Introduction
The term “respiratory failure” includes “pump failure” (ventilatory failure: manifested mainly as hypercapnia) and “lung failure” (gas exchange failure manifested mainly as hypoxaemia) []. Long-term home mechanical ventilation is increasingly used by patients with chronic ventilatory failure (CVF) due to advanced diseases such as chronic obstructive pulmonary disease (COPD), restrictive thoracic disease and neuromuscular diseases []. The last reported (and underestimated) prevalence of European patients requiring long-term assisted ventilation is 6.6 per 100,000 population []. Other surveys report prevalences ranging from 9.9 to 23 per 100,000 population [-].
CVF may be associated with severe dyspnoea, limiting exercise capacity. Long-term non-invasive ventilation (NIV) may reduce patients’ symptoms, improve health-related quality of life (HRQL) and, in many cases, reduce mortality and hospitalisations [-]. The effects on exercise capacity depend on the underlying diseases leading to CVF [].
Pulmonary rehabilitation programmes including aerobic exercise training have stronger evidence of effectiveness in improving exercise capacity, dyspnoea and HRQL than almost all other therapies in patients with COPD, including those with very severe disease, and with a lower level of evidence in other pathologies [-]. Therefore, current guidelines recommend pulmonary rehabilitation, including exercise training, in these patients [, ]. Although there is some evidence of effectiveness of exercise training also in patients with CVF [], there are few data in patients requiring long-term NIV.
Assisted ventilation is increasingly used during exercise training programmes in order to train patients at intensity levels higher than allowed by their clinical and pathophysiological conditions []. This, as well as other tools [], may allow to widen the “personalised” sequential levels of pulmonary rehabilitation for the most severely affected patients []. This narrative review updates the possibilities of exercise training in patients with CVF and the use of NIV as a tool to increase the benefits of exercise in these patients.
Methods
We searched papers published (or with at least the summary) in English language between 1985 and 2018 in PubMed and Scopus databases using the keywords “chronic respiratory failure AND exercise,” “non invasive ventilation AND exercise,” “pulmonary rehabilitation” and “exercise training.”
Exercise Training for Patients with CVF
Well-designed randomised controlled trials (RCTs) of different length (from 2 months to 2 years) showed that adding night-time NIV to day-time exercise training in severe stable COPD patients resulted in significant improvement in exercise capacity and HRQL compared to patients undergoing exercise training alone [-]. Two randomised cross-over trials on small populations of patients showed that walking with NIV resulted in improved oxygenation, decreased dyspnoea and increased walking distance in patients with COPD under home NIV [, ]. However, another randomised cross-over physiological study on few patients showed that the use of NIV during walking without supplemental oxygen did not prevent exercise-induced hypoxaemia [].
Exercise training has also been evaluated in a RCT in patients with kyphoscoliosis under NIV with beneficial effects on exercise capacity, muscle strength, dyspnoea and HRQL after 12 weeks []. In a RCT on a small sample size of patients with restrictive thoracic disease, home-based exercise training with NIV was effective and feasible [], confirming an old physiological small study []. A non-randomised study showed that an individually tailored pulmonary rehabilitation programme plus night-time NIV was feasible in hypercapnic patients with interstitial lung disease and significantly improved exercise capacity and HRQL [].
In a recent RCT on an adequate sample size of obese patients with obstructive apnoea syndrome treated with continuous positive airway pressure (CPAP), the addition of respiratory muscle training or NIV to exercise training did not result in any further improvement in functional capacity as compared to exercise training alone. However, the addition of NIV to exercise training was superior in improving cardiometabolic risk factors []. A single-centre pilot RCT showed that in patients with obesity hypoventilation syndrome, a 3-month rehabilitation programme, in addition to NIV, resulted in improved weight loss, exercise capacity and HRQL at the end of the rehabilitation period, but these effects were not maintained at 12 months [].
A recent retrospective study has shown that pulmonary rehabilitation was feasible and resulted in improvements in exercise capacity and HRQL also in patients awaiting lung transplantation on nocturnal NIV. Furthermore, despite more severe disease, patients under NIV had a greater benefit from rehabilitation than patients without NIV [].
Recently, wearable ventilators have been proposed for exercise [, ]. A study examined the effect of NIV in environments with different temperatures and humidities during different activities []. Overall, NIV resulted in similar physiological and perceptual responses under all environmental conditions. Use of NIV increased heart rate during the most strenuous tasks, indicating that NIV may stress cardiovascular function during moderate-to-high intensity activities. Whether these observations can be applied also to patients with CVF is unknown.
Physiological Effects of NIV on Exercise
In patients with COPD, NIV during exercise unloads the dysfunctional inspiratory muscles with an inspiratory positive airway pressure (IPAP) [] and reduces the work of breathing (WOB) with an expiratory positive airway pressure (EPAP) or with CPAP [].
Muscle blood flow and metabolic demand are matched in patients with COPD at submaximal exercise []. However, when WOB increases with increasing exercise intensity, blood flow may switch from the limbs to the respiratory muscles, leading to earlier peripheral muscle fatigue. This condition may be improved by adding assisted ventilation during exercise [, ].
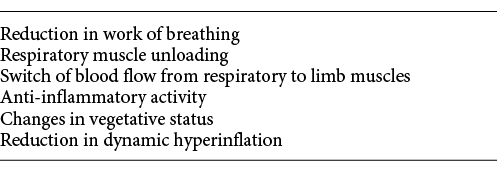
Other mechanisms may work. Assisted ventilation may prevent the inflammatory response to exercise in patients with COPD and muscle wasting [] and influence some endogenous factors in healthy people []. Furthermore, NIV may reduce the sympathetic activation during exercise with positive effects on the cardiovascular system as well as on muscle function [, ]. Nevertheless, there are no physiological studies in patients with CVF under long-term NIV. Table 1 summarises the potential mechanisms of NIV action during exercise.
Theoretically, in COPD patients, CPAP might reduce the dynamic hyperinflation, relieving dyspnoea and increasing exercise capacity []. However, for optimal benefits, the level of CPAP should be tailored to the individual patient measuring the “intrinsic” positive end-expiratory pressure, a difficult or impossible manoeuvre to perform on a routine setting [].
With inspiratory pressure support, each breath may be triggered and supported by the patient or by the ventilator []. In severe COPD patients during exercise, an IPAP relieves dyspnoea and increases exercise tolerance, reducing the high WOB [], and patients can longer sustain exercise-induced lactataemia []. Furthermore, a double-blind RCT has shown that during exercise non-invasive IPAP with an EPAP improved central haemodynamics and cerebral oxygenation in patients with COPD and exercise-induced desaturations [].
Proportional assist ventilation (PAV) provides inspiratory flow and pressure in proportion to patients’ effort and timing []. Non-invasive PAV increases exercise capacity of COPD patients without any relevant haemodynamic effect [, ].
NIV and Exercise Training Programmes
In a RCT [], patients with stable COPD without respiratory failure (mean forced expiratory volume at 1 s [FEV1]: 48% pred.; mean arterial carbon dioxide tension [PaCO2]: 39.5 mm Hg) undergoing an outpatient exercise training programme were randomised to training with or without a PAV mask. Twenty-eight percent of patients in the PAV group dropped out due to lack of compliance with equipment or setting. Both groups showed significant improvements in exercise tolerance, dyspnoea and leg fatigue. Another similar RCT [] evaluated patients with more severe COPD (mean FEV1: 28% pred.; mean PaCO2: 42.6 mm Hg) undergoing supervised outpatient exercise training. Patients were randomised to exercise with or without non-invasive PAV. Mean training intensity and peak work rate after training were higher and lactate at iso-workload after training was reduced more in the group under PAV []. Exercise training with NIV was associated with a reduction in inflammatory markers in patients with COPD []. Other RCTs have confirmed the benefits of NIV during exercise training [-] and during exercise training with the addition of heliox or inspiratory muscle training [, ].
These studies indicate that NIV-assisted exercise training may be indicated also for patients with COPD not requiring long-term assisted ventilation, with severe clinical and/or physiological conditions as assessed by the level of dyspnoea, airway obstruction or PaCO2.
However, 2 recent meta-analyses were inconclusive on the effect of NIV in exercise training programmes in COPD [, ]. A meta-analysis [] including RCTs that compared NIV during exercise training versus exercise training alone or exercise training with sham NIV in patients with COPD concluded that the small number (6) of included studies with small numbers of participants, as well as the high risk of bias within some of the included studies, limited the ability to draw strong evidence-based conclusions. Another meta-analysis [] found only 8 studies (7 RCTs) providing a proper description of a training schedule. Due to the small number of the available studies, the small sample sizes and the complete absence of power calculation, the authors required more RCTs with larger sample sizes based on statistical power calculations and designed to investigate the effect of training duration and intensity on rehabilitation. The ATS/ERS pulmonary rehabilitation statement [] concluded that NIV during exercise training is “difficult and labor intensive” and may only be feasible in specialist units. The authors of the present review share the conclusions of those meta-analyses [, ] and the ATS/ERS statement [] and additionally suggest more studies with sham ventilation as a control.
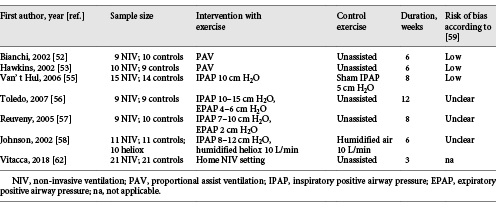
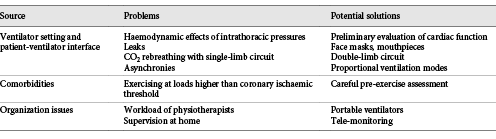
A summary of relevant RCTs on the use of NIV during exercise training is shown in Table 2. Potential problems using NIV in exercise training sessions are shown in Table 3 [].
The use of NIV during exercise training may be difficult in naïve patients not familiar with ventilators, interfaces and ventilator settings. Recently, patients with CVF on home nocturnal NIV and long-term oxygen therapy for at least 6 months were studied []. Patients of the study group performed NIV during exercise training sessions with the same ventilator, mask (85.7% face mask, 14.3% nasal mask) and, at the start of exercise, ventilatory setting (mean IPAP: 17.4 cm H2O; EPAP: 6.5 cm H2O; inspiratory time: 1.2 s) as used at home. The control group performed exercise without NIV. The addition of NIV resulted in a significantly greater improvement in endurance time. The incremental exercise test and dyspnoea improved significantly in both groups. Only patients with NIV improved their respiratory muscle function and leg fatigue, whereas HRQL was significantly improved only in controls [].
Some Technical Considerations
Studies in patients with CVF [, , ] used only relatively low levels of IPAP (15–17 cm H2O) during exercise with NIV. The effectiveness of the proposed pressures as high as needed to reduce PaCO2 in the long term [] during exercise training in patients with CVF is still unknown. Long-term NIV with adequate pressure to improve gas exchange did not have an overall adverse effect on cardiac performance []. Nevertheless, confirming an earlier study [] in patients with pre-existing heart failure, the application of very high inspiratory pressures might reduce cardiac output []. However, the cardiovascular effects of the intrathoracic pressures during exercise in patients with CVF and different cardiovascular functions are unknown. A study indicated that NIV with IPAP (16 cm H2O) and EPAP (5 cm H2O) may improve stroke volume and exercise tolerance in selected patients with advanced COPD []. However, impaired responses of stroke volume and cardiac output, associated with a lack of improvement in exercise capacity, were found in a sub-group of patients with severe hyperinflation at rest []. Therefore, a preliminary evaluation of lung and cardiac function should be performed prior to submission to exercise with NIV.
During high-intensity exercise requiring high ventilatory levels, many if not most of the patients may breathe (also) through their mouth, with increasing air leaks, therefore requiring a full-face mask or a mouthpiece. Full-face masks may be more uncomfortable than nasal masks, potentially reducing the compliance with the procedure. Figure 1 shows a patient exercising with a face mask.

Fig. 1
A patient exercising with a face mask.
The use of a plateau exhalation valve when NIV is added to exercise in patients with severe COPD must be considered. During exercise, with the increase in exhalation flow and respiratory rate, a reduced ability of a plateau exhalation valve to exhale gases out of the circuit may result in CO2 rebreathing in patients ventilated by a single-limb circuit. This problem was evaluated by a study in patients with stable severe COPD performing a maximal symptom-limited cycle exercise test while ventilated on pressure support []. As compared to rest, during exercise there was a significant increase in mean expiratory flow and fractional concentration of end-tidal CO2 and a significant decrease in mean expiratory flow of plateau exhalation valve; the tidal fractional concentration of inspired CO2 significantly increased at peak exercise []. Therefore, a double-limb circuit might be necessary.
Most patients with CVF have a high prevalence of comorbidities, among which ischaemic cardiac disease is frequent []. The relief of exercise-induced dyspnoea associated with this “mechanical doping” [] might lead patients with unknown cardiac ischaemia to exercise at an intensity higher than their coronary ischaemic threshold. A careful clinical and physiological assessment of the patient is required before submission to this modality of training.
In a study by Bianchi et al. [], there was a high rate of dropouts among patients exercising with NIV. The long time required by the operators to apply interfaces, to check for leaks and to tailor the ventilator setting to the individual patient may be other practical drawbacks. The need of a greater physiotherapist-to-patient ratio increases the costs, whereas well-conducted standard pulmonary rehabilitation programmes are effective and do not require complex and sophisticated machinery or a personalised physiotherapist [].
An additional issue is the evaluation and reduction of potential risks of exercise under NIV or even invasive assisted ventilation in ventilator-dependent patients in locations far from healthcare institutions. Tele-monitoring may be useful. Tele-monitoring is increasingly proposed for ventilator-dependent patients []. With tele-rehabilitation programmes, patients may perform exercises at home under supervision by a physiotherapist who may prescribe and change strategies and settings at distance []. Tele-rehabilitation might offer a valid aid in monitoring also patients performing exercise under NIV, but at present, there is no evidence yet.
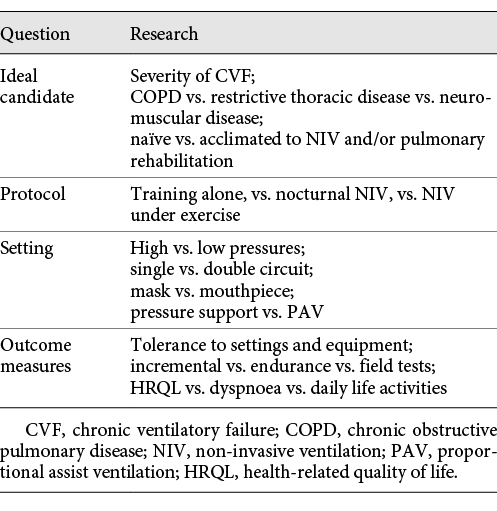
Several questions remain open (Table 4): future research should evaluate (1) the ideal candidate; (2) the most effective protocols; (3) the most effective and least harmful setting; and (4) the most appropriate outcome measures.
Potential Alternatives and Future Applications
The type of ventilatory mode may significantly affect exercise performance. Inefficient mechanical unloading and patient-ventilator asynchronies may limit the tolerance for exercise []. Proportional modes of assisted ventilation like PAV can translate into longer and more efficient training sessions []. A preliminary study [] in intubated patients showed that proportional ventilation modes such as PAV and the more recently introduced Neurally Adjusted Ventilatory Assist (NAVA) [] during exercise resulted in higher work efficiency and less increase in oxygen consumption compared to ventilation with inspiratory pressure support []. Whether these results can be translated to patients with CVF is unknown.
Alternative strategies other than NIV might be useful to improve exercise capacity in patients with CVF. High-flow nasal cannula (HFNC) can deliver up to 60 L/min of reheated, humidified air via nasal cannula, with or without additional oxygen. Above a flow of 20 L/min, HFNC generates a positive pressure in the upper airways [], inducing an increase in alveolar ventilation, improvements in gas exchange and a reduction in WOB in patients with COPD [, ]. Preliminary reports indicate that HFNC may improve exercise performance, oxygen saturation and perceived symptoms in patients with severe COPD and ventilatory limitation []. Whether these preliminary results can also be applied to patients with CVF should be the object of future research.
Tidal expiratory flow limitation (EFLT) increases “intrinsic” positive end-expiratory pressure at rest and during exercise. The Forced Oscillatory Technique system can monitor EFLT by measuring within-breath changes in reactance at 5 Hz []. Automatic adjustment of EPAP to minimize EFLT during effort or training might allow to tailor EPAP, maintaining or improving blood gases, WOB and dyspnoea with better comfort.
Conclusions
There is a need for other and better-quality RCTs, compared with sham, to investigate the effect of optimal training duration and intensity of NIV-assisted exercise training in patients with CVF.
Disclosure Statement
The authors declare that there is no actual or potential conflict of interest.
References
- 1. Ambrosino N, Guarracino F. Respiratory Failure. In Palange P, Simonds A (eds): ERS Handbook of Respiratory Medicine 2n Ed. 2013, pp 162-165.
- 2. Ambrosino N, Vitacca M. The patient needing prolonged mechanical ventilation: a narrative review. Multidiscip Respir Med. 2018;13(1):6.
- 3. Lloyd-Owen SJ, Donaldson GC, Ambrosino N, Escarabill J, Farre R, Fauroux B, et al Patterns of home mechanical ventilation use in Europe: results from the Eurovent survey. Eur Respir J. 2005;25(6):1025–31.
- 4. Rose L, McKim DA, Katz SL, Leasa D, Nonoyama M, Pedersen C, et alCANuVENT Group. Home mechanical ventilation in Canada: a national survey. Respir Care. 2015;60(5):695–704.
- 5. Garner DJ, Berlowitz DJ, Douglas J, Harkness N, Howard M, McArdle N, et al Home mechanical ventilation in Australia and New Zealand. Eur Respir J. 2013;41(1):39–45.
- 6. Escarrabill J, Tebé C, Espallargues M, Torrente E, Tresserras R, Argimón Jen nombre del equipo del Plan Director de las Enfermedades del Aparato Respiratorio (PDMAR) y del Observatorio de Terapias Respiratorias (Obs TRD). Variability in home mechanical ventilation prescription. Arch Bronconeumol. 2015;51(10):490–5.
- 7. Köhnlein T, Windisch W, Köhler D, Drabik A, Geiseler J, Hartl S, et al Non-invasive positive pressure ventilation for the treatment of severe stable chronic obstructive pulmonary disease: a prospective, multicentre, randomised, controlled clinical trial. Lancet Respir Med. 2014;2(9):698–705.
- 8. MacIntyre EJ, Asadi L, Mckim DA, Bagshaw SM. Clinical outcomes associated with home mechanical ventilation: a systematic review. Can Respir J. 2016;2016:6547180.
- 9. Murphy PB, Rehal S, Arbane G, Bourke S, Calverley PM, Crook AM, et al Effect of home noninvasive ventilation with oxygen therapy vs oxygen therapy alone on hospital readmission or death after an acute COPD exacerbation: A randomized clinical trial. JAMA. 2017;317(21):2177–86.
- 10. Salturk C, Karakurt Z, Takir HB, Balci M, Kargin F, Mocin OY, et al Comparison of exercise capacity in COPD and other etiologies of chronic respiratory failure requiring non-invasive mechanical ventilation at home: retrospective analysis of 1-year follow-up. Int J Chron Obstruct Pulmon Dis. 2015;10:2559–69.
- 11. Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et alATS/ERS Task Force on Pulmonary Rehabilitation. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–64.
- 12. McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;2(2):CD003793.
- 13. Paneroni M, Simonelli C, Vitacca M, Ambrosino N. Aerobic exercise training in very severe COPD: a systematic review and meta-analysis. Am J Phys Med Rehabil. 2017;96:541–8.
- 14.
- 15. Carone M, Patessio A, Ambrosino N, Baiardi P, Balbi B, Balzano G, et al Efficacy of pulmonary rehabilitation in chronic respiratory failure (CRF) due to chronic obstructive pulmonary disease (COPD): The Maugeri Study. Respir Med. 2007;101(12):2447–53.
- 16. Ambrosino N, Xie L. The Use of non-invasive ventilation during exercise training in COPD patients. COPD. 2017;14(4):396–400.
- 17. Camillo CA, Osadnik CR, van Remoortel H, Burtin C, Janssens W, Troosters T. Effect of “add-on” interventions on exercise training in individuals with COPD: a systematic review. ERJ Open Res. 2016;2(1):00078–02015.
- 18. Ambrosino N, Clini EM. Response to pulmonary rehabilitation: toward personalised programmes?Eur Respir J. 2015;46(6):1538–40.
- 19. Garrod R, Mikelsons C, Paul EA, Wedzicha JA. Randomized controlled trial of domiciliary noninvasive positive pressure ventilation and physical training in severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;162(4 Pt 1):1335–41.
- 20. Duiverman ML, Wempe JB, Bladder G, Jansen DF, Kerstjens HA, Zijlstra JG, et al Nocturnal non-invasive ventilation in addition to rehabilitation in hypercapnic patients with COPD. Thorax. 2008;63(12):1052–7.
- 21. Duiverman ML, Wempe JB, Bladder G, Vonk JM, Zijlstra JG, Kerstjens HA, et al Two-year home-based nocturnal noninvasive ventilation added to rehabilitation in chronic obstructive pulmonary disease patients: a randomized controlled trial. Respir Res. 2011;12(1):112.
- 22. Dreher M, Storre JH, Windisch W. Noninvasive ventilation during walking in patients with severe COPD: a randomised cross-over trial. Eur Respir J. 2007;29(5):930–6.
- 23. Menadue C, Alison JA, Piper AJ, Flunt D, Ellis ER. Non-invasive ventilation during arm exercise and ground walking in patients with chronic hypercapnic respiratory failure. Respirology. 2009;14(2):251–9.
- 24. Walker DJ, Walterspacher S, Ekkernkamp E, Storre JH, Windisch W, Dreher M. Walking with non-invasive ventilation does not prevent exercise-induced hypoxaemia in stable hypercapnic COPD patients. COPD. 2015;12(5):546–51.
- 25. Cejudo P, López-Márquez I, López-Campos JL, Márquez E, de la Vega F, Barrot E, et al Randomized controlled trial of exercise training in chronic respiratory failure due to kyphoscoliosis. Respir Care. 2014;59:375–82.
- 26. Borel JC, Verges S, Pepin JL, Vivodtzev I, Levy P, Wuyam B. Home exercise training with non-invasive ventilation in thoracic restrictive respiratory disorders: a randomised study. Respir Physiol Neurobiol. 2009;167(2):168–73.
- 27. Tsuboi T, Ohi M, Chin K, Hirata H, Otsuka N, Kita H, et al Ventilatory support during exercise in patients with pulmonary tuberculosis sequelae. Chest. 1997;112(4):1000–7.
- 28. Dreher M, Ekkernkamp E, Schmoor C, Schoenheit-Kenn U, Winterkamp S, Kenn K. Pulmonary rehabilitation and noninvasive ventilation in patients with hypercapnic interstitial lung disease. Respiration. 2015;89(3):208–13.
- 29. Vivodtzev I, Tamisier R, Croteau M, Borel JC, Grangier A, Wuyam B, et al: Ventilatory support or respiratory muscle training as adjuncts to exercise in obese CPAP-treated patients with obstructive sleep apnoea: a randomised controlled trial. Thorax. 2018. pii: thoraxjnl-2017-211152. doi: . [Epub ahead of print].
- 30. Mandal S, Suh ES, Harding R, Vaughan-France A, Ramsay M, Connolly B, et al Nutrition and Exercise Rehabilitation in Obesity hypoventilation syndrome (NERO): a pilot randomised controlled trial. Thorax. 2018;73(1):62–9.
- 31. Kneidinger N, Gloeckl R, Schönheit-Kenn U, Milger K, Hitzl W, Behr J, et al Impact of nocturnal noninvasive ventilation on pulmonary rehabilitation in patients with end-stage lung disease awaiting lung transplantation. Respiration. 2018;95(3):161–8.
- 32. Porszasz J, Cao R, Morishige R, van Eykern LA, Stenzler A, Casaburi R. Physiologic effects of an ambulatory ventilation system in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;188(3):334–42.
- 33. Furlanetto KC, Pitta F. Oxygen therapy devices and portable ventilators for improved physical activity in daily life in patients with chronic respiratory disease. Expert Rev Med Devices. 2017;14(2):103–15.
- 34. Bajema A, Swinbourne AL, Gray M, Leicht AS. Effect of portable non-invasive ventilation & environmental conditions on everyday activities. Respir Physiol Neurobiol. 2017;243:55–9.
- 35. Brochard L. Pressure support ventilation. In: Tobin MJ. Principles and practice of mechanical ventilation. 2nd ed.New York: McGraw-Hill inc; 2006. pp. 221–50.
- 36. Navalesi P, Maggiore S. Positive End-Expiratory Pressure. In: Tobin MJ. Principles and practice of mechanical ventilation. 2nd ed.New York: McGraw-Hill inc; 2006. pp. 273–325.
- 37. Louvaris Z, Habazettl H, Asimakos A, Wagner H, Zakynthinos S, Wagner PD, et al Heterogeneity of blood flow and metabolism during exercise in patients with chronic obstructive pulmonary disease. Respir Physiol Neurobiol. 2017;237:42–50.
- 38. Borghi-Silva A, Oliveira CC, Carrascosa C, Maia J, Berton DC, Queiroga F Jr, et al Respiratory muscle unloading improves leg muscle oxygenation during exercise in patients with COPD. Thorax. 2008;63(10):910–5.
- 39. Babcock MA, Pegelow DF, Harms CA, Dempsey JA. Effects of respiratory muscle unloading on exercise-induced diaphragm fatigue. J Appl Physiol (1985). 2002;93(1):201–6.
- 40. Hannink JD, van Hees HW, Dekhuijzen PN, van Helvoort HA, Heijdra YF. Non-invasive ventilation abolishes the IL-6 response to exercise in muscle-wasted COPD patients: a pilot study. Scand J Med Sci Sports. 2014;24(1):136–43.
- 41. Kawazu T, Nakamura T, Moriki T, Kamijo YI, Nishimura Y, Kinoshita T, et al Aerobic exercise combined with noninvasive positive pressure ventilation increases serum Brain-Derived Neurotrophic Factor in healthy males. PM R. 2016;8(12):1136–41.
- 42. Borghi-Silva A, Reis MS, Mendes RG, Pantoni CB, Simões RP, Martins LE, et al Noninvasive ventilation acutely modifies heart rate variability in chronic obstructive pulmonary disease patients. Respir Med. 2008;102(8):1117–23.
- 43. Haarmann H, Folle J, Nguyen XP, Herrmann P, Heusser K, Hasenfuß G, et al Impact of non-invasive ventilation on sympathetic nerve activity in Chronic Obstructive Pulmonary Disease. Hai. 2017;195(1):69–75.
- 44. O’Donnell DE, Sanii R, Younes M. Improvement in exercise endurance in patients with chronic airflow limitation using continuous positive airway pressure. Am Rev Respir Dis. 1988;138(6):1510–4.
- 45. Petrof BJ, Calderini E, Gottfried SB. Effect of CPAP on respiratory effort and dyspnea during exercise in severe COPD. J Appl Physiol (1985). 1990;69(1):179–88.
- 46. Maltais F, Reissmann H, Gottfried SB. Pressure support reduces inspiratory effort and dyspnea during exercise in chronic airflow obstruction. Am J Respir Crit Care Med. 1995;151(4):1027–33.
- 47. Polkey MI, Hawkins P, Kyroussis D, Ellum SG, Sherwood R, Moxham J. Inspiratory pressure support prolongs exercise induced lactataemia in severe COPD. Thorax. 2000;55(7):547–9.
- 48. Rodrigues MK, Oliveira MF, Soares A, Treptow E, Neder JA. Additive effects of non-invasive ventilation to hyperoxia on cerebral oxygenation in COPD patients with exercise-related O2 desaturation. Clin Physiol Funct Imaging. 2013;33(4):274–81.
- 49. Younes M. Proportional assist ventilation. In: Tobin MJ. Principles and practice of mechanical ventilation. 2nd ed.New York: McGraw-Hill inc; 2006. pp. 335–64.
- 50. Bianchi L, Foglio K, Pagani M, Vitacca M, Rossi A, Ambrosino N. Effects of proportional assist ventilation on exercise tolerance in COPD patients with chronic hypercapnia. Eur Respir J. 1998;11(2):422–7.
- 51. Carrascossa CR, Oliveira CC, Borghi-Silva A, Ferreira EM, Maya J, Queiroga F Jr, et al Haemodynamic effects of proportional assist ventilation during high-intensity exercise in patients with chronic obstructive pulmonary disease. Respirology. 2010;15(8):1185–91.
- 52. Bianchi L, Foglio K, Porta R, Baiardi R, Vitacca M, Ambrosino N. Lack of additional effect of adjunct of assisted ventilation to pulmonary rehabilitation in mild COPD patients. Respir Med. 2002;96(5):359–67.
- 53. Hawkins P, Johnson LC, Nikoletou D, Hamnegård CH, Sherwood R, Polkey MI, et al Proportional assist ventilation as an aid to exercise training in severe chronic obstructive pulmonary disease. Thorax. 2002;57(10):853–9.
- 54. Márquez-Martín E, Ruiz FO, Ramos PC, López-Campos JL, Azcona BV, Cortés EB. Randomized trial of non-invasive ventilation combined with exercise training in patients with chronic hypercapnic failure due to chronic obstructive pulmonary disease. Respir Med. 2014;108(12):1741–51.
- 55. van ’t Hul A. Van’ t Hul A, Gosselink R, Hollander P, Postmus P, Kwakkel G: training with inspiratory pressure support in patients with severe COPD. Eur Respir J. 2006;27(1):65–72.
- 56. Toledo A, Borghi-Silva A, Sampaio LM, Ribeiro KP, Baldissera V, Costa D. The impact of noninvasive ventilation during the physical training in patients with moderate-to-severe chronic obstructive pulmonary disease (COPD). Clinics (São Paulo). 2007;62(2):113–20.
- 57. Reuveny R, Ben-Dov I, Gaides M, Reichert N. Ventilatory support during training improves training benefit in severe chronic airway obstruction. Isr Med Assoc J. 2005;7(3):151–5.
- 58. Johnson JE, Gavin DJ, Adams-Dramiga S. Effects of training with heliox and noninvasive positive pressure ventilation on exercise ability in patients with severe COPD. Chest. 2002;122(2):464–72.
- 59. Zhou LQ, Li XY, Li Y, Guo BP, Guan LL, Chen X, et al [Inspiratory muscle training followed by non-invasive positive pressure ventilation in patients with severe chronic obstructive pulmonary disease: a randomized controlled trial]. Nan Fang Yi Ke Da Xue Xue Bao. 2016;36(8):1069–74.
- 60. Menadue C, Piper AJ, van ’t Hul AJ, Wong KK. Non-invasive ventilation during exercise training for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014;5(5):CD007714.
- 61. Ricci C, Terzoni S, Gaeta M, Sorgente A, Destrebecq A, Gigliotti F. Physical training and noninvasive ventilation in COPD patients: a meta-analysis. Respir Care. 2014;59(5):709–17.
- 62. Vitacca M, Kaymaz D, Lanini B, Vagheggini G, Ergün P, Gigliotti F, et al Non-invasive ventilation during cycle exercise training in patients with chronic respiratory failure on long-term ventilatory support: A randomized controlled trial. Respirology. 2018;23(2):182–9.
- 63. Duiverman ML, Maagh P, Magnet FS, Schmoor C, Arellano-Maric MP, Meissner A, et al Impact of High-Intensity-NIV on the heart in stable COPD: a randomised cross-over pilot study. Respir Res. 2017;18(1):76.
- 64. Ambrosino N, Nava S, Torbicki A, Riccardi G, Fracchia C, Opasich C, et al Haemodynamic effects of pressure support and PEEP ventilation by nasal route in patients with stable chronic obstructive pulmonary disease. Thorax. 1993;48(5):523–8.
- 65. Oliveira CC, Carrascosa CR, Borghi-Silva A, Berton DC, Queiroga F Jr, Ferreira EM, et al Influence of respiratory pressure support on hemodynamics and exercise tolerance in patients with COPD. Eur J Appl Physiol. 2010;109(4):681–9.
- 66. Ou YE, Lin ZM, Hua DM, Jiang Y, Huo YT, Luo Q, et al Evaluation of carbon dioxide rebreathing during exercise assisted by noninvasive ventilation with plateau exhalation valve. Int J Chron Obstruct Pulmon Dis. 2017;12:291–8.
- 67. Griffo R, Spanevello A, Temporelli PL, Faggiano P, Carone M, Magni G, et alSUSPIRIUM Investigators. Frequent coexistence of chronic heart failure and chronic obstructive pulmonary disease in respiratory and cardiac outpatients: evidence from SUSPIRIUM, a multicentre Italian survey. Eur J Prev Cardiol. 2017;24(6):567–76.
- 68. Ambrosino N. Assisted ventilation as an aid to exercise training: a mechanical doping?Eur Respir J. 2006;27(1):3–5.
- 69. Ambrosino N, Vitacca M, Dreher M, Isetta V, Montserrat JM, Tonia T, et alERS Tele-Monitoring of Ventilator-Dependent Patients Task Force. Tele-monitoring of ventilator-dependent patients: a European Respiratory Society Statement. Eur Respir J. 2016;48(3):648–63.
- 70. Vitacca M, Bianchi L, Guerra A, Fracchia C, Spanevello A, Balbi B, et al Tele-assistance in chronic respiratory failure patients: a randomised clinical trial. Eur Respir J. 2009;33(2):411–8.
- 71. Romer LM, Polkey MI. Exercise-induced respiratory muscle fatigue: implications for performance. J Appl Physiol (1985). 2008;104(3):879–88.
- 72. Akoumianaki E, Dousse N, Lyazidi A, Lefebvre JC, Graf S, Cordioli RL, et al Can proportional ventilation modes facilitate exercise in critically ill patients? A physiological cross-over study : pressure support versus proportional ventilation during lower limb exercise in ventilated critically ill patients. Ann Intensive Care. 2017;7(1):64.
- 73. Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, et al Neural control of mechanical ventilation in respiratory failure. Nat Med. 1999;5(12):1433–6.
- 74. Bräunlich J, Köhler M, Wirtz H. Nasal highflow improves ventilation in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:1077–85.
- 75. Biselli PJ, Kirkness JP, Grote L, Fricke K, Schwartz AR, Smith P, et al Nasal high-flow therapy reduces work of breathing compared with oxygen during sleep in COPD and smoking controls: a prospective observational study. J Appl Physiol (1985). 2017;122(1):82–8.
- 76. Fraser JF, Spooner AJ, Dunster KR, Anstey CM, Corley A. Nasal high flow oxygen therapy in patients with COPD reduces respiratory rate and tissue carbon dioxide while increasing tidal and end-expiratory lung volumes: a randomised crossover trial. Thorax. 2016;71(8):759–61.
- 77. Cirio S, Piran M, Vitacca M, Piaggi G, Ceriana P, Prazzoli M, et al Effects of heated and humidified high flow gases during high-intensity constant-load exercise on severe COPD patients with ventilatory limitation. Respir Med. 2016;118:128–32.
- 78. Dellacà RL, Santus P, Aliverti A, Stevenson N, Centanni S, Macklem PT, et al Detection of expiratory flow limitation in COPD using the forced oscillation technique. Eur Respir J. 2004;23(2):232–40.