While caring for active duty, retired uniformed services personnel, and beneficiaries, BAMC also provides burn and trauma casualty care to civilians. BAMC works in collaboration with the Southwest Texas Regional Advisory Council (STRAC) and University Hospital (UH), San Antonio’s other level 1 trauma center, to provide trauma care to residents of the city and 22 counties in southwest Texas from San Antonio to Mexico (26,000 square mile area). There are no level 2 centers in the region, which allows both UH and BAMC to avoid some of the dilution experienced by trauma centers in other large urban areas. In addition to serving its patient population, BAMC serves as a platform to provide and maintain trauma casualty care skills for military medical personnel.
In response to concerns about the readiness of military medical personnel to care for traumatically injured combat casualties, the National Defense Authorization Act of 1996 required the DoD to implement training programs within civilian trauma centers. In the years to follow, several civilian-military partnerships were established to support training and sustaining readiness in trauma care for military medical personnel., The published reports describing the benefit of these affiliations’ focus on surgical case exposure for surgeons. The surgical caseloads experienced by military surgeons in civilian level 1 trauma centers far exceeded the exposure in in-garrison military hospitals. In general, experience in civilian level 1 trauma centers exposed military surgeons to a comprehensive trauma practice and supported sustainment of combat surgical skills.
There are limited published data related to the emergency care experiences in level 1 trauma centers or the emergency care exposure needs of military emergency medicine physicians. To our knowledge, this is the first report describing the overall trauma patient population treated at the only level 1 trauma center in the DoD. The purpose of this study was to characterize and compare the trauma patient populations treated at the DoD level 1 trauma center and the civilian level 1 trauma center in a major metropolitan city. A secondary purpose was to determine if the populations were representative of the trauma patients treated in a combat setting.
Methods
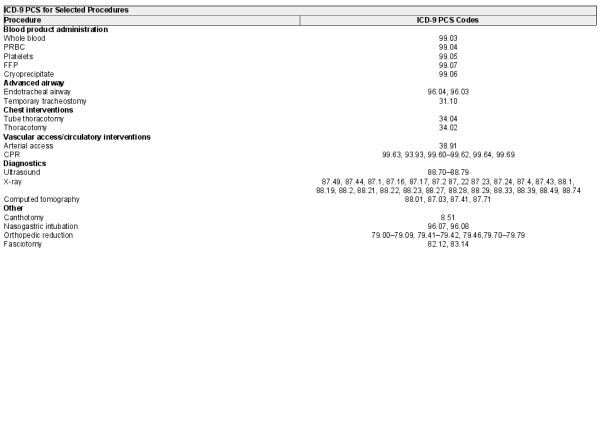
We obtained a nonhuman subjects research determination for de-identified data from the US Air Force 59th Medical Wing and the University of Texas Health Science Center at San Antonio Institutional Review Boards. Data requests were submitted to the Trauma Registries for BAMC and UH. We included all traumatic injuries from any mechanism of injury (MOI) treated at either facility from January 1, 2015 to December 31, 2017. We excluded patients less than 18 years of age. Data elements in the query included demographic information, injury descriptors, diagnoses, emergency department procedures, and outcome data (ventilation, intensive care unit (ICU), and hospital days). We used the International Classification of Disease, version 9 (ICD-9-PCS) procedure codes provided by the BAMC query to determine the incidence of procedures performed in the emergency department at BAMC (see Appendix A for list of ICD-9-PCS codes). We utilized data published by Schauer et al. (2019) to provide rates of procedures performed on patients treated in in-theater military emergency department settings.
Statistical Analysis
Descriptive statistics on sex, age, MOI, injury severity and type, injury body region, and procedures obtained from BAMC and UH data were calculated using Microsoft Excel version 2016 (version 16.0, Redmond, WA) and IBM SPSS version 23. For a representation of the distribution of injury severity, the ISS data were categorized into groups: minor (1–15), moderate (16–25), severe (26–50), and critical (51–75). Descriptive statistics included counts and percentages with 95% confidence intervals [95% CI] for categorical variables and medians with interquartile ranges (IQR) for continuous variables. We conducted two-proportion Z-tests to examine differences between samples in categorical variables (eg, injury type; procedure categories) and Wilcoxon-rank sum test for continuous variables (eg, age).
Results
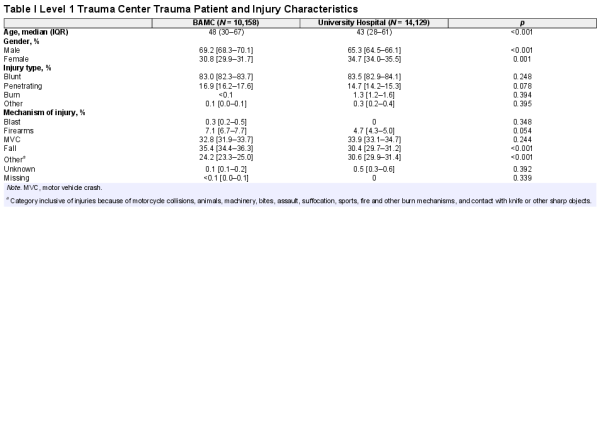
The final sample for BAMC consisted of 10,158 patients (69.2% male, Agemed = 48, IQR = 30–67) and for UH 14,129 patients (65.3% male, Agemed = 43, IQR = 28–61). BAMC reported a usual staff of 50 EM physicians and 19 trauma surgeons, and UH reported approximately 44 full-time EM physicians (33 full-time and 22 part-time) and 16 trauma surgeons. Case exposures for each EM physician and trauma surgeon were calculated to be approximately 203 and 535 patients for BAMC, and 321 and 883 for UH. Demographic and injury characteristics for trauma patients seen in each facility are displayed in Table I. Two-proportion Z-tests indicated that there were no significant differences in injury types between the two centers; blunt trauma was the most common injury type (~83% for both centers). For MOI, BAMC treated a significantly greater proportion of falls in comparison to UH (35.4% versus 30.4%; Z = 4.68, p < 0.001). BAMC also received a greater proportion of patients with injuries because of firearms, with the difference marginally significant (7.1 versus 4.7; Z = 1.99, P = 0.054). Of note, UH received a significantly greater proportion of patients with injuries because of “other” mechanisms (eg, fires, assault, bites) than BAMC (30.6% versus 24.2%; Z = −4.53, p < 0.001).
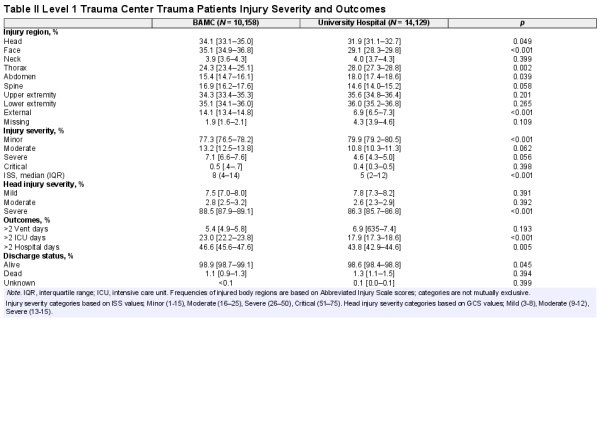
Injury region and severity are displayed in Table II. The majority of patients treated within BAMC and UH suffered lower and/or upper extremity injuries. BAMC received a significantly greater proportion of patients with face injuries (35.1% versus 29.1%; Z = 6.43, p < 0.001) and external injuries (14.1% versus 6.9%; Z = 5.84, p < 0.001) than UH, as well as a marginally significant greater proportion of head injuries (34.1% versus 31.9%; Z = 2.47, p = 0.049). UH received significantly greater proportions of patients with thorax injury than BAMC (28.0% versus 24.3%; Z = −3.33, p = 0.002), as well as injuries to the abdomen (18.0% versus 15.4%; Z = −2.16, p = 0.039). There were no significant differences in proportions of moderate to critical injured patients between the two centers; however, UH received a significantly greater proportion of patients with minor injuries than BAMC (79.9% versus 77.3%; Z = −4.20, p < 0.001). Finally, BAMC received a significantly greater proportion of patients with severe head injuries than UH (88.5% versus 86.3%; Z = 4.79, p < 0.001).
Outcomes and discharge status are displayed in Table II. A significantly greater proportion of BAMC trauma patients spent more than 2 days in the ICU (23.0% versus 17.7%; Z = 4.40, p < 0.001) and in the hospital (46.6% versus 43.8%; Z = 2.97, p = .005) than UH trauma patients; there were no differences in proportion of patients who spent more than 2 days on a ventilator (Z = −1.21, p = 0.193). BAMC had a greater proportion of patients alive at discharge than UH, with a marginally significant difference (98.9% versus 98.7%; Z = −2.08, p = 0.045).
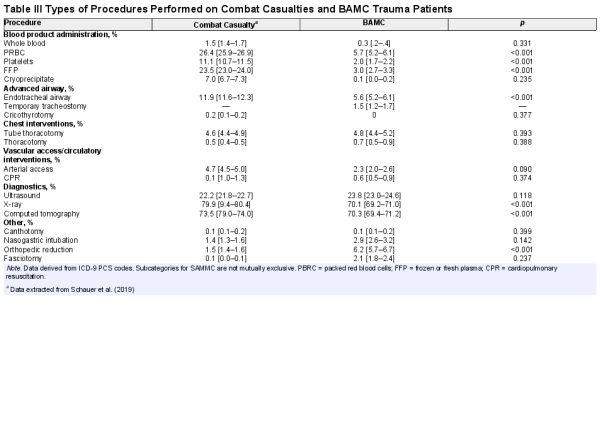
We compared procedures performed on BAMC trauma patients to procedures performed on combat casualties treated in emergency departments in Iraq and Afghanistan, using data from Schauer et al. (see Table III). Within the BAMC sample, the majority of patients underwent diagnostic procedures, including computerized tomography (CT) scans (70.3%), X-rays (70.1%), and ultrasound scans (23.8%). Other common procedures included orthopedic reductions (6.2%), endotracheal airway (5.6%), and tube thoracotomy (4.8%). Other critical procedures occurred at lower rates, including fasciotomy (2.1%), temporary tracheostomy (1.5%), and canthotomy (0.1%). Two-proportion Z-tests revealed a significantly greater proportion of combat casualties received PRBC (26.4% versus 5.7%; Z = 11.79, p < 0.001), platelets (11.1% versus 2.0%; Z = 4.44, p < 0.001), and fresh or frozen plasma (23.5% versus 3.0%; Z = 9.10, p < 0.001) than BAMC patients. In addition, significantly greater proportions of combat casualties received endotracheal airways (11.9% versus 5.6%; Z = 4.60, p < 0.001), X-rays (79.9% versus 70.1%; Z = 17.24, p < 0.001), and CT scans (73.5% versus 70.3%; Z = 5.27, p < 0.001). A significantly greater proportion of BAMC patients underwent orthopedic reductions than combat casualties (6.2% versus 1.5%; Z = −4.59, p < 0.001).
Discussion
We found little difference between the trauma patients treated at the military level 1 trauma center, BAMC, and those treated at the closest civilian level 1 trauma center, UH. The centers had similar injury types and injury severity, indicating parity between the hospitals. A significantly greater proportion of patients at BAMC spent more than two days in hospital and in the ICU in comparison to UH, possibly related to the higher incidence of severe head injury in the BAMC population. In addition, though not statistically significant, BAMC also treated more patients with an ISS in the severe category (7.1% versus 4.6%). During our study period, UH treated 3,971 more adult trauma patients than BAMC, with estimated exposure rates per physician higher for both EM physicians and trauma surgeons in the civilian center. The opportunity for military physicians to rotate through UH emergency services may increase case exposure and enhance deployment readiness.
Differences were seen in the mechanism of injury, with BAMC treating significantly more patients injured from falls and firearms. BAMC patients were significantly older than UH patients, and many of the falls treated at BAMC are older adult dependents with prior service who are routed to BAMC because of eligibility for MHS care. Proportions of blunt (BAMC: 83% and UH: 83.5%) and penetrating (BAMC: 16.9% and UH 14.7%) injuries were similar to those observed in another urban civilian level 1 trauma center (81.5% and 15.7%, respectively). Based on published reports from recent conflicts in Iraq and Afghanistan, the majority of patients treated in combat settings had penetrating injuries (29–63%) because of explosives (48.3–77.0%). Except for in instances of terroristic bombing or mass shootings, trauma centers outside of war zones do not typically treat high numbers of patients with blast injuries.
For injury regions, a majority of patients were treated for extremity injuries at both trauma centers. BAMC treated more patients with facial and head injuries, and a greater portion were severe head injuries; UH saw more patients with thorax and abdominal injuries. In combat casualties, the most common body regions injured were extremities (23.9–49.7%) and head/neck (14.8–57.5%). This is not surprising, considering one of the most common mechanisms of injury during recent conflicts were improvised explosive devices, and that body armor would lend protection to the soldiers’ chest and abdomen.
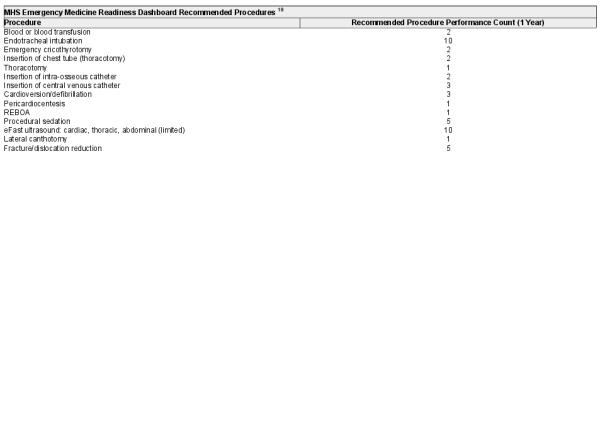
In our comparison of procedures performed at BAMC to those performed in the in-theater emergency departments, the most notable differences were in the larger percentage of endotracheal intubations performed, and blood products administered to the combat casualty patients. All other procedures were performed at similar rates when comparing BAMC to the combat setting, with the exception of orthopedic reduction, X-rays, and CT scans (increased in BAMC patients). Differences in these three procedures may be linked to the differences in mechanism of injury. Blast mechanism of injury on the battlefield frequently leads to injuries not amenable to reduction, including major limb destruction and amputation. The MHS Readiness Dashboard for emergency medicine lists 14 required procedures for deployment readiness (see Appendix B). Although we were unable to determine specific metrics of procedure performance per physician, the results provide information on opportunities physicians had to perform eight of the listed procedures within the BAMC emergency department. The limited opportunities for performance of blood product administration and endotracheal intubation in the BAMC ED relative to combat casualty settings may point to a need to supplement predeployment training with simulation or other patient care opportunities. Further research needs to be done to determine the exact metrics per physician, per year, and to compare to predeployment-required procedures and procedure counts.
Even with the trauma experience in MHS facilities and existing civilian-military partnerships, there has been ongoing concern that the peacetime mission of the MHS is not sufficient to maintain medical readiness for wartime deployments. The results of our study demonstrate the important role of the only DoD level 1 trauma center in supporting the readiness of emergency care physicians and trauma surgeons and point to certain procedural experiences potentially in need of further supplementations. We also elucidate an opportunity to increase trauma exposure by building on the relationship between BAMC and the UH trauma centers. The San Antonio Uniformed Services Health Education Consortium (SAUSHEC) has an established partnership with UH, which allows military trainees to complete rotations in the UH trauma center. Expanding this agreement to include military physicians would increase trauma case exposure and result in enhanced readiness. Further research and more detailed data are needed on the case metrics and experiences of emergency medicine physicians and trauma surgeons. The MHS can use the data to determine what additional learning experiences are required to meet the recommended requirements for combat casualty care.
Limitations
The current study is not without limitations. This study is based on registry data and we are unable to link the procedures or other data to specific physician type. We can only describe the exposure potential in each setting. Although data support the notion that medical personnel trained at BAMC are able to perform procedures critical for emergency care in war zones, they do not provide information on the quality or successful performance of personnel. In spite of the fact that we submitted similar data requests to the two trauma registries, the returned data sets were different and made some comparisons difficult to complete. Because of the large sample within the current study, differences between BAMC and UH may not hold practical significance despite reaching statistical significance. ICD-9-PCS codes were used to calculate the frequency of procedures within the BAMC sample and these codes may not fully account for all procedures performed in the combat ED settings. Finally, rates of procedures found within BAMC, a level 1 trauma center, may not reflect opportunities provided by other facilities, including the two level 2 and two level 3 trauma centers within the MHS.
Conclusions
The trauma patients treated at a military level 1 trauma center were similar to those treated in the civilian level 1 trauma center in the same city, indicating the effectiveness of the only DoD level 1 trauma center to provide experience comparable to that provided in civilian trauma centers. However, further research is needed to determine if the exposure rates to specific procedures are adequate to meet predeployment readiness requirements.
ACKNOWLEDGMENTS
Brooke Army Medical Center Trauma Program: Jason Forcum, RN & Gina Pickard, BSN, RN; University Health Systems: Trauma Registry - Michael Shiels, MSN, RN & Tracy Cotner-Pouncy, RN; UT Health SA Trauma Research - Rachelle Jonas RN.
The views expressed are solely those of the authors and do not reflect the official policy or position of the US Army, US Navy, US Air Force, the Department of Defense, or the US Government.
References
- 1.
- 2.
- 3.
- 4. Thorson CM, Dubose JJ, Rhee P, et al: Military trauma training at civilian centers: a decade of advancements. J Trauma Acute Care Surg2012; 73: S483–9.
- 5. Allen CJ, Straker RJ, Murray CR, et al: Recent advances in forward surgical team training at the US Army trauma training department. Mil Med2016; 181: 553–9.
- 6. Place RJ, Porter CA, Azarow K, Beitler AK: Trauma experience comparison of army forward surgical team surgeons at ben Taub hospital and Madigan Army medical center. Current Surg2001; 58: 90–3.
- 7. Schreiber MA, Holcomb JB, Conaway CW, Campbell KD, Wall M, Mattoz KL: Military training performed in a civilian trauma center. J Surg Res2002; 104: 8–14.
- 8. Maureen M, York GB, Hirshon JM, Jenkins DH, Scalea TM: Trauma readiness training for military deployment: a comparison between a U.S. trauma center and an air force theater hospital in Balad, Iraq. Mil Med2011; 176: 769–76.
- 9. Hight RA, Salcedo ES, Martin SP, Cocanour CS, Utter G, Galante JM: Level I academic trauma center integration as a model for sustaining combat surgical skills: the right surgeon in the right place for the right time. J Trauma Acute Care Surg2015; 78: 1176–81.
- 10. Saldanha V, Yi F, Lewis JD, Ingalls NK: Staying at the cutting edge: partnership with a level 1 trauma center improves clinical currency and wartime readiness for military surgeons. Mil Med2016; 181: 459–62.
- 11. Hall A, Speegle D, Glaser J: Civilian-military trauma partnerships and the visiting surgeon model for maintaining medical readiness. J Surg Ed2018; 00: 1–7.
- 12. Schauer SG, Naylor JF, Oliver JJ, Maddry JK, April MD: An analysis of casualties presenting to military emergency departments in Iraq and Afghanistan. Am J Emerg Med2019; 37: 94–9.
- 13. Howard JT, Kotwal RS, Turner CA, et al: Use of combat casualty care data to assess the US military trauma system during the Afghanistan and Iraq conflicts, 2001-2017. JAMA Surg2019; 154: 600–608;. doi: .
- 14. Janak JC, Mazuchowski EL, Kotwal RS, et al: Patterns of anatomic injury in critically injured combat casualties: a network analysis. Sci Rep2019; 9: 13767. doi: .
- 15. Lairet J, Bebarta VS, Maddry JK, et al: Prehospital interventions performed in Afghanistan between November 2009 and march 2014. Mil Med2019; 184: 133–7.
- 16. Kotwal RS, Staudt AM, Trevino JD, et al: A review of casualties transported to role 2 medical treatment facilities in Afghanistan. Mil Med2018; 183: 134–45.
- 17. Morrison JJ, Oh J, DuBose JJ, et al: En-route care capability from point of injury impacts mortality after severe wartime injury. Annals of Surg2013; 257: 330–4.
- 18.
- 19. Hutter PJ, Roski J, Woodson J, et al: Overview readiness of medical providers in the military health system: overview of operational and policy considerations. Health Aff2019; 38: 1274–80.
- 20.