Introduction
Parkinson's disease is a neurodegenerative disease characterized by the progressive loss of dopaminergic neurons. The resulting movement disorder causes not only a combination of bradykinesia, tremor and rigidity but also postural changes. Among the postural changes, a forward-stooped posture with flexion of the cervical and thoracic spine is common., Forward stooped posture can cause significant discomfort, contributes to an increased risk of falls, and reduces the quality of life.,– Treatment options are limited as postural changes (like other axial symptoms such as postural instability and gait disorders) do not respond well to pharmacological therapy.,,– Deep brain stimulation appears to have some efficacy in stooped posture in small studies,, but the lack of randomized controlled trials of deep brain stimulation for stooped posture, strict selection criteria, its invasive nature, and its limited availability at specialized centres limit its use for the general patient population.
Among the non-invasive techniques, exercise and physical therapy are widely in use and are among the treatments of choice for Parkinson's disease patients with a stooped posture. Four randomized trials, one controlled trial and two case series have already demonstrated that targeted physical exercise significantly corrects forward postural abnormalities in Parkinson's disease.– Previous research observed an average improvement of 8°–23° of the forward trunk flexion after 3 or 4 weeks of intervention, respectively. One study reported that eight weeks of aquatic physiotherapy reduced forward neck flexion by 65°. Although alternative sports such as yoga and pilates, which provide low-level evidence (owing to the small sample size) on the improvement of posture in healthy controls,– can have beneficial effects on the cardinal motor symptoms and impaired balance in Parkinson's disease,– their influence on the stopped posture in Parkinson's disease has not yet been studied. No other study has ever investigated the influence of sport climbing on posture in Parkinson's disease patients specifically.
In our recent randomized controlled trial on sport climbing, we proved that sport climbing is a safe, feasible and engaging activity for Parkinson's disease patients and is also highly effective in reducing motor symptoms of Parkinson's disease. The sport climbing trial included a pre-planned secondary analysis of the posture. We hypothesized that climbing improves posture due to its holistic effects on the musculoskeletal system: it strengthens the shoulder girdle and trunk muscles, increases hip and shoulder flexibility and forces the patient to recline the head repeatedly and stretch the torso and limbs.– Additionally, we examine the correlations between posture and non-motor symptoms of Parkinson's disease as well as the influence of age on posture in our cohort, given that forward-stooped posture correlated with age in previous observations.– We also sought to identify a possible effect of body mass index on the forward-stooped posture in Parkinson's disease, as body weight seemed to influence the posture in a healthy population.
In summary, effective therapeutic options to improve postural abnormalities in Parkinson's disease are rare. Physical activity is among the most promising option, is widely used, non-invasive and low-risk., Sport climbing could counteract postural deformities by increasing upper body strength and flexibility in relevant joints, which is the underlying hypothesis of the study.
Methods
This study is part of the Climb up! Head up! project, which was approved by the ethical committee of the Medical University of Vienna (No. 1774/2012), registered within the US National Library of Medicine (No: NCT04569981) and was performed according to the 1964 Declaration of Helsinki. All subjects provided written informed consent before being included in the trial.
The methods have been published in our recent publication. In brief, this was a randomized semi-blind trial (unblinded patients, blinded assessors) of 12 weeks duration, investigating an intervention group, ‘sport climbing group’ and a control group, ‘unsupervised training group’. Using a table-generated permuted block randomization approach, we randomized the patients to one of two groups of equal sample size. Sport climbers followed a 12-week, 90 min/week supervised top-rope sport climbing course in an indoor climbing gym, with an instructor-to-patient ratio of 1: 3-4. Only certified climbing trainers served as instructors. The participants received lessons in top-rope climbing, the most common style at indoor climbing walls. Top-rope climbing involves a ‘belayer’, that is, a person standing on the ground securing the rope holding the climber. The participants were actively engaged throughout the whole 90 min, either as climbers or as belayers.
The unsupervised training group independently followed the ‘European Physiotherapy Guidelines for Parkinson's Disease’ and World Health Organization recommendations for an active lifestyle for 12 weeks., The recommendations advise patients to perform moderate aerobic physical activities for 150 min/per week, strength training twice a week and balance exercises three times per week., We instructed the patients to complete a training log and performed telephonic follow-up calls every 7–10 days. We discouraged changes in dopaminergic medication and deep brain stimulation settings throughout the study period wherever possible without compromising the patient's well-being; however, changes in both medication and DBS settings were allowed and did not constitute an exclusion criterion if they occurred during the study period.
We included patients with mild to moderate idiopathic Parkinson's disease (Hoehn & Yahr stage 2-3), diagnosed according to the UK Brain Bank criteria without prior climbing experience and recruited them between June 2018 and May 2019 from the Medical University of Vienna Movement Disorders Clinic. Patients were deemed ineligible for the trial if they had a history of stroke, severe orthopaedic problems, severe visual or hearing problems and significant cognitive impairment (Mini-Mental State Examination score <24).
The pre-specified secondary analysis examines the effect of sport climbing versus unsupervised physical exercise on posture and the association of posture with body mass index, age and non-motor symptoms of Parkinson's disease. All raters performing the clinical evaluation were blinded to the patient's group allocations. All assessments at baseline and after 12 weeks at the end of the intervention were performed in the patients’ best ON-state.
Analysis of the postural assessment was pre-specified as part of the sport climbing trial. The horizontal distance of the seventh cervical vertebra to the wall was measured using a digital caliper (Preciva 150 mm, measurement accuracy 0.01 mm). For this purpose, participants were instructed to stand upright with their back, sacrum and heels against a wall (see Figure 1).
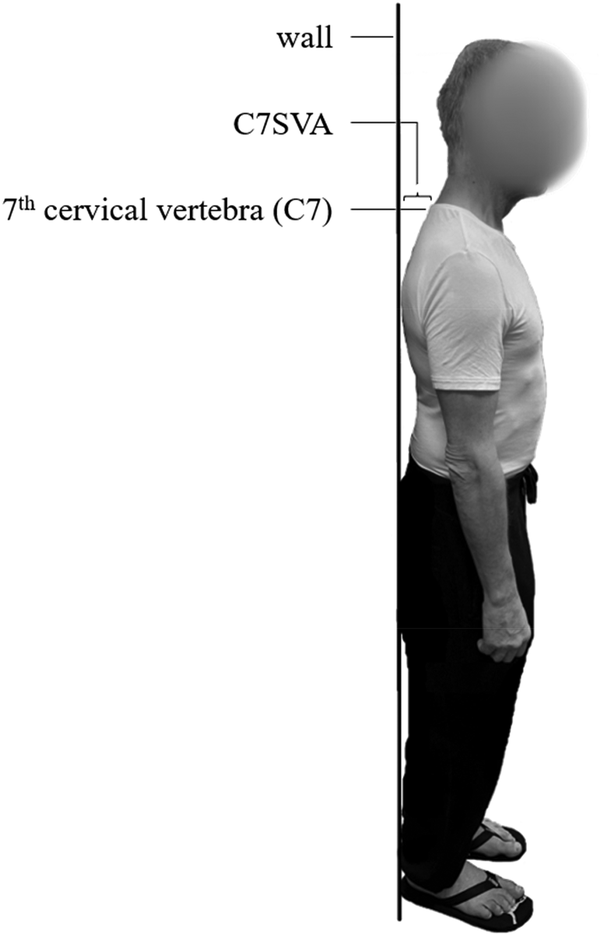
Figure 1
Definition of the C7 sagittal vertical axis. The C7 sagittal vertical axis (C7SVA) is defined as the horizontal distance of the seventh cervical vertebra (C7) to the wall. We measured the horizontal distance between the C7 and the wall using a digital caliper.
This test is a simple but highly reliable method to analyze posture in Parkinson's disease patients without the influence of a potentially confounding head position.
The motor symptoms of Parkinson's disease were assessed with the Movement Disorder Society-Sponsored Revision of the Unified Parkinson's Disease Rating Scale part III (including axial rigidity, posture, and postural stability) and the Hoehn & Yahr stage.
Health-related quality-of-life outcome measures were assessed at baseline and the endpoint with the following questionnaires: quality of life with the Parkinson's Disease Questionnaire, depression with the Beck Depression Inventory, fatigue with the Parkinson's Fatigue Scale, physical activity with the Physical Activity Scale for the Elderly, and fear of falling with the Falls Self-Efficacy Scale. Body mass index was calculated using the usual formula of dividing the patient's weight by their height in metres squared.
The horizontal distance of the seventh cervical vertebra to the wall at baseline and after 12 weeks was compared by group (sport climbing vs. unsupervised training). We then separately calculated absolute mean differences for each group between baseline and after 12 weeks with robust 95% confidence intervals. We formally tested for the influence of the group assignment on the horizontal distance of the seventh cervical vertebra to the wall using a linear regression model. The mean score of the horizontal distance of the seventh cervical vertebra to the wall after 12 weeks served as the dependent variable and the assignment to the intervention group as an indicator-covariate. We report both coefficients and P-values derived from the t-statistic of the covariate. Influencing factors on the posture were analyzed using multivariable logistic regression. A two-sided P-value below 0.05 was considered statistically significant. We used STATA 16 (Stata Corp, College Station, TX) for all analyses.
Sample size considerations were based on the effect of the intervention on the absolute difference in the horizontal distance of the seventh cervical vertebra to the wall before and after 12 weeks. We expected no effect (absolute difference of 0 cm) within the control group, with a standard deviation of 2 cm, based on previous experience. No previously published data was available on the estimated effect in the intervention group.
The available sample size of 48 subjects (24 per group) would show an effect of at least d = 0.73 with a power of 0.8 based on a probability of error of the first kind of 0.05. Given the aforementioned expected characteristics of the control group, this effect size corresponds to an absolute difference of at least 1.4 cm or larger for the intervention group.
Results
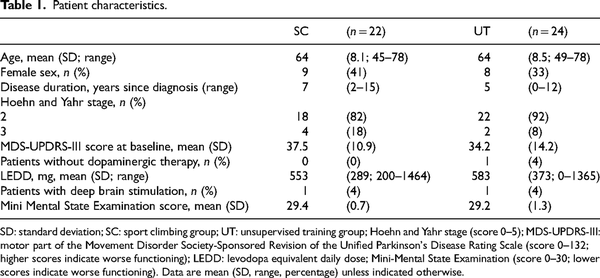
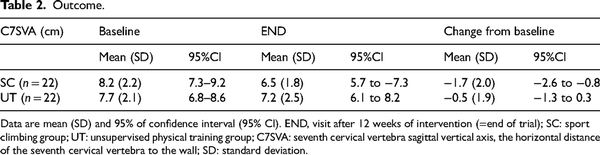
Forty-eight patients were included in the study. Of those, 46 were included in the analysis due to two dropouts in the sport climbing group (one due to unrelated health reasons and one due to a loss of interest in the study). The baseline characteristics are summarized in Table 1.
We achieved well-matched groups concerning baseline characteristics (see Table 1). With 99% course participation, adherence to the intervention was extremely high. We observed no adverse events during the study period, either in the sport climbing group or in the unsupervised training group.
At baseline, the mean horizontal distance of the seventh cervical vertebra to the wall did not significantly differ between the two groups (sport climbing group: 8.2 cm, 95%CI [7.3, 9.2], unsupervised training group: 7.7 cm; 95%CI [6.8, 8.6], mean difference 0.5 cm, 95%CI [−0.7, 1.8]).
According to the regression model, the change in the horizontal distance of the seventh cervical vertebra to the wall over 12 weeks was significantly associated with being part of the sport climbing group versus the unsupervised training group (coeff. 1.2; P = 0.044). This effect remained statistically significant when controlling for body mass index and age (coeff. 1.2; P = 0.048).
None of the health-related quality-of-life outcome scores (Parkinson's Disease Questionnaire, Beck Depression Inventory, Parkinson's Fatigue Scale, Physical Activity Scale for the Elderly, Falls Self-Efficacy Scale) were significantly associated with a change in the horizontal distance of the seventh cervical vertebra to the wall, neither in the intervention nor in the control group.
Within a period of 12 weeks, there was a significant improvement in the horizontal distance of the seventh cervical vertebra to the wall in the sport climbing group (−1.7 cm (95%CI [−2.6, −0.8]), but not in the unsupervised training group (−0.5 cm; 95%CI [−1.3, 0.2]; Table 2 and Figure 2).
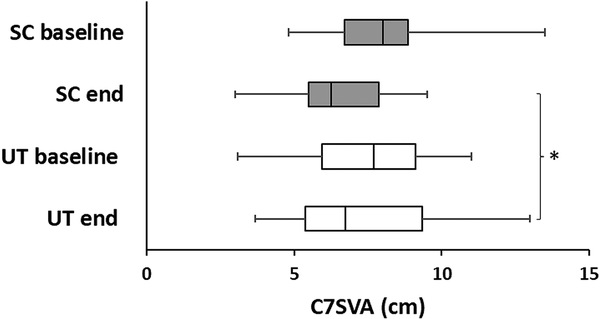
Figure 2
The effect of sport climbing on posture in Parkinson's disease. Boxplot of the horizontal distance of the seventh cervical vertebra (C7) to the wall (C7SVA) according to groups. Within each box, a vertical line indicates the median value; boxes range from the 25th to the 75th percentile of the value distribution of each group (interquartile range); horizontal lines indicate the minimum and maximum values, respectively. The figure shows the effect of climbing on the C7SVA at baseline and after 12 weeks compared to unsupervised physical training. Climbing significantly reduced the C7SVA after 12 weeks, while unsupervised physical training did not. SC, sport climbing group (green); UT, unsupervised physical training group (gray); C7SVA: C7 sagittal vertical axis distance; level of significance: *P < 0.05.
Discussion
In this secondary analysis of a randomized trial, we investigated the effect of sport climbing on the stooped posture of Parkinson's disease patients and demonstrated that sport climbing can potentially decrease the forward flexion of the cervical spine in PD patients. Posture improvement was observed in Parkinson's disease patients regardless of age or body mass index. The improvement of this biomechanical measure was not associated with an improvement of quality-of-life outcome measures.
Although we did not directly compare sport climbing to other sports in our study, we found similarities in previous observations that posture-specific physical therapy is a reliable method to improve postural symptoms of Parkinson's disease.–
Why does sport climbing improve posture in Parkinson's disease? The stooped posture found in Parkinson's disease is most often not a fixed deformity and is, therefore, amenable to corrective exercises. The strengthening effect sport climbing has on the back and shoulder girdle muscles,,– may enable the patient to yield a more upright posture.,
Another explanation for the effectiveness of sport climbing for Parkinson's disease could be found in the fact that sport climbing improves flexibility in the trunk and spine.,
With its high demands on movement planning and execution, climbing also trains spatial body awareness, a crucial component of maintaining and correcting posture.,, Proprioception is considered an essential element for neuromotor control of the upper body, and its improvement by visual or tactile feedback training is associated with a reduction in forward bent posture in Parkinson's disease.–,,
Rigidity is one of the contributing factors to postural abnormalities, and Parkinson's disease patients with a bradykinetic-rigid type suffer from postural abnormalities more often than patients with a tremor-dominant type. We have demonstrated that sport climbing reduces rigidity by 30% after 12 weeks; a finding that indicates another possible therapeutic effect of climbing on postural abnormalities.
In our study, the improvement in the biomechanical postural marker did not affect the subjective sensation of postural safety in the Falls Efficacy Scale. Stooped posture does influence postural stability by partially reducing stabilizing postural reflexes,; an improvement of stooped posture could, therefore, potentially improve postural stability. However, a forward bending posture is also used as a preventative stance to protect against falls. This could explain why a more upright stance did not decrease the participants’ fear of falling.
Because the C7SVA is a biomechanical measure that does not always affect patients’ subjective symptoms or quality of life, the conclusions that can be drawn from this study may be somewhat limited. The analysis could not be completed on all patients because of two dropouts, one due to a loss of interest in the intervention. This study did not record long-term results after the climbing training. The relatively small sample size of our study could limit its power. As with all studies on active interventions, a self-selection bias or participation might have occurred via the recruiting process, not only favouring patients with high intrinsic motivation but also means of participating in the study (i.e., transportation to and from the climbing hall and advantageous geographical location).
In summary, sport climbing improves forward-stooped posture in mild to moderate Parkinson's disease. A variety of mechanisms, including increased trunk muscle strength, stretching of shortened muscles, improvement of proprioception, and cognitive effects, may contribute to this effect.
Clinical messages
Sport climbing improves a biomechanical measure of posture in mild to moderately affected Parkinson's disease patients.
Acknowledgements
The authors want to express our sincere gratitude to all patients and climbing instructors of the Climbing Center’ Climb on Marswiese’ to support this project's enthusiastic participation and support. The authors would also like to thank the private donors who made the project possible and the Hilde-Ulrichs-Foundation for Parkinson's Research, Germany. LG was endorsed by the Marietta Blau grant from the Austrian Federal Ministry of Science and Research and the City of Vienna's scholarship. Finally, the authors would like to thank Mr Albert Robwein, MA, for his proofreading and language editing efforts.
Data availability statement The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declaration of conflicting interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs Agnes Langer https://orcid.org/0000-0001-9932-0474
ORCID iDs Jakob Gruber https://orcid.org/0000-0001-5915-618X
ORCID iDs Lucia Gassner https://orcid.org/0000-0002-7734-0682
References
- 1. Doherty KM, van de Warrenburg BP, Peralta MC, et al. Postural deformities in Parkinson's disease. Lancet Neurol 2011; 10: 538–549.
- 2. Ando Y, Fujimoto KI, Ikeda K, et al. Postural abnormality in Parkinson's disease: a large comparative study with general population. Mov Disord Clin Pract 2019; 6: 213–221.
- 3. Alwardat M, Schirinzi T, Di Lazzaro G, et al. The effect of postural deformities on back function and pain in patients with Parkinson's disease. NeuroRehabilitation 2019; 44: 419–424.
- 4. Jacobs JV, Dimitrova DM, Nutt JG, et al. Can stooped posture explain multidirectional postural instability in patients with Parkinson's disease? Exp Brain Res 2005; 166: 78–88.
- 5. Latt MD, Lord SR, Morris JG, et al. Clinical and physiological assessments for elucidating falls risk in Parkinson's disease. Mov Disord 2009; 24: 1280–1289.
- 6. Debû B, De Oliveira Godeiro C, Lino JC, et al. Managing gait, balance, and posture in Parkinson's disease. Curr Neurol Neurosci Rep 2018; 18: 23.
- 7. Maffoni M, Giardini A, Pierobon A, et al. Stigma experienced by Parkinson's disease patients: a descriptive review of qualitative studies. Parkinsons Dis 2017; 2017: 7203259.
- 8. Corallo F, De Cola MC, Lo Buono V, et al. Observational study of quality of life of Parkinson's patients and their caregivers. Psychogeriatrics 2017; 17: 97–102.
- 9. Moreira RC, Zonta MB, Araújo APS, et al. Quality of life in Parkinson's disease patients: progression markers of mild to moderate stages. Arq Neuropsiquiatr 2017; 75: 497–502.
- 10. Tinazzi M, Gandolfi M, Ceravolo R, et al. Postural abnormalities in Parkinson's disease: an epidemiological and clinical multicenter study. Mov Disord Clin Pract 2019; 6: 576–585.
- 11. Sharpe G, Macerollo A, Fabbri M, et al. Non-pharmacological treatment challenges in early Parkinson's disease for axial and cognitive symptoms: a mini review. Front Neurol 2020; 11: 576569.
- 12. Vorovenci RJ, Biundo R, Antonini A. Therapy-resistant symptoms in Parkinson's disease. J Neural Transm (Vienna) 2016; 123: 19–30.
- 13. Kataoka H, Ueno S. Can postural abnormality really respond to levodopa in Parkinson's disease? J Neurol Sci 2017; 377: 179–184.
- 14. Schlenstedt C, Gavriliuc O, Boße K, et al. The effect of medication and deep brain stimulation on posture in Parkinson's disease. Front Neurol 2019; 10: 1254.
- 15. Roediger J, Artusi CA, Romagnolo A, et al. Effect of subthalamic deep brain stimulation on posture in Parkinson's disease: a blind computerized analysis. Parkinsonism Relat Disord 2019; 62: 122–127.
- 16. Keus S, Munneke M, Graziano M, et al. European physiotherapy guideline for Parkinson’s disease. Developed with twenty European professional associations. Netherlands: KNGF/ParkinsonNet, 2014.
- 17. Gandolfi M, Tinazzi M, Magrinelli F, et al. Four-week trunk-specific exercise program decreases forward trunk flexion in Parkinson's disease: a single-blinded, randomized controlled trial. Parkinsonism Relat Disord 2019; 64: 268–274.
- 18. Morrone M, Miccinilli S, Bravi M, et al. Perceptive rehabilitation and trunk posture alignment in patients with Parkinson disease: a single blind randomized controlled trial. Eur J Phys Rehabil Med 2016; 52: 799–809.
- 19. Capecci M, Serpicelli C, Fiorentini L, et al. Postural rehabilitation and Kinesio taping for axial postural disorders in Parkinson's disease. Arch Phys Med Rehabil 2014; 95: 1067–1075.
- 20. Volpe D, Giantin MG, Manuela P, et al. Water-based vs. non-water-based physiotherapy for rehabilitation of postural deformities in Parkinson's disease: a randomized controlled pilot study. Clin Rehabil 2017; 31: 1107–1115.
- 21. Kawami Y, Marumoto K, Shiomi Y, et al. The effect of comprehensive physiotherapy-based rehabilitation on stooped posture in Parkinson's disease. J Phys Ther Sci 2018; 30: 1440–1445.
- 22. Greendale GA, Huang MH, Karlamangla AS, et al. Yoga decreases kyphosis in senior women and men with adult-onset hyperkyphosis: results of a randomized controlled trial. J Am Geriatr Soc 2009; 57: 1569–1579.
- 23. Lee SM, Lee CH, O'Sullivan D, et al. Clinical effectiveness of a Pilates treatment for forward head posture. J Phys Ther Sci 2016; 28: 2009–2013.
- 24. Hürer C, Angın E, Tüzün EH. Effectiveness of clinical pilates and home exercises in sagittal cervical disorientation: randomized controlled study. J Comp Eff Res 2021; 10: 365–380.
- 25. Ahearn EL, Greene A, Lasner A. Some effects of supplemental pilates training on the posture, strength, and flexibility of dancers 17 to 22 years of age. J Dance Med Sci 2018; 22: 192–202.
- 26. Ni M, Mooney K, Signorile JF. Controlled pilot study of the effects of power yoga in Parkinson's disease. Complement Ther Med 2016; 25: 126–131.
- 27. Deuel LM, Seeberger LC. Complementary therapies in Parkinson disease: a review of acupuncture, Tai Chi, Qi Gong, Yoga, and Cannabis. Neurotherapeutics 2020; 17: 1434–1455.
- 28. Suárez-Iglesias D, Miller KJ, Seijo-Martínez M, et al. Benefits of pilates in Parkinson's disease: a systematic review and meta-analysis. Medicina (Kaunas) 2019; 55(8): 476. https://doi.org/10.3390/medicina55080476
- 29. Langer A, Hasenauer S, Flotz A, et al. A randomised controlled trial on effectiveness and feasibility of sport climbing in Parkinson's disease. NPJ Parkinsons Dis 2021; 7: 49.
- 30. Buechter RB, Fechtelpeter D. Climbing for preventing and treating health problems: a systematic review of randomized controlled trials. Ger Med Sci 2011; 9: Doc19.
- 31. Muehlbauer T, Stuerchler M, Granacher U. Effects of climbing on core strength and mobility in adults. Int J Sports Med 2012; 33: 445–451.
- 32. MacKenzie R, Monaghan L, Masson RA, et al. Physical and physiological determinants of rock climbing. Int J Sports Physiol Perform 2020; 15: 168–179.
- 33. Aras D, Akalan C. Sport rock climbing: as a type of physical activity to improve health-related physical fitness parameters. J Sports Med Phys Fitness 2015; 56: 1304–1310.
- 34. Forsyth AL, Joshi RY, Canning CG, et al. Flexed posture in Parkinson disease: associations with nonmotor impairments and activity limitations. Phys Ther 2019; 99: 893–903.
- 35. Kashihara K, Imamura T. Clinical correlates of anterior and lateral flexion of the thoracolumbar spine and dropped head in patients with Parkinson's disease. Parkinsonism Relat Disord 2012; 18: 290–293.
- 36. Khlebtovsky A, Djaldetti R, Rodity Y, et al. Progression of postural changes in Parkinson's disease: quantitative assessment. J Neurol 2017; 264: 675–683.
- 37. Shaghayeghfard B, Ahmadi A, Maroufi N, et al. Evaluation of forward head posture insitting and standing positions. Eur Spine J 2016; 25: 3577–3582.
- 38. Kim J, Shin W. How to do random allocation (randomization). Clin Orthop Surg 2014; 6: 103–109.
- 39. Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 2020; 54: 1451–1462.
- 40. Domingos J, Keus SHJ, Dean J, et al. The European physiotherapy guideline for Parkinson's disease: implications for neurologists. J Parkinsons Dis 2018; 8: 499–502.
- 41. Peto V, Jenkinson C, Fitzpatrick R, et al. The development and validation of a short measure of functioning and well being for individuals with Parkinson's disease. Qual Life Res 1995; 4: 241–248.
- 42. Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry 1961; 4: 561–571.
- 43. Brown RG, Dittner A, Findley L, et al. The Parkinson fatigue scale. Parkinsonism Relat Disord 2005; 11: 49–55.
- 44. Washburn RA, Smith KW, Jette AM, et al. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol 1993; 46: 153–162.
- 45. StataCorp. Stata statistical software: release 16. College Station, TX: StataCorp LLC., 2019.
- 46. van Wegen EEH, de Goede CJT, Kwakkel G, et al. Sensor assisted self-management in Parkinson's disease: a feasibility study of ambulatory posture detection and feedback to treat stooped posture. Parkinsonism Relat Disord 2018; 46: S57–S61.
- 47. Kim SH, Seo DY. Effects of a therapeutic climbing program on muscle activation and SF-36 scores of patients with lower back pain. J Phys Ther Sci 2015; 27: 743–746.
- 48. Granacher U, Lacroix A, Muehlbauer T, et al. Effects of core instability strength training on trunk muscle strength, spinal mobility, dynamic balance and functional mobility in older adults. Gerontology 2013; 59: 105–113.
- 49. Im B, Kim Y, Chung Y, et al. Effects of scapular stabilization exercise on neck posture and muscle activation in individuals with neck pain and forward head posture. J Phys Ther Sci 2016; 28: 951–955.
- 50. Park SH, Lee MM. Effects of lower trapezius strengthening exercises on pain, dysfunction, posture alignment, muscle thickness and contraction rate in patients with neck pain; randomized controlled trial. Med Sci Monit 2020; 26: e920208.
- 51. Mehri A, Letafatkar A, Khosrokiani Z. Effects of corrective exercises on posture, pain, and muscle activation of patients with chronic neck pain exposed to anterior-posterior perturbation. J Manipulative Physiol Ther 2020; 43: 311–324.
- 52. Fil-Balkan A, Salci Y, Keklicek H, et al. Sensorimotor integration training in Parkinson`s disease. Neurosciences (Riyadh) 2018; 23: 208–215.
- 53. Kim SH, Yun SJ, Dang QK, et al. Measurement and correction of stooped posture during gait using wearable sensors in patients with Parkinsonism: a preliminary study. Sensors (Basel) 2021; 21.
- 54. Bloem BR, Beckley DJ, van Dijk JG. Are automatic postural responses in patients with Parkinson's disease abnormal due to their stooped posture? Exp Brain Res 1999; 124: 481–488.