INTRODUCTION
Large-scale combat operations will create many new challenges for combat casualty medical care not seen during the past two decades of operations during the Global War on Terrorism. In near-peer combat operations, the enemy will have significant and layered antiair assets, which severely restricts access to aerial medevac. Consequently, time between the point of injury (POI) and arrival at an established medical facility where deliberate damage control resuscitation and surgery will occur may increase. During the Global War on Terrorism, up to 67% of casualties arrived to surgical capability within the first hour after sustaining injuries, the so-called “Golden Hour.”, In near-peer conflicts, presurgical care may span hours or days instead of minutes.,
Soldiers wound in action and sustaining penetrating injuries or open fractures are at high risk of developing infection., Penetrating abdominal trauma may result in infection between 4% and 31% of the time. Open fractures also significantly increase risk of developing infection, although rates are dependent on severity of injury, host factors, and fracture location. Approximately one-fourth of combat-related type III open tibial fractures resulted in deep wound infections., It is unclear how time to first administration of antibiotics impacts the risk of developing infection., Nevertheless, evidence suggests that prophylactic antibiotics improve infection-related outcomes for open fractures and that infection risk increases dramatically hours after wound colonization., Other studies have suggested that early antibiotic administration, within 3 h of injury, is the most important factor in preventing infection., Accordingly, current Tactical Combat Casualty Care (TCCC) guidelines recommend antibiotic prophylaxis (moxifloxacin for casualty who can take oral medicine versus ertapenem for others) for all open combat wounds. Studies implicate a broad array of infectious agents against which protection is necessary. These include Gram-negative (e.g., Acinetobacter, Enterobacter, Escherichia coli, and Pseudomonas) and Gram-positive bacteria (Coagulase-negative Staphylococci and Enterococcus). Other agents include mold or yeast and anaerobes.
This paper builds upon the current body of knowledge by utilizing the Department of Defense Trauma Registry (DODTR) to explore associations with prehospital administration of antibiotics among combat casualties with open wounds. Specifically, we examined demographics, procedures, and medicines administered with the intent of generating hypotheses for future research to explain reasons why casualties do or do not receive antibiotics.
MATERIALS AND METHODS
Study Design and Setting
We conducted a retrospective cohort analysis of combat casualties captured as part of the DODTR. Details of this registry and methodology of data abstraction were described previously., The U.S. Army Institute of Surgical Research (USAISR) regulatory office reviewed protocol H-20-015nh and determined that it was exempt from Institutional Review Board review. We obtained only deidentified data.
Selection of Participants
We identified subjects undergoing emergency department interventions as trauma patients in Iraq and Afghanistan from January 2007 to August 2016. We have previous published details of the specific search terms utilized. Within the database, we searched for all subjects with a documented open wound regardless of mechanism. The senior author (S.G.S.) made the determination of which wounds were open based upon assessment of the International Classification of Diseases (ICD) codes. We included only those subjects with an abbreviated injury scale (AIS) score of 1 or greater in the neck, thorax, abdomen, or spine (body regions 3-6) to restrict our capture to those subjects with significant wounds most likely to require antibiotic prophylaxis. Our intent was to highlight the population most likely to benefit from the intervention under study.
Data Collection
The DODTR, formerly known as the Joint Theater Trauma Registry, is the Department of Defense’s data repository for traumatic injuries., The DODTR includes information on demographics, injury producing incidents, diagnoses, treatments, and outcomes of injuries sustained by U.S./non-U.S. Military and U.S./non-U.S. civilian personnel in wartime and peacetime (including humanitarian) from the POI to final disposition. Short-term outcome data are also available for non-U.S. casualties. The DODTR comprises all patients admitted to a Role 3 (fixed-facility) or forward resuscitative surgical detachment (FRSD) with an ICD 9th Edition (ICD-9) diagnosis of traumatic injury (ICD-9 between 800 and 959.9), near-drowning/drowning with associated injury (ICD-9 994.1), or inhalational injury (ICD-9 987.9), and trauma occurring within 72 h from presentation.
We defined the prehospital setting as any location before reaching surgical capabilities, such as an FRSD or field hospital (Role 3). This definition included Role 1 (POI, casualty collection point, and battalion aid station) and Role 2 (temporary, limited capability forward-positioned hospital inside the combat zone without surgical support) facilities. We categorized interventions performed upon arrival at the FRSD or field hospital as emergency department and not prehospital.
We collected data on casualty characteristics to include demographics, mechanism of injury, AIS, and survival to hospital discharge. We also collected data on procedures performed related to hemorrhage control, airway management, pneumothorax treatment, and volume replacement. Finally, we included specific medications administered including not only antibiotics but also analgesic medicines. The primary intervention of interest was prehospital administration of antibiotics. We also collected data on which antibiotics were administered and by which route. We categorized subjects as having received no antibiotics if their data did not include a specific type of antibiotic or if the antibiotic was only administered topically (including ocular administration). We compared all measured characteristics including demographics, procedures, and medicines administered between antibiotics recipients and nonrecipients to identify adherence to TCCC guidelines.
Data Analysis
We performed all statistical analyses using Microsoft Excel (version 10, Redmond, Washington) and JMP Statistical Discovery from SAS (version 13, Cary, NC). We compared study variables between the patients receiving prehospital antibiotics versus patients not receiving prehospital antibiotics. We used a Student t-test for continuous variables, the Wilcoxon rank sum test for ordinal variables, and the Pearson chi-squared test for nominal variables. We reported categorical variables as numerators with percentages, ordinal variables as medians with interquartile ranges, and continuous variables as means with standard deviations. For groups demonstrating differences in our primary outcome of mortality between subjects receiving prehospital antibiotics versus no prehospital antibiotics, we constructed regression models to control for potential confounders.
RESULTS
We identified 18,366 encounters meeting inclusion criteria. U.S. Military casualties comprised the largest proportion (n = 6945) of subjects followed by non-North Atlantic Treaty Organization (NATO) military forces (n = 5353). The median age was 25 years (interquartile range 21-30). The most common mechanisms of injury were explosives (56.6%), followed by firearms (32.4%). Most patients survived to hospital discharge (96.2%).
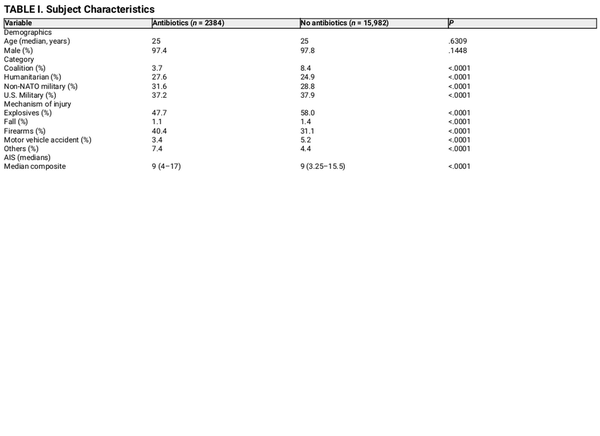
Antibiotic recipients (n = 2384) were comparable to nonrecipients (n = 15,982) with regard to age and sex. Antibiotic recipients were more likely to be non-NATO military or humanitarian casualties, more likely to have sustained injuries from firearms, and less likely to have sustained injuries from explosives (Table I).
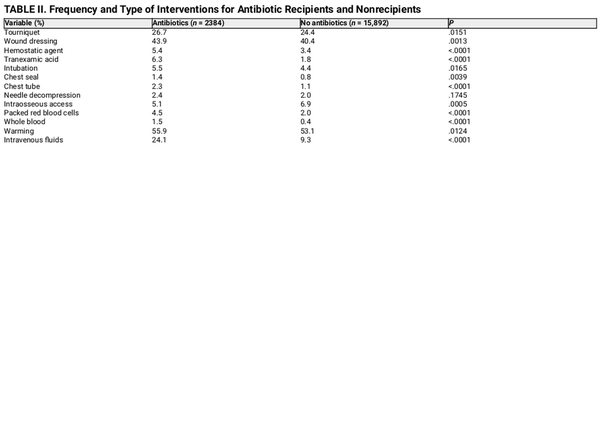
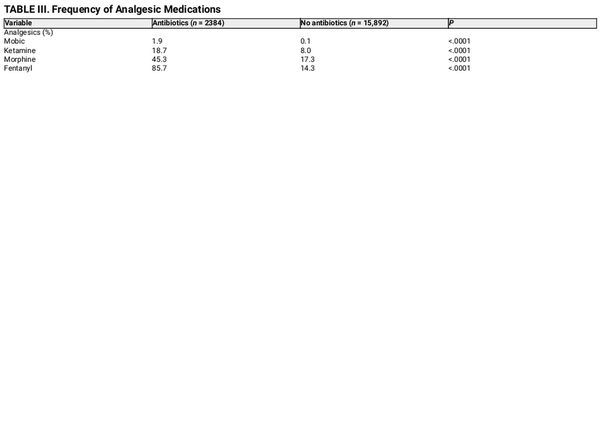
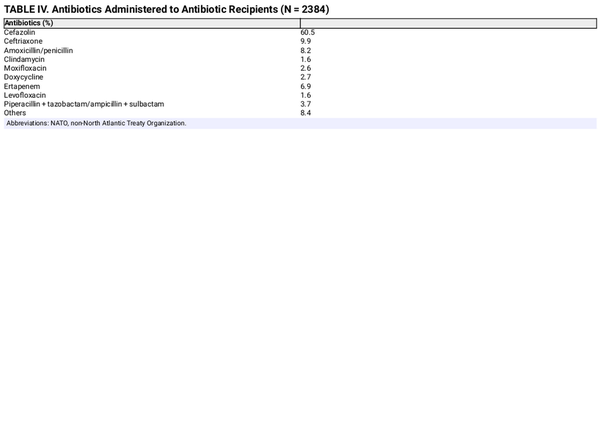
The most common interventions performed either prehospital or following military treatment facility arrival (including surgery) were limb wound warming, dressings, tourniquets, fluids, and pain medications. Antibiotic recipients were more likely to have received any intervention (Table II). Morphine was the most administered analgesic, followed by fentanyl and ketamine. Antibiotic recipients were more likely to receive all analgesic medication (Table III). Cefazolin was the most commonly administered antibiotic (60.5%, Table IV).
Antibiotic recipients had a slightly higher survival to hospital discharge than nonrecipients (97.4% versus 96.0%, P < .001). The multivariate logistics regression model identified several associations with prehospital antibiotic administration, including tachycardia (heart rate over 100 beats per minute; OR 3.4, 95% CI, 1.1-10.5), intubation (OR 2.0, 95% CI, 1.1-3.8), and administration of tranexamic acid (OR 5.6, 95% CI, 1.2-26.5). The other characteristics and interventions included in univariate analyses (Tables II and III) were not associated with prehospital antibiotic receipt in the multivariate regression analysis.
DISCUSSION
In this study, we analyzed the associations between prehospital administration of antibiotics to combat trauma casualties and their demographics, mechanism of injury, other interventions received, and survival. U.S. Military personnel comprised the largest proportion of subjects receiving prehospital wound prophylaxis, closely followed by non-NATO military personnel. Only 13% of all subjects meet indications for prehospital systemic antibiotic therapy per TCCC guidelines. This is alarming, as antibiotic prophylaxis for open fractures has been associated with a lower rate of infection, and early administration of antibiotics after injury may significantly reduce infection rates when compared to delayed administration.
Some groups were more likely than others to receive prehospital antibiotics. Specifically, patients recorded having heart rates above 100 beats per minute were more likely to have received prehospital antibiotics (OR 3.4). Similarly, patients requiring tranexamic acid (OR 5.6) or intubation (OR 2.0) were more likely to receive prehospital antibiotics. This is consistent with the expectation that sicker patients are more likely to receive all available prophylactic measures. Conversely, patients experiencing injuries from explosives were less likely to receive antibiotic prophylaxis. It is possible that clinicians overlooked this intervention in the face of complex injury patterns among patients experiencing trauma from explosives requiring myriad additional damage control resuscitation interventions.
The strong association between penetrating injuries and infection makes the prehospital administration of antibiotics a widely recommended intervention, especially when patients are delayed from definitive medical care., There was a clear reduction in infection rates when systemic antibiotic prophylaxis was administered to combat casualties in Iraq. Similarly, prehospital systemic antibiotic administration was associated with lower infection rates and mortality for patients with penetrating and/or open wounds sustained in combat. However, our study demonstrated that only 13% of eligible casualties received this treatment. The retrospective observational design of this study makes it impossible to establish the causative factors for this finding because data points were limited to those already available in the medical records. That said, we suspect that it is multifactorial with contributing factors including medic focus on more immediate life-saving interventions (e.g., hemorrhage control) and lack of emphasis by commanders and during predeployment training given a myriad of competing priorities. Added emphasis in educational curricula such as the Joint Field Hospital Trauma Management Course and Tactical Combat Medical Course, among others, coupled with increased command emphasis will likely have a material impact on improving compliance with antibiotic administration guidelines.
Other examples of suboptimal adherence to TCCC guidelines for combat casualties exist. Only 4.1% of combat casualties undergoing massive transfusion (10+ units of blood product transfusion) within 24 h received tranexamic acid, despite a clear indication for use., Data from the prehospital setting show similarly low tranexamic acid administration for patients meeting criteria per TCCC guidelines. For patients receiving massive transfusion, there was also poor adherence to balanced resuscitation TCCC guidelines, specifically with regard to the use of platelet products. Other interventions with suboptimal compliance with TCCC guidelines include minimization of crystalloid for resuscitation of patients with hemorrhage, battlefield analgesia,, and chest seal placement.
Recent studies suggest that prehospital antibiotic prophylaxis very likely reduces the risk of infection for open fractures and penetrating injuries. One of the important goals of orthopedic care of open fractures is early identification and timely administration of appropriate antibiotics. There is a clear benefit when antibiotics are given within 3 h after injury, with infection rates increasing from 4.7% to 7.4% if antibiotics are delayed beyond 3 h. These findings, in addition to our own, highlight the importance of compliance with TCCC guidelines for early, prehospital antibiotic administration for appropriate patients. This will likely require ongoing efforts to pursue clinical opportunities for military personnel outside of military treatment facilities given relatively low procedural volume and case complexity in these locations—increased exposure to patients with significant trauma leading to open wounds will provide more repetitions for the medical force to become familiar with the TCCC antibiotic guidelines. In addition to command emphasis, other important measures might include checklists, ongoing education (e.g., added emphasis in existing courses such as Tactical Combat Medical Care course), and ongoing quality assurance monitoring by the Joint Trauma System.
Prehospital antibiotic administration will take on added importance in future conflicts. The Army’s current operating concept (multidomain operations) envisions a spectrum of violence to include large-scale combat operations. In this kinetic environment, lack of air superiority coupled with contested ground lines of communication will preclude rapid evacuation for many casualties. Prolonged hold times will potentially magnify the clinical impact of prehospital antibiotic administration.
Limitations
Our study has several limitations. First, we did not have data on the amount of time between POI and administration of antibiotics. This makes it impossible for us to assess the time-based relationship between the intervention under study and outcomes although it is conceivable that earlier administration of antibiotics after injury may yield better outcomes. Second, we did not have access to the original patient records as part of this does not have any salient data points. For example, there was a lack of information on antibiotic dosages. Third, all subjects in this study were alive upon arrival to hospital facilities. The exclusion of nonsurvivors may have prevented us from analyzing prehospital administration of antibiotics in the most serious cases. This may have skewed our results in various ways, limiting our understanding of prehospital antibiotic administration in more severely injured casualties. That said, we speculate that exclusion of this gravely injured population that rapidly succumbed to noninfectious pathology may lead to understating of the survival benefits of antibiotics in this cohort. Fourth, the available data did not include information regarding infection occurring posthospital treatment and does not inform our understanding of other factors that could impact infection risk such as wound management techniques. Fifth, as a strictly observational and retrospective study, we cannot establish causal relationships. The retrospective design places the data at risk of errors to include recall bias, which may impact our measured outcomes. We lacked control over data collection, and it is likely that the dataset lacks information on many confounding variables, limiting the strengths of our conclusions. Indeed, the DODTR itself has inherent limitations because of incomplete information. The absence of relevant data points as noted earlier hinders a comprehensive analysis. We also cannot speak to the reasons for our findings of suboptimal compliance with TCCC recommendations to include the extent that our findings may simply represent limitations in documentation. Finally, we restricted our analysis to patients with significant injuries (as determined by AIS > 1) to the neck, thorax, abdomen, or spine. Our intent in doing so was to capture those casualties most likely to require antibiotic prophylaxis, but this limits the generalizability of our findings to a broader population of combat casualties. We do not stratify our findings by specific body region of injury although this would be an interesting area for future studies to examine.
CONCLUSION
Administration of prehospital antibiotics occurs infrequently for U.S. Military patients despite recommendations from the TCCC for early antibiotics in patients with open wounds. Non-NATO military forces were given prehospital antibiotics more frequently. There was an association between injury severity, indicated by tachycardia and intervention of intubation and tranexamic acid, and administration of prehospital antibiotics. These findings highlight the need for additional educational and quality assurance initiatives to improve adherence to TCCC guidelines with regard to prehospital antibiotic administration. Future studies are necessary to determine reasons for suboptimal TCCC guideline compliance. This will become increasingly important in the event of future conflicts with near-peer adversaries.
ACKNOWLEDGMENTS
The authors acknowledge the DODTR for providing the data for this study.
REFERENCES
- 1. April MD, Stednick PJ, Christian NB: A descriptive analysis of notional casualties sustained at the joint readiness training center: implications for health service support during large-scale combat operations. Med J (Ft Sam Houst Tex) 2021; 3–8.
- 2. Kotwal RS, Howard JT, Orman JA, et al: The effect of a golden hour policy on the morbidity and mortality of combat casualties. JAMA Surg 2016; 151(1): 15–24.doi: .
- 3. Shackelford SA, Del Junco DJ, Mazuchowski EL, et al: The golden hour of casualty care: rapid handoff to surgical team is associated with improved survival in war-injured US service members. Ann Surg 2023; in press.doi: .
- 4. Keenan S, Riesberg JC: Prolonged field care: beyond the “Golden Hour”. Wilderness Environ Med 2017; 28(2S): S135–9.doi: .
- 5. Keenan S: Deconstructing the definition of prolonged field care. J Spec Oper Med 2015; 15(4): 125.doi: .
- 6. Tribble DR, Murray CK, Lloyd BA, et al: After the battlefield: infectious complications among wounded warriors in the trauma infectious disease outcomes study. Mil Med 2019; 184(Suppl 2): 18–25.doi: .
- 7. Klaus J, Bereswill S, Heimesaat M: Pre-hospital systemic antibiotic prophylaxis for penetrating trauma: is the military usage applicable to civil emergency medical services? A mini-review. Curr Trends Microbiol 2020; 14: 21–9.
- 8. Murray C: Field wound care: prophylactic antibiotics. Wilderness Environ Med 2017; 28(2S): S90–S102.doi: .
- 9. Collinge C, McWilliams-Ross K, Kelly K, et al: Substantial improvement in prophylactic antibiotic administration for open fracture patients: results of a performance improvement program. J Orthopedic Trauma 2014; 28(11): 620–5.doi: .
- 10. Burns T, Stinner D, Mack A, et al: Microbiology and injury characteristics in sever open tibia fractures from combat. J Trauma Acute Café Surg 2012; 72(4): 1062–7.doi: .
- 11. Penn-Barwell JG, Bennett PM, Mortiboy DE, Fries CA, Groom AF, Sargeant ID: Factors influencing infection in 10 years of battlefield open tibia fractures. Strategies Trauma Limb Reconstr 2016; 11(1): 13–8.doi: .
- 12. Zuelzer DA, Hayes CB, Hautala GS, et al: Early antibiotic administration is associated with a reduced infection risk when combined with primary wound closure in patients with open tibia fractures. Clin Orthop Relat Res 2021; 479(3): 613–9.doi: .
- 13. Lloyd BA, Murray CK, Shaikh F, et al: Infectious disease clinical research program trauma infectious disease outcomes study group. Antimicrobial prophylaxis with combat-related open soft-tissue injuries. Mil Med 2018; 183(9-10): e260–5.doi: .
- 14. Grote S, Polzer H, Prall W, et al: Prevention of infection in the current treatment of open fractures: an evidence-based systematic analysis. Orthopade 2012; 41(1): 32–42.doi: .
- 15. Quinn R, Macias D: The management of open fractures. Wilderness Environ Med 2006; 17(1): 41–8.doi: .
- 16. Melamed E, Blumenfeld A, Kalmovich B, et al: Israeli defense forces medical corps consensus group on prehospital care of orthopedic injuries. Prehosp Disaster Med 2007; 22(1): 22–5.doi: .
- 17. Hospenthal D, Murray C, Andersen R, et al: Guidelines for the prevention of infection after combat-related injuries: 2011 update: endorsed by the Infectious Diseases Society of America and the Surgical Infection Society. J Trauma 2011; 71(2 Suppl 2): S210–34. doi: .
- 18. Anonymous A: Tactical Combat Casualty Care (TCCC) guidelines for medical personnel 15 December 2021. J Spec Oper Med 2022; 22(1): 11–7.doi: .
- 19. TerBeek BR, Loos PE, Pekari TB, Tennent DJ: Efficacy of vancomycin powder in mitigating infection of open penetrating trauma wounds on the battlefield: an evidence-based review. J Spec Oper Med 2022; 22(1): 76–80.doi: .
- 20. Mende K, Stewart L, Shaikh F, et al: Microbiology of combat-related extremity wounds: trauma infectious disease outcomes study. Diagn Microbiol Infect Dis 2019; 94(2): 173–9.doi: .
- 21. Schauer SG, Naylor JF, Hill GJ, Arana AA, Roper JL, April MD: Association of prehospital intubation with decreased survival among pediatric trauma patients in Iraq and Afghanistan. Am J Emerg Med 2018; 36(4): 657–9.doi: .
- 22. April MD, Becker TE, Fisher AD, Naylor JF, Schauer SG: Vital sign thresholds predictive of death in the combat setting. Am J Emerg Med 2021; 44: 423–7.doi: .
- 23. Schauer SG, Naylor JF, Oliver JJ, Maddry JK, April MD: An analysis of casualties presenting to military emergency departments in Iraq and Afghanistan. Am J Emerg Med 2019; 37(1): 94–9.doi: .
- 24. Schauer SG, Naylor JF, April MD, et al: Prehospital resuscitation performed on hypotensive trauma patients in afghanistan: the prehospital trauma registry experience. Mil Med 2019; 184(5-6): e154–7.doi: .
- 25. Schauer SG, Wheeler AR, April MD, et al: An analysis of the pediatric casualties undergoing massive transfusion in Iraq and Afghanistan. Am J Emerg Med 2020; 38(5): 895–9.doi: .
- 26. Lack W, Karunaker M, Angerame M, et al: Type III open tibia fractures: immediate antibiotic prophylaxis minimizes infection. J Orthopedic Trauma 2015; 29(1): 1–6.doi: .
- 27. Gerhardt R, Matthews J, Sullivan S: The effect of systemic antibiotic prophylaxis and owund irrigation on penetrating combat owunds in a return-to-duty population. Prehosp Emerg Care 2009; 12(4): 500–4.doi: .
- 28. Smit L, Boyle M: antibiotic prophylaxis in prehospital trauma care: a review of the literature. Australas J Paramedicine 2014; 11: 1–8.doi: .
- 29. April MD, Fisher AD, Bridwell RE, et al: Massive transfusion thresholds associated with combat casualty mortality during operations in Afghanistan and Iraq: implications for role 1 logistical support chains. Med J (Fort Sam Houston, Tex) 2023; 11–7.
- 30. Fisher AD, Carius BM, April MD, Naylor JF, Maddry JK, Schauer SG: An analysis of adherence to tactical combat casualty care guidelines for the administration of tranexamic acid. J Emerg Med 2019; 57(5): 646–52.doi: .
- 31. Schauer SG, April MD, Naylor JF, et al: Prehospital administration of tranexamic acid by ground forces in Afghanistan: the prehospital trauma registry experience. J Spec Oper Med 2017; 17(3): 55–8.doi: .
- 32. April MD, Fisher AD, Hill R, et al: Adherence to a balanced approach to massive transfusion in combat casualties. Mil Med 2023; 188(3-4): e524–30.doi: .
- 33. EE C, Hamm J, Fisher AD, et al: Trends in prehospital blood, crystalloid, and colloid administration in accordance with changes in tactical combat casualty care guidelines. Mil Med 2022; 187(11-12): e1265–70.doi: .
- 34. Schauer SG, Fisher AD, April MD, et al: Battlefield analgesia: adherence to tactical combat casualty care guidelines. J Spec Oper Med 2019; 19(1): 70–4.doi: .
- 35. Schauer SG, Naylor JF, Maddry JK, Hinojosa-Laborde C, April MD: Trends in prehospital analgesia administration by US forces from 2007 through 2016. Prehosp Emerg Care 2019; 23(2): 271–6.doi: .
- 36. Schauer SG, April MD, Naylor JF, et al: Chest seal placement for penetrating chest wounds by prehospital ground forces in Afghanistan. J Spec Oper Med 2017; 17(3): 85–9.doi: .
- 37. Patzakis MJ, Wilkins J: Factors influencing infection rate in open fracture wounds. Clin Orthop Relat Res 1989; 243: 36–40.doi: .
- 38. Carius BM, April MD, Schauer SG: Procedural volume within military treatment facilities-implications for a ready medical force. Mil Med 2020; 185(7–8): e977–81.doi: .