In adults at risk for contrast-induced nephropathy, no prophylactic hydration was noninferior to hydration
- Wagner, Brent MD, FACP, FASN
Question
In adults at risk for contrast-induced nephropathy (CIN), is no prophylactic hydration noninferior to guideline-based, standard prophylactic hydration for preventing CIN?
Methods
Design
Randomized controlled trial (A MAstricht Contrast-Induced Nephropathy Guideline [AMACING] trial). ClinicalTrials.gov NCT02106234.
Allocation
Concealed.
Blinding
Blinded (laboratory personnel).
Follow-up period
35 days.
Setting
Maastricht University Medical Centre, Maastricht, The Netherlands.
Patients
660 adults ≥ 18 years of age (mean age 72 y, 62% men) who were referred for an elective diagnostic or interventional procedure that required intravascular iodinated contrast material and had high risk for CIN (estimated glomerular filtration rate [eGFR] 45 to 59 mL/min/1.73 m2 and either diabetes, ≥ 2 of age > 75 years, anemia [hematocrit < 0.39 L/L for men and < 0.36 L/L for women], cardiovascular disease, or use of nonsteroidal antiinflammatory drugs or diuretic nephrotoxic medication); or eGFR 30 to 45 mL/min/1.73 m2; or multiple myeloma or lymphoplasmacytic lymphoma with small chain proteinuria. Exclusion criteria included renal replacement therapy, emergency procedures, intensive care admission, or no referral for IV hydration.
Intervention
No prophylactic hydration (n = 332) or guideline-based, standard prophylactic IV hydration with a standard (0.9% NaCl, 3 to 4 mL/kg/h, 4 h before and after contrast administration) or long protocol (0.9% NaCl, 1 mL/kg/h for 12 h before and after contrast administration) (n = 328). Contrast medium for all patients was prewarmed intravascular iopromide, 300 mg iodine/mL.
Outcomes
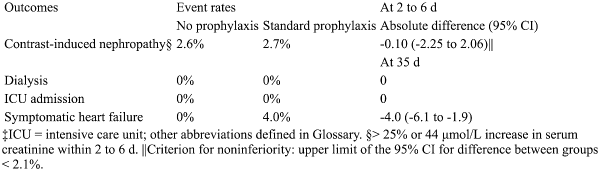
Primary outcome was CIN (> 25% or > 44 μmol/L increase in serum creatinine within 2 to 6 d). Secondary outcomes included major adverse events (including dialysis, intensive care unit admission, and such complications of prophylactic IV hydration as symptomatic heart failure). Prespecified subgroup analysis was done for diabetes vs no diabetes, eGFR < 45 vs ≥ 45 mL/min/1.73 m2, IV vs intraarterial contrast administration route, and interventional vs diagnostic procedure.
Patient follow-up
91% (intention-to-treat).
Main results
The main results are in the Table. There were no differences in CIN between subgroups (P for interaction > 0.05 for all analyses). Groups did not differ for major adverse events except for symptomatic heart failure (Table).
Conclusion
In adults at risk for contrast-induced nephropathy (CIN), no prophylaxis was noninferior to prophylactic hydration for prevention of CIN.