What is already known about the topic?
Given the general frailty, higher frequency of chronic disease, and accelerated aging in prison, an increase in end-of-life situations among prisoners is likely.
To date, little is known about the need for and implementation of end-of-life care in prison healthcare systems, apart from the United States and the United Kingdom, where the majority of the existing studies focus.
What this paper adds?
The estimated annual prevalence of sick prisoners requiring end-of-life care was 15.2 (confidence interval: 12.5–18.3) per 10,000 prisoners.
The observed number of sick prisoners requiring end-of-life care was twice as high as the expected number, standardized for age and sex, based on the general population.
In all, 82% of the identified ill prisoners were eligible for temporary or permanent release on medical grounds according to French law, but only 62% of them submitted such a request.
Overall, regardless of the number of prisoners with need for end-of-life care, and despite legislation explicitly allowing requests for compassionate release in these cases, only a limited number of prisoners request such release, and of these requests, only half are granted.
Implications for practice, theory, or policy
Knowledge of prisoners’ profiles (medical, social, and jurisdictional) and the estimated prevalence of ill prisoners requiring palliative care could help French authorities to adequately develop national guidance for end-of-life care in this population.
Although compassionate release is possible, some ill prisoners requiring end-of-life care should remain in prison.
Background
After the heartbreaking call “Don’t let me die in prison” published in the JAMA almost 10 years ago, “Dying alone in prison” continues to be an urgent question of debate in Western societies,– reinforced by recent criticisms from official bodies in the face of difficulties in implementing compassionate release.–
The general frailty and co-existing health conditions (as well as frequent addiction problems), among criminals prior to their incarceration, are accentuated during custody by pathogenic factors associated with a lack of hygiene, lack of activity, deficient nutrition, excessive smoking, or even drug use, in addition to violence, anxiety, the stress of prison life, social isolation, and the hopelessness of living such a long time without experiencing freedom., Combined with a higher frequency of chronic disease– and substandard medical care,,, this phenomenon has led to an increase in end-of-life situations among prisoners, with the accompanying economical, legal, ethical, and societal repercussions.– Thus, ensuring adequate end-of-life care for dying prisoners has emerged in the past 20 years as a critical issue for correctional healthcare in Western countries.,,–
Different initiatives have been developed both inside and outside prisons to deal with this issue.,– In France, the organization of end-of-life care for prisoners falls under the responsibility of the Ministry for Health.
French legislation allows for adjustments to the conditions of imprisonment (adjournment of a sentence or non-custodial alternatives outside of prison) for prisoners whose health is severely deteriorated and who are in a life-threatening situation, or for prisoners whose health status is permanently incompatible with imprisonment. Adjustments to the conditions of imprisonment for medical reasons, consisting of non-custodial alternatives outside of prison, may include, for example, monitoring with an electronic monitoring, placement under the authority of authorized associations, or parole with supervision. These alternative conditions do not change the length of the sentence handed down. Adjournment of a sentence on medical grounds allows for prisoners to be released indefinitely, but if their health status recovers sufficiently, they will return to prison to finish serving their sentence.
Yet, more than a hundred people die in French prisons from natural causes every year,, and the impact of the legislation has been called into question., Therefore, we aimed to assess the number and characteristics of prisoners requiring end-of-life care in French prisons. These data could help (re)organize the care system appropriately according to the actual needs of prisoners.
Materials and methods
The PARME study is a mixed-methods study combining quantitative and qualitative approaches. The methods and results of the qualitative study are described in a separate work. The study received official authorization from the Ministry for Justice, the Ministry for Health, and the prison service administration, which facilitated the adherence of health professionals, the access for the researchers to the prisons, and the completeness of the data collection.
Study design
We used a quantitative approach comprising a prospective national survey conducted over a 3-month period in each correctional administrative area.
Setting/participants
Information was collected from the care system point of view. Participants were physicians from all dedicated establishments delivering healthcare to prisoners throughout France, namely eight interregional hospital secured units (UHSI), four specialized mentally ill hospital unit (UHSA), and the National Health Rehabilitation Department of Fresnes (EPNSF) (collectively termed hospital units), as well as in their detention facilities through the 177 consultations and ambulatory care units (UCSA), recently officially renamed “health units.”
Population and sampling
Prisoners requiring end-of-life care were defined as all patients with serious, chronic, or progressive illness, at an advanced or terminal phase, with a life expectancy of <1 year and treated in dedicated healthcare facilities for prisoners during the study period.
Data collection
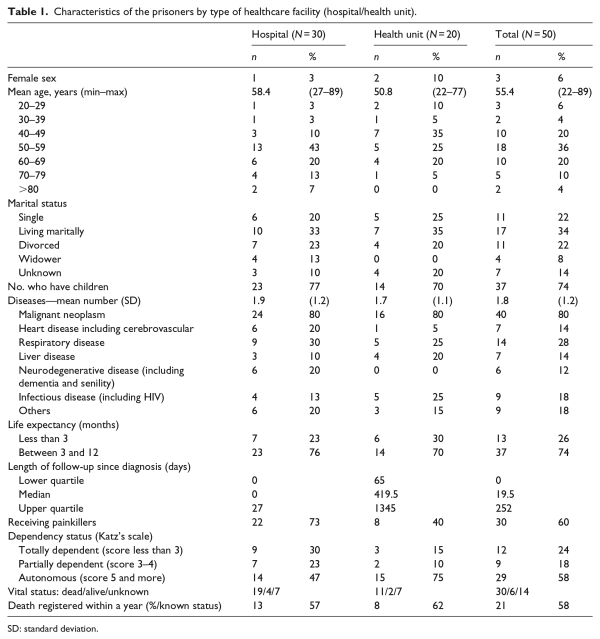
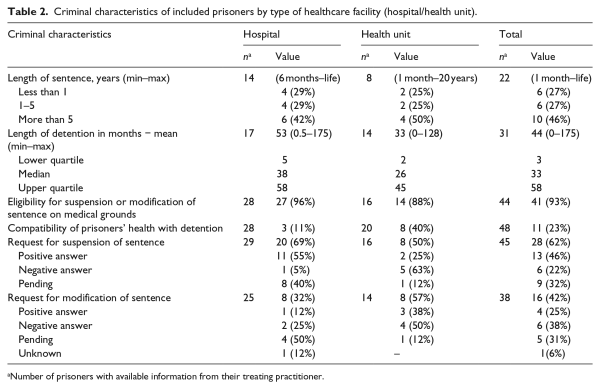
Data collection was carried out in three periods of 3 months from 2011 to 2013 according to the agreements from Ministries (Figure 1). An inclusion list was prepared by the physician from each site to identify patients requiring end-of-life care and each patient was assigned an identifier. This list was kept in each medical unit to link the identification number to the relevant patient and guaranteed anonymity of the data for the researchers. Duplicates arising, for example, from transfer to another healthcare facility during the 3 months of data collection, were eliminated by checking the initials, date of birth, and original jail of each patient. Questionnaires were completed for each patient by their treating physician to obtain socio-demographic data, medical, and criminal characteristics. Medical information concerned in particular the diagnosis of life-threatening disease(s), prognosis, co-morbidity, and the reason(s) the patient required palliative care, as well as current treatment, pain treatment, the degree of autonomy assessed by Katz’s scale adapted to prison (Figure 2), the prisoner’s status (awaiting sentence, already sentenced) and the length of detention, the end date of sentence, and the existence of any requests for suspension or reduction in the sentence for medical reasons.
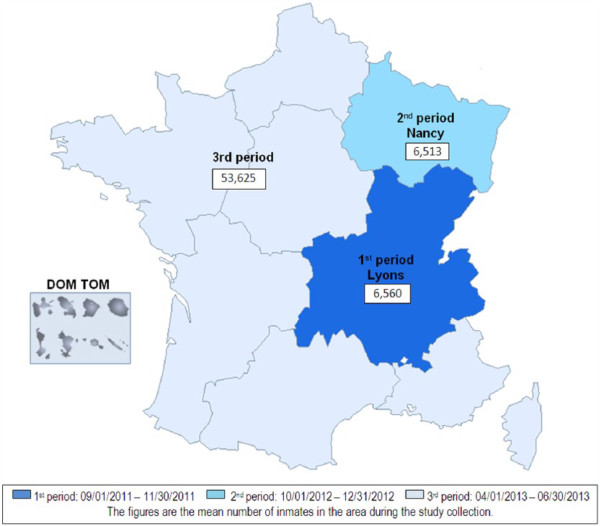
Figure 1
Geographical distribution of prisoners included in the study by study period.
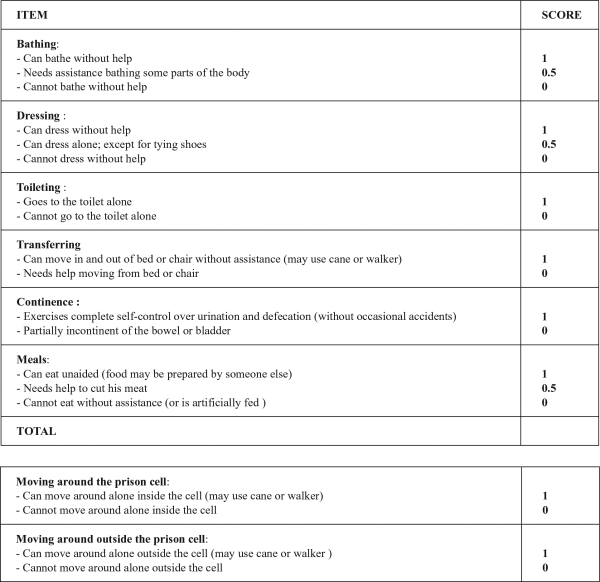
Figure 2
Katz’s scale with two supplementary questions adapted to the correctional context.
Data on the total number of prisoners during the study period were obtained from the national prison service (Figure 1).
Statistical analysis
Clinical and socio-demographic variables collected by investigators are described as mean ± standard deviation (SD) for normally distributed continuous variables, or median (interquartile, range) for non-normally distributed variables and number (percentage) for qualitative variables. Since the information came from medical practitioners, the number of data available and the value for each criminal-related characteristic are reported.
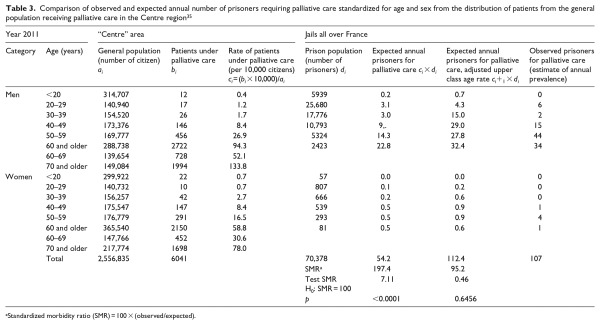
The quarterly incidence rate was the number of new cases registered by the average prison population during the study period. The annual estimated prevalence was calculated using the mean number of prisoners in the year 2011 (n = 70,378) as the denominator and the sum of prevalent cases plus four times the quarterly value of incident cases as the numerator (confidence interval (CI) using a 90% binomial law). The estimated number of prisoners requiring palliative care was standardized by the indirect method from the distribution by age and sex of patients receiving palliative care in the “Centre” region of France which is the most accurate existing data for the study period. An adjusted analysis was also performed using rates for people 10 years older in the free community. All analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
The mean prison population was 66,698 during the study period. In total, 60 palliative care situations were declared by physicians. Among these, 10 cases were excluded: 2 patients refused to consent for their data to be collected, 2 questionnaires were not completed, and 6 situations were excluded because their life expectancy was greater than a year. The characteristics of the 50 prisoners (31 prevalent cases and 19 incident cases) included in the analysis are shown in Tables 1 and 2. The prisoners included in the study were mostly men (47 versus 3 women); however, overall the proportion of women in our sample is quite similar to that of the total prison population, at around 4%. The average age was higher for patients reported in hospitals (UHSI) and logically older than the overall jail population (where the mean age is 34.3 years). The mean length of detention was four times that of the mean of overall prison population (9.9 months), and sentence duration is longer than in the overall prison population (less than 1 year for 36%, 1–5 years for 41%, and up to 5 years for 23%). The prisoners included had a family (current life couple in a third of cases, children for three of four patients). However, the existence of a family did not necessarily mean that those families were present, and the participating physicians were in contact with only half of the families of hospitalized prisoners.
The quarterly incidence rate was 2.8 for 10,000 prisoners (CI: 1.7–4.4 per 10,000 prisoners). The estimated annual prevalence rate of sick prisoners requiring palliative care was 15.2 per 10,000 prisoners (CI: 12.5–18.3 per 10,000 prisoners).
The observed number of sick prisoners requiring palliative care was twice as high as the expected number standardized for age and sex based on the general population, but similar to the number that would be expected among persons 10 years older in the free community (Table 3).
Overall, 33 patients submitted a request for release, and half of these (16/33) received a positive answer. There was a discrepancy between the number of actual requests and the number of patients who met the criteria for release on medical grounds (82% of the 50). Thus, 12 patients could have taken advantage of this measure but did not make any such request. According to physicians, the reasons why no requests were submitted were as follows: no desire to submit a request, subject not addressed, death before request, request for alternative conditions for detention, healthcare adapted to health problem, and one prisoner who thought he did not meet the criteria. According to the treating physicians, 11 persons (3 in UHSI and 8 in UCSA) had a health status that was compatible with detention despite having a life expectancy of <1 year. The reasons given to justify the compatibility of the patient’s health with continued prison detention were mainly the autonomy of the patient, a good health status, and less frequently the fact that the prisoner’s living conditions within the prison were adapted to their state of health. Only 6 of 13 patients with life expectancy <3 months submitted a request for release, and two were refused.
Discussion
The PARME study is the first national study to focus on prisoners requiring end-of-life care in France. The participation rate was very high in this study, since the two researchers (A.C. and A.G.-M.) had official authorizations from the national penitentiary service and from the Ministry for Health to enter all study sites for the purposes of the study. They also followed up with participating physicians regularly by phone contact during the study period to ensure timely notification of all cases and encourage exhaustive data recording. Due to the greater vulnerability of the prison population, –, there was, as expected, a high number of ill prisoners requiring palliative care, namely around twice the expected rate in the general French population standardized for age and sex. Worldwide, studies have been mainly performed in the United States, United Kingdom, and Australia and they focused on specific diseases,, – and therefore, figures are scarce to estimate the size of this specific population. Nevertheless, in these countries, palliative care units were often put in place in prison, albeit with different initiatives developed both inside and outside prisons. Thus, estimations could be made using the analysis of the prisoners’ death rates from natural causes. Noonan and Ginder analyzed prisoners’ death statistics from local and state jails all over the United States and estimated the current prisoners’ death rate at around 2 per 1000 for all causes and 1.5 per 1000 for natural causes., Cancer and heart disease accounted for more than half (56%) of all prison deaths in 2011 in the United States. Although the prison population was five times lower than in the United States, the figures are similar for England and Wales, with 60% of deaths from natural causes. The charitable organization Inquest published annual statistics regarding deaths in prison for England and Wales (http://www.inquest.org.uk/statistics/deaths-in-prison, accessed 30 December 2013) and reported a stable mortality rate in prison, at around 2.1 per 1000 for all causes and 1.3 per 1000 for natural causes over the past 5 years. The average age at death in English and Welsh jails was 52 years for men and 44 years for women. The median mortality rate in Europe was 26 deaths per 10,000 prisoners in 2011 and increased to 28 in 2012. The latest figures for France come from the Council of Europe working from data provided by the prison administration. They recorded 166 deaths in custody in France in 2012 (mortality rate of 2.5/1000 for all deaths) and 30.7% (n = 51) from natural causes including illness. Accordingly, the mortality rate of 0.77 per 1000 for natural deaths in France is half that reported for the United States and United Kingdom. These figures are compatible with our results and the 13 natural deaths recorded during the 3-month period of our study. The adjusted analysis confirmed the common assertion of a 10-year lag in the physiological age of prisoners compared to chronological age.,, Despite the willingness to push dying prisoners outside the prison environment, our study showed that the need for adequate end-of-life care for dying prisoners has emerged as a critical issue for French correctional healthcare.
Our study had some limits. First, the term “palliative care” covered a range of disparate meanings during the study period,, and therefore, our inclusion criteria were restricted to the central idea of “life-threatening illness with life expectancy of less than a year,” although this timeframe can be difficult to predict. Second, prisoners requiring palliative care could be identified by the court who received the requests of suspension of the sentence due to impaired health status, by the prison administration, or by the public hospital department in charge of the prisoner’s care. The medical point of view was chosen for accuracy, relevance, and completeness. In turn, missing data were high for the criminal characteristics of patients without systematic access to these types of data. Third, our study was performed over three different periods of time, according to the progressive granting of agreement from various Ministries. The Lyon UHSA (Vinatier) was the first in France and the only one open at the beginning of our study. For this reason, the French prison administration gave us the authorization to start a feasibility study in the Lyon area, which was then extended to Nancy and the surrounding area in a second prospective, confirmatory feasibility phase. Finally, the national survey was a prospective study with an inclusion period of 3 months, launched simultaneously throughout the whole country, excluding the regions of Nancy and Lyon where data collection had previously been performed during the feasibility phase. The collection of both these regions was considered by the Scientific Council as a relevant and valid measure in terms of criteria for inclusion and exclusion and investigative methods used, enabling extension of the investigation to a larger area without the need to re-collect data. Finally, no exact statistics on the number of people who actually benefit from palliative care in a given year are available for France, so we used the most accurate and relevant data to our study period, which was based on hospital and home care in the “Centre” region of France. The age and sex structure of the population of this region is similar to that of the overall French population, albeit slightly older.
Our findings are surprising given that in France, the legislator has ruled that prison is not the place for a natural end of life. The study physicians considered that 93% of the ill prisoners identified were eligible for a suspended sentence or parole, and more than three quarters of the situations identified in this study were inconsistent with continued detention. It is therefore surprising that only two-thirds of ill prisoners submitted a request for compassionate release and that only half of these requests were granted.
Multiple hypotheses could explain these findings. It is possible that some prisoners were not aware of their own health status or of the possibility of requesting release. Some may have preferred to stay in prison regardless, either because they felt confident there or because they were close to the end of their sentence. In some cases, a minimum sentence precludes any reconsideration of the sentence. The idea that the suspension implies a return to custody if the health status improves coupled with the fact that the time spent on release for medical grounds is not deducted from the total sentence may have worried sick prisoners, who feel that it only added to the length of their sentence. The prosecutor could oppose release mostly due to the risk of reoffending. Life expectancy can be difficult to predict., Jail could also represent the social environment of reference for some people, and they prefer to stay inside instead of requesting release, especially when they have served a long sentence and have aged in jail (half of our sample were sentenced to more than 5 years and had already spent more than 3 years in jail) with few or no relatives outside. Finally, the conditions for obtaining an adjournment or suspension of a sentence as stipulated in Article 720-1-1 of the Code of Criminal Procedure vary widely in real-life application. The concept of “health incompatible with detention” could be distorted by the court or the judge in favor of the concept that “adequate care is being provided in detention.” In this situation, the presence of a dedicated hospital or the ability to adjust the conditions of life in prison sometimes lead medical experts to believe that the patient’s state of health is compatible with detention because they are receiving sufficient care. This finding goes against the precept that the conditions of detention are not usual housing conditions and involve constraints that would not exist outside the prison (unsuitable bedding, non-specific diet, lack of privacy, hygiene subject to the shower schedules, etc.). It also skews the primary mission of UHSI, which were not intended to be places for extended stays. These hypotheses and considerations on prisoners’ situations and trajectories are carefully examined in a separate analysis of the qualitative data from this study.
Overall, France has been reluctant to promote palliative care units in the prison sector, probably because terminally ill prisoners are supposed to be released, given that the law provides for this option. Prison palliative and hospice care units have been created in the United States and the United Kingdom, and many promising practices have already been proposed, such as the use of peer volunteers, multi-disciplinary teams, special health units inside the prison, staff training, and partnerships with community hospices.,, Nevertheless, figures are not easily available to plan for resources. Our study contributes to providing important data regarding end-of-life care in prisons in France and could serve as an example for other countries, although the methodology would need to be adapted to the context and legislation in other countries.
Conclusion
Although the law allows for compassionate release, there are more ill prisoners requiring end-of-life care in jail than expected. Some should remain in prison regardless, particularly those whose only social ties are in prison, or those with a high risk of criminal reoffending. Knowledge of the profile of prisoners (medical, social, and jurisdictional) and the estimated prevalence of ill prisoners requiring palliative care could help define healthcare needs for dying prisoners in agreement with humanitarian values and the Right to Health and Medical Care promulgated by the European Commission of Human Rights and the United Nations Bill of Human Rights.
The PARME study group consists of the following: Yvain Auger (MD, UHSI Pitié Salpêtrière Paris), Christophe Bartolli (MD, UHSI Marseille), Paule Bayle (MD, UHSI Toulouse), Régis Bedry (MD, UHSI Bordeaux), Benoit Bernard (MD, UHSI de Rennes), Jean-René Binet (professor in civil law, University of Rennes), Emmanuelle Blanchet (MD, UHSI Nancy), Philippe Chossegros (MD, UHSI Lyons), Sebastien Grignard (MD, UCSA Besançon), Frédéric Grimopont (MD, UHSI Lille), Caroline Guibet Lafaye (PhD in philosophy, CNRS Paris), Christian Guinchard (lecturer in sociology, Besançon), Paul Mbanzoulou (PhD in law, ENAP Agen), and Emmanuel Picavet (professor of applied ethics, Université Paris 1 Panthéon-Sorbonne). L.P. and R.A. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. The authors thank especially Chrystelle Vidal, Elisabeth Monnet, and Maxime Desmarets for their help on epidemiological analysis and Franck Leroux for data management. They would like to thank Pierre Yves Chaumontet (MD, UHSI Lyons) for his contribution to the work. The authors thank all the people involved in the study from the Ministry of Health, the Ministry of Justice, and from all participating centers. Finally, they would like to thank Fiona Ecarnot for translation.
Declaration of conflicting interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding This study received national grants from the “Fondation de France” no. 00014944 in 2010 and no. 00032581 in 2012.
Legal and ethical issues This study received official approval from the Ministry for Justice and the Ministry for Health and from the prison service administration for a feasibility phase in 2011, and then for an extended study phase in 2012–2013, which improved the adherence of health professionals, facilitated access to the prisons for the researchers, and contributed to the completeness of the data collection. The study was approved by the French National Health Products Safety Agency (ANSM) on 05/08/2011 under number 2011-A00791-40 and by the Ethics Committee Est II on 08/10/2011 under number CPP 11/613. The protocol was registered on clinicaltrials.gov under number NCT02362295.
References
- 1. Linder JF, Meyers FJ. Palliative care for prison inmates: “don’t let me die in prison.” JAMA 2007; 298(8): 894–901.
- 2. Reimeringer C, Gautier S. Dix ans de loi Kouchner: funeste anniversaire de la suspension de peine médicale. Dedans: Dehors 2012; 76: 10–14.
- 3. Bedard R. When dying alone in prison is too harsh a sentence. The New York Times, 2015, p. A19.
- 4.
- 5. The Lancet. Compassionate release in the USA. Lancet 2013; 381: 1598.
- 6.
- 7.
- 8. Mouquet MC. La santé des personnes entrées en prison en 2003. Etudes etrésultats no. 386, 2005. Drees: Ministère des solidarités, de la santé et de la famille.
- 9. Dubler NN. The collision of confinement and care: end-of-life care in prisons and jails. J Law Med Ethics 1998; 26: 149–156.
- 10. Semaille C, Le Strat Y, Chiron E, et al.; Prevacar Group. Prevalence of human immunodeficiency virus and hepatitis C virus among French prison inmates in 2010: a challenge for public health policy. Euro Surveill 2013; 18(28): 20524.
- 11. Fazel S, Hope T, O’Donnell I, et al. Health of elderly male prisoners: worse than the general population, worse than younger prisoners. Age Ageing 2001; 30(5): 403–407.
- 12. Mathew P, Elting L, Cooksley C, et al. Cancer in an incarcerated population. Cancer 2005; 104(10): 2197–2204.
- 13. Binswanger IA, Krueger PM, Steiner JF. Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. J Epidemiol Community Health 2009; 63(11): 912–919.
- 14. Bautista-Arredondo S, González A, Servan-Mori E, et al. A cross-sectional study of prisoners in Mexico City comparing prevalence of transmissible infections and chronic diseases with that in the general population. PLoS ONE 2015; 10(7): e0131718.
- 15. Wilper AP, Woolhandler S, Boyd JW, et al. The health and health care of US prisoners: results of a nationwide survey. Am J Public Health 2009; 99(4): 666–672.
- 16. Observatoire International des Prisons (OIP). Rapport sur les conditions de détention en France. Paris: La Découverte, 2011, 336 pp.
- 17. Payne S, Turner M, Kidd H, et al. An evaluation of current end of life care provision in prisons in Lancashire and Cumbria. Lancaster: International Observatory on End of Life Care, Division of Health Research, Lancaster University, 2009.
- 18. Knox C. Challenges providing end-of-life care in prisons and jails. Text online, 2013, http://essentialsofcorrectionalnursing.com/2013/08/27/challenges-providing-end-of-life-care-in-prisons-and-jails/ (2013, accessed 12 December 2015).
- 19. Maschi T, Marmo S, Han J. Palliative and end-of-life care in prisons: a content analysis of the literature. Int J Prison Health 2014; 10(3): 172–197.
- 20. Cohn F. The ethics of end-of-life care for prison inmates. J Law Med Ethics 1999; 27(3): 252–259.
- 21. Phillips LL, Allen RS, Harris GM, et al. Aging prisoners’ treatment selection: does prospect theory enhance understanding of end-of-life medical decisions? Gerontologist 2011; 51(5): 663–674.
- 22. Turner M, Payne S, Barbarachild Z, et al. Care or custody? An evaluation of palliative care in prisons in North West England. Palliat Med 2011; 25(4): 370–377.
- 23. Cloyes KG, Berry PH, Martz K, et al. Characteristics of prison hospice patients: medical history, hospice care, and end-of-life symptom prevalence. J Correct Health Care 2015; 21(3): 298–308.
- 24. Hoffman HC, Dickinson GE. Characteristics of prison hospice programs in the United States. Am J Hosp Palliat Care 2011; 28(4): 245–252.
- 25. Stone K, Papadopoulos I, Kelly D. Establishing hospice care for prison populations: an integrative review assessing the UK and USA perspective. Palliat Med 2012; 26(8): 969–978.
- 26. Cloyes KG, Rosenkranz S, Wold D, et al. To be truly alive: motivation among prison inmate hospice volunteers and the transformative process of end-of-life peer care service. Am J Hosp Palliat Care 2014; 31(7): 735–748.
- 27.
- 28.
- 29.
- 30. Aebi MF, Delgrande N. SPACE I—Council of Europe annual penal statistics: prison populations (Survey 2013). Strasbourg: Council of Europe, 2015.
- 31. Lagarrigue A, Mongiati M, Bayle P, et al. Deprivation of liberty and end of life: does die with dignity mean to die free? Med Palliat 2014; 13: 200–206.
- 32. Chassagne A, Godard A, Cretin E, et al. The collision of inmate and patient: end-of-life issues in French prisons. J Correct Health Care 2017; 23(1): 66–75.
- 33.
- 34. Kue Young T. Population health: concepts and methods. 2nd ed. New York: Oxford University Press, 2005.
- 35.
- 36.
- 37. Noonan M, Ginder S. Mortality in local jails and state prisons, 2000-2011—statistical tables. Washington, DC: Bureau of Justice Statistics ( 2013 issue from Bureau of Justice Statistics, Deaths in Custody Reporting Program, 2001–2011 and National Prisoner Statistics, 2001–2011).
- 38. Binswanger IA, Stern MF, Deyo RA, et al. Release from prison—a high risk of death for former inmates. N Engl J Med 2007; 356(2): 157–165 (Erratum in: N Engl J Med 2007; 356(5): 536).
- 39. Walmsley R. World prison population list. 10th ed. International Centre for Prison Studies, 2013.
- 40. Morton JB. An administrative overview of the older inmate. Washington, DC: US Department of Justice, National Institute of Corrections, 1992.
- 41. Falter RG. Selected predictors of health services needs of inmates over age 50. J Correct Health Care 1999; 6(2): 149–175.
- 42. Van Mechelen W, Aertgeerts B, De Ceulaer K, et al. Defining the palliative care patient: a systematic review. Palliat Med 2013; 27(3): 197–208.
- 43. Sigurdardottir KR, Oldervoll L, Hjermstad MJ, et al. How are palliative care cancer populations characterized in randomized controlled trials? A literature review. J Pain Symptom Manage 2014; 47(5): 906.e17–14.e17.
- 44.
- 45. Gwilliam B, Keeley V, Todd C, et al. Development of Prognosis in Palliative care Study (PiPS) predictor models to improve prognostication in advanced cancer: prospective cohort study. BMJ 2011; 343: 1–15.
- 46. Gibbins J, Bloor S, Reid C, et al. The use of a modified “surprise” question to identify and recruit dying patients into a research project in an acute hospital setting. BMJ Support Palliat Care 2012; 2: A8.
- 47. Ratcliff M, Craig E. The GRACE Project: guiding end-of-life care in corrections 1998-2001. J Palliat Med 2004; 7(2): 373–379.
- 48. Fletcher A, Payne S, Waterman D, et al. Palliative and end of life care in prisons in England and Wales—approaches taken to improve inequalities. BMJ Support Palliat Care 2014; 4: A19.