Rotator cuff disease is one of the most common causes of shoulder pain and dysfunction. The prevalence of rotator cuff tears has been documented as ranging from 4% to 51%, varying with age. Of patients with symptomatic full-thickness rotator cuff tears who present for treatment, approximately 27% to 47% will have a contralateral full-or partial-thickness rotator cuff tear. Studies of patients undergoing rotator cuff surgery also report a high (39%) prevalence of tears in the contralateral arm. Although these contralateral tears may initially be asymptomatic, they possess the risk of progressively increasing shoulder dysfunction.
The decision to seek and undergo treatment for rotator cuff tears is often complex, with patients citing varied factors in their decision-making. Some of these patients opt to undergo surgical management for both shoulders within a short time frame. Patients undergoing staged bilateral arthroscopic rotator cuff repair (ARCR) have good outcomes regardless of hand dominance or the laterality of the first repair. The optimal timing for staging is thought to be approximately 9 months.
Despite this, to our knowledge, there are currently no studies reporting specific patient preferences on the management of bilateral rotator cuff tears. The purpose of this study was to investigate patient preferences for undergoing short-interval staged bilateral RCR; timing of surgeries; and order of surgeries. Second, we sought to determine patient-reported outcomes following ARCR, patients' satisfaction with timing and laterality of staged bilateral RCR, and factors in decision-making when undergoing the staged procedures in a short time interval (within 12 months). We hypothesize that there is no correlation between the timing of surgery or initial surgical limb and patient satisfaction after short-interval staged bilateral RCR.
Materials and Methods
Patient Selection
A query in an institutional database was obtained for the period from January 2010 to December 2019 for patients who underwent bilateral RCRs within a 12-month period. The inclusion criteria were as follows: (1) age 18 to 100 years, (2) primary ARCR, (3) bilateral RCR, and (4) a minimum follow-up of 2 years after the second surgical procedure. Patients were excluded in the following cases: (1) their second RCR was a revision repair, (2) an open RCR was performed, or (3) the contralateral RCR surgery was performed more than 12 months after the original date of surgery. Of the 546 patients identified from the data query, 257 met the inclusion criteria through retrospective chart review. Two patients were found to have died, leaving 255 eligible patients. Ninety of the 255 eligible patients responded to the REDCap surveys and were included in the study. A flowchart of patient inclusion is provided in Figure 1.
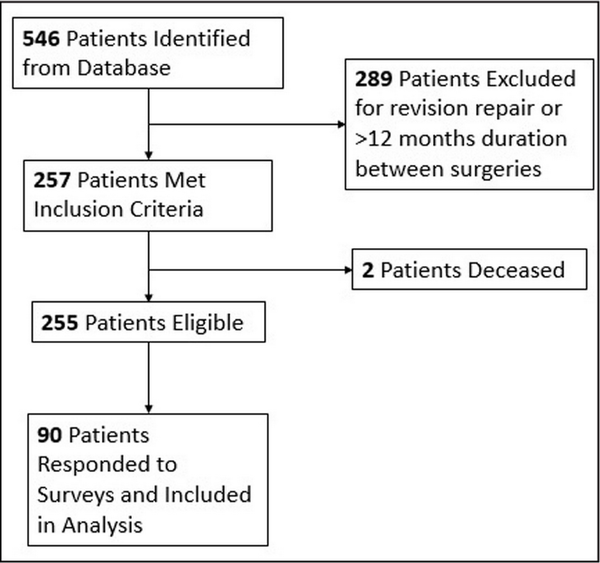
Figure 1
Flowchart of patient inclusion/exclusion.
Because this was a descriptive study, there was no targeted enrollment size. All patients meeting the inclusion criteria were included for analysis.
Data Collection
Descriptive data were recorded as provided by the database and included sex, age at primary procedure, months between surgeries, hand dominance, occupational status, and size of tear (partial vs full thickness). The American Shoulder and Elbow Surgeons standardized assessment (ASES), Single Assessment Numeric Evaluation (SANE), and Simple Shoulder Test (SST) scores were also recorded.
Eligible patients were sent surveys via REDCap and received follow-up phone calls. Patients were evaluated for postoperative ASES scores, determining factors for electing to have surgery (adapted from Weekes et al), choice of initial surgical arm, number of months between surgeries, and satisfaction with timing (months postoperative between procedures). Decision-making factors were scored on a scale of 1 to 5, with 1 representing highest importance and 5 representing lowest importance. These scores were converted to a system in which 1 or 2 was considered highly important, 3 or 4 was moderately important, and 5 was not important.
Statistical Analysis
Parametric continuous data were presented as mean (SD), and P values were calculated by performing t tests. Nonparametric continuous data were also presented as mean (SD) for easier interpretation and calculated by performing Mann-Whitney tests. Categorical data were presented as cell count (percentage). Chi-square or Fisher's exact tests were used to calculate P values for categorical data. P<.05 was deemed significant. All statistical analyses were done using R Studio, version 3.6.3, software (Posit, PBC).
Results
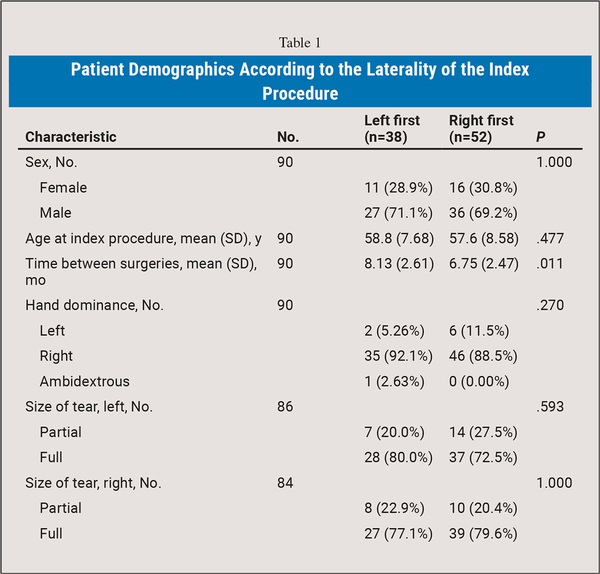
Complete preoperative and postoperative clinical data were available for 90 patients (63 men and 27 women) who underwent short-interval staged bilateral ARCR. Table 1 shows the basic demographic information, including the mean age at the time of index surgery, hand dominance, and order of laterality of surgery. Rotator cuff tears were recorded as partial- or full-thickness tears. The majority of both left and right shoulder tears were full thickness (75.6% and 78.6%, respectively). Of the 90 total patients, 57.8% elected to undergo right shoulder ARCR first. Forty-eight patients (53.3%) had surgery on their dominant arm first. The mean time between index procedure and secondary procedure was 6.75 months for those undergoing the right shoulder first and 8.13 months for those undergoing the left shoulder first.
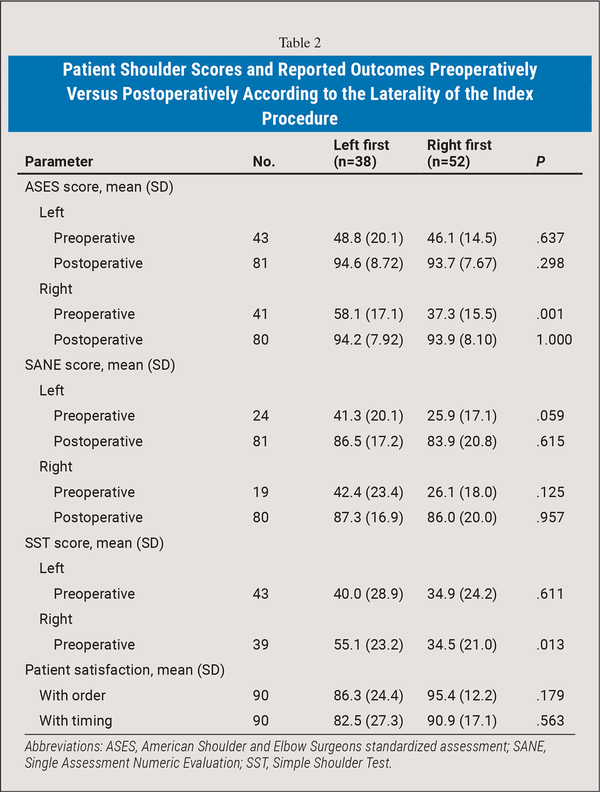
Preoperative and postoperative ASES, SANE, and SST questionnaires were compared. Preoperatively, the mean ASES scores were 47.3 for left shoulders and 44.9 for right shoulders. The mean SANE scores were 33.0 for both shoulders. The mean SST scores were 37.0 and 41.4 for left and right shoulders, respectively. Overall, the satisfaction scores for order (left vs right first) and timing were 91.6 and 87.3 (of 100), respectively. There was no statistical significance in postoperative ASES or SANE scores when comparing shoulders; however, both scores were significantly increased compared with pre-operative analysis (Table 2). Satisfaction scores for order and timing also were not statistically significant between groups. Of note, patients who had surgery on their left shoulder first had a lower satisfaction score for the order of surgeries (86.3) than patients who had surgery on their right arm first (95.4) (P=.179).
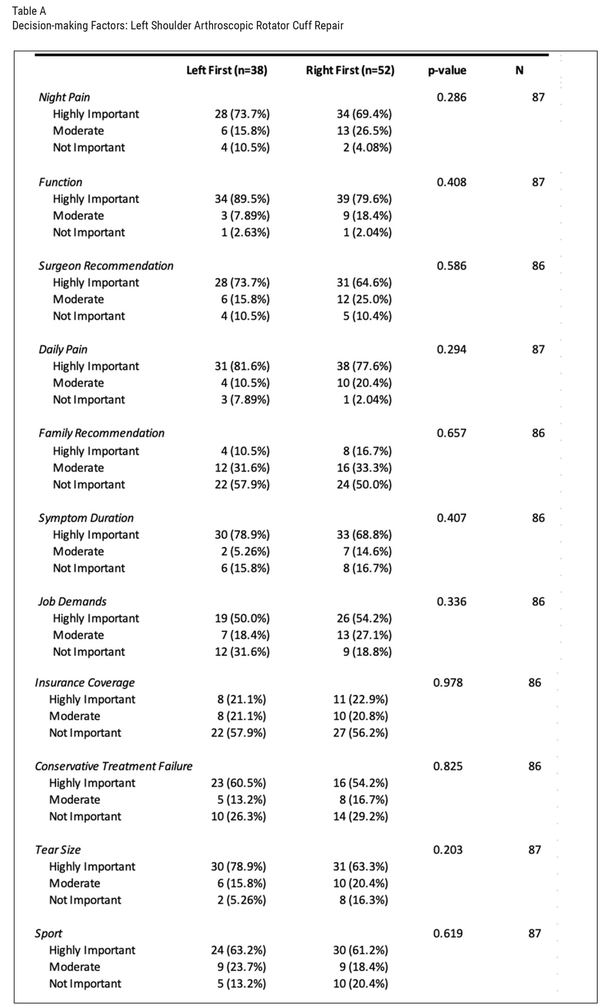
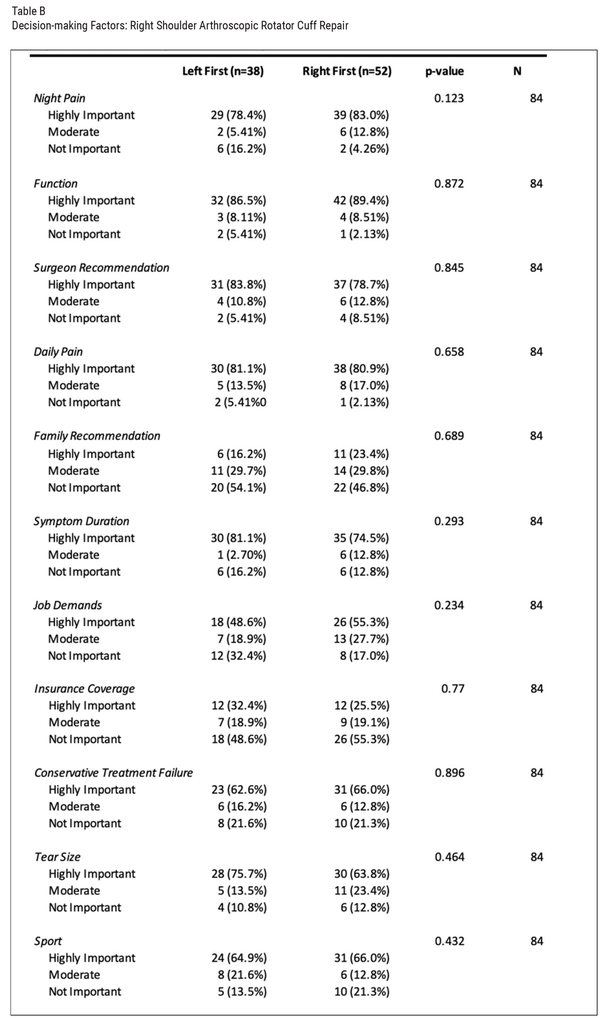
Decision-making factors noted as highly important for the majority of patients included night pain (71.3% left, 81.0% right), function (83.9% left, 88.1% right), surgeon recommendation (68.6% left, 81.0% right), daily pain (79.3% left, 81.0% right), symptom duration (73.3% left, 77.4% right), job demands (52.3% left, 52.4% right), conservative treatment failure (57.0% left, 64.3% right), size of tear (70.1% left, 69.0% right), and sport participation (62.1% left, 65.5% right).
Factors noted as not important or only moderately important for most patients included family recommendations (16.2% left, 23.4% right) and insurance concerns (32.4% left, 25.5% right) (Table A and Table B). None of the patient decision-making factors were statistically different between patients who underwent left vs right ARCR, regardless of which side was performed first.
Discussion
This study found that most patients who undergo short-interval (<12 months) staged bilateral ARCR are satisfied with the order and timing of their surgery. The ASES and SANE scores were almost equal in both shoulders, regardless of which side the ARCR was performed on first. After surveying patients, the most common highly important decision-making factors to undergo surgery were impaired shoulder function, daily pain, and night pain. These were also consistent for the index and contralateral staged procedures.
Simultaneous (single-staged) bilateral RCRs have been studied. Some theoretical advantages of undergoing single-staged ARCR include reduced hospitalization costs and shorter recovery times. Chu et al studied 51 patients who underwent simultaneous ARCR compared with 42 patients who elected to have staged procedures. The second operative shoulder of the simultaneous group showed significantly greater improvement than the second shoulder of the staged group for ASES score, forward flexion, and abduction. This may have been because of the order in which the surgeries were performed in the staged group. In the staged group, the more symptomatic tear was repaired first; however, no statistically significant differences were noted in shoulder function scores and range of motion from preoperative to final follow-up between the two groups. Another study found that patients who underwent simultaneous bilateral ARCR had higher rates of revision RCR, reverse total shoulder arthroplasty, and postoperative infection compared with patients in a control group. These findings suggest that short-interval staged bilateral RCR may be a safer option for patients than single-staged bilateral RCR.
Most patients with bilateral rotator cuff tears will opt for staged treatment given the demands of immobility during recovery. Orthopedic surgeons may have their own postoperative protocol, and the American Society of Shoulder and Elbow Therapists has formulated a consensus statement on rehabilitation following ARCR. Patients should expect a minimum of 4 to 5 months postoperatively before work- and sport-specific rehabilitation activities can commence. Although some patients may elect to get through both shoulder recoveries at once, others will elect to have a longer total recovery time (through staged ARCR) and still have function of their nonsurgical arm during recovery of each surgery.
Challenges arise when managing patients who desire staged bilateral ARCRs. The amount of time needed between the index surgery and the second surgery to minimize postoperative complications while optimizing clinical and structural outcomes is a source of debate. Kim et al reviewed 166 shoulders both with magnetic resonance imaging at 9 months and clinical outcome scores at 2 years. They identified significantly inferior outcomes and higher rates of retears in the index procedure when the second, contralateral procedure was performed within 9 months. The second procedure had no difference in outcomes. Rhee et al also used magnetic resonance imaging to evaluate staged bilateral RCRs at 12 months post-operatively. Almost 64% of patients with nonhealing in the index procedure had subsequent failure in the other shoulder. Another retrospective study categorized more than 11,000 patients by 3-month intervals in which staged bilateral ARCRs were performed. Contrary to Kim et al, those authors found that only patients undergoing simultaneous or bilateral ARCR with less than 3 months between surgeries had an increase in clinical or structural complications, including revision RCR, stiffness, infection, venous thromboembolic events, and emergency department visits. They also discovered that patients with Medicare had higher rates of emergency department visits following ARCR, likely because of more significant comorbidities.
Although there are proven risks involved with staged bilateral ARCR within certain time frames, rotator cuff tears can be debilitating and multiple surgeries within a shorter time span may be necessary. Deciding which shoulder to have operated on first and the timing between surgeries was the primary focus of the current study. Shoulder function (83.9% left, 88.1% right), daily pain (79.3% left, 81.0% right), and night pain (71.3% left, 81.0% right) were the most influential factors when deciding which shoulder to fix first. These results align with the most substantial indications for RCRs: pain, weakness, and loss of range of motion. The period of nonoperative management of rotator cuff tears is used to monitor for improvement in pain and function. Without substantial improvement, patients will seek out surgical intervention, which aligns with our findings. Hand dominance did not play an important role in decision-making. Only 56.7% of right hand–dominant and 25% of left hand–dominant patients elected to have their dominant shoulder operated on first. A study of 144 patients concluded that there was no difference in functional outcome of ARCR between dominant- and nondominant-side surgery. This further proves that patient preference is based on symptomatology.
Another factor that may impact a patient's decision to undergo surgical intervention is recommendations from other individuals. Although family recommendations did not play a substantial role in patient preference (50% right, 57.9% left), almost three-fourths of patients stated that surgeon recommendation was a “highly important” factor in decision-making. Patients rely on surgeon guidance to help them make difficult decisions. It is important to educate patients on their pathology and both the nonoperative and the operative treatments and allow them to make the final decision. Smits et al found that surgeons were more likely to recommend nonoperative treatment when patients only preferred operative treatment if there was consensus among surgeons that operative treatment was a useful option. This emphasizes the importance of strategies to help patients reflect on their values and ensure that their preferences are consistent with those values.
Incorporating all decision-making factors, patients reported a mean satisfaction score of 91.6 (100 being best) with the order of the surgeries and a mean satisfaction score of 87.3 with the timing of surgery. With significant improvement seen in ASES and SANE scores postoperatively, staged bilateral ARCR continues to be a reliable option for the surgical management of rotator cuff tears.
Surgeon Authors' Current Protocols
Part of the purpose of the current study was to determine if there is an optimal interval of waiting between staged bilateral RCRs. Our surgeons often counsel patients to proceed when they have some functional use of the previously operated on extremity. Historically, we have found this range to be from 8 weeks onward depending on surgeon discretion and the size of the tear and functional deterioration on the second extremity. One author recommends a minimum of 4 months between procedures, as most patients will have acceptable functional use of the first operated on extremity. However, our institution does not currently have a standard protocol in place related to the timing of staged repairs. Based on our study's findings and a review of the literature, there may be no “ideal” interval between repairs because several factors exist: the recovery of the index RCR, degree of dysfunction and pain of the contralateral shoulder, and risk of tear progression if surgery is delayed. Further investigation may be warranted with a larger patient population to definitively determine an ideal interval.
Limitations
This study had limitations. First, this was a retrospective study. Because data were used that were originally collected for other purposes, not all relevant information was available for every patient. Second, patients were recruited by convenience sampling and thus were prone to selection bias and may not represent the general population. There was an overall low rate of patient responses via REDCap online surveys and follow-up phone calls. Of the 255 patients who met the inclusion criteria, 90 (35.3%) responded and were included in the study. Each patient was sent a REDCap online survey that was followed by reminder emails. If patients did not complete the online survey, phone calls were made to try to reach them for their response. Conclusions were reached with the responses obtained; however, a larger response rate may have altered our findings. Third, this study was subject to recall bias because patient measures were subjective and patients were, at a minimum, 2 years postoperatively from their second surgery. Fourth, although patients had staged surgery, it is unclear from our data set if both shoulders were symptomatic on initial presentation. Hence, the decision to undergo surgery on one side vs another may not have been preference but rather due to symptom presentation. Hand dominance was included in the initial data set with hopes of discovering if patients preferred to have their dominant arm operated on first. Because of the low response rate (only 8 patients were left-handed), a meaningful conclusion could not be reached. Future studies with larger patient populations may investigate the importance of hand dominance in staged RCRs. Finally, confounding factors, such as other concomitant shoulder pathology, may have hindered patient outcomes.
Conclusion
Most patients who underwent short-interval staged bilateral RCR were satisfied with the order and timing of the surgeries, and the laterality of the index procedure did not influence postoperative outcome. Decision-making factors such as night pain and function played a key role in the timing and order of bilateral RCRs.
References
- 1. Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31(4):589–604–. PMID:
- 2. Aleem AW, Syed UAM, Wascher J , , et al. Functional outcomes after bilateral arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25(10):1668–1673–. PMID:
- 3. Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease: a comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88(8):1699–1704–. PMID:
- 4. Keener JD, Steger-May K, Stobbs G, Yamaguchi K. Asymptomatic rotator cuff tears: patient demographics and baseline shoulder function. J Shoulder Elbow Surg. 2010;19(8):1191–1198–. PMID:
- 5. Ro KH, Park JH, Lee SH, Song DI, Jeong HJ, Jeong WK. Status of the contralateral rotator cuff in patients undergoing rotator cuff repair. Am J Sports Med. 2015;43(5):1091–1098–. PMID:
- 6. Weekes DG, Campbell RE, Allegretto JR , , et al. A prospective study of patient factors and decision-making for surgical repair of symptomatic full-thickness rotator cuff tears. Orthopedics. 2020;43(2):85–90–. PMID:
- 7. Wang C, Yang P, Zhang D , , et al. Bilateral single-staged arthroscopic rotator cuff repair is comparable to staged procedures: a retrospective follow up study of 2 years. BMC Musculoskel Dis. 2021;22(1):409.
- 8. Kim HJ, Kee YM, Kim JY, Rhee YG. Safe time frame of staged bilateral arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2019;28(9):1707–1715–. PMID:
- 9. Odum SM, Troyer JL, Kelly MP, Dedini RD, Bozic KJ. A cost-utility analysis comparing the cost-effectiveness of simultaneous and staged bilateral total knee arthroplasty. J Bone Joint Surg Am. 2013;95(16):1441–1449–. PMID:
- 10. Pak CH, Moon YL, Sim SW, Elsayed MI. Bilateral arthroscopic rotator cuff repair using a single-stage procedure. Orthopedics. 2015;38(5):e423–e427–. PMID:
- 11. Chu J, Shieh JS, Wu K , , et al. Simultaneous or staged bilateral arthroscopic rotator cuff repair: an observational study of intraoperative and postoperative outcomes. Orthop J Sports Med. 2021;9(10):23259671211041994. PMID:
- 12. Cancienne JM, Denard PJ, Garrigues GE, Werner BC. The relationship of staged, bilateral arthroscopic primary rotator cuff repair timing and postoperative complications. Am J Sports Med. 2021;49(8):2027–2034–. PMID:
- 13. Thigpen CA, Shaffer MA, Gaunt BW, Leggin BG, Williams GR, Wilcox RB III. The American Society of Shoulder and Elbow Therapists' consensus statement on rehabilitation following arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25(4):521–535–. PMID:
- 14. Rhee SM, Kim DH, Kim SH, Jeong HJ, Oh JH. The clinical outcomes and their associated factors in staged bilateral arthroscopic rotator cuff repair. Arthroscopy. 2018;34(10):2799–2807–. PMID:
- 15. Wolf BR, Dunn WR, Wright RW. Indications for repair of full-thickness rotator cuff tears. Am J Sports Med. 2007;35(6):1007–1016–. PMID:
- 16. Kelly MA, Mc Donald CK, Boland A, Groarke PJ, Kaar K. The effect of hand dominance on functional outcome following single row rotator cuff repair. Open Orthop J. 2017;11:562–566–. PMID:
- 17. Smits LJH, Wilkens SC, Ring D, Guitton TG, Chen NC. Do patient preferences influence surgeon recommendations for treatment? Arch Bone Jt Surg. 2019;7(2):118–135–. PMID: