The prevalence of obesity doubled since the 1980s, resulting in exponentially higher incidence rates of diet-related diseases [, ]. These drastic changes cannot be attributed to rapid increases in the genetic predisposition for obesity only nor sudden reductions in individuals’ personal responsibility in making food decisions [, ]. Decreases in physical activity, due to industrialization onset in the 1910s, predated the uptick in obesity rates []. Converging evidence convincingly demonstrates that the timeline of rising obesity rates has mirrored increases in the availability of calorie-dense, nutrient-poor ultra-processed foods (UPFs) in the environment, thus implicating UPFs as a primary causal driver of the obesity pandemic [].
The term “UPF” originated from the NOVA Food Classification System [], which is the most prominent approach used across disciplines in the scientific literature for categorizing foods based on their level of processing [, ]. Industrial processing is common in our modern food supply and involves techniques that can be beneficial (e.g., canning vegetables to increase shelf life) or harmful (e.g., creating cheap, nutrient-poor ingredients like corn syrup and refined oils) for public health []. Thus, the NOVA system was created to differentiate between forms of food processing and underscore the uniquely problematic natures of UPFs [, ]. While numerous terms have been used to describe rewarding foods [, ] and adoption of a uniform term remains controversial [-], we use the UPF term to align with the widely used NOVA system.
NOVA categorizes UPFs as group 4 foods, reflecting the highest degree of processing and greatest deviation from naturally occurring foods []. UPFs have few, if any, whole food ingredients []. Instead, UPFs have been industrially formulated to maximize palatability (and therefore profitability) by combining artificially elevated amounts of rewarding ingredients like hydrogenated oils, refined carbohydrates (e.g., white flour, added sugars), sodium, and other additives (e.g., flavor enhancers) [, ]. Categories of UPFs include packaged snacks (e.g., potato chips, cookies), candy, frozen desserts, packaged white flour bread/pasta, sugary breakfast cereals/bars, fast foods (e.g., pizza, French fries), and beverages with added sugars (e.g., soda, sweet tea, sports drinks) (for a comprehensive description and list, see []). While homemade versions of some of the aforementioned foods have been enjoyed for generations (e.g., cookies, breads), research has demonstrated that the recent uptick in the availability of industry-created UPFs poses the greatest public health risk, as UPFs are conveniently accessible, affordable, heavily marketed, and dominate the food supply [-].
Notably, emerging evidence suggests that UPFs are so highly reinforcing that they may trigger addictive biological and behavioral responses, thus directly driving forward excessive patterns of food intake and contributing to obesity []. While the changing food environment has been considered extensively in the context of obesity [], less attention has been paid to how potentially addictive UPFs may also contribute to disordered eating, particularly binge-type eating disorders. Thus, the overarching aim of this editorial is to evaluate how food addiction (FA), a clinical presentation consistent with a substance-based addiction to UPFs, encompasses unique theoretical, phenotypic, and treatment perspectives relative to obesity and existing eating disorders. Specifically, we review (1) how the changing food environment contributes to problematic eating behavior, (2) the operationalization of FA, (3) the association between FA and obesity, (4) the association between FA and eating disorders, and (5) the diagnostic and public health implications of FA.
The Changing Food Environment and Eating Behavior
The rise in UPFs in the modern food environment began in the 1980s [], which coincides with when major tobacco corporations acquired large food companies (e.g., Kraft, General Foods) and became the biggest producers of UPFs [, ]. Tobacco industry documents reveal that tactics used to formulate cigarettes to be as addictive as possible have been applied to create reinforcing UPFs with optimal combinations of rewarding ingredients (e.g., fat, sugar) to maximize palatability and profitability [-]. The food industry has been extremely successful in profiting from UPFs, which now account for over 60% of all calories consumed in the USA []. Emerging empirical evidence supports the direct role that UPFs play in motivating overeating behavior. For instance, an inpatient-feeding trial demonstrated that eating a diet of UPFs, compared to a macronutrient-matched diet of minimally processed whole foods, led individuals to consume 500 more calories per day [].
Research has not only linked UPFs to obesity and all-cause mortality [, ], but UPFs are also the predominant food type consumed during binge episodes [, , -]. A review of food diaries of individuals with eating disorders found that 100% of the foods consumed in binge episodes were UPFs []. While anorexia nervosa (AN) (i.e., restrictive eating leading to dangerously low body weight) was included in the first Diagnostic and Statistical Manual of Mental Disorders (DSM) in the 1950s [], the clinical emergence of binge-type eating disorders occurred between 1980 and 2013 []. Thus, when UPFs began to increasingly dominate the food environment, clinical and academic recognition of binge-type eating disorders increased substantially. This suggests that greater exposure to UPFs may be a key factor in the emergence of binge-type eating disorders. However, traditional approaches to conceptualizing eating disorders have focused less on whether UPFs may directly contribute to binge eating.
In contrast, the FA model emphasizes that the attributes of UPFs, the proposed addictive substance, trigger compulsive patterns of excessive intake. Individual differences are important in addiction models, as only a subset of those who use addictive substances exhibit the individual risk factors that enhance susceptibility for becoming addicted (e.g., reward dysfunction, emotion dysregulation, impulsivity) []. Although the FA concept first emerged in the scientific literature in the 1950s, there has been a marked increase in this area since the early 2000s []. At this time, animal models demonstrated that UPFs (and UPF ingredients like sugar and fat) could cause biological (e.g., dopamine down-regulation) and behavioral (e.g., use despite consequences, withdrawal) responses akin to addictive substances [-]. Neuroimaging technology demonstrated that obesity was associated with neural differences in the reward system (e.g., lower D2 receptor availability, heighten striatal activation to UPF food cues) seen in addictive disorders []. This spurred ongoing scientific investigation into whether UPFs directly motivate overeating behavior, akin to how addictive substances perpetuate problematic use, and trigger the FA phenotype in at-risk individuals [].
Operationalizing UPF Addiction
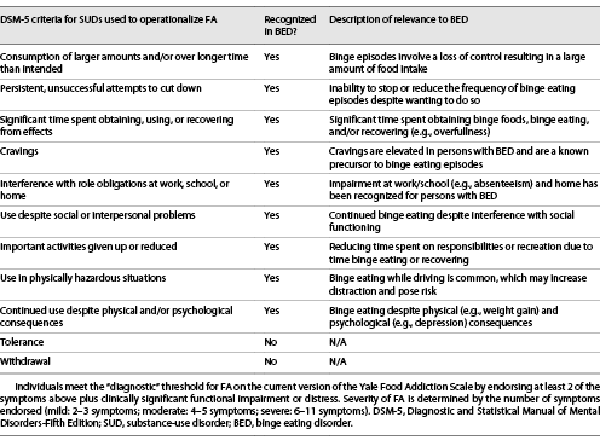
The empirical literature to date is consistent with conceptualizing FA as a substance-based addiction to UPFs []. FA is most commonly operationalized using the Yale Food Addiction Scale (YFAS), a self-report questionnaire that asks individuals the extent to which they experience problematic patterns of UPF consumption that align with the DSM diagnostic criteria for substance-use disorders (SUDs) [, ]. The current version of the YFAS aligns with the 11 DSM-Fifth Edition (DSM-5) symptoms of SUDs [, ]. Examples of YFAS symptoms include continued UPF intake despite negative physical/psychosocial consequences, persistent yet unsuccessful attempts to cut down on UPFs, withdrawal, and tolerance (see Table 1 for a list of all 11 criteria). Consistent with DSM-5 diagnostic criteria for SUDs [], individuals can meet a “diagnostic” score for FA on the current versions of the YFAS by endorsing at least two of the 11 behavioral indicators of addiction plus clinical impairment/distress [, ]. Further paralleling DSM-5 criteria, severity thresholds for this “diagnostic” score are defined by the number of symptoms endorsed (mild: 2–3 symptoms; moderate: 4–5 symptoms; severe: 6–11 symptoms) [, ]. The YFAS measures have been adapted and validated for the assessment of developmentally appropriate indicators of FA in youths [, ] and in dozens of different languages (e.g., Japanese, Spanish, Farsi) []. While not intended to be a diagnostic tool, the YFAS measures have demonstrated excellent clinimetric properties, evidenced by incremental associations between FA symptoms and diagnostic score severity with clinically significant outcomes, including poorer quality of life, more severe psychopathology, and worse treatment outcomes [-]. The YFAS measures also exhibit strong clinimetric sensitivity, given their ability to differentiate between individuals with compulsive patterns of UPF intake versus healthy controls and to detect changes in response to interventions (e.g., decreases in FA following behavioral weight loss treatment and bariatric surgery) [].
Using the YFAS “diagnostic” score, recent meta-analyses have estimated the prevalence of FA in general population samples to be 12–15% for children and adolescents and 14–20% for adults [, ]. The prevalence of FA is thus similar to rates of SUDs with legal addictive substances (alcohol-use disorder: 19.2%; tobacco-use disorder: 18.2%) [, ]. Biological and behavioral evidence has convincingly highlighted parallels in the mechanisms implicated in both FA and SUDs, such as reward dysfunction, emotion dysregulation, impulsivity, elevated cravings, and psychological comorbidities (e.g., depression, anxiety, childhood trauma) [-]. FA is more likely to occur in individuals with a family history of addiction and has a high co-occurrence rate with other SUDs [], which supports its conceptualization as an addictive disorder.
The Association between FA and Obesity
Early support for the plausibility of FA in humans resulted from neuroimaging studies showing overlapping responses in reward-related neural regions among individuals with a SUD for relevant drug cues and persons with obesity for UPF cues [, ]. Yet, obesity is a heterogenous condition that may be caused by a caloric imbalance or an array of other factors (e.g., medication side effects) [, ] and is thus an imprecise and insufficient proxy for FA. As such, operationalizing FA using behavioral criteria that align with DSM-5 diagnostic indicators of SUDs is a more theoretically informed approach for evaluating the relevance of FA within obesity.
Notably, only a subset (19–28%) of individuals with obesity meet for FA on the YFAS measures [, ], suggesting that FA may represent a subtype of obesity characterized by greater susceptibility to the reinforcing natures of UPFs. In support, in studies of obesity, persons with versus without FA report elevated intake of UPFs and increased tendencies related to enhanced addiction vulnerability (e.g., impulsivity, emotion dysregulation) []. Addictive-like UPF consumption may at least partially explain observations that individuals with obesity and FA, compared to those with only obesity, endorse more frequent and severe maladaptive eating behaviors (e.g., emotional eating, uncontrolled eating) and an array of comorbidities, including poorer cardiometabolic indicators (e.g., higher visceral fat, poorer glycemic control), an increased prevalence and severity of comorbid physical (e.g., hypercholesterolemia, neuropathy) and psychological (e.g., depression, trauma) disorders, and higher psychological distress [, -].
It is important to note that FA is prevalent across weight classes (e.g., 12–17% of youths and adults with normal weight) and exhibits similar associations, regardless of BMI, with addiction risk factors (e.g., impulsivity), poorer quality of life, compulsive eating behaviors, and increased physical and psychological comorbidities [, -]. For all adults, FA may also increase the risk of weight gain over time [-]. Strikingly, adults in the USA with versus without FA reported gaining, on average, nearly six times more weight during the first year of COVID-19 (12.42 vs. 2.14 pounds, respectively), and FA predicted weight gain above and beyond BMI []. No studies have yet evaluated the associations between FA and weight gain in youths, but findings in adults suggest the need for future research.
Implications of FA for the Treatment of Obesity
FA has been strongly related to clinical outcomes relevant to obesity like dietary adherence, treatment participation, and weight loss. Individuals with versus without FA report consuming significantly greater quantities of UPFs [, -] and are more likely to exhibit compulsive patterns of consumption with these foods [], which likely interferes with adherence to the sustained caloric restriction required for weight loss. FA has been associated with poorer outcomes in behavioral weight loss treatments for both adults and youths, including lower attendance, higher attrition, lower weight loss, and higher weight regain [, ]. Particularly strong evidence comes from a randomized clinical trial of 609 adults with overweight or obesity enrolled in a 12-month behavioral weight loss program, which found that FA was the strongest psychosocial predictor of treatment dropout and poorer weight loss []. In two studies of adults who had bariatric surgery, FA was associated with less weight loss and greater weight regain (mean follow-up durations were 7.7 and 13.7 years) [, ]. However, some studies, particularly those with smaller sample sizes and/or briefer durations, have not found an association between FA and weight loss (e.g., []).
While existing data indicate the potential need to screen for FA at the onset of weight control interventions, it is important to acknowledge that there are no existing evidence-based treatments for FA. Many gold-standard behavioral weight loss treatments focus primarily on calorie intake and the approach of consuming all foods in moderation. From an addiction standpoint, intermittent substance use can enhance reinforcement and trigger problematic patterns of subsequent use []. A crucial next step is to adapt and evaluate whether empirically supported treatments for reducing the use of addictive substances (e.g., alcohol) may be similarly efficacious for reducing UPF intake among persons with FA. Behavioral and pharmacological treatments for FA informed by the addiction literature would ideally target the roles of mechanisms that perpetuate UPF reinforcement and addictive-like eating behavior, such as heightened UPF reward, UPF cravings, and impulsivity, as well as core features unique to addictive disorders like withdrawal and tolerance []. These novel treatments may have the potentials to improve behavioral weight loss intervention outcomes among those with both FA and obesity.
The Association between FA and Eating Disorders
A common critique of why FA does not warrant consideration as a distinct clinical presentation stems from the elevated prevalence rates of FA observed among individuals with clinical eating disorders. A recent meta-analysis estimated the prevalence of FA among youths and adults as 44% for persons with AN, 48% in those with bulimia nervosa (BN), and 55% among individuals with binge eating disorder (BED) [], though individual studies have reported higher rates (e.g., 83.6% FA prevalence across eating disorder diagnoses []). While persons with eating disorders may be more likely to exhibit FA, this co-occurrence represents just a fraction of the estimated FA rates in the general population.
Lifetime prevalence rates of eating disorders have been estimated at 0.6% for AN, 1.0% for BN, and 2.8% for BED []. Given that 12–20% of individuals in general population samples endorse FA [, ], FA appears to capture a clinical phenotype that extends far beyond existing eating disorder diagnoses, with a similar scope as rates of alcohol- (19.2%) and tobacco-use disorders (18.2%) [, ]. In the absence of eating disorders, individuals with FA report clinically significant impairment and distress and elevated depressive symptoms, impulsivity, and negative affect [, ]. Thus, it is necessary to maintain the perspective that individuals with FA and a clinical eating disorder represent a small proportion of those who exhibit FA in the general population. Nevertheless, a growing body of evidence suggests that FA has clinical relevance in the context of existing eating disorders.
FA and AN
The overlap between AN and FA is thought to be driven by subjective, rather than objective, experiences of loss-of-control eating []. Greater endorsement of FA symptoms among individuals with AN has been associated with increased fears of overeating or experiencing a loss of control overeating behavior, rather than increased binge eating episodes and/or UPF intake []. While it is not implausible that addictive mechanisms may be relevant to AN [], the theoretical underpinnings of FA posit that objective experiences of compulsive UPF consumption motivate and maintain subsequent addictive-like eating behaviors. As a parallel example, a person would not be diagnosed with an alcohol-use disorder if they feared overdrinking but did not actually consume significant quantities of alcohol.
FA and Binge-Type Eating Disorders
Research has supported the clinical utility of FA in identifying a more severe phenotype of binge-type eating disorders like BN and BED. There is substantial overlap between the symptoms of binge-type eating disorders and the diagnostic criteria for addictive disorders (see Table 1) [, ]. Prior studies have yielded neurobiological and behavioral evidence of overlapping mechanisms in SUDs and BN/BED, including reward dysfunction, emotion dysregulation, and impulsivity (for a review, see []). Therefore, the many features and mechanisms shared by SUDs and BN/BED contribute to the overlapping prevalence rates of FA and BN/BED.
However, not everyone with BN/BED meets the FA criteria. Among individuals with BED or BN, those with versus without FA present with increased severity and frequency of binge eating episodes, greater intensity of food cravings, elevated symptoms of depression and anxiety, and a poorer quality of life (for a review, see []). FA has also been associated with both poorer prognosis and outcomes (e.g., less reduction in binge eating frequency) in treatments for disordered eating [-], although more research in this area is needed. Thus, FA appears to be an indicator of severe presentations of BN/BED, which may require additional interventions targeting addiction mechanisms to improve treatment outcomes.
Implications of FA for the Treatment of Binge-Type Eating Disorders
The common features between BN/BED and SUDs translate to the numerous similarities in evidence-based treatments for these disorders, such as restructuring automatic negative thoughts that promote cravings, developing alternative emotional coping strategies, and identifying emotional and situational triggers for problematic patterns of intake []. There are several key distinctions between SUDs and BN/BED that speak to the potential novelty and clinical utility of FA. Perspectives of binge-type eating disorders do not address core symptoms unique to SUDs, like withdrawal or tolerance, although evidence is growing that these mechanisms may be contributing to eating pathology []. Phenotypically, while BN/BED are diagnosed by the presence of distinct, 2-h binge eating episodes, addictive patterns of substance use can present as binge consumption (e.g., exceeding a threshold of alcoholic beverages on one occasion) or grazing (e.g., consuming alcohol throughout the day). Thus, addressing compulsive patterns of food intake that occur outside of binges is an important area of clinical focus.
Treatments for BN/BED do not consider the possibility that the reinforcing properties of UPFs may directly motivate and maintain binge eating episodes akin to an addictive substance. If the addictive potential of UPFs is contributing to binge eating, this does not mean that individuals need to completely abstain from all UPFs (which may have unintended consequences of increasing unhealthy patterns of dietary restraint for some individuals). Harm reduction approaches are empirically supported treatments for addictive disorders that recognize the addictive potential of the substance and implore strategies that help individuals engage in moderate, less harmful patterns of intake []. A similar approach could be adapted for FA that considers both the variability in the addictive profile of specific UPFs and situational factors that moderate risk. There is also emerging evidence that existing pharmacological (e.g., naltrexone and bupropion) and psychosocial interventions designed to address addictive mechanisms are beneficial in treating BN/BED [, ], but larger randomized control trials are needed. The inclusion of other intervention targets associated with disordered eating, such as challenging thin body ideals and shape/weight concerns, would not be contraindicated in addiction-focused treatments and could continue to be important aspects of treatment for individuals with BN/BED and FA. In sum, it will be important to use an individualized and flexible approach to integrate addiction tenants into interventions for disordered eating.
Implication for Diagnostic Conceptualizations and Public Health
The emerging evidence that UPFs may be addictive and that a substantial percentage of the population exhibits clinically significant FA requires us to reconsider the adequacy of our current diagnostic conceptualizations. Although the inclusion of a FA phenotype has been previously discussed surrounding the release of the DSM-5 [], it was rejected in part due to the idea that compulsive overeating was already accounted for by BED. Since that time, the science on FA has grown substantially (see [] for a review) and has elucidated the clinical utility of FA as a unique behavioral phenotype and as an indicator of more severe presentations of obesity and eating disorders. Even if we assume that FA is appropriately captured by existent eating disorders (which appears unlikely), the differences in prevalence between eating disorders (0.6–2.8%) [] and FA (12–20%) [, ] suggest that scores of adults and children who report clinical impairment/distress are undiagnosed and untreated using the current approach. While eating disorders predominantly occur in females, FA occurs at a similar rate across sexes []. Thus, males with FA may be particularly likely to be missed based on the current diagnostic conceptualizations. The inclusion of FA as a provisional SUD diagnosis in the DSM-5 and/or the ICD would expedite the scientific evaluation of the validity of FA and the development of novel treatments that adapt evidence-based addiction interventions to help those with FA reduce UPF intake.
There are also important public health lessons to be learned from the field of addiction (see [-]). Addiction epidemics often occur because a novel and potent addictive substance is created, but its addictive potential is undetected or underestimated. The environment changes in a manner that makes the addictive substance more accessible and, in the case of legal substances, heavily marketed and socially acceptable. Given that the individual risk profile for addiction (e.g., genetic profile, trauma exposure) does not quickly change on a population level, the increased prevalence rates of SUDs are primarily attributable to the addictive potency of the substance and accessibility within the surrounding environment. While the addictive substance is most problematic to those who develop a SUD, broader public health risks exist due to the potential for widespread subclinical overconsumption that results in negative health consequences []. Addictive substances (particularly legal ones) are highly profitable and the industries (or individuals) that produce and sell these addictive substances benefit.
Educational efforts and treatment advances alone have not been successful at turning back the tide of addiction epidemics. Instead, policy initiatives that alter the environment (e.g., increased taxation, limitations on product availability) and/or reformulation of the product (e.g., removing menthol from cigarettes, developing non-opioid pain medication) have been necessary to reduce the morbidity and mortality associated with addiction epidemics [-]. Of key importance have been efforts to protect children and adolescents (e.g., restricting marketing to youths, age limits on purchase of addictive substances), as prevention is more effective than treatment in reducing harms associated with addictive substances []. The ability to institute these effective changes requires addressing opposition from industries that are rich and politically powerful. However, change is possible. The epidemics and public health responses associated with industrial tobacco products and opioid prescription medications are recent examples of meaningful public health wins that reduce the negative impact of addictive substances and save millions of lives [-].
Conclusion
We propose that the rapid dominance of UPFs in our food supply beginning in the 1980s has resulted in another addiction epidemic, wherein FA and subclinical patterns of UPF overconsumption have contributed to increases in binge-type eating disorders, obesity, and diet-related diseases in the past 40 years. Notably, the clinical correlates of FA both within the contexts of obesity and binge-typical eating disorders and as a distinct presentation underscore the need to develop and evaluate evidence-based treatments for FA. Lastly, the lessons learned from past addiction epidemics are relevant for the negative public health consequences of FA and UPFs, particularly the need for policies that reduce the accessibility of UPFs in the modern food environment, reformulate UPFs to reduce their addictive potentials, and minimize risks for children and adolescents to develop FA.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
No funding was received.
Author Contributions
Erica M. LaFata and Ashley N. Gearhardt were each involved in developing, drafting, and finalizing the manuscript.
References
- 1. Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, et alGlobal Burden of Disease Study 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017 Jul;377(1):13–27. https://doi.org/10.1056/nejmoa1614362.of Disease Study 2015.
- 2. Costa MF, Peixoto SW. Non-communicable disease risk factor collaboration. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016 Apr;387(10027):1513–30.
- 3. Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011 Aug;378(9793):804–14. https://doi.org/10.1016/s0140-6736(11)60813-1.
- 4. Grannell A, Fallon F, Al-Najim W, le Roux C. Obesity and responsibility: is it time to rethink agency?Obes Rev. 2021 Aug;22(8):e13270. https://doi.org/10.1111/obr.13270.
- 5. Monteiro CA, Cannon G, Levy RB, Moubarac JC, Louzada ML, Rauber F, et al. Ultra-processed foods: what they are and how to identify them. Public Health Nutr. 2019 Feb;22(5):936–41. https://doi.org/10.1017/s1368980018003762.
- 6. Lawrence MA, Baker PI. Ultra-processed food and adverse health outcomes. BMJ. 2019 May;365:l2289. https://doi.org/10.1136/bmj.l2289.
- 7. Pagliai G, Dinu M, Madarena MP, Bonaccio M, Iacoviello L, Sofi F. Consumption of ultra-processed foods and health status: a systematic review and meta-analysis. Br J Nutr. 2021 Feb;125(3):308–18. https://doi.org/10.1017/s0007114520002688.
- 8. Gibney MJ, Forde CG, Mullally D, Gibney ER. Ultra-processed foods in human health: a critical appraisal. Am J Clin Nutr. 2017 Sep;106(3):717–24. https://doi.org/10.3945/ajcn.117.160440.
- 9. Monteiro CA, Cannon G, Moubarac JC, Levy RB, Louzada ML, Jaime PC. The UN decade of nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018 Jan;21(1):5–17. https://doi.org/10.1017/s1368980017000234.
- 10. Fazzino TL, Rohde K, Sullivan DK. Hyper-palatable foods: development of a quantitative definition and application to the US food system database. Obesity. 2019 Nov;27(11):1761–8. https://doi.org/10.1002/oby.22639.
- 11. Schulte EM, Avena NM, Gearhardt AN. Which foods may be addictive? The roles of processing, fat content, and glycemic load. PLoS One. 2015 Feb;10(2):e0117959. https://doi.org/10.1371/journal.pone.0117959.
- 12. Fazzino TL, Dorling JL, Apolzan JW, Martin CK. Meal composition during an ad libitum buffet meal and longitudinal predictions of weight and percent body fat change: the role of hyper-palatable, energy dense, and ultra-processed foods. Appetite. 2021 Dec;167:105592. https://doi.org/10.1016/j.appet.2021.105592.
- 13. Gearhardt AN, Schulte EM. Is food addictive? A review of the science. Annu Rev Nutr. 2021 Oct;41(1):387–410. https://doi.org/10.1146/annurev-nutr-110420-111710.
- 14. Gibney MJ. Ultra-processed foods: definitions and policy issues. Curr Dev Nutr. 2019 Feb;3(2):nzy077. https://doi.org/10.1093/cdn/nzy077.
- 15. Moubarac JC, Parra DC, Cannon G, Monteiro CA. Food classification systems based on food processing: significance and implications for policies and actions–a systematic literature review and assessment. Curr Obes Rep. 2014 Jun;3(2):256–72. https://doi.org/10.1007/s13679-014-0092-0.
- 16. Monteiro CA, Cannon G, Lawrence M, Costa Louzada M, Pereira Machado P. Ultra-processed foods, diet quality, and health using the NOVA classification system. Rome: Food and Agriculture Organization of the United Nations; 2019. [cited 2022 Aug 16]. Available from: https://www.fao.org/3/ca5644en/ca5644en.pdf.
- 17. Hall KD. Did the food environment cause the obesity epidemic?Obesity. 2018 Jan;26(1):11–3. https://doi.org/10.1002/oby.22073.
- 18. Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. Ultra: processed products are becoming dominant in the global food system. Obes Rev. 2013 Sep;14(Suppl 2):21–8. https://doi.org/10.1111/obr.12107.
- 19. Nguyen KH, Glantz SA, Palmer CN, Schmidt LA. Transferring racial/ethnic marketing strategies from tobacco to food corporations: Philip Morris and Kraft General Foods. Am J Public Health. 2020 Feb;110(3):329–36. https://doi.org/10.2105/ajph.2019.305482.
- 20. Nguyen KH, Glantz SA, Palmer CN, Schmidt LA. Tobacco industry involvement in children’s sugary drinks market. BMJ. 2019 Mar;364:l736. https://doi.org/10.1136/bmj.l736.
- 21. Moodie R, Stuckler D, Monteiro C, Sheron N, Neal B, Thamarangsi T, et al. Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet. 2013 Feb;381(9867):670–9. https://doi.org/10.1016/s0140-6736(12)62089-3.
- 22. Moss M. Hooked: food, free will, and how the food giants exploit our addictions. New York: Penguin Random House; 2021.
- 23. Monteiro CA. Ultra-processing. There is no such thing as a healthy ultra-processed product. World Public Health Nutrition Association; 2011 [cited 2022 Aug 16]. Available from: https://wphna.org/worldnutritionjournal/index.php/wn/article/download/473/419.
- 24. Hall KD, Ayuketah A, Brychta R, Cai H, Cassimatis T, Chen KY, et al. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metab. 2019 Jul;30(1):226. https://doi.org/10.1016/j.cmet.2019.05.020.
- 25. Taneri PE, Wehrli F, Roa-Díaz ZM, Itodo OA, Salvador D, Raeisi-Dehkordi H, et al. Association between ultra-processed food intake and all-cause mortality: a systematic review and meta-analysis. Am J Epidemiol. 2022 Jul;191(7):1323–35.
- 26. Canhada SL, Luft VC, Giatti L, Duncan BB, Chor D, Fonseca MJMD, et al. Ultra-processed foods, incident overweight and obesity, and longitudinal changes in weight and waist circumference: the Brazilian longitudinal study of adult health (ELSA-Brasil). Public Health Nutr. 2020 Oct;23(6):1076–86. https://doi.org/10.1017/s1368980019002854.
- 27. Canella DS, Levy RB, Martins APB, Claro RM, Moubarac JC, Baraldi LG, et al. Ultra-processed food products and obesity in Brazilian households (2008–2009). PLoS One. 2014 Mar;9(3):e92752. https://doi.org/10.1371/journal.pone.0092752.
- 28. Mendonça Rd D, Pimenta AM, Gea A, de la Fuente-Arrillaga C, Martinez-Gonzalez MA, Lopes ACS, et al. Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra follow-up (SUN) cohort study. Am J Clin Nutr. 2016 Nov;104(5):1433–40. https://doi.org/10.3945/ajcn.116.135004.
- 29. Louzada ML, Baraldi LG, Steele EM, Martins APB, Canella DS, Moubarac JC, et al. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev Med. 2015 Dec;81:9–15. https://doi.org/10.1016/j.ypmed.2015.07.018.
- 30. Askari M, Heshmati J, Shahinfar H, Tripathi N, Daneshzad E. Ultra-processed food and the risk of overweight and obesity: a systematic review and meta-analysis of observational studies. Int J Obes. 2020 Aug;44(10):2080–91. https://doi.org/10.1038/s41366-020-00650-z.
- 31. Allison S, Timmerman GM. Anatomy of a binge: food environment and characteristics of nonpurge binge episodes. Eat Behav. 2007 Jan;8(1):31–8. https://doi.org/10.1016/j.eatbeh.2005.01.004.
- 32. Pursey KM, Collins CE, Stanwell P, Burrows TL. Foods and dietary profiles associated with “food addiction” in young adults. Addict Behav Rep. 2015 Dec;2:41–8. https://doi.org/10.1016/j.abrep.2015.05.007.
- 33. Ayton A, Ibrahim A, Dugan J, Galvin E, Wright OW. Ultra-processed foods and binge eating: a retrospective observational study. Nutrition. 2021 Apr;84:111023. https://doi.org/10.1016/j.nut.2020.111023.
- 34. Dell’Osso L, Abelli M, Carpita B, Pini S, Castellini G, Carmassi C, et al. Historical evolution of the concept of anorexia nervosa and relationships with orthorexia nervosa, autism, and obsessive--compulsive spectrum. Neuropsychiatr Dis Treat. 2016 Jul;12:1651–60. https://doi.org/10.2147/ndt.s108912.
- 35. Anthony JC, Warner LA, Kessler RC. Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: basic findings from the National Comorbidity Survey. Exp Clin Psychopharmacol. 1994 Aug;2(3):244–68. https://doi.org/10.1037/1064-1297.2.3.244.
- 36. Meule A. Focus: addiction: back by popular demand: a narrative review on the history of food addiction research. Yale J Biol Med. 2015 Sep;88(3):295–302.
- 37. Murphy CM, Stojek MK, MacKillop J. Interrelationships among impulsive personality traits, food addiction, and body mass index. Appetite. 2014 Feb;73:45–50. https://doi.org/10.1016/j.appet.2013.10.008.
- 38. Davis C, Loxton NJ, Levitan RD, Kaplan AS, Carter JC, Kennedy JL. “Food addiction” and its association with a dopaminergic multilocus genetic profile. Physiol Behav. 2013 Jun;118:63–9. https://doi.org/10.1016/j.physbeh.2013.05.014.
- 39. Schulte EM, Grilo CM, Gearhardt AN. Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clin Psychol Rev. 2016 Mar;44:125–39. https://doi.org/10.1016/j.cpr.2016.02.001.
- 40. Avena NM, Rada P, Hoebel BG. Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev. 2008 Jan;32(1):20–39. https://doi.org/10.1016/j.neubiorev.2007.04.019.
- 41. Gold MS, Avena NM. Animal models lead the way to further understanding food addiction as well as providing evidence that drugs used successfully in addictions can be successful in treating overeating. Biol Psychiatry. 2013 Oct;74(7):e11. https://doi.org/10.1016/j.biopsych.2013.04.022.
- 42. Schulte EM, Smeal JK, Gearhardt AN. Foods are differentially associated with subjective effect report questions of abuse liability. PLoS One. 2017 Aug;12(8):e0184220. https://doi.org/10.1371/journal.pone.0184220.
- 43. Schulte EM, Sonneville KR, Gearhardt AN. Subjective experiences of highly processed food consumption in individuals with food addiction. Psychol Addict Behav. 2019 Mar;33(2):144–53. https://doi.org/10.1037/adb0000441.
- 44. Volkow ND, Wang GJ, Fowler JS, Telang F. Overlapping neuronal circuits in addiction and obesity: evidence of systems pathology. Philos Trans R Soc Lond B Biol Sci. 2008 Oct;363(1507):3191–200. https://doi.org/10.1098/rstb.2008.0107.
- 45. Gearhardt AN, Corbin WR, Brownell KD. Development of the Yale Food Addiction Scale Version 2.0. Psychol Addict Behav. 2016 Feb;30(1):113–21. https://doi.org/10.1037/adb0000136.
- 46. Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale Food Addiction Scale. Appetite. 2009 Apr;52(2):430–6. https://doi.org/10.1016/j.appet.2008.12.003.
- 47. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5). 5th ed.Washington, DC: American Psychiatric Association Publishing; 2013.
- 48. Schulte EM, Gearhardt AN. Development of the modified yale food addiction scale version 2.0. Eur Eat Disord Rev. 2017 Jul;25(4):302–8. https://doi.org/10.1002/erv.2515.
- 49. Schiestl ET, Gearhardt AN. Preliminary validation of the Yale Food Addiction Scale for children 2.0: a dimensional approach to scoring. Eur Eat Disord Rev. 2018 Nov;26(6):605–17. https://doi.org/10.1002/erv.2648.
- 50. Gearhardt AN, Roberto CA, Seamans MJ, Corbin WR, Brownell KD. Preliminary validation of the yale food addiction scale for children. Eat Behav. 2013 Dec;14(4):508–12. https://doi.org/10.1016/j.eatbeh.2013.07.002.
- 51. Meule A, Gearhardt AN. Ten years of the yale food addiction scale: a review of version 2.0. Curr Addict Rep. 2019;6(3):218–28. https://doi.org/10.1007/s40429-019-00261-3.
- 52. Minhas M, Murphy CM, Balodis IM, Samokhvalov AV, MacKillop J. Food addiction in a large community sample of canadian adults: prevalence and relationship with obesity, body composition, quality of life and impulsivity. Addiction. 2021 Oct;116(10):2870–9. https://doi.org/10.1111/add.15446.
- 53. Fielding-Singh P, Patel ML, King AC, Gardner CD. Baseline psychosocial and demographic factors associated with study attrition and 12-month weight gain in the DIETFITS trial. Obesity. 2019 Dec;27(12):1997–2004. https://doi.org/10.1002/oby.22650.
- 54. Camacho-Barcia L, Munguía L, Gaspar-Pérez A, Jimenez-Murcia S, Fernández-Aranda F. Impact of food addiction in therapy response in obesity and eating disorders. Curr Addict Rep. 2022;2. https://doi.org/10.1007/s40429-022-00421-y.
- 55. Praxedes DRS, Silva-Junior AE, Macena ML, Oliveira AD, Cardoso KS, Nunes LO, et al. Prevalence of food addiction determined by the yale food addiction scale and associated factors: a systematic review with meta-analysis. Eur Eat Disord Rev. 2022 Mar;30(2):85–95. https://doi.org/10.1002/erv.2878.
- 56. Yekaninejad MS, Badrooj N, Vosoughi F, Lin CY, Potenza MN, Pakpour AH. Prevalence of food addiction in children and adolescents: a systematic review and meta-analysis. Obes Rev. 2021 Jun;22(6):e13183. https://doi.org/10.1111/obr.13183.
- 57. World Health Organization. Global status report on alcohol and health 2018. Geneva: World Health Organization; 2019.
- 58. World Health Organization. WHO report on the global tobacco epidemic 2019: offer help to quit tobacco use. Geneva: World Health Organization; 2019.
- 59. Zawertailo L, Attwells S, deRuiter WK, Le TL, Dawson D, Selby P. Food addiction and tobacco use disorder: common liability and shared mechanisms. Nutrients. 2020 Dec;12(12):3834. https://doi.org/10.3390/nu12123834.
- 60. Nunes-Neto PR, Kohler CA, Schuch FB, Solmi M, Quevedo J, Maes M, et al. Food addiction: prevalence, psychopathological correlates and associations with quality of life in a large sample. J Psychiatr Res. 2018 Jan;96:145–52. https://doi.org/10.1016/j.jpsychires.2017.10.003.
- 61. Maxwell AL, Gardiner E, Loxton NJ. Investigating the relationship between reward sensitivity, impulsivity, and food addiction: a systematic review. Eur Eat Disord Rev. 2020 Jul;28(4):368–84. https://doi.org/10.1002/erv.2732.
- 62. Naish KR, MacKillop J, Balodis IM. The concept of food addiction: a review of the current evidence. Curr Behav Neurosci Rep. 2018 Dec;5(4):281–94. https://doi.org/10.1007/s40473-018-0169-2.
- 63. Minhas M, Murphy CM, Balodis IM, Acuff SF, Buscemi J, Murphy JG, et al. Multidimensional elements of impulsivity as shared and unique risk factors for food addiction and alcohol misuse. Appetite. 2021 Apr;159:105052. https://doi.org/10.1016/j.appet.2020.105052.
- 64. Hoover LV, Yu HP, Cummings JR, Ferguson SG, Gearhardt AN. Co-occurrence of food addiction, obesity, problematic substance use, and parental history of problematic alcohol use. Psychol Addict Behav. 2022. https://doi.org/10.1037/adb0000870.
- 65. Volkow ND, Wise RA. How can drug addiction help us understand obesity?Nat Neurosci. 2005 May;8(5):555–60. https://doi.org/10.1038/nn1452.
- 66. Saxena I, Suman S, Kaur AP, Mitra P, Sharma P, Kumar M. The multiple causes of obesity. In: Rao V, Rao L, editors. Role of obesity in human health and disease [Internet]. London: IntechOpen; 2021. [cited 2022 Aug 16]. Available from: https://www.intechopen.com/chapters/77606.
- 67. Thaker VV. Genetic and epigenetic causes of obesity. Adolesc Med State Art Rev. 2017 Nov;28(2):379–405.
- 68. Schulte EM, Gearhardt AN. Attributes of the food addiction phenotype within overweight and obesity. Eat Weight Disord. 2021 Aug;26(6):2043–9. https://doi.org/10.1007/s40519-020-01055-7.
- 69. Pursey KM, Gearhardt AN, Burrows TL. The relationship between “food addiction” and visceral adiposity in young females. Physiol Behav. 2016 Apr;157:9–12. https://doi.org/10.1016/j.physbeh.2016.01.018.
- 70. Kiyici S, Koca N, Sigirli D, Aslan BB, Guclu M, Kisakol G. Food addiction correlates with psychosocial functioning more than metabolic parameters in patients with obesity. Metab Syndr Relat Disord. 2020 Apr;18(3):161–7. https://doi.org/10.1089/met.2019.0108.
- 71. Nicolau J, Romerosa JM, Rodriguez I, Sanchis P, Bonet A, Arteaga M, et al. Associations of food addiction with metabolic control, medical complications and depression among patients with type 2 diabetes. Acta Diabetol. 2020 Sep;57(9):1093–100. https://doi.org/10.1007/s00592-020-01519-3.
- 72. Brewerton TD. Food addiction as a proxy for eating disorder and obesity severity, trauma history, ptsd symptoms, and comorbidity. Eat Weight Disord. 2017 Jun;22(2):241–7. https://doi.org/10.1007/s40519-016-0355-8.
- 73. Flint AJ, Gearhardt AN, Corbin WR, Brownell KD, Field AE, Rimm EB. Food-addiction scale measurement in 2 cohorts of middle-aged and older women. Am J Clin Nutr. 2014 Mar;99(3):578–86. https://doi.org/10.3945/ajcn.113.068965.
- 74. Brytek-Matera A, Obeid S, Akel M, Hallit S. How does food addiction relate to obesity? Patterns of psychological distress, eating behaviors and physical activity in a sample of Lebanese adults: the MATEO study. Int J Environ Res Public Health. 2021 Oct;18(20):10979. https://doi.org/10.3390/ijerph182010979.
- 75. Merlo LJ, Klingman C, Malasanos TH, Silverstein JH. Exploration of food addiction in pediatric patients: a preliminary investigation. J Addict Med. 2009 Mar;3(1):26–32. https://doi.org/10.1097/adm.0b013e31819638b0.
- 76. Wenzel KR, Weinstock J, McGrath AB. The clinical significance of food addiction. J Addict Med. 2020 Sep;14(5):e153–e159. https://doi.org/10.1097/adm.0000000000000626.
- 77. Kidd C, Loxton NJ. A narrative review of reward sensitivity, rash impulsivity, and food addiction in adolescents. Prog Neuropsychopharmacol Biol Psychiatry. 2021 Jul;109:110265. https://doi.org/10.1016/j.pnpbp.2021.110265.
- 78. Meule A, Hermann T, Kubler A. Food addiction in overweight and obese adolescents seeking weight-loss treatment. Eur Eat Disord Rev. 2015 May;23(3):193–8. https://doi.org/10.1002/erv.2355.
- 79. Schiestl ET, Rios JM, Parnarouskis L, Cummings JR, Gearhardt AN. A narrative review of highly processed food addiction across the lifespan. Prog Neuropsychopharmacol Biol Psychiatry. 2021 Mar;106:110152. https://doi.org/10.1016/j.pnpbp.2020.110152.
- 80. Skinner J, Jebeile H, Burrows T. Food addiction and mental health in adolescents: a systematic review. Lancet Child Adolesc Health. 2021 Oct;5(10):751–66. https://doi.org/10.1016/s2352-4642(21)00126-7.
- 81. Penzenstadler L, Soares C, Karila L, Khazaal Y. Systematic review of food addiction as measured with the Yale Food Addiction Scale: implications for the food addiction construct. Curr Neuropharmacol. 2019;17(6):526–38. https://doi.org/10.2174/1570159x16666181108093520.
- 82. Gordon EL, Ariel-Donges AH, Bauman V, Merlo LJ. What is the evidence for “food addiction?” A systematic review. Nutrients. 2018 Apr;10(4):477. https://doi.org/10.3390/nu10040477.
- 83. Schulte EM, Kral TVE, Allison KC. A cross-sectional examination of reported changes to weight, eating, and activity behaviors during the COVID-19 pandemic among United States adults with food addiction. Appetite. 2022 Jan;168:105740. https://doi.org/10.1016/j.appet.2021.105740.
- 84. Filgueiras AR, Pires de Almeida VB, Koch Nogueira PC, Alvares Domene SM, Eduardo da Silva C, Sesso R, et al. Exploring the consumption of ultra-processed foods and its association with food addiction in overweight children. Appetite. 2019 Apr;135:137–45. https://doi.org/10.1016/j.appet.2018.11.005.
- 85. Ayaz A, Nergiz-Unal R, Dedebayraktar D, Akyol A, Pekcan AG, Besler HT, et al. How does food addiction influence dietary intake profile?PLoS One. 2018 Apr;13(4):e0195541. https://doi.org/10.1371/journal.pone.0195541.
- 86. Burrows T, Hides L, Brown R, Dayas CV, Kay-Lambkin F. Differences in dietary preferences, personality and mental health in Australian adults with and without food addiction. Nutrients. 2017 Mar;9(3):285. https://doi.org/10.3390/nu9030285.
- 87. Lopez-Lopez DE, Saavedra-Roman IK, Calizaya-Milla YE, Saintila J. Food addiction, saturated fat intake, and body mass index in Peruvian adults: a cross-sectional survey. J Nutr Metab. 2021 Jul;2021:99641431–7. https://doi.org/10.1155/2021/9964143.
- 88. de Almeida VBP, Filgueiras AR, Nogueira PCK, Sesso R, Sawaya AL, Domene SMA. The impact of food addiction behaviours on the treatment of overweight students. Br J Nutr. 2021:1–23. https://doi.org/10.1017/s0007114521004189.
- 89. Tompkins CL, Laurent J, Brock DW. Food addiction: a barrier for effective weight management for obese adolescents. Child Obes. 2017 Dec;13(6):462–9. https://doi.org/10.1089/chi.2017.0003.
- 90. Martin-Fernandez KW, Creel DB, Schuh LM. Psychosocial and behavioral correlates of weight loss 12 to 15 years after bariatric surgery. J Behav Med. 2022 Apr;45(2):252–9. https://doi.org/10.1007/s10865-021-00263-5.
- 91. Clark SM, Saules KK, Schuh LM, Stote J, Creel DB. Associations between relationship stability, relationship quality, and weight loss outcomes among bariatric surgery patients. Eat Behav. 2014;15(4):670–2. https://doi.org/10.1016/j.eatbeh.2014.09.003.
- 92. Meule A, Gearhardt AN. Five years of the Yale Food Addiction Scale: taking stock and moving forward. Curr Addict Rep. 2014 Sep;1(3):193–205. https://doi.org/10.1007/s40429-014-0021-z.
- 93. Vannicelli M. A dualistic model for group treatment of alcohol problems: abstinence-based treatment for alcoholics, moderation training for problem drinkers. Int J Group Psychother. 2002 Apr;52(2):189–213. https://doi.org/10.1521/ijgp.52.2.189.45498.
- 94. Adams RC, Sedgmond J, Maizey L, Chambers CD, Lawrence NS. Food addiction: implications for the diagnosis and treatment of overeating. Nutrients. 2019 Sep;11(9):2086. https://doi.org/10.3390/nu11092086.
- 95. Fauconnier M, Rousselet M, Brunault P, Thiabaud E, Lambert S, Rocher B, et al. Food addiction among female patients seeking treatment for an eating disorder: prevalence and associated factors. Nutrients. 2020 Jun;12(6):1897. https://doi.org/10.3390/nu12061897.
- 96. Hudson JI, Hiripi E, Pope HG Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey replication. Biol Psychiatry. 2007 Feb;61(3):348–58. https://doi.org/10.1016/j.biopsych.2006.03.040.
- 97. Gearhardt AN, Boswell RG, White MA. The association of “food addiction” with disordered eating and body mass index. Eat Behav. 2014 Aug;15(3):427–33. https://doi.org/10.1016/j.eatbeh.2014.05.001.
- 98. Ivezaj V, White MA, Grilo CM. Examining binge-eating disorder and food addiction in adults with overweight and obesity. Obesity. 2016 Oct;24(10):2064–9. https://doi.org/10.1002/oby.21607.
- 99. Tran H, Poinsot P, Guillaume S, Delaunay D, Bernetiere M, Begin C, et al. Food addiction as a proxy for anorexia nervosa severity: new data based on the Yale Food Addiction Scale 2.0. Psychiatry Res. 2020 Nov;293:113472. https://doi.org/10.1016/j.psychres.2020.113472.
- 100. Albayrak O, Focker M, Kliewer J, Esber S, Peters T, de Zwaan M, et al. Eating-related psychopathology and food addiction in adolescent psychiatric inpatients. Eur Eat Disord Rev. 2017 May;25(3):214–20. https://doi.org/10.1002/erv.2509.
- 101. C Barbarich-Marsteller NC, W Foltin R, Timothy Walsh B. Does anorexia nervosa resemble an addiction?Curr Drug Abuse Rev. 2011 Sep;4(3):197–200. https://doi.org/10.2174/1874473711104030197.
- 102. Schreiber LRN, Odlaug BL, Grant JE. The overlap between binge eating disorder and substance use disorders: diagnosis and neurobiology. J Behav Addict. 2013 Dec;2(4):191–8. https://doi.org/10.1556/jba.2.2013.015.
- 103. Munguia L, Gaspar-Perez A, Jimenez-Murcia S, Granero R, Sanchez I, Vintro-Alcaraz C, et al. Food addiction in eating disorders: a cluster analysis approach and treatment outcome. Nutrients. 2022 Mar;14(5):1084. https://doi.org/10.3390/nu14051084.
- 104. Romero X, Aguera Z, Granero R, Sanchez I, Riesco N, Jimenez-Murcia S, et al Is food addiction a predictor of treatment outcome among patients with eating disorder? Eur Eat Disord Rev. 2019 Nov;27(6):700–11. https://doi.org/10.1002/erv.2705.
- 105. Hilker I, Sanchez I, Steward T, Jimenez-Murcia S, Granero R, Gearhardt AN, et al. Food addiction in bulimia nervosa: clinical correlates and association with response to a brief psychoeducational intervention. Eur Eat Disord Rev. 2016 Nov;24(6):482–8. https://doi.org/10.1002/erv.2473.
- 106. N Gearhardt AN, White AM, N Potenza M. Binge eating disorder and food addiction. Curr Drug Abuse Rev. 2011 Sep;4(3):201–7. https://doi.org/10.2174/1874473711104030201.
- 107. Parnarouskis L, Gearhardt AN. Preliminary evidence that tolerance and withdrawal occur in response to ultra-processed foods. Curr Addict Rep. 2022:1–8. https://doi.org/10.1007/s40429-022-00425-8.
- 108. Marlatt GA, Witkiewitz K. Harm reduction approaches to alcohol use: health promotion, prevention, and treatment. Addict Behav. 2002 Nov;27(6):867–86. https://doi.org/10.1016/s0306-4603(02)00294-0.
- 109. Kwag KH, Kim YR, Lee YK, Lee HR, Lee JY, Lee J, et al. Feasibility and acceptability of a digital tele-guided intervention targeting components of the addictive appetite model for bulimia nervosa and binge-eating disorder in Korea. Int J Eat Disord. 2022;55(7):977–82. https://doi.org/10.1002/eat.23754.
- 110. Carbone EA, Caroleo M, Rania M, Calabrò G, Staltari FA, de Filippis R, et al. An open-label trial on the efficacy and tolerability of naltrexone/bupropion SR for treating altered eating behaviours and weight loss in binge eating disorder. Eat Weight Disord. 2021 Apr;26(3):779–88. https://doi.org/10.1007/s40519-020-00910-x.
- 111. Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry. 2013 Aug;170(8):834–51. https://doi.org/10.1176/appi.ajp.2013.12060782.
- 112. DeShazo RD, Johnson M, Eriator I, Rodenmeyer K. Backstories on the US opioid epidemic. Good intentions gone bad, an industry gone rogue, and watch dogs gone to sleep. Am J Med. 2018 Jun;131(6):595–601. https://doi.org/10.1016/j.amjmed.2017.12.045.
- 113. Healton C, Pack R, Galea S. The opioid crisis, corporate responsibility, and lessons from the tobacco master settlement agreement. JAMA. 2019 Dec;322(21):2071–2. https://doi.org/10.1001/jama.2019.17144.
- 114. Richman I, Krumholz HM. Lessons from the opioid epidemic to reinvigorate tobacco control initiatives. JAMA. 2018 Jan;319(4):339–40. https://doi.org/10.1001/jama.2017.19739.
- 115. Brownell KD, Warner KE. The perils of ignoring history: big tobacco played dirty and millions died. How similar is Big Food?Milbank Q. 2009 Mar;87(1):259–94. https://doi.org/10.1111/j.1468-0009.2009.00555.x.
- 116. Giovino GA. The tobacco epidemic in the United States. Am J Prev Med. 2007 Dec;33(6 Suppl l):S318–S326. https://doi.org/10.1016/j.amepre.2007.09.008.
- 117. McLellan AT, Koob GF, Volkow ND. Preaddiction: a missing concept for treating substance use disorders. JAMA Psychiatry. 2022 Aug;79(8):749–51. https://doi.org/10.1001/jamapsychiatry.2022.1652.