INTRODUCTION
Telemedicine is defined as the practice of medicine when the doctor and patient are widely separated using two-way voice and visual communication (as by satellite or computer). Described by Lilly et al., “Tele-ICU is care provided to critically ill patients by off-site clinicians using audio, video, and electronic links to leverage technical, informational, and clinical resources.” It also includes the capability to detect patient instability, laboratory derangements, order additional studies, makes diagnoses, implement treatment strategies, as well as communicate with other healthcare providers, patients and their families. The intent of tele-ICU is not to replace bedside clinicians, but to enhance patient safety with “a second set of eyes” via built in redundancy and to improve patient outcomes through standardization of best practices. In civilian settings, these tools have been shown to decrease patient mortality, length of stay (LOS), and costs. Approximately 10% of ICU beds nationwide are monitored with tele-ICU services, and, as the demand for critical care services outpaces the training of the critical care workforce, the utilization of tele-ICU technologies is likely to grow.–
General Leonard Wood Army Community Hospital (GLWACH) is a small medical treatment facility (MTF) with limited resources with respect to subspecialists and ancillary services. In 2009, GLWACH identified the lack of board-certified critical care physicians and limited baseline critical care capabilities as gaps that reduced surgical opportunities, challenged critical skill sustainment, exposed potential patient safety issues, and resulted in costly patient transfers to network hospitals. These transfers resulted in decreased continuity of care caused patient and family inconvenience. Hospital leadership consequently developed a plan with the specific project goals to improve care for the sickest patients and increase local capability, improve patient quality of life, challenge nurses and medical staff to practice at the top of their licenses, improve clinical outcomes, and to lower costs through collaborative partnership. The solution chosen to address these goals was to develop and implement a tele-ICU program at GLWACH. The vision of the hospital was to provide patients with the highest quality critical care while simultaneously utilizing the clinical skills of the medical providers and maintaining their readiness for deployment. This manuscript describes this process improvement project and reviews outcomes and costs associated with it.
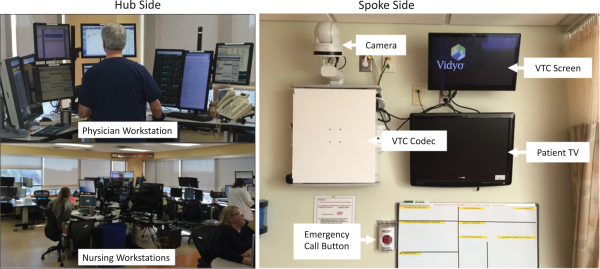
FIGURE 1
Images of the tele-ICU hub at Baptist Hospital, Little Rock, AK and spoke site at George Leonard Wood Army Medical Center, Missouri. The Hub Side a close up view of the physician workstation and a wide-angle view of the hub unit with multiple workstations where nurses and a physician provide 24/7 coverage for over 200 ICU patients. The Spoke Side shows the teleICU components installed in a spoke site ICU patient room from the patient perspective. Items include a high-definition camera with a video codec (enables videoteleconferencing) below it, a monitor, and the emergency call button.
METHODS
GLWACH is a 60-bed hospital located at the US Army installation Fort Leonard Wood, Missouri. It has four ICU beds available for care of critically ill patients. There are no board certified critical care physicians on staff; thus, in order to better serve patients with the highest quality critical care, the hospital leadership began planning to introduce a tele-ICU program to the hospital in 2012.
During the planning phase for tele-ICU, GLWACH leadership initially sought collaboration within the military, seeking a military facility that could provide tele-ICU support. Unfortunately, no military organization at that time supported tele-ICU services. Baptist Health in Little Rock, AR, provided tele-ICU services to community-based hospitals with limited access to critical care subspecialists using a team comprised of critical care physicians and nurses to remotely monitor adult ICU patients located in these facilities. During this first year of planning, leadership of both GLWACH and Baptist Health performed site visits at each location and planned the best way to implement the system. In early 2013 there was approval to implement the tele-ICU program at GLWACH and funding was secured to install the necessary communication and information technologies. The program became operational in the last quarter of 2013.
The goal of the Baptist Health tele-ICU program is to improve patient outcomes and increase the standard of care provided at smaller medical facilities. It is staffed by 15 physicians, 30 nurses, and other support staff. Median critical care experience for tele-ICU clinicians is more than 10 years. A typical 12-hour shift is staffed by one physician and 5–6 nurses to provide comprehensive monitoring and tele-consultation to 120–150 ICU patients. This tele-ICU platform has smart monitoring technologies and evidence-based decision support that facilitates application of standardized ICU care across the system, further improving quality measures and clinical outcomes.
Orientation and training for staff at GLWACH on the implementation of the tele-ICU program were conducted in collaboration with the tele-ICU service provider. All nurses were trained ICU nurses. Representatives from Baptist Health visited GLWACH and supported training by hospital leadership. GLWACH ICU nurses and physician staff were encouraged and supported to visit the Baptist Heath tele-ICU center to obtain better understanding of their capabilities. Equipment training was minimal as contacting Baptist Health was at the push of a button or making a phone call. A Competency Based Orientation (CBO) that reviewed the rationale, workflow, and implementation of the tele-ICU program was completed by all GLWACH staff that worked in the ICU.
Four ICU beds were electronically equipped to ensure availability of continuous transmission of audio, video, and patient physiologic data to the tele-ICU hub at Baptist Health (Fig. 1). Each room also was equipped with a red “emergency” button on the wall that immediately calls the tele-ICU team and activates the in-room camera/microphone system (Fig. 1). This button could be pushed by staff, the patient, or family as deemed necessary. The facility also had two mobile tele-ICU carts that were available to be used in isolation rooms, as well as respond to codes or rapid response calls throughout the hospital. A dedicated phone line from the Baptist tele-ICU to the central nursing station at GLWACH was established for consultation performed remote from the bedside. There were multiple contingency plans and policies in place in the event of equipment or communication failure both at GLWACH and at the Baptist Health tele-ICU hub. In general, contingency operations relied upon good communication using the phone system in the event that video communications and physiologic vital sign streams were degraded or unavailable. If all communications were lost, algorithms were developed to determine if patients would need to be transferred to other facilities.
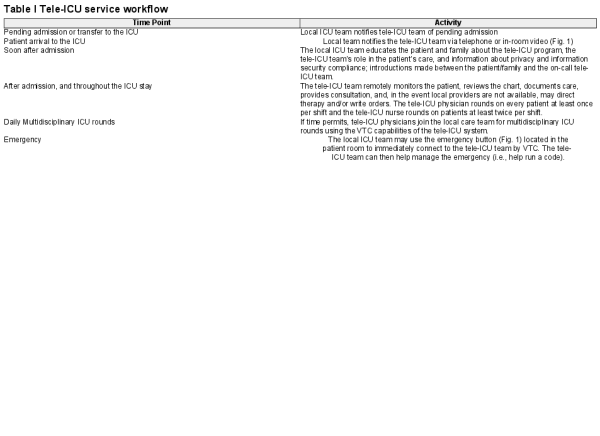
The tele-ICU workflow involves several steps (Table I). The tele-ICU team is notified of pending admissions or transfers by local staff (on-call physicians, patient administration, etc.) and an “SBAR” report is given. The tele-ICU team is also notified and given a report via telephone or in-room video system at the time of patient arrival in the ICU. At the time of admission, the patient and family are also given an introduction about the tele-ICU team, the tele-ICU team’s role in the patient’s care, and information about privacy and information security compliance. After admission, and throughout the ICU stay, the tele-ICU team remotely monitors the patient, reviews the chart, documents care, provides consultation, and, in the event local providers are not available, may direct therapy and/or write orders. The tele-ICU physician rounds on every patient at least once per shift and the tele-ICU nurse rounds on patients at least twice per shift. If time permits, tele-ICU physicians typically join the local care team for multidisciplinary ICU rounds using the video teleconferencing capabilities of the tele-ICU system.
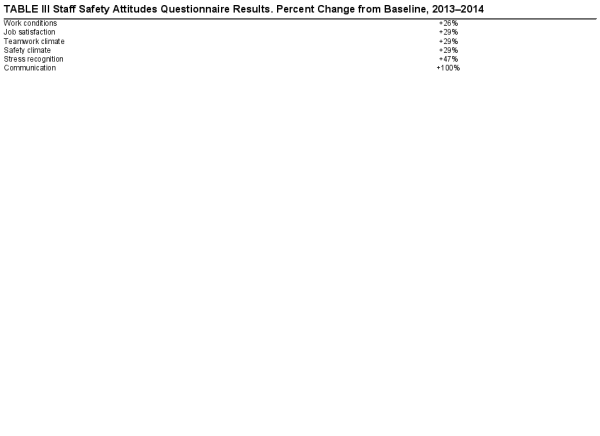
To report on this experience, we examined the impact of the introduction of the tele-ICU program at GLWACH by reviewing ICU volume and acuity, as well as costs before and after implementation of the tele-ICU services. Acute Physiology and Chronic Health Evaluation IV (APACHE IV) scores and hospital case mix index (CMI) were compared between pre and post tele-ICU implementation. GLWACH leadership administered the Safety Attitudes Questionnaire (SAQ) to assess staff attitudes before and after implementation.
RESULTS
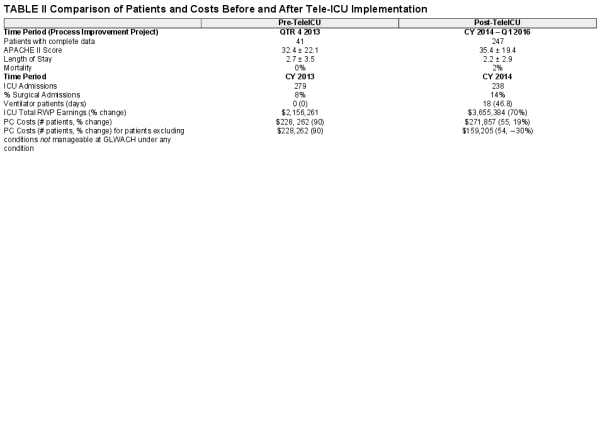
Initial and sustaining costs for the tele-ICU are shown in Table II. Comparison of patient characteristics before and after implementation is shown in Table II. None of the trends described below were statistically significant. After the implementation of the tele-ICU program, there was a sustained increase in the average number of ICU patients per day, hospital volume and variety (as indicated by the case mix index; Supplementary figure 1 and 2). The percentage of surgical admissions to the ICU increased from 8% to 14%. Overall patient illness severity increased as measured by APACHE IV scores (Supplementary figure 3). Illness severity increased initially for ventilated patients then returned to baseline for this patient population (Supplementary figure 4). Length of ICU stay was unchanged. 5 patients died in the post intervention period whereas none died in the quarter prior to implementing tele-ICU. Hospital administrative data revealed a 70% increase in total relative work product (RWP) associated ICU earnings, a reduction in purchased care RWPs (fiscal year [FY] 2013 to FY2014 was 1,126 vs 547 or a 51.4% decline) and reduced purchase care costs for network referrals for care that could be rendered at GLWACH ($228,000 vs. $159,000, 30% reduction). One military beneficiary with a cerebral infarction, a diagnosis that is not managed at GLWACH at any time, was cared for by the civilian network at a purchase cost of $112,651. Excluding this outlier, return on investment (ROI) in year one of the tele-ICU process improvement project was calculated as the difference between RWP earnings plus the purchased care savings less the cost of tele-ICU implementation, or $233,311 (19%). Seventy-five percent of SAQ surveys were returned. There were substantial improvements in all SAQ metrics indicating that there was a positive influence and culture change following tele-ICU implementation (Table III).
DISCUSSION
Implementation of the tele-ICU program at GLWACH partnered with Baptist Health tele-ICU was successful in multiple domains. It demonstrated a steady increase in patient volume and complexity while simultaneously reducing patient deferments to network hospitals which reduced purchased care costs and saved the hospital money. Contrary to other patient populations, the ventilated patient illness severity trend showed a rapid increase and then decline to baseline. This likely represents recognition that the most appropriate ventilated patients in this community hospital are post-operative patients and those with acute exacerbations of chronic obstructive pulmonary disease vise the more critically ill patients with severe pneumonia or the acute respiratory distress syndrome. Additionally, clinical staff were surveyed about their attitudes towards safety and about the safety culture at GLWACH before and after tele-ICU implementation. Safety attitudes and safety cultural perception improved across all measurements.
These findings are consistent with those published by Dr. Davis and colleagues who reported findings about the Navy’s Tele Critical Care (TCC) Service. This service was found to increase monthly admission volume, decrease the number of patient disengagements to network hospitals, increase average monthly patient APACHE II scores, and decrease network expenditures at one small Naval Medical Center. Like the Navy TCC service, this project noted an increase in mortality after implementation of the tele-ICU monitoring at GLWACH. Like Dr. Davis, we propose that this was related to an increased number of deaths associated with withdraw of care that occurred locally vise transferring the patient to a network hospital. No adverse outcomes related to the TCC system were reported. Dr. Van Gent and colleagues found that the implementation of the same TCC system had a significant impact in the surgical population admitted to the same Naval Hospital. The percentage of surgical ICU admissions had a statistically significant increase, as well as increase in monthly average APACHE II scores with no reported adverse outcomes. This implementation allowed expansion of surgical services that would otherwise be transferred to another facility due to lack of post-operative ICU support. We similarly found increased surgical volume in the ICU after initiation of tele-ICU monitoring at GLWACH.
The Navy experience was remarkably less costly than the one described here. Dr. Davis reports that the Navy implementation of TCC services cost $50,000, all for equipment procurement (a single mobile VTC cart). Nevertheless, because the Navy solution relied upon (1) military intensivist support and (2) native hardware and software solutions, their TCC service solution did not require the same costs as our commercial solution. In particular, costs for software licensing and telemedicine services are remarkably more with a commercial solution (a $648,680 difference). Another notable difference was their use of a single VTC cart vise installation of dedicated hardware in four patient rooms at GLWACH (a $222,425 difference). Of note, since the time of their publication, the Navy has installed dedicated hardware in each of their monitored ICU rooms (personal communication, JCP).
Prior to the introduction of the tele-ICU program, GLWACH struggled with a “culture of can’t” as clinicians lacked confidence in the facility’s ability to manage complex patients given the limited critical care experience of their staff and lack of expert availability. Patients with even the potential to deteriorate were routinely transferred to the closest civilian hospital with critical care support – an approximately 2-hour drive – rather than risking admission locally. This culture also diminished the number and acuity of surgeries performed at the facility as patients who might require additional post-operative monitoring would be deferred to the network for their procedure to avoid the risk of decompensation without availability of expeditious expert consultation [personal communication by authors JCP and PN with GLWACH personnel].
This culture is a “catch 22” in which lack of experience resulted in decreased patient volume, acuity, and complexity which then resulted in degraded clinical skills of nurses and providers as the patient population diminished and lost diversity which further contributed to lost experience and decreased confidence. Ultimately, this clinical environment and the hospital culture degraded clinician readiness for deployment.
Implementation of the tele-ICU system measurably changed the hospital culture. By adding the critical care expert’s “back-up,” provided by the tele-ICU service, GLWACH clinicians felt confident in their ability to provide appropriate patient care and to recognize clinical decompensation early enough to prepare for safe patient transfer. Increased confidence translated into increased admissions and surgical volume, increased patient acuity and case mix, and decreased purchased care costs. This culture change, and the changes in patient population associated with it, directly impacted the readiness of clinicians at GLWACH through sustainment of clinical skills like ventilator management, shock resuscitation, and post-operative care.
ICU telemedicine is an evolving technology that increases the availability of critical care resources and has shown improvement in clinical outcomes.– One single center, civilian study showed improvement in mortality and length of stay with the implementation of a tele-ICU program. These improvements, in part were related to higher adherence to best practices as well as prompt responses to alerts to physiologic instability, and earlier involvement of an intensivist. This study also showed reduction in ventilator associated pneumonias and catheter related bloodstream infections.
Findings from this single center study were further expanded by a multicenter study of implementation of a tele-ICU programs. Published in 2014, Lilly et al. preformed a multicenter analysis of pre/post tele-ICU implementation in 56 ICUs across the United States, spanning 15 states and serving rural, suburban, and urban populations. This study showed an association between the following tele-ICU interventions and reduced mortality: (1) early intensivist management, (2) coordinated timely usage of performance information, (3) achievement of higher rates of adherence to best practices, (4) shorter alarm response times, (5) more frequent interdisciplinary rounds, and (6) a more effective ICU committee. Individually, each component had a small effect, but cumulatively their additive effects improve outcomes. Although not measured directly, similar tele-ICU processes likely contribute to improving patient outcomes at GLWACH. Dr. Kahn stated in his editorial in JAMA, “Telemedicine alone does not equate to quality improvement but is merely a tool for quality improvement and in the right setting and with the right goals, telemedicine can indeed be used to help improve outcomes.” The ability for the tele-ICU program to have positive effects on patient outcomes require collaboration between the local and tele-ICU team and acceptance by the local care team: unfortunately, tele-ICU implementation without local staff buy in will likely not show improvement in patient care metrics.
Nettesheim and colleagues recently published a manuscript that further highlights the importance of telemedicine utilization within military medicine. As both technology and necessity have advanced, it is important for military practitioners to be facile with the utilization of these technologies. The technology may be as simple as asynchronous communication via email or text message or as complex as real-time video teleconferencing. The shortage of critical care staff nationwide is certainly reflected within the Military Health System (MHS), and even more so in the remote, austere setting.,, Telemedicine can be used to fill the void of provider shortages and provide real-time guidance for caregivers deployed to austere locations, but will only be effective if adopted by both the deployed provider and the clinicians providing the telemedical consultation. It also provides opportunity to rapidly promote clinicians from “novice” to “expert” by having a critical care specialist able to walk the on-site provider through medical management of complex patients that they would otherwise not be comfortable managing.
CONCLUSIONS
This is the first publication of tele-ICU care in the U.S. Army. It demonstrates that the culture of care at GLWACH changed following the implementation of the tele-ICU program and was associated with an increased volume, acuity, complexity, and variety of patient admissions to the hospital. The increased volume of care at the hospital was directly related to decreased transfer of patients with higher complexity to the local civilian network resulting in reduced purchased care costs and a positive return on investment for the hospital. These findings support the implementation of tele-ICU in the MHS as a cost-effective method to sustain readiness among critical care clinicians and improve safety culture in MHS hospitals. A model that utilizes a dedicated military telecritical care service may be more cost-effective than civilian collaborations due to savings associated with service contracts.
ACKNOWLEDGMENTS
The authors would like to thank CPT Ian Ritter, MC, USA, and Mr. Efren Tragico, Baptist Health, Little Rock, AK for their support of this manuscript in both championing the clinical effort to implement the tele critical care system and with providing the data to incorporate in the manuscript. Authors RDM and JCP wrote the manuscript after receiving the data. Authors JI and PN provided first person accounts of project, vouch for data accuracy, and helped edit the manuscript. Author JCP was responsible for final manuscript preparation and submission and takes responsibility for the validity of the manuscript’s conclusions.
The views expressed are solely those of the authors and do not reflect the official policy or position of the US Army, US Navy, US Air Force, the Department of Defense, or the US Government.
References
- 1.
- 2. Lilly C, Thomas E: Tele-ICU: experience to date. J Intensive Care Med2009; 25(1): 16–22. doi:10.1177/0885066609349216.
- 3. Goran S: A second set of eyes: an introduction to Tele-ICU. Crit Care Nurse2010; 30(4): 46–55. doi:10.4037/ccn2010283.
- 4. Lilly C, Fisher K, Ries M, et al: A national ICU telemedicine survey. Chest2012; 142(1): 40–47. doi:10.1378/chest.12-0310.
- 5. Angus D, Kelley M, Schmitz R, White A, Popovich J: Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population?JAMA2000; 284(21): 2762–2770. doi:10.1001/jama.284.21.2762.
- 6. Afessa B: Tele-intensive care unit: The horse out of the barn*. Crit Care Med2010; 38(1): 292–293. doi:10.1097/ccm.0b013e3181b9d4dc.
- 7.
- 8. Sexton J, Helmreich R, Neilands T, et al: The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res2006; 6. doi: 110.1186/1472-6963-6-44
- 9. The Uniformed Business Office User Guide, Defense Health Agency, May 2018.
- 10. Davis K, Perry-Moseanko A, Tadlock M, Henry N, Pamplin J: Successful implementation of low-cost tele-critical care solution by the U.S. Navy: initial experience and recommendations. Mil Med2017; 182(5): e1702–e1707. doi:10.7205/milmed-d-16-00277.
- 11. Van Gent J, Davis K, Henry N, et al: The initial impact of tele-critical care on the surgical services of a community military hospital. Mil Med2018; 183(11–12): e494–e499. doi:10.1093/milmed/usy051.
- 12. Wilcox M, Adhikari N: The effect of telemedicine in critically ill patients: systematic review and meta-analysis. Critical Care2012; 16(4): R127. doi:10.1186/cc11429.
- 13. Lilly C: Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA2011; 305(21): 2175. doi:10.1001/jama.2011.697.
- 14. Lilly C, McLaughlin J, Zhao H, Baker S, Cody S, Irwin R: A multicenter study of ICU telemedicine reengineerng of adult critical care. Chest2014; 145(3): 500–507. doi:10.1378/chest.13-1973.
- 15. Kahn J: The use and misuse of ICU telemedicine. JAMA2011; 305(21): 2227. doi:10.1001/jama.2011.716.
- 16. Goran SF: Measuring tele-ICU impact: does it optimize quality outcomes for the critically ill patient?J Nurs Manag2012; 20(3): 414–28.
- 17. Nettesheim N, Powell D, Vasios W, et al: Telemedical support for military medicine. Mil Med2018; 183(11–12): e462–e470.
- 18. Nam JJ, Colombo CJ, Mount CA, et al: Critical care in the military health system: a survey-based summary of critical care services. Mil Med2018; 183(11–12): e471–e477.
- 19. Rasmussen TE, Baer DG, Cap AP, Lein BC: Ahead of the curve: sustained innovation for future combat casualty care. J Trauma Acute Care Surg2015; 79(4Suppl 2): S61–4.
- 20. Hwang JS, Lappan CM, Sperling LC, Meyerle JH: Utilization of telemedicine in the U.S. military in a deployed setting. Mil Med2014; 179(11): 1347–53.