INTRODUCTION
Navy Dentistry faces complex and demanding environments which mandate high levels of operational dental readiness to reduce preventable dental emergencies for deployed Sailors and Marines. As a result, providers at all levels search for mechanisms to improve oral health, dental readiness, and deployability. With the advent of computer-aided design/computer-assisted manufacturing (CAD/CAM) technologies, new dental treatment delivery options can be provided to broaden access to care and enhance oral health, while sustaining a high level of readiness. Dental CAD/CAM systems not only support the timely delivery of restorative care but also affect how military dental personnel fabricate and place restorations.
Briefly, dental restorations are materials or prostheses used to treat missing or decayed teeth and oral structures in efforts to restore form and function. Restorative procedures can be broadly categorized as direct or indirect. Direct restorative procedures are characterized by placement of soft or malleable materials, such as dental amalgam or resin-based composites directly into tooth preparations. These materials harden shortly after placement through a chemical reaction or light-induced polymerization process. Indirect restorations are typically placed when substantial amounts of tooth structure must be replaced, or a complete-coverage restoration is required to protect the tooth. Crowns, inlays, onlays, and veneers are examples of indirect restorations and comprise materials including ceramics, metal-ceramic hybrids, and cast-gold alloys.
The workflow for treating a patient utilizing a traditional indirect dental restoration, such as a crown, involves several time-consuming steps (Fig. 1). Following preparation of a decayed or damaged tooth, an impression or imprint of the tooth and associated dental arch is accomplished using an elastomeric material. At this stage, a chairside interim restoration is made for the patient. The purpose of an interim restoration is to protect the tooth from external insult during the time required to fabricate a definitive restoration. Interim restorations are made of resins or acrylic materials and are intended to survive for several weeks. Deployment of personnel with one or more interim restoration is problematic, since most Sailors and Marines are deployed without close dental support. These short-term dental restorations are prone to dislodgment and/or fracture when left in place for extended periods, potentially resulting in at-sea or in-field dental emergencies requiring mission-hampering transport of affected personnel to dental facilities.
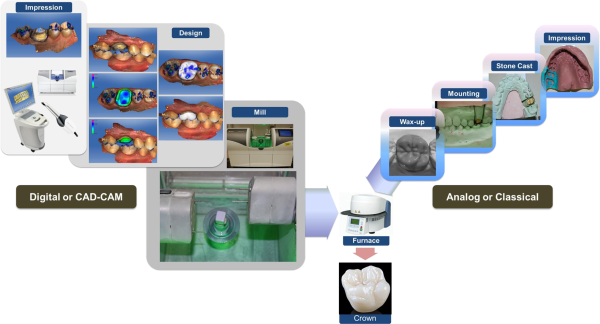
FIGURE 1
Images of digital and classical dental prosthetic workflow.
In a conventional (i.e., non-deployed, non-emergency) situation, fabrication and placement of an interim restoration are followed by a series of laboratory procedures. The impression that was generated in a clinical setting is forwarded to a dental laboratory for performance of traditional “analog” procedures. The impression is used to generate a replica of the patient’s tooth. A dental laboratory technician then completes a series of technically demanding analog procedures to generate a restoration, which meets precise anatomic, functional, and esthetic requirements.
It is important to recognize, the traditional analog workflow generally requires at least two clinical appointments. Due to the high operational tempo and short periods available to prepare for deployments, the time required to accomplish the foregoing procedures may preclude such therapy. Furthermore, if the process is initiated and the service member is deployed before the definitive restoration can be placed, the risk of a dental emergency during deployment is increased due to potential failure of an interim restoration.
In contrast, the CAD/CAM workflow utilizes digital technology for scanning, designing, and producing a dental restoration or prosthesis (Fig. 1). The scanning device digitizes the prepared surfaces of one or more teeth into three dimensional (3D) units of information that are used by software to translate real-world objects into digital representations. The scanning process is intended to provide the same spatial information captured in the analog impression, but is performed using topographic mapping of the teeth and adjacent soft tissues. While there are instances in which a provider may select an analog impression procedure, direct scanning of the oral cavity eliminates the need for impression trays, the associated impression material, dental stone, etc. Moreover, the operator is able to minimize or eliminate delays associated with dental cast fabrication, cast segmentation, and die trimming. Instead, the operator is able to interact with a CAD software to design a restoration which satisfies biologic and functional requirements.– The desired unit may then be fabricated using CAM fabrication technologies (i.e., milling, selective laser melting/sintering, etc).
Clinical data indicate the long-term performance and survivability of digitally fabricated restorations are comparable to those generated by analog means, which makes digitally fabricated restorations a viable alternative to traditional restorations.– By leveraging digital technologies, CAD/CAM workflow yields streamlined processes and supports same-day restorative solutions. Notably, milled restorations can be delivered during a single clinical visit, without the need for interim placement. This approach can positively impact dental health status and readiness posture, and can reduce non-battle injuries of deployed military service members, which Simecek et al. reported to be 15% in recent conflicts.
The objective of this investigation was to compare the placement rates of digitally fabricated indirect restorations with those of traditional direct restorations (i.e., dental amalgam restorations, composite resin restorations) and indirect restorations fabricated using traditional processes (i.e., ceramic crowns, metal-ceramic crowns).
METHODS
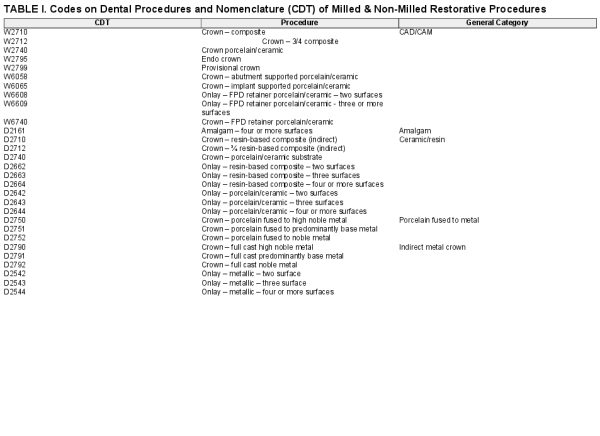
All dental procedures completed by U.S. Navy dentists at Navy and Marine Corps dental treatment facilities (DTFs) are recorded in the Dental Common Access System (DENCAS) or the Corporate Dental Access system (CDA). Procedure codes are used to track productivity, and are based on the Department of Defense Common Dental Terminology (CDT) Dental Procedure Codes and Dental Weighted Values (DWV). In this investigation, DENCAS and CDA were queried to determine monthly procedure code counts for the items of interest. Monthly totals for dental procedures associated with CAD/CAM and analog restorations from January 2008 through June 2017 were determined and subsequently analyzed. Dental procedure codes for 4+ surface amalgams were also included in the analysis, since these restorations may be used in place of commonly-utilized indirect restorations. Table I summarizes the individual CDT codes queried for this investigation. Individual CDT codes were grouped into categories designated as CAD/CAM, Porcelain Fused to Metal (PFM), Ceramic/Resin, Full Metal Restorations (FMR), and Amalgam.
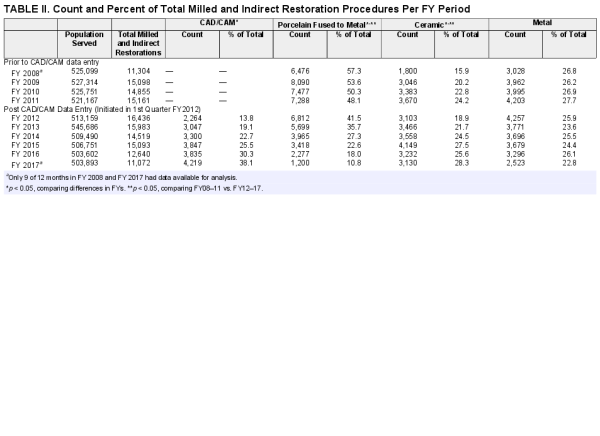
The Navy began tracking CAD/CAM restoration treatment data at the start of federal fiscal year (FY) 2012. Accordingly, data analyzed in this study utilized treatment code counts of traditional direct restorations and indirect laboratory-fabricated restorations since January 2008 and CAD/CAM restoration placement counts since October 2011. Monthly restoration totals were calculated for each general CDT code category listed in Table I and percentages determined (monthly placement percentages) to illustrate how each general category contributed to the total number of coronal restorations per month and FY. Only three-fourths of FY 2008 and 2017 data were included due to the limitations of the procedure code database.
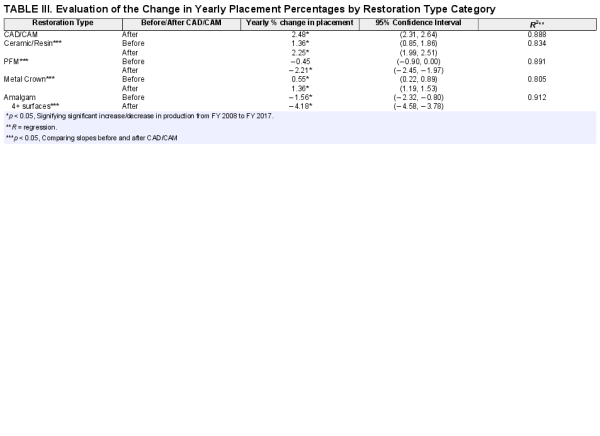
Scatterplots were generated using monthly placement percentages for the prescribed categories and were overlaid with simple linear regression lines and corresponding 95% confidence intervals. Regression analysis was performed for each category to: (1) determine whether monthly placement percentages were significantly increasing, decreasing, or remaining the same before CAD/CAM implementation; (2) determine whether monthly placement percentages were significantly increasing, decreasing, or remaining the same after CAD/CAM implementation; and (3) to determine whether the trends in monthly placement percentages for each category before and after CAD/CAM implementation were significantly different from one another.
Before and after significance was calculated by regression analysis utilizing the following factors: (1) placement percentage per month, (2) a binary indicator variable indicating whether the period was before or after CAD/CAM implementation (October 2011), and (3) an interaction term between the placement percentage and the indicator variable. By introducing the interaction term, significant differences between the monthly placement percentages before and after CAD/CAM implementation were identifiable. Month-over-month changes were multiplied by 12 to indicate a yearly percent change. This study was reviewed by the Naval Medical Research Unit San Antonio Institutional Review Board and determined not to meet the definition of human subject research. Statistical analysis was conducted using SAS v9.4 and R version 3.3.3.
RESULTS
Starting in January 2008, the breakdown of coronal coverage restorations was as follows: 22.0% PFM, 4.4% Ceramic/Resin, 11.3% FMR, and 62.4% Amalgam. By June 2017, the breakdown changed as follows: 28.3% CAD/CAM, 6.8% PFM, 17.73% Ceramic/Resin, 15.8% FMR, and 31.4% Amalgam. The difference in percent contribution between January 2008 and June 2017 is more distinct when Amalgam (direct) restorations are excluded from the analysis (Table II). In January 2008, PFM restorations accounted for 57.3% of all indirect restorations, followed by 26.8% FMR and 15.9% Ceramic/Resin. By June 2017, CAD/CAM restorations accounted for 38.1% of all indirect restorations, followed by 28.3% Ceramic/Resin, 22.8% FMR, and 10.8% PFM.
While CAD/CAM data could only be analyzed beginning in FY 2012, it had the largest yearly percent increase among all treatments (yearly %Δ = 2.48%, 95% CI [2.31%, 2.64%], p < 0.001) (Table III). PFM saw decreases before and after CAD/CAM implementation (Table III, Fig. 2). However, the decreases in the before period (yearly %Δ = −0.45%, 95% CI [−0.90%, 0.00%]) were on the border of established statistical significance (p = 0.052). Marginal yearly decreases during the before CAD/CAM period for PFMs accelerated substantially during the after CAD/CAM period (yearly %Δ = −2.21%, 95% CI [−2.45%, −1.97%], p < 0.001) and significantly differed from the before CAD/CAM period (p < 0.001).
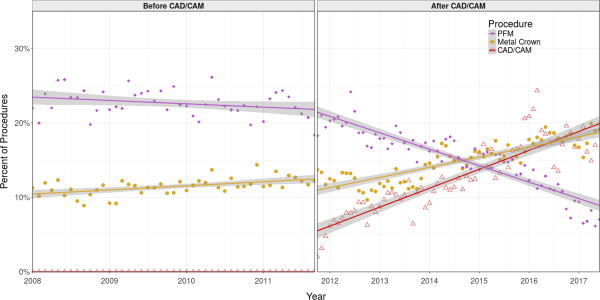
FIGURE 2
Scatterplots of monthly procedures by percent of total restorations comparing porcelain fused to metal (PFM) and Metal Crown to CAD/CAM for both the before (FY 2009-FY 2011) and after (FY 2012-FY 2017) CAD/CAM periods.
Ceramic/Resin restorations displayed increasing utilization from the beginning of the study period (January 2008) to the end of the investigation (June 2017), with a significant yearly increase in the before period (yearly %Δ = 1.36%, 95% CI [0.85%, 1.86%], p < 0.001) and amplified increase in the after period (yearly %Δ = 2.25%, 95% CI [1.99%, 2.51%], p < 0.001) (Table III, Fig. 3). These yearly changes significantly differed between the before and after CAD/CAM implementation period (p = 0.002).
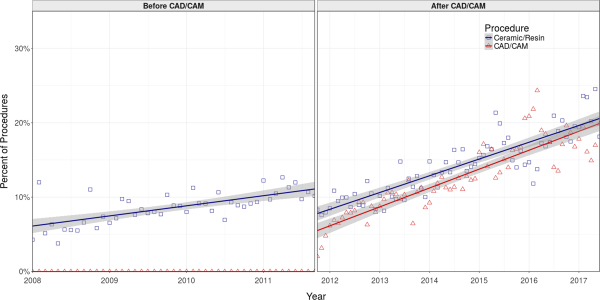
FIGURE 3
Scatterplots of monthly procedures by percent of total restorations comparing complete Ceramic/Resin restorations to CAD/CAM for both the before (FY 2009-FY 2011) and after (FY 2012-FY 2017) CAD/CAM periods.
Increases in FMR restorations in the before period were minimal (yearly %Δ = 0.55%, 95% CI [0.22, 0.89]), but significant (p = 0.001) (Table III, Fig. 2). This upward trend continued in the after period with a substantially significant increase in yearly placement change percentage (yearly %Δ = 1.36, 95% CI [1.19, 1.53] p < 0.001). This increase in the yearly % Δ differed significantly from the before period (p < 0.001).
Amalgam, which contributed the largest percentage of restorations, significantly decreased during the before CAD/CAM implementation period (yearly %Δ = −1.56, 95% CI [−2.32, −0.80], p < 0.001) and intensified after CAD/CAM implementation (yearly%Δ = −4.18, 95% CI [−4.58, −3.78], p < 0.001) (Table III, Fig. 2). Further, the yearly %Δ between the before and after CAD/CAM implementation period was statistically significant (p < 0.001).
DISCUSSION
CAD/CAM and intra-oral optical digital impression systems have been available in dentistry for over 30 years, but have recently become much more predictable with significant advances in scanning, design, and milling technologies., CAD/CAM dentistry, with its improved ease of use, allows dentists in many cases to provide high-quality esthetic indirect restorations to patients in a single appointment, avoid long-term temporization of prepared teeth, and positively impact operational dental readiness. From a practical perspective, the greatest advantage of CAD/CAM in dentistry is the single treatment session concept. This allows tooth preparation, optical impression capture, virtual design, precision milling, customization, and restoration placement in a single session. Digital workflow eliminates several clinical steps which are time-consuming and invasive, as well as the traditional dental laboratory procedures which are technique sensitive and labor intensive.
Digital workflow data accessed from DENCAS and CDA confirm that the percentage of CAD/CAM restorations placed has steadily increased since the Navy started tracking production in October 2011. CAD/CAM represented 17.8% of all coronal coverage restorations and 38.1% of indirect restorations when averaged across the available data for FY 2017. The data reflect a growing acceptance by Navy dental providers of CAD/CAM systems and their benefits. Numerous positive reports have been published in recent years describing the positive clinical properties of CAD/CAM restorations; however, to the best of our knowledge this is the first report to explore placement rates.– This increase in CAD/CAM as well as Ceramic/Resin restorations provides a glimpse into a larger trend in dentistry toward more esthetically appealing restorations in addition to leveraging digital technologies to enhance dental practice. Further evidence suggests that digital workflow in dentistry is more cost-effective than traditional analog pathways which commonly require 2 or more weeks. Using available technologies, Navy dentists can generate complete-coverage restorations (i.e., crowns) in a single appointment. These restorations display life cycles and esthetic properties similar to their analog counterparts. In addition, patients appear to favor digital approaches to traditional analog methods.,
Results of this investigation indicate a distinct shift in the types of restorations placed before and after CAD/CAM the implementation period. The use of large dental amalgam restorations was declining at an annual rate of 1.56% before the introduction of CAD/CAM technologies, and displayed an annual decline of 4.18% after the introduction of CAD/CAM technologies. A similar trend was observed for PFM placements. While the introduction of CAD/CAM restorations probably contributed to the decline in amalgam and PFM placements, an accompanying increase in laboratory-fabricated Ceramic/Resin restoration placement rates should not be overlooked.
The quality of CAD/CAM digital restorations identifies them as predictable alternatives to traditional dental treatment methods. Efficiency of the digital workflow and quality of the resultant restorations are persuading an increasing number of dentists to adopt CAD/CAM technologies.– Navy dentistry has embraced the aforementioned technologies and has deployed these systems on multiple platforms including ships. Tangible benefits may include reduction of patient waiting times, improved clinical productivity and a positive effect on dental readiness status for Sailors and Marines. In addition, military personnel could benefit from electronic capture and transmission of digital information, as well as remote design capabilities (e.g., a provider/master technician need not be on site). A secure electronic infrastructure also would minimize the time and expense associated with mailing/shipping.
Although increased CAD/CAM utilization in the Navy is expected, several factors may limit the widespread utilization of such technologies. First, many dentists are unfamiliar with existing CAD/CAM platforms and must overcome steep learning curves to incorporate digital workflow into practice. Second, deployment of CAD/CAM systems into small clinics with a limited patient population may not be cost effective when system and maintenance costs are taken into consideration. Third, such restorations are not suitable for all clinical applications (e.g., long-span prostheses in high-stress areas). These mitigating factors can help explain the limited percentage of CAD/CAM restorations placed in Navy treatment facilities. Despite the foregoing conditions, the number of CAD/CAM restorations is likely to increase for the following reasons: (1) incorporation of CAD/CAM technologies into dental school curricula, (2) advancement of CAD/CAM systems equipped with fast-evolving user interfaces, (3) increased placement of CAD/CAM technology in Navy clinics, and (4) training of a greater proportion of Navy providers in digital CAD/CAM technology.
Rapidly improving 3D software and hardware for fabricating high-quality dental restorations through subtractive CAD/CAM technologies has resulted in the growing adoption and implementation of these restorations by Navy dental providers. Digital workflow should be continually monitored to evaluate further utilization changes by Navy dentists. Monitoring placement rates will provide policy makers, strategists, and planners with insight on how to best manage current systems in order to maximize efficiency and usage. Additionally, given the variety and uniqueness of environments in which Navy dentists work, a potential exists to modify current CAD/CAM systems in order to more effectively integrate them into all Navy platforms.
CONCLUSION
Navy Dentistry has steadily increased the role of CAD/CAM systems in the provision of dental care to Navy and Marine Corps service members in order to meet operational and mission objectives. Based on the data presented from this study, CAD/CAM productivity is projected to rise in the Navy. As CAD/CAM restorations account for a greater percentage of coronal coverage restorations, further epidemiological research should focus on the following aspects of CAD/CAM usage: (1) longevity or survival rate of CAD/CAM restorations placed within military settings, (2) cost and manpower analysis of maintaining CAD/CAM units and instructing providers on how to use them, and (3) impact on military dental laboratories associated with increased CAD/CAM usage. The increase in deployment of state-of-art CAD/CAM technology by Navy dental providers suggests that the benefits, such as reduced patient treatment time and improved esthetics, of CAD/CAM utilization outweigh their implementation costs.
REFERENCES
- 1. Hartzell D: Readiness requires a team. J Am Coll Dent2012; 79(1): 18–20.
- 2. Leiendecker T: The Department of Defense oral health and readiness classification system. Mil Med2008; 173(1 Suppl): 1–2.
- 3. Burns DR., et al: A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J Prosthet Dent2003; 90(5): 474–97.
- 4. Ng J., Ruse D., Wyatt C: A comparison of the marginal fit of crowns fabricated with digital and conventional methods. J Prosthet Dent2014; 112(3): 555–60.
- 5. Freedman M., Quinn F., O’Sullivan M: Single unit CAD/CAM restorations: a literature review. J Ir Dent Assoc2007; 53(1): 38–45.
- 6. Fasbinder D.J: The CEREC system: 25 years of chairside CAD/CAM dentistry. J Am Dent Assoc2010; 141(Suppl 2): 3S–4S.
- 7. Beier US., et al: Clinical performance of all-ceramic inlay and onlay restorations in posterior teeth. Int J Prosthodont2012; 25(4): 395–402.
- 8. Posselt A., Kerschbaum T: Longevity of 2328 chairside Cerec inlays and onlays. Int J Comput Dent2003; 6(3): 231–48.
- 9. Otto T., Schneider D: Long-term clinical results of chairside Cerec CAD/CAM inlays and onlays: a case series. Int J Prosthodont2008; 21(1): 53–9.
- 10. Otto T: Up to 27-years clinical long-term results of chairside Cerec 1 CAD/CAM inlays and onlays. Int J Comput Dent2017; 20(3): 315–29.
- 11. Christensen G.J: Is now the time to purchase an in-office CAD/CAM device?J Am Dent Assoc2006; 137(2): 235–6. 238.
- 12. Simecek JW., et al: The incidence of dental disease nonbattle injuries in deployed U.S. Army personnel. Mil Med2014; 179(6): 666–73.
- 13. Mormann W.H: The origin of the Cerec method: a personal review of the first 5 years. Int J Comput Dent2004; 7(1): 11–24.
- 14. Mormann W.H: The evolution of the CEREC system. J Am Dent Assoc2006; 137(Suppl): 7S–13S.
- 15. Guichet D: Digitally enhanced dentistry: the power of digital design. J Calif Dent Assoc2015; 43(3): 135–41.
- 16. Joda T., Bragger U: Patient-centered outcomes comparing digital and conventional implant impression procedures: a randomized crossover trial. Clin Oral Implants Res2016; 27(12): e185–9.
- 17. Shembesh M., et al: An in vitro comparison of the marginal adaptation accuracy of CAD/CAM restorations using different impression systems. J Prosthodont2017; 26(7): 581–6.
- 18. Belli R., et al: Fracture rates and lifetime estimations of CAD/CAM all-ceramic restorations. J Dent Res2016; 95(1): 67–73.
- 19. Batson ER., et al: Clinical outcomes of three different crown systems with CAD/CAM technology. J Prosthet Dent2014; 112(4): 770–7.
- 20. Abdel-Azim T., et al: Comparison of the marginal fit of lithium disilicate crowns fabricated with CAD/CAM technology by using conventional impressions and two intraoral digital scanners. J Prosthet Dent2015; 114(4): 554–9.
- 21. Joda T., Bragger U: Digital vs. conventional implant prosthetic workflows: a cost/time analysis. Clin Oral Implants Res2015; 26(12): 1430–5.
- 22. Wismeijer D., et al: Patients’ preferences when comparing analogue implant impressions using a polyether impression material versus digital impressions (Intraoral Scan) of dental implants. Clin Oral Implants Res2014; 25(10): 1113–8.
- 23. Gallardo Y.R, et al: Patient outcomes and procedure working time for digital versus conventional impressions: a systematic review. J Prosthet Dent2018; 119(2): 214–219.
- 24. Tsirogiannis P., Reissmann DR., Heydecke G: Evaluation of the marginal fit of single-unit, complete-coverage ceramic restorations fabricated after digital and conventional impressions: a systematic review and meta-analysis. J Prosthet Dent2016; 116(3): 328–335 e2.
- 25. Seelbach P., Brueckel C., Wostmann B: Accuracy of digital and conventional impression techniques and workflow. Clin Oral Investig2013; 17(7): 1759–64.
- 26. Su TS., Sun J: Comparison of marginal and internal fit of 3-unit ceramic fixed dental prostheses made with either a conventional or digital impression. J Prosthet Dent2016; 116(3): 362–7.