Introduction
The tricuspid valve was historically considered to have limited clinical significance compared to the left-sided valves and has been coined the “forgotten” or “neglected” valve. This concept has gradually changed [], and over the last decade, there are accumulating data to suggest that tricuspid regurgitation (TR) has a significant clinical impact [–]. Development of percutaneous interventions for TR has also attracted attention to this valve and its clinical significance. Data suggest that severe TR is associated with worse clinical outcome independent of left and right ventricular (RV) function and pulmonary hypertension [, ]. TR was shown to have prognostic significance in patients with reduced [] as well as preserved left ventricular ejection fraction (LVEF) []. However, the clinical importance of the full range of TR severities in a large cohort and particularity mild TR is sparse, and specific data regarding the clinical characteristics of these patients are limited. The aim of the present study was to assess the clinical characteristics of subjects with TR and the impact of graded TR severity on clinical outcome, with particular emphasis on subjects with mild TR.
Methods
All consecutive subjects that underwent echocardiography examinations recorded in the echocardiography database of a university-affiliated laboratory during a 5-year period (2011–2016) were retrieved for analysis. Medical diagnosis of the subjects (ICD-9 coding) was retrieved from the electronic medical record of the subjects in a university-affiliated hospital. Echocardiographic measurements were performed according to standard recommendations of the American Society of Echocardiography (ASE) and the European Association of Cardiovascular Imaging (EACVI) []. LVEF was measured at rest and was assessed either by the Simpson biplane method or qualitatively. Organic TR was defined as TR in association with any congenital defect or primary abnormality of the valvular leaflets. Severity of TR was assessed according to an integrative assessment of multiple parameters including color jet area, width of vena contracta, density of continuous wave Doppler signal, hepatic flow pattern, leaflet coaptation, as well as right atrial (RA) and RV size, as recommended by the ASE and EACVI [, ]. TR was graded into mild, moderate, severe, and massive TR according to the EACVI grading system. Mild-moderate TR was grouped with mild TR, and moderate-severe TR was grouped with moderate TR. “Free” and torrential TR was considered as massive TR for the purposes of this analysis. RA pressure was estimated from the assessment of inferior vena cava width and collapsibility with inspiration. RV function was assessed semi-quantitatively using assessments including fractional area change, tricuspid annular plane systolic excursion, and tissue Doppler S wave. Reduced RV function was defined as any reduction in systolic function. RV chamber size was determined by measuring the RV internal diameter in the apical 4 chamber, in accordance with guidelines. RV dilatation was defined as any enlargement of the RV. Data on mortality were retrieved from the National Census Bureau and included mortality up to February 2022. All hospitalizations in the cardiac intensive care and cardiology department were retrieved for analysis of cardiovascular hospitalizations. The Institutional Ethical Committee for Human Studies of the university-affiliated hospital approved the study protocol (number 0043-22). Informed consent was waived by the Ethical Committee as the study was observational and data were recorded retrospectively.
SPSS version 17.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. Comparison of the clinical characteristics was performed using the Kruskal-Wallis test for continuous variables and the χ2 test for categorical variables. For assessment of the total number of comorbidities, diagnoses included heart failure, hypertension, diabetes mellitus, ischemic heart disease, atrial fibrillation, chronic renal failure, and prior stroke. Age was also included and counted as 1 point for subjects older than 65 years and 2 points above 75 years. Comorbidities and additional echocardiographic pathologies included pacemaker\defibrillator implantation, pulmonary hypertension (TR velocity >2.8 m/s), severe mitral regurgitation, LVEF <50%, reduced RV function, and diastolic dysfunction (e’ <10). Survival was analyzed per subject, using the first echocardiographic examination performed. Follow-up time was calculated using Kaplan-Meier estimate of potential follow-up []. Kaplan-Meier curves, with the log-rank test, were used to compare survival according to TR severity. Multivariable Cox proportional hazards regression analysis was used to evaluate independent variables associated with survival. Variables included in the multivariable Cox regression analysis incorporated age, sex, and other clinically significant variables on univariable analysis. As the massive TR category consisted of a relatively limited cohort of subjects, it was grouped with severe TR for the Cox regression analysis. Proportionality assumptions of the Cox regression models were evaluated by log-log survival curves and with the use of Schoenfeld residuals. An evaluation of the existence of confounding or interactive effects was made between variables and their possible collinearity. A p value of <0.05 was considered statistically significant.
Results
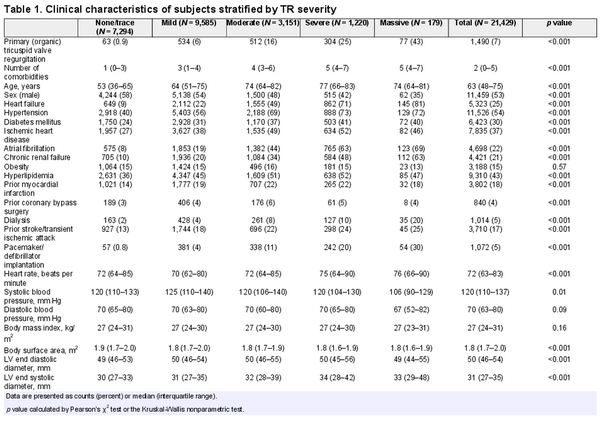
A total of 21,429 subjects were included in the analysis. 9,585 (45%) subjects had mild TR, 3,151 (15%) subjects had moderate TR, 1,220 (5.7%) had severe TR, and 179 (0.8%) had massive TR. Table 1 provides the clinical characteristics and echocardiographic measurements of the subjects stratified according to the severity of the TR. Primary organic TR was evident in 7% of the subjects with increasing prevalence of primary disease with increasing TR severity. The most common etiology of the primary TR was prolapse/flail leaflets. Subjects with significant TR were significantly older with a higher proportion of women. The prevalence of heart failure increased significantly with the severity of the TR. There was a higher prevalence of hypertension, diabetes, ischemic heart disease, atrial fibrillation, prior stroke, and chronic renal failure including dialysis with TR severity. More subjects with TR had an implanted electrophysiology device (pacemaker/defibrillator). These subjects had increased LV mass and a higher incidence of reduced LV ejection fraction and severe mitral regurgitation. Indices of diastolic dysfunction (low mitral e’ annulus velocity or elevated mitral E/e’ ratio) were more prevalent with TR severity. Peak TR gradient was also higher. As expected, there was increasing RA and RV dilatation and reduction in RV systolic function with severity of the TR. A significant increase in the number of comorbidities, additional echocardiographic pathologies, and presence of implantable devices were noted with increasing TR severity (Table 1; Fig. 1).
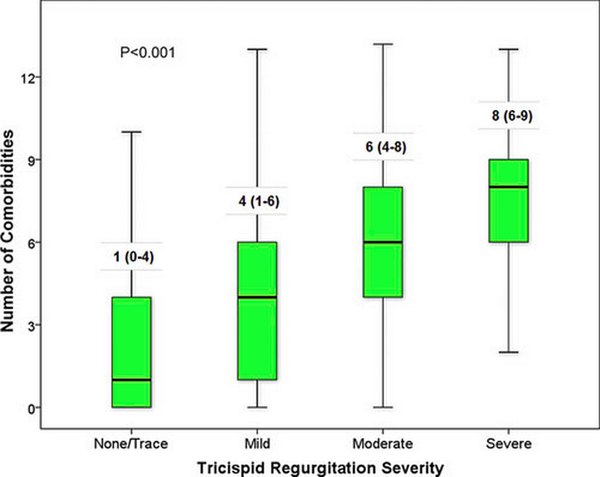
Fig. 1
Box plot of the number of comorbidities, echocardiographic pathologies, and implantable devices stratified according to the severity of TR. Kruskal-Wallis test: p < 0.0001.
Clinical Outcome
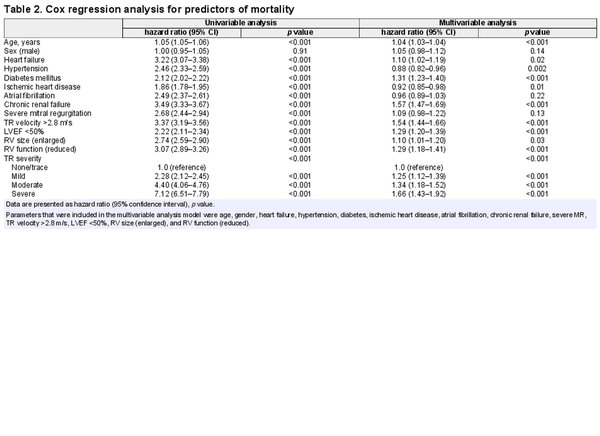
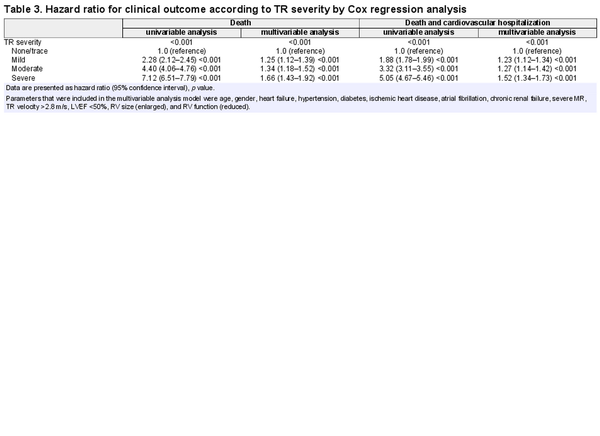
A total of 6,225 patients (29%) died at a median follow-up duration of 3,184 days. Survival was significantly lower with increasing TR severity. Kaplan-Meier analysis (Fig. 2a) demonstrated that prognosis was worse with increasing severity of the TR and this was graded and incremental with TR severity. Cox regression analysis after adjustment for age, sex, and other significant clinical variables including heart failure demonstrated that all three levels of TR severity were independent incremental predictors of mortality (Table 2). Subjects with severe TR had a 66% increased mortality rate compared to subjects with minimal TR (HR 1.66 CI: 1.43–1.92, p < 0.001). Importantly, even mild TR (HR 1.25, 95% CI: 1.12–1.39, p < 0.001) as well as moderate TR (HR 1.34, 95% CI: 1.18–1.52, p < 0.001) were independent predictors of increased mortality (Table 2). Cardiovascular hospitalizations were also significantly increased incrementally with TR severity grade (Fig. 2b; Table 3). Adjustment for significant variables demonstrated that all three levels of TR severity were independent incremental predictors of cardiovascular hospitalization and mortality, for mild TR (HR 1.23, 95% CI: 1.12–1.34, p < 0.001), moderate TR (HR 1.27, 95% CI: 1.14–1.42, p < 0.001), and severe TR (HR 1.52, 95% CI: 1.34–1.73, p < 0.001). No interaction was seen between TR severity and RV failure, reduced LV ejection fraction, or increased pulmonary pressure, suggesting that the increased mortality was present in all subgroups.
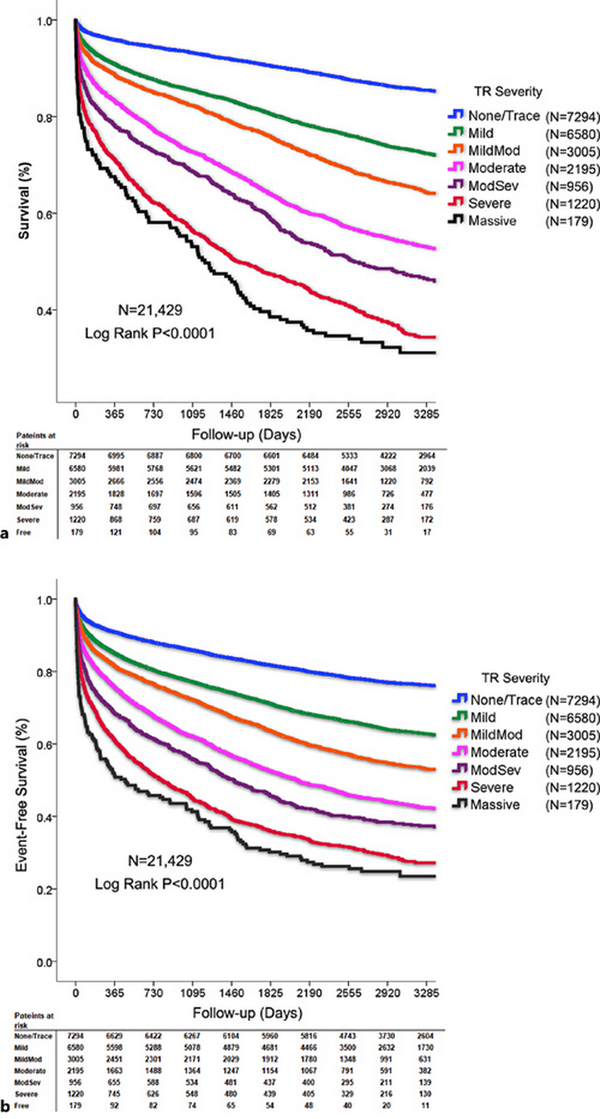
Fig. 2
Kaplan-Meier survival analysis according to TR. a Survival was significantly lower with increasing TR severity (log-rank, p < 0.0001). b Event-free survival including cardiovascular hospitalization or mortality was significantly lower with increasing TR severity (log-rank, p < 0.0001).
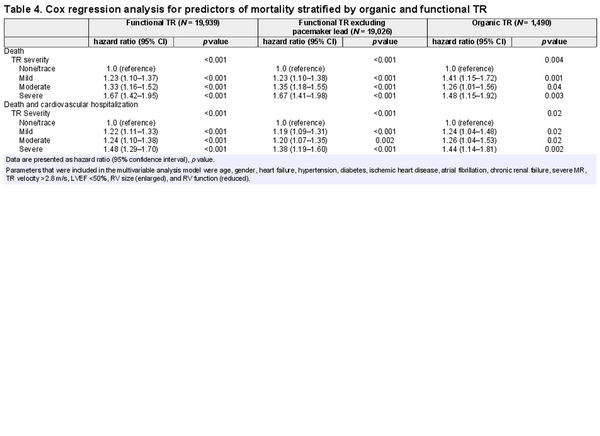
Analysis of functional TR and organic TR separately demonstrated that in both subsets, survival was significantly associated with TR severity as well as cardiovascular hospitalization and mortality (Table 4). Mild and moderate TR were significant predictors of a worse clinical outcome in both subsets. We also analyzed subjects with functional TR with the exclusion of subjects with a pacemaker lead (N = 19,026, Table 4). There was a graded independent increase in mortality (mild TR, HR 1.23, 95% CI: 1.10–1.38, p < 0.001) as well as mortality and cardiovascular hospitalization with TR severity. Analysis of subjects with functional TR with the exclusion of pacemaker lead, pulmonary hypertension, RV failure, severe MR, and heart failure (N = 6,290) demonstrated that isolated functional mild TR was an independent predictor of mortality (N = 3,852; HR 1.27, 95% CI: 1.10–1.46, p < 0.001) as well as death and cardiovascular hospitalization.
Given the potential for TR to exhibit variability on repeat examination due to changes in clinical status and loading conditions, we analyzed the effect of TR severity on mortality in a subset of cohort with a repeat echocardiography study available. Data were available in 5,479 of the subjects (26%), with a median time of 273 days from the baseline study. The repeat examination revealed some variability in TR severity. Nevertheless, TR severity was associated with increased mortality. Cox regression analysis demonstrated an incremental increase in mortality with TR severity including mild TR. Mild TR was an independent predictor of mortality compared to subjects with none or trivial TR (HR 1.36, 95% CI: 1.20–1.54, p < 0.001).
Discussion
The present study demonstrates that the majority of subjects with TR have functional TR and that TR severity has significant prognostic implications. Increasing severity of TR was independently and incrementally associated with mortality as well as with death and cardiovascular hospitalizations. Even mild TR had prognostic significance. In addition, severity of TR was strongly associated with numerous detrimental clinical characteristics including older age, cardiovascular risk factors, and comorbidities such as AF and CRF.
TR severity was a predictor of increased mortality and cardiovascular hospitalizations even after adjustment for numerous clinical and echocardiographic parameters, suggesting that TR severity is an independent marker of a poor prognosis. The results were demonstrated in subjects with functional TR and with organic TR. These findings are consistent with previously published data [–]; the present study further substantiates this finding with data from a large real-world cohort.
However, the present study also reveals the interesting and novel finding that moderate and even mild TR have independent significant prognostic value and are predictive of increased mortality as well as cardiovascular hospitalizations. This finding has been suggested by previous studies that consistently demonstrate an incremental increase in mortality with TR severity, although most did not reach statistical significance perhaps due to size limitations after adjustment for clinical variables []. This finding was noted in a large study in patients with heart failure with reduced EF and functional TR [] and in a recent meta-analysis []. The meta-analysis demonstrated that even mild or moderate TR were associated with elevated mortality risk with incrementally higher mortality rates, results similar to the present study. A very recent study demonstrated in a large cohort that even mild TR was independently associated with increased mortality []. This study examined a limited number of clinical variables; our study confirms their findings while adjusting for a larger number of clinical variables.
It remains speculative why mild or even moderate TR should have prognostic significance as these valve abnormalities generally do not have a substantial hemodynamic impact. One possible explanation suggested by the authors of the meta-analysis is that any degree of TR may reflect the progressive nature of TR severity, as TR progression has been associated with worse outcomes. In addition, the increased mortality rate in milder severities of TR raises the question to how accurate the quantification of TR by echocardiography is by the current semi-quantitative and qualitative techniques. Furthermore, variations in clinical status and loading conditions can result in fluctuations in the severity of TR and may lead to an underestimation of its severity. It is possible that the TR severity may be systematically underestimated in milder severities and emphasizes the importance of accurate assessment of TR severity as this conveys prognostic significance.
The present study suggests that the prognostic significance of TR, at least when mild, is not related to hemodynamic impairment caused by the valve pathology but is mainly related to the fact that TR is associated with numerous comorbidities in these subjects and is a marker of a higher disease burden. Functional TR often results from RV dilatation leading to tethering of leaflets or tricuspid annular shape changes including dilatation, increased planarity, and increased circularity []. These changes may also result from atrial enlargement and atrial myopathy, or subtle changes in RV geometry. As such, even mild TR may harbinger right-sided dysfunction. In the present study, TR severity was consistently associated with numerous detrimental clinical attributes and many echocardiographic abnormalities which may be either a cause or a consequence of the TR severity. Assessing the total number of comorbidities and associated pathologies demonstrated that as TR severity increased, patients had increasing number of clinical issues. The large size of the present study and the high prevalence of clinical comorbidities in this hospital-based population underscores these findings. As the vast majority of subjects with TR have functional disease, this finding is not surprising. These findings emphasize the fact that while severe TR in itself is detrimental and can cause a reduced outcome and, if possible, should be treated at the appropriate time to prevent complications, TR is also a marker of a sicker patient with a higher disease burden. This important finding has clear clinical implications and should be taken into account when assessing these subjects for interventions.
There are several limitations in the present study. The study was a retrospective echocardiographic study based on a clinical laboratory database. Clinical data on background disease were accessed from electronic medical records with the inherent limitations of such data. In addition, we cannot exclude other clinical issues not apparent in the present data that may have an impact on the results. Data on medications and laboratory data including natriuretic peptides were not available. The study cohort was based on subjects undergoing an echocardiography study in a university hospital setting and therefore may not be generalizable to a community population.
Conclusions
TR is associated with older and sicker patients with a higher disease burden. Even mild TR severity is an independent predictor of a worse clinical outcome. TR should be considered not only as valvular pathology but also as a marker of a subject with clinically advanced cardiovascular disease.
Statement of Ethics
The research was conducted according to internationally accepted ethical standards for research practice and reporting. The Institutional Committee for Human Studies of Hadassah Medical Center approved the study protocol, approval number 0043-22. Patient consent was waived by the Institutional Review Board due to the retrospective observational design of the study with usage of deidentified anonymous data.
Conflict of Interest Statement
The authors declare no conflict of interest.
Funding Sources
The authors received no specific funding for this work.
Author Contributions
Conceptualization: I.G., D.R.S, and D.L.; methodology, formal analysis, writing, and original draft preparation: I.G. and D.L.; investigation, D.R.S; resources, G.E.G.; writing, review, and editing, D.L., D.R.S, G.E.G., O.A., and I.G.; and supervision: I.G. and D.P. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
The data of this study are available from Hadassah Medical Center but restrictions apply to the availability of these data, which were used under the license for the current study and are not publicly available. Further inquiries can be directed to the corresponding author.
References
- 1. Bruce CJ, Connolly HM Right-sided valve disease deserves a little more respect Circulation 2009 May 26 119 20 2726–34
- 2. Nath J, Foster E, Heidenreich PA Impact of tricuspid regurgitation on long-term survival J Am Coll Cardiol 2004 Feb 4 43 3 405–9
- 3. Bar N, Schwartz LA, Biner S, Aviram G, Ingbir M, Nachmany I, et al Clinical outcome of isolated tricuspid regurgitation in patients with preserved left ventricular ejection fraction and pulmonary hypertension J Am Soc Echocardiogr 2018 Jan 31 1 34–41
- 4. Benfari G, Antoine C, Miller WL, Thapa P, Topilsky Y, Rossi A, et al Excess mortality associated with functional tricuspid regurgitation complicating heart failure with reduced ejection fraction Circulation 2019 Jul 16 140 3 196–206
- 5. Wang N, Fulcher J, Abeysuriya N, McGrady M, Wilcox I, Celermajer D, et al Tricuspid regurgitation is associated with increased mortality independent of pulmonary pressures and right heart failure: a systematic review and meta-analysis Eur Heart J 2019 Feb 1 40 5 476–84
- 6. Chorin E, Rozenbaum Z, Topilsky Y, Konigstein M, Ziv-Baran T, Richert E, et al Tricuspid regurgitation and long-term clinical outcomes Eur Heart J Cardiovasc Imaging 2020 Feb 1 21 2 157–65
- 7. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging Eur Heart J Cardiovasc Imaging 2015 Mar 16 3 233–70
- 8. Lancellotti P, Tribouilloy C, Hagendorff A, Popescu BA, Edvardsen T, Pierard LA, et al Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging Eur Heart J Cardiovasc Imaging 2013 Jul 14 7 611–44
- 9. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, et al 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American college of cardiology/American heart association task force on practice guidelines J Am Coll Cardiol 2014 Jun 10 63 22 e57–185
- 10. Schemper M, Smith TL A note on quantifying follow-up in studies of failure time Control Clin Trials 1996 Aug 17 4 343–6
- 11. Offen S, Playford D, Strange G, Stewart S, Celermajer DS Adverse prognostic impact of even mild or moderate tricuspid regurgitation: insights from the national echocardiography database of Australia J Am Soc Echocardiogr 2022 Aug 35 8 810–7
- 12. Ton-Nu TT, Levine RA, Handschumacher MD, Dorer DJ, Yosefy C, Fan D, et al Geometric determinants of functional tricuspid regurgitation: insights from 3-dimensional echocardiography Circulation 2006 Jul 11 114 2 143–9