Introduction
Health anxiety, often designated as hypochondriasis, is a global health problem on the rise affecting 1–5% of the adult population (Fink et al., ; Kosic, Lindholm, Jarvholm, Hedman-Lagerlof, & Axelsson, ; Sunderland, Newby, & Andrews, ) and is very common among medical patients (Weck, Richtberg, & Neng, ). It is characterized by obsessive rumination with fears of harboring a serious illness and tends to persist despite medical reassurance (Fink et al., ). Although patients frequently attend medical care, their primary disorder is rarely recognized and thus remains untreated. Consequently, health anxiety is associated with extensive use of health care services (Fink, Ornbol, & Christensen, ), increased rates of occupational disability, depression and anxiety, and lowered quality of life (Sunderland et al., ). These costs are potentially avoidable if effective treatment is available.
Fortunately, long-term cost-effective treatments do exist (Axelsson & Hedman-Lagerlof, ; Thomson & Page, ); so far, cognitive behavioral therapy (CBT) being the most frequently investigated. However, acceptance and commitment therapy (ACT), has also demonstrated promising results across a wide range of mental health problems (A-Tjak et al., ; Frostholm & Rask, ), including health anxiety (Eilenberg, Fink, Jensen, Rief, & Frostholm, ; Eilenberg, Hoffmann, Jensen, & Frostholm, ). ACT is considered a ‘third wave’ CBT approach that aims to increase patients' behavioral repertoire, also designated as ‘psychological flexibility’, in two ways: firstly by changing the way patients relate to distressing symptoms by gradually increasing the ability to ‘open up’ and ‘stay present’ to thoughts, feelings, and bodily sensations, and secondly to enhance engagement with value-based activities to create a meaningful life based on long-term goals and values (Hayes, ). In spite of evidence-based treatments, the limited availability of clinics or specialists and regional variability, restrict patients' access to treatment. Therefore, low intensity and easily accessible treatment options are needed (Holmes et al., ).
Harnessing new technologies has the potential to greatly increase the availability of evidence-based treatments (Holmes et al., ). One of these developments is internet-delivered psychological treatment programs, which consist of highly structured online modules accompanied by homework assignments and often clinician guidance. The common principle is that the treatment mirrors the same techniques and processes of change as in traditional face-to-face treatment. Internet-delivered treatment has several advantages such as independence of geographical distance to the clinic, fewer or no scheduled appointments, less interference with patients' daily life, and possibly less perceived stigma (Brown, Glendenning, Hoon, & John, ; Rusch, Angermeyer, & Corrigan, ). A recent meta-analysis found that internet-delivered CBT (iCBT) produced equivalent effects to face-to-face treatment for anxiety and mood disorders (Carlbring, Andersson, Cuijpers, Riper, & Hedman-Lagerlof, ). Four RCTs from two research groups have already shown that iCBT was effective, long-lasting, and cost-effective for health anxiety (Hedman, Axelsson, Andersson, Lekander, & Ljotsson, ; Hedman et al., , , ; Newby et al., ). However, importantly, internet-delivered ACT (iACT) seems to compare favorably to iCBT in terms of mean adherence to protocol (Brown et al., ), which is a well-documented limitation restraining the potential effectiveness of internet-delivered treatments (Donkin et al., ). In a recent pilot study, we showed that iACT was a feasible and potentially efficacious treatment for health anxiety (Hoffmann, Rask, Hedman-Lagerlof, Ljótsson, & Frostholm, ). Still, the efficacy of iACT for health anxiety needs to be investigated in a randomized design.
Although one of the key goals when developing a new treatment is to avoid harm, the potential adverse events are often neglected when examining psychological treatments. A meta-analysis of individual treatment responses found that symptom deterioration was frequently reported in iCBT (Rozental, Magnusson, Boettcher, Andersson, & Carlbring, ) underlining the need for additional systematic assessment of adverse events.
The aim of the study
The aim of this study was to investigate the efficacy of iACT for health anxiety in an RCT. Based on our previous pilot study (Hoffmann et al., ), we expected that iACT would lead to clinically significant reductions of health anxiety, somatic symptoms, symptoms of anxiety and depression as well as increases in quality of life and psychological flexibility compared with an active control condition receiving an internet-delivered discussion forum (iFORUM). In addition, adverse events such as symptom deterioration and negative effects attributed to treatment were systematically examined.
Methods
Study design and participants
This study is an individually randomized, controlled trial of iACT v. an active control condition encompassing iFORUM, performed at the Research Clinic for Functional Disorders and Psychosomatics at Aarhus University Hospital, Denmark. Patients self-referred through the clinic's webpage using their unique national identification number to log into a portal consisting of; (1) written consent allowing the clinician to access the patient's health information in the national Electronic Patient Record prior to assessment, (2) subjective description of their health problem by enquiring ‘Please describe your health anxiety in your own words and how you feel at the moment?’, and (3) baseline questionnaires measuring health anxiety symptoms among other measures of mental and physical health. Information about this study was available on the clinic's webpage (http://funktionellelidelser.dk) and on the Danish anxiety association's webpage (www.angstforeningen.dk), and electronic information about the trial was also sent to general practitioners (GP) nationwide. To further facilitate recruitment, two patient videos were produced to illustrate symptoms of health anxiety and the principles of internet-delivered treatment. These were available on the webpage and shared through the hospital's Facebook page.
Eligible patients had severe health anxiety according to the empirically based diagnostic criteria established by Fink et al. () and a self-reported Whiteley Index-7 (WI-7) score of >21.4 (scale range 0–100), which is established as a clinically relevant cut-off score (Fink et al., ). Health anxiety had to be the principal diagnosis if comorbid disorders were present according to the diagnostic assessment based on the 10th edition of the International Classification of Diseases and Related Health Problems (ICD-10) (World Health Organization, Collaborating Centres for Classification of Diseases, ). Patients were ≥18 years and able to speak, read, and write Danish, were Danish residents, and had access to computer and internet. Exclusion criteria were acute suicidal risk, current abuse of narcotics, alcohol, or non-prescribed medication, life-time diagnosis of psychoses, bipolar affective disorder or depression with psychotic symptoms (ICD-10: F20–29, F30–31, F32.3, F33.3), and pregnancy at time of trial entry. Other exclusion criteria were former treatment for health anxiety at the clinic, lack of informed consent, and changes in anxiety medication within the past 2 months. If patients had changed dose or recently started anxiety medication, they were preliminarily included and reassessed for eligibility after 2 months of stable medication. Patients were asked to keep a stable dosage throughout the trial.
Assessment
Self-referrals were initially screened by a psychologist (first author, DH) in accordance with the eligibility criteria, and ineligible patients were telephoned and advised to consult their GP. Potentially eligible patients were invited to a thorough video-based clinical assessment. Health information from referral questionnaires and the electronic patient records were examined prior to the assessment. Trained psychologists and a psychiatrist conducted a shortened and modified version of the diagnostic interview Schedules for Clinical Assessment in Neuropsychiatry (SCAN) (Petersen et al., ) assessing health anxiety (Fink et al., ) and the corresponding diagnoses of hypochondriacal disorder according to ICD-10 (World Health Organization, Collaborating Centres for Classification of Diseases, ) as well as illness anxiety disorder (IAD) and somatic symptom disorder (SSD) according to DSM-5, respectively (American Psychiatric Association, ). The interview also screened for major depressive disorder, anxiety disorders, obsessive-compulsive disorder, and somatoform disorders based on the criteria from ICD-10. The assessment lasted 1–2 hours including a brief patient history, a clinical summary, and information about the project. Subsequently, eligible patients had 2 weeks to provide written consent and complete the randomization through the web portal. This allowed time for patients to consider whether they wanted to proceed to the final inclusion and randomization.
With consent, assessments were video recorded, and assessors rated and discussed clinical cases in supervision. The treatment, as well as technical issues, were also discussed at the weekly supervisions. An external supervisor with extensive experience with internet-delivered treatment and health anxiety (EHL) participated monthly. Medical supervision was provided by a psychiatrist (CUR) and by medical doctors at the clinic when needed.
Randomization and masking
Eligible patients were randomly assigned to receive either iACT or iFORUM in a 1:1 computer-generated ratio with no restrictions or matching allowing up to 150 patients in total. After clinical assessment, the randomization followed automatically the next time the patient logged in, i.e. the assessor was blinded to the forthcoming allocation. Randomized patients were allocated to the next available therapist; yet pairing patients to the initial assessor when possible.
Intervention
The iACT program was based on an existing, empirically supported manual for group-based ACT (ACT-G) (Eilenberg et al., ). The treatment platform was developed as a web app with a responsive design allowing access through computers, mobile devices, and tablets. The development, content, and feasibility of iACT have been presented elsewhere (Hoffmann et al., ). In brief, iACT was a clinician-guided, self-help program consisting of seven modules opened consecutively over 12 weeks of treatment (see online Supplementary material online for a ‘Program demonstration’). Four psychologists and a trainee psychology student provided the written clinical guidance, which was not restricted by predetermined templates. Messages were answered within 48 h on weekdays. The modules featured fixed content such as text, illustrations, audio files (mindfulness exercises), video clips, and interactive worksheets automatically stored and shared with the clinician, and an encrypted and embedded message system enabling written communication. An automatic (mobile) text message system notified patients about new modules, messages, questionnaires, or low activity. Likewise, a clinician-monitored control panel notified clinicians about patients' activity (e.g. missed questionnaires).
The iFORUM consisted of seven discussion forums consecutively opened over 12 weeks with a new topic related to health anxiety such as health care, relationships, or work. Patients were encouraged to share their experiences anonymously. The discussions were monitored for ethical reasons, but aside from that, there was no clinician interference. Thus, iFORUM aimed to control for the effect of emotional support and having contact to the health care system and can therefore not be considered as an active specific treatment but as an active control condition with unspecific effects. After 6-month follow-up (6-MFU), the patients from iFORUM were invited to cross over to iACT.
Outcomes
Self-report Questionnaires were administered at baseline, month 1 (randomization), 2 (4 weeks into treatment), 3 (8 weeks into treatment), 4 (post-treatment), and 10 months after baseline (i.e. 6-MFU) (see online Supplementary material online regarding ‘Questionnaires’). Patients were telephoned and asked to answer the primary outcome measure if data were missing at post-treatment or at 6-MFU.
The primary outcome was changes in self-reported health anxiety symptoms from baseline to 6-MFU measured by the 7-item WI-7 (Fink et al., ). Patients rated their illness worries during the last 4 weeks on a 5-point rating scale from 1 = ‘Not at all’ to 5 = ‘A lot’ (scale range: 7–35) in response to questions like: ‘Do you worry a lot about your health’. The WI-7 has been shown to have high reliability and good external validity (Christensen, Bech, & Fink, ). To further enable comparison with former trials, we included the Health Anxiety Inventory Short-form (SHAI) as a secondary outcome measuring 18 health anxiety items on a categorical 4-point scale from 1 to 4 (scale range: 18–72) (Salkovskis, Rimes, Warwick, & Clark, ). The SHAI has demonstrated high reliability, criterion validity, and sensitivity to treatment (Alberts, Hadjistavropoulos, Jones, & Sharpe, ).
Other secondary outcomes were symptoms of depression, anxiety, and somatic symptoms measured on subscales of the Symptom Checklist-92 (SCL-92) (Derogatis & Cleary, ), namely SCL-dep (13 items, scale range: 13–65), SCL-anx (10 items, scale range: 10–50), and SCL-som (12 items, scale range: 12–60). All items were rated on a 5-point rating scale ranging from 1 = ‘Not at all’ to 5 = ‘A lot’. Quality of life was measured on the 5-item WHO Well-being Index (WHO-5) (Topp, Ostergaard, Sondergaard, & Bech, ) on a 6-point rating scale ranging from 0 = ‘At no time’ to 5 = ‘All of the time’ (scale range: 0–25). Psychological flexibility was measured by the 7-item Acceptance and Action Questionnaire-II (AAQ-II) (Bond et al., ) employing a 7-point rating scale from 1 = “Never true” to 7 = ‘Always true’ (scale range: 7–49).
All scales were transformed into a 0–100 score point scale ((score-min)/(max-min)) × 100 to facilitate comparison of changes between measures in this study and previous ones (Eilenberg et al., ).
Adverse events encompassing symptom deterioration on the WI-7 from baseline to 6-MFU, events requiring acute hospitalization, and negative effects were summarized. Negative effects were measured at 4 months (post-treatment) by the 32-item Negative Effects Questionnaire (NEQ) measuring six factors encompassing symptoms, hopelessness, failure, stigma, dependency, and quality (Rozental, Kottorp, Boettcher, Andersson, & Carlbring, ). Each negative effect was attributed to either ‘The treatment I received’ or ‘Other circumstances’, and the impact was rated from 0 = ‘Not at all’ to 4 = ‘Extremely’.
Adherence was summarized as the median number of completed modules, and treatment completion was defined a priori as three or more modules completed (Hoffmann et al., ). Patient activity also encompassed number of logins, submitted worksheets, and messages sent. Treatment satisfaction was rated on a 6-point rating scale at post-treatment by the following questions; ‘Would you recommend the treatment program to others’, ‘What do you think about receiving psychological treatment over the internet’ and ‘How useful did you find the information in the internet program’?
Statistical analysis
Based on data from a previous RCT of ACT-G from the clinic (Eilenberg et al., ), we expected a 17-point difference in improvement between-groups on the WI-7. Power calculations showed that 45 patients in each group would be required to yield 80% power to detect a difference of 17 points (0–100) with an alpha level of 0.05 and 25% data attrition.
Data were summarized using either the mean and standard deviation (S.D.) for normally distributed variables, the median and interquartile range (IQR) for skewed variables, or the count and percentage for categorical variables. The primary outcome (WI-7) and the secondary outcomes (SHAI, SCL-dep, SCL-anx, SCL-som, WHO-5 and AAQ-II) were all analyzed using a linear mixed model with the given outcome as the dependent variable and group × time as a categorical variable and their interaction as the only independent variables. Using this model, we first calculated the mean score of the outcome in both groups at each time point and then tested whether there was a significant interaction effect (i.e. different changes over time in the groups). If this was the case, the treatment effect was calculated as the mean difference in change over time from baseline to 6-MFU. The model was also used to calculate between-group effect sizes at all timepoints (Cohen's d), i.e. the difference between the mean scores of iACT and iFORUM at each time point divided by the pooled S.D., and within group effect sizes (standardized response mean, SRM), i.e. the difference between the mean scores at 6-MFU and baseline divided by the S.D. of the difference. Due to a baseline difference in age, we made a sensitivity analysis in which we adjusted for age in our linear mixed model for the WI-7.
Clinically significant improvement was calculated using the criteria proposed by Fallon et al. (), where patients had to have a double improvement of 25% or greater over baseline scores on two measures of health anxiety, namely the WI-7 and the SHAI in our trial. The proportion of patients in the two groups with a clinically significant improvement was compared using a risk ratio (RR), and an estimate was calculated of the number needed to treat (NNT) to achieve one additional case of clinically significant improvement. Furthermore, we calculated and compared the proportion of patients scoring below the cut-off for non-clinical cases on the WI-7 < 21.4 at 6-MFU using a RR (Fink et al., ).
Finally, negative effects were summarized based on the NEQ. We tested whether negative effects were associated with treatment completion, i.e. number of modules completed or symptom deterioration on WI-7 from baseline to 6-MFU by using Wilcoxon rank-sum tests. All analyses were done on an intention to treat (ITT) basis using Stata version 15.1 for Windows.
Results
Self-referral
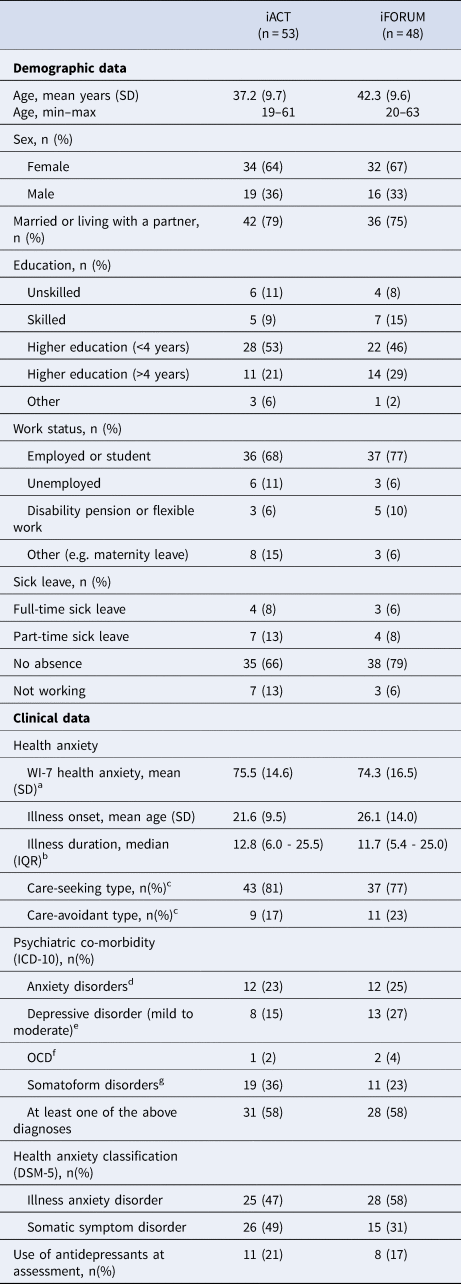
Between 18 March 2016 and 29 March 2017, 151 adult patients self-referred to the trial (Fig. 1). Of the total, 38% found the treatment via the internet themselves, whereas the remaining patients learned about it from their GP (23%), a friend (15%), through advertisement (11%), or other sources (13%). In total, 132/151 (87%) were screened for eligibility, and 101/151 patients (66%) were included in the trial. The main reason for exclusion at assessment was another principal psychiatric disorder. Only six eligible patients declined participation. Compared to the final sample, they did not differ on demographic characteristics or baseline level of health anxiety [t(105) = 1.48, p= 0.14]. Eligible patients were randomly assigned to receive iACT (n = 53) or iFORUM (n = 48). Baseline demographics and clinical characteristics are summarized in Table 1.
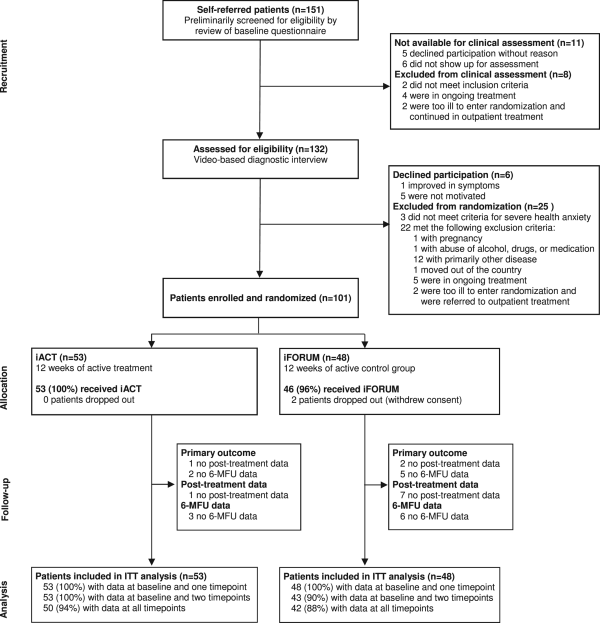
Fig. 1
CONSORT Trial profile. iACT, internet-delivered Acceptance and Commitment Therapy.
Attrition and adherence
There was no data loss at baseline and at randomization (Fig. 1). Full primary outcome data at all time points were available for 90/101 (89%) patients, and partial data including both baseline and 6-MFU were available for 94/101 (93%) patients. Two patients withdrew their consent but were still included in the ITT.
In terms of treatment adherence, the median number of completed modules was 7 (IQR 5–7) in iACT and 2 (IQR 0–7) in iFORUM (see online Supplementary material online regarding ‘Treatment adherence’). No patients receiving iACT completed less than three modules which were previously defined as cut-off for treatment non-completion (Hoffmann et al., ). Patients in iACT sent a median of 14 (IQR 10–20) messages to their clinician, whereas the median number of postings among patients in iFORUM was 2.5 (IQR 0–6.5). The majority of patients in iFORUM (30/48 (63%)) posted at least one message.
Primary outcome measure
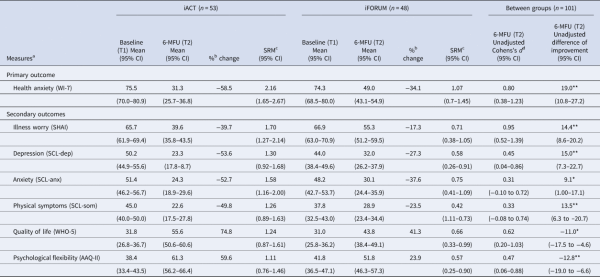
Figure 2 displays the improvement on the primary outcome measure, WI-7, and Table 2 presents the means, confidence interval (CI), and effect sizes at baseline and 6-MFU. There was different development over time in the two groups on WI-7 as indicated by the significant interaction effect between group and time [χ2(5) = 39.97, p < 0.001]. The unadjusted difference in mean improvement from baseline to 6-MFU was 19.0 points (95% CI 10.8–27.2) in favor of iACT. The standardized between-group effect size on WI-7 at 6-MFU was d= 0.80 (95% CI 0.38–1.23).
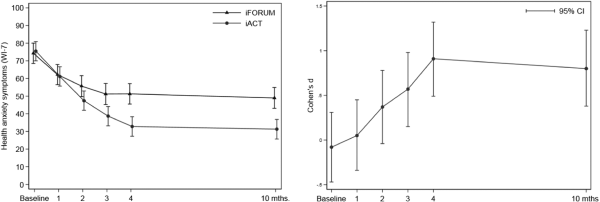
Fig. 2
Effect of the treatment on the primary outcome: health anxiety symptoms. Effect of the treatment on the primary outcome WI-7 based on a linear mixed model. The left graph shows the mean values and 95% CI of two treatment groups at each time point (smaller values are in favor of the treatment). The right graph illustrates the unadjusted Cohen's d effect sizes with 95% CI at all time points throughout treatment. Positive effect sizes are in favor of the treatment. Baseline corresponds to the time of self-referral and 1 month to randomization and treatment initiation after the diagnostic assessment.
From baseline to 6-MFU, 34/50 (68%) patients in iACT had a clinically significant improvement of ≥25% improvement over baseline on both the WI-7 and SHAI compared to 14/43 (33%) patients in iFORUM, corresponding to an RR of 2.09 (CI 95% 1.31–3.33, p = 0.002). The estimated NNT to achieve one additional case of clinically significant improvement with iACT compared to iFORUM was 2.8 (CI 95% 1.8–6.1, p< 0.001).
Furthermore, 18/51 (35%) patients in iACT had a WI-7 score <21.4 score point at 6-MFU and were no longer clinical cases compared to 7/43 (16%) patients in iFORUM which were a statistically significant between-group difference (RR 2.17; 95% CI 1.00–4.70, p= 0.050).
When adjusting for age, the treatment effect was of a similar magnitude as the unadjusted treatment effect, 19.0 points (95% CI 10.8–27.2).
3.4 Secondary outcome measures
All secondary outcomes revealed a significant interaction effect between group and time with p values ranging from <0.001 to 0.009. As seen in Table 2, the between-group effect sizes ranged from small to large at 6-MFU in favor of iACT (d= 0.31 to 0.95).
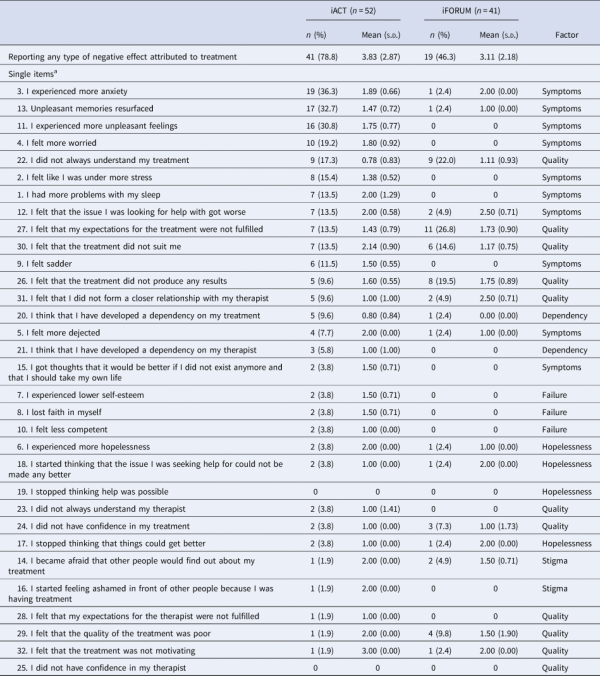
3.5 Adverse events
No patients experienced any serious adverse events requiring acute hospitalization, and only patients in iFORUM experienced symptom deterioration on the WI-7 (5/43 (11.6%)). At least one negative effect attributed to treatment was reported by 41/52 (78.8%) and 19/41 (46.3%) patients in iACT and iFORUM, respectively, with a mean number of 3.8 and 3.1 among the affected patients (Table 3). The item most frequently reported in iACT was; ‘I experienced more anxiety’ (item 3). There were few negative effects related to dependency of the treatment or clinician, feelings of failure, hopelessness or stigma. Negative effects were neither associated with treatment completion in iACT (z = 0.163, p= 0.87) and iFORUM (z = −1.326, p= 0.19), nor to symptom deterioration on WI-7 from baseline to 6-MFU in iACT [t(49) = 0.195, p= 0.85] and iFORUM [t(41) = −0.911, p= 0.37].
Additional help-seeking and treatment satisfaction
No statistically significant difference was found in additional help-seeking during treatment in both groups [χ2(1) = 0.71, p= 0.40]. Regarding patient satisfaction, 47/52 (90%) of the patients receiving iACT reported that they would ‘Definitely’ or ‘Most likely’ recommend the treatment program to others. Most patients, 46/52 (88%), found receiving treatment over the internet either ‘Very good’ or ‘Good’, and the information in iACT was found to be ‘Very useful’ or ‘Mostly useful’ to 49/52 (94%) patients in iACT.
Discussion
Main findings
We found that 12 weeks of clinician-guided iACT significantly decreased symptoms of health anxiety compared to an active control condition. Improvements were sustained at 6-MFU with an unadjusted mean difference of 19.0 points and a large standardized between-group effect size on the primary outcome. The NNT was 2.8 to achieve one case of clinically significant improvement, and 35% of patients in iACT were no longer clinical cases (Fink et al., ). In addition, patients receiving iACT also reported significant improvements on all secondary outcomes compared to patients in iFORUM, and no patients in iACT reported symptom deteriorations on the primary outcome at 6-MFU. The negative effects attributed to treatment were neither associated with treatment completion nor with the final outcome. Taken together, the results showed that clinician-guided iACT can be a highly effective and acceptable treatment for patients with health anxiety.
Comparison to other studies
Since this was the first RCT to investigate iACT for health anxiety, our results cannot be directly compared to studies using the same treatment model and type of delivery. However, one RCT investigated group-based ACT (ACT-G) for health anxiety and found an unadjusted mean difference on the WI-7 of 20.5 points (95% CI 11.7–29.4) from baseline to 6-MFU (Eilenberg et al., ), which is almost equivalent to the effect of iACT. Moreover, 14/52(27%) patients attending ACT-G were no longer clinical cases as judged by the cut-off score on WI-7 compared to 35% in iACT thus suggesting comparable efficacy of face-to-face and internet-delivered ACT for health anxiety. The content of the iACT program was based on the ACT-G manual, which supports the notion that internet-delivered treatment is a new and feasible way to deliver the same therapeutic principles.
Our results were also in accordance with the four previous trials on iCBT for health anxiety (Hedman et al., ; ), IAD and SSD (Hedman et al., ; Newby et al., ). Even though comparison is hampered by the various outcome measures applied, all studies with a control condition found large between-group effect sizes on their primary outcome (Hedman et al., , ; Newby et al., ).
In terms of adherence, iACT is said to compare favorably to iCBT (Brown et al., ). A meta-analysis found that patients in iCBT in average completed 81% of their treatment (van Ballegooijen et al., ). In our study, patients averagely completed 88% of their treatment modules. This compares favorably to the iCBT studies for health anxiety were patients averagely completed between 57 and 79% of their treatment modules (Hedman et al., , ; Newby et al., ). Poor adherence is a widespread challenge, which may limit the potential effectiveness of internet-delivered treatments (Donkin et al., ). The particular focus on personal values in ACT and creating a meaningful life may be a possible strength of this treatment model motivating patients to stay in treatment. Accordingly, iACT seems to be a promising new treatment option for health anxiety with some potential advantages over iCBT when it comes to adherence. It may be as effective as iCBT, but more studies are needed; preferably directly comparing iACT to iCBT.
Adverse events
Adverse events are prevalent in psychotherapy but seldom reported (Rozental et al., ). In our trial, only patients in iFORUM (11.6%) reported symptom deterioration at 6-MFU. A meta-analysis of 29 iCBT studies found an average individual deterioration rate of 17.4% in control groups and 5.8% in active treatment groups (Rozental et al., ). The lesser deterioration in our control patients may be explained by iFORUM being an active control condition, and some patients did gain a small effect after participation. Still, no patients in iACT reported any deterioration which compares favorably to the reported 5.8% of patients in iCBT.
Regarding negative effects during iACT treatment, the most frequently reported factor was 'symptoms' among the six factors encompassing symptoms, hopelessness, failure, stigma, dependency, and quality (Rozental et al., ). Specifically, increased anxiety was reported by 36% of the patients in iACT (item 3). Even though negative effects have not been thoroughly examined in the previous trials, two of the iCBT trials for health anxiety assessed negative effects using an open-ended one-item question (Hedman et al., , ). They also found increased anxiety as the main patient-reported negative effect. Consequently, it seems common that patients experience more anxiety during treatment while changing maladaptive behaviors. In our study, few negative effects were reported on dependency of the treatment or clinician, feelings of failure, and hopelessness. Interestingly, only 4% of patients in iACT reported fear of being perceived negatively for undergoing treatment, even though stigma related to psychiatric treatment is a common problem (Rusch et al., ). Internet-delivered treatment may inflict less stigma than face-to-face treatment and thus minimize a common barrier to treatment.
Strengths and limitations
Core strengths of the present study were: randomized design with an active comparison, thorough diagnostic assessment by trained clinicians, well-validated outcome measures, high level of adherence, and low attrition rates. Limitations included lack of post-treatment clinician-based diagnostic assessment, non-blinded allocation for the patients, and treatment crossover which may have confounded the results of iFORUM by decreasing the patients' expectations to its potential benefit. Still, most patients in iFORUM reported small improvements suggesting that it was an active and beneficial control condition. Lastly, applying self-referral could affect the generalizability of the study sample and results. However, in a secondary analysis, we found only minor demographic and clinical differences among self-referred patients in iACT and clinician-referred patients in ACT-G suggesting generalizability of our study sample (Hoffmann, Rask, Hedman-Lagerlof, Eilenberg, & Frostholm, ). Altogether, these limitations are not likely to greatly affect the significant results of this study.
Clinical implications
Patients with health anxiety have often been considered treatment-resistant. There is now substantial evidence for efficacious treatments, and we found that iACT is a new effective, feasible, and easily accessible treatment with minimal adverse effects. The beneficial effects of iACT were obtained without the clinician ever meeting the patient face-to-face during referral, assessment, and treatment. This may have substantial clinical value since harnessing these new technologies has the potential of providing evidence-based treatment to many patients, which is often limited due to capacity, geographical distance, time, and perceived stigmatization. Moreover, the high degree of flexibility reduces inference with patients' daily life, and it might have incremental economic benefits such as the patient not having to take time off work. Harnessing technology such as patient self-referral and internet-delivered treatment may have broad application in the dissemination of health care services. In future studies, we plan to investigate specific mechanisms of change to better understand ‘how’ and ‘why’ iACT translates into the events leading to a successful outcome.
Conclusions
In Conclusion, patient self-referral and 12 weeks of clinician-guided iACT was an effective and acceptable treatment setup that improved health anxiety and overall mental health. The study contributes to the development of feasible, easily accessible treatment options for patients with health anxiety who often risk being undetected and untreated.
Acknowledgements
We would like to thank the clinical staff at the Research Clinic for Functional Disorders and Psychosomatics at Aarhus University Hospital Tina Carstensen, Greta Lassen Lund and Katrine Ingeman Beck for their commitment as therapists in the study. Many thanks to our colleagues Malene Skjøth for language revision, research assistant Lise Hassing for monitoring iFORUM and Nicolaj Knudsen for his skilful development of the treatment platform. In particular, we wish to thank the patients for their participation. We thank the Danish foundation TrygFonden for supporting this work (grant no. 102644). The funder of the study was not involved in the study design, patient recruitment, data collection, data analysis, data interpretation, or writing of the report.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291720001312.
Conflicts of interests
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The study was approved by the Ethical Committee in Central Region Denmark, January 2016 (ID no. 1-10-72-321-15) and by the Danish Data Protection Agency, February 2016 (ID no. 1-16-02-51-16). The protocol is published online at clinicaltrials.gov (ID no. NCT02735434).
References
- A-Tjak J. G., Davis M. L., Morina N., Powers M. B., Smits J. A., & Emmelkamp P. M. (2015). A meta-analysis of the efficacy of acceptance and commitment therapy for clinically relevant mental and physical health problems. Psychotherapy and Psychosomatics, 84(1), 30–36. doi:.
- Alberts N. M., Hadjistavropoulos H. D., Jones S. L., & Sharpe D. (2013). The short health anxiety inventory: A systematic review and meta-analysis. Journal of Anxiety Disorders, 27(1), 68–78. doi:.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association. doi: ISBN: 978-0-89042-554-1.
- Axelsson E., & Hedman-Lagerlof E. (2019). Cognitive behavior therapy for health anxiety: Systematic review and meta-analysis of clinical efficacy and health economic outcomes. Expert Review of Pharmacoeconomics & Outcomes Research, 19(6), 663–676. doi:.
- Bond F. W., Hayes S. C., Baer R. A., Carpenter K. M., Guenole N., Orcutt H. K., … Zettle R. D. (2011). Preliminary psychometric properties of the acceptance and action questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42(4), 676–688. doi:http://dx.doi.org/10.1016/j.beth.2011.03.007.
- Brown M., Glendenning A., Hoon A. E., & John A. (2016). Effectiveness of web-delivered acceptance and commitment therapy in relation to mental health and well-being: A systematic review and meta-analysis. Journal of Medical Internet Research, 18(8), e221. doi:.
- Carlbring P., Andersson G., Cuijpers P., Riper H., & Hedman-Lagerlof E. (2018). Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: An updated systematic review and meta-analysis. Cognitive Behaviour Therapy, 47(1), 1–18. doi:.
- Christensen K. S., Bech P., Fink P. (2010). Measuring mental health by questionnaires in primary care – unidimensionality, responsiveness and compliance. European Psychiatric Review, 3(1), 9–12.
- Derogatis L. R., & Cleary P. A. (1977). Confirmation of the dimensional structure of the SCL-90: A study in construct validation. Journal of Clinical Psychology, 33(4), 981–989. doi:http://dx.doi.org/10.1002/1097-4679(197710)33:4<981::AID-JCLP2270330412>3.0.CO;2-0.
- Donkin L., Christensen H., Naismith S. L., Neal B., Hickie I. B., & Glozier N. (2011). A systematic review of the impact of adherence on the effectiveness of e-therapies. Journal of Medical Internet Research, 13(3), e52. doi:.
- Eilenberg T., Fink P., Jensen J. S., Rief W., & Frostholm L. (2016). Acceptance and commitment group therapy (ACT-G) for health anxiety: A randomized controlled trial. Psychological Medicine, 46(1), 103–115. doi:.
- Eilenberg T., Hoffmann D., Jensen J. S., & Frostholm L. (2017). Intervening variables in group-based acceptance & commitment therapy for severe health anxiety. Behaviour Research and Therapy, 92, 24–31. doi:.
- Fallon B. A., Ahern D. K., Pavlicova M., Slavov I., Skritskya N., & Barsky A. J. (2017). A randomized controlled trial of medication and cognitive-behavioral therapy for hypochondriasis. The American Journal of Psychiatry, 174(8), 756–764. doi:.
- Fink P., Ewald H., Jensen J., Sorensen L., Engberg M., Holm M., & Munk-Jorgensen P. (1999). Screening for somatization and hypochondriasis in primary care and neurological in-patients: A seven-item scale for hypochondriasis and somatization. Journal of Psychosomatic Research, 46(3), 261–273. doi:.
- Fink P., Ornbol E., & Christensen K. S. (2010). The outcome of health anxiety in primary care. A two-year follow-up study on health care costs and self-rated health. PLoS ONE, 5(3), e9873. doi:.
- Fink P., Ornbol E., Toft T., Sparle K. C., Frostholm L., & Olesen F. (2004). A new, empirically established hypochondriasis diagnosis. The American Journal of Psychiatry, 161(9), 1680–1691. doi:.
- Frostholm L., & Rask C. U. (2019). Third wave treatments for functional somatic syndromes and health anxiety across the age span: A narrative review. Clinical Psychology in Europe, 1(1), 1–33. doi:.
- Hayes S. C. (2016). Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies – republished article. Behavior Therapy, 47(6), 869–885. doi:.
- Hedman E., Andersson G., Andersson E., Ljotsson B., Ruck C., Asmundson G. J., & Lindefors N. (2011). Internet-based cognitive-behavioural therapy for severe health anxiety: Randomised controlled trial. The British Journal of Psychiatry: The Journal of Mental Science, 198(3), 230–236. doi:.
- Hedman E., Andersson E., Lindefors N., Andersson G., Ruck C., & Ljotsson B. (2013). Cost-effectiveness and long-term effectiveness of internet-based cognitive behaviour therapy for severe health anxiety. Psychological Medicine, 43(2), 363–374. doi:.
- Hedman E., Axelsson E., Andersson E., Lekander M., & Ljotsson B. (2016). Exposure-based cognitive-behavioural therapy via the internet and as bibliotherapy for somatic symptom disorder and illness anxiety disorder: Randomised controlled trial. The British Journal of Psychiatry: The Journal of Mental Science, 209(5), 407–413. doi:.
- Hedman E., Axelsson E., Gorling A., Ritzman C., Ronnheden M., El Alaoui S., … Ljotsson B. (2014). Internet-delivered exposure-based cognitive-behavioural therapy and behavioural stress management for severe health anxiety: Randomised controlled trial. The British Journal of Psychiatry : The Journal of Mental Science, 205(4), 307–314. doi:.
- Hoffmann D., Rask C. U., Hedman-Lagerlof E., Eilenberg T., & Frostholm L. (2019). Accuracy of self-referral in health anxiety: Comparison of patients self-referring to internet-delivered treatment versus patients clinician-referred to face-to-face treatment. BJPsych Open, 5(5), e80. doi:.
- Hoffmann D., Rask C. U., Hedman-Lagerlof E., Ljótsson B., & Frostholm L. (2018). Development and feasibility testing of internet-delivered acceptance and commitment therapy for severe health anxiety: Pilot study. JMIR Mental Health, 5(2), e28. doi:.
- Holmes E. A., Ghaderi A., Harmer C. J., Ramchandani P. G., Cuijpers P., Morrison A. P., … Craske M. G. (2018). The lancet psychiatry commission on psychological treatments research in tomorrow's science. The Lancet Psychiatry, 5(3), 237–286. doi:.
- Kosic A., Lindholm P., Jarvholm K., Hedman-Lagerlof E., & Axelsson E. (2020). Three decades of increase in health anxiety: Systematic review and meta-analysis of birth cohort changes in university student samples from 1985 to 2017. Journal of Anxiety Disorders, 71, 102208. doi:.
- Newby J. M., Smith J., Uppal S., Mason E., Mahoney A. E. J., & Andrews G. (2018). Internet-based cognitive behavioral therapy versus psychoeducation control for illness anxiety disorder and somatic symptom disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 86(1), 89–98. doi:.
- Petersen M. W., Schroder A., Jorgensen T., Ornbol E., Dantoft T. M., Eliasen M., & Fink P. (2019). RIFD – A brief clinical research interview for functional somatic disorders and health anxiety. Journal of Psychosomatic Research, 122, 104–111. doi:.
- Rozental A., Kottorp A., Boettcher J., Andersson G., & Carlbring P. (2016). Negative effects of psychological treatments: An exploratory factor analysis of the negative effects questionnaire for monitoring and reporting adverse and unwanted events. PLoS ONE, 11(6), e0157503. doi:.
- Rozental A., Magnusson K., Boettcher J., Andersson G., & Carlbring P. (2017). For better or worse: An individual patient data meta-analysis of deterioration among participants receiving internet-based cognitive behavior therapy. Journal of Consulting and Clinical Psychology, 85(2), 160–177. doi:.
- Rusch N., Angermeyer M. C., & Corrigan P. W. (2005). Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. European Psychiatry: The Journal of the Association of European Psychiatrists, 20(8), 529–539. doi:.
- Salkovskis P. M., Rimes K. A., Warwick H. M., & Clark D. M. (2002). The health anxiety inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine, 32(5), 843–853.
- Sunderland M., Newby J. M., & Andrews G. (2013). Health anxiety in Australia: Prevalence, comorbidity, disability and service use. The British Journal of Psychiatry: The Journal of Mental Science, 202(1), 56–61. doi:.
- Thomson A. B., & Page L. A. (2007). Psychotherapies for hypochondriasis. The Cochrane Database of Systematic Reviews, (4), CD006520. doi:.
- Topp C. W., Ostergaard S. D., Sondergaard S., & Bech P. (2015). The WHO-5 well-being index: A systematic review of the literature. Psychotherapy and Psychosomatics, 84(3), 167–176. doi:.
- van Ballegooijen W., Cuijpers P., van Straten A., Karyotaki E., Andersson G., Smit J. H., & Riper H. (2014). Adherence to internet-based and face-to-face cognitive behavioural therapy for depression: A meta-analysis. PLoS ONE, 9(7), e100674. doi:.
- Weck F., Richtberg S., & Neng J. M. (2014). Epidemiology of hypochondriasis and health anxiety: Comparison of different diagnostic criteria. Current Psychiatry Reviews, 10(1), 14–23. doi:.
- World Health Organization, Collaborating Centres for Classification of Diseases. (2014). ICD-10: International statistical classification of diseases and related health problems: Version 2014. Geneva: WHO.