Introduction
The size of the common bile duct (CBD) is a predictor of biliary obstruction, and its measurement is an essential factor in the evaluation of the biliary system. The normally accepted range for the diameter of the CBD is 2–7 mm [, ]. CBD dilation generally implies obstructive pathologies and is a critical feature in distinguishing obstructive from non-obstructive causes of CBD dilation. Whether the CBD diameter undergoes any biological change with time is still highly under debate. Some authors said that with an increase in age, the diameter of CBD also increases normally. Wu et al. [] reported that physiologically, the CBD diameter increases by 1 mm every decade, and its widest inner diameter could reach up to 10 mm. However, studies such as the one described by Horrow et al. [] stated that there was no significant relationship between age and CBD size.
Furthermore, there are no claims regarding the CBD diameter size in patients with gall bladder stones. Not enough studies have been reported regarding whether the CBD size is affected in patients with cholelithiasis without any CBD lesions. To assess this difference in opinions, we investigated the CBD diameter in both the asymptomatic population and the population with gall bladder stones. Moreover, we compared the CBD dilation in both populations.
Our study involves 2 sections; the first part includes evaluating the relationship between age and CBD diameter in individuals without biliary abnormalities. The second part consists of the investigation of the CBD size in patients with gall bladder stones. Although ultrasound is still the first imaging study widely available to examine the biliary system, MRCP was chosen as our imaging modality to examine the size of the CBD because of its higher sensitivity and specificity where the biliary tree is concerned [-]. The purposes of this study are to determine whether the CBD increases physiologically with age in individuals without biliary abnormalities; to determine if there is a dilation of the CBD in gall bladder stones patients; and to investigate if there are any significant differences in CBD size between the asymptomatic population and cholelithiasis population.
Methods
For the first part of our study, 7,090 prospective candidates who underwent an abdominal MRI were identified between January 2016 and December 2019 at the Nanjing First Hospital. Those individuals were between 16 and 95 years old and had undergone MRCP examination for differential diagnosis or cause of Abdominal discomfort. MRCP is a procedure that uses T2 sequence magnetic resonance imagery to non-invasively evaluate the anatomy and pathology of the biliary system []. Patients having had prior gall bladder, biliary, pancreatic, hepatic, or gastrointestinal surgeries were excluded from this study. Further exclusion criteria comprised those having been diagnosed in the past or were diagnosed at that time with CBD stones/lesions; cases having a history of jaundice; and those with pancreatic and liver tumours. Patients on opioids were likewise not selected. The final cohort study for our first sample consisted of 517 patients, including 280 female and 237 male patients, aged 18–92 years.
For the second part of our study, 2,467 prospective candidates who underwent MRCP for suspected gall bladder stones were identified between August 2018 and December 2020 at the Nanjing First Hospital. Those individuals were between 18 years old and 92 years old.
Our exclusion criteria for this second part were previous abdominal surgeries, CBD stones/lesions, pancreatic or liver diseases, and patients taking opioids. The final sample for our second part of the study was composed of 204 patients, including 75 male and 129 female patients from 18 years to 90 years old. Only patients in whom the entire extrahepatic bile duct was illustrated were included in the study.
Before image acquisition, participants fasted 6 h to reduce fluid secretions within the stomach and duodenum, reduce bowel peristalsis, and promote gall bladder distension. Using the images obtained from MRCP, each patient’s inner diameter of the extrahepatic bile duct was measured digitally from the screen and recorded at the widest estimated site. The largest diameter of each duct was calculated from perpendicular cross sections at the particular points of the tree by placing an electronic calliper perpendicular to the long axis at the widest visible portion of the CBD on MRCP for all the patients [, ] (shown in Fig. 1). The image was then amplified to maximise the accuracy of measurement. Pre- and post-amplification yielded the same measurement.
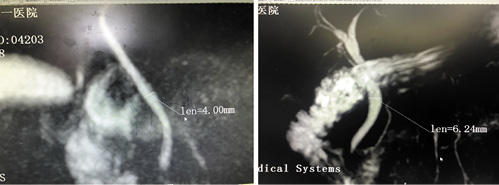
Fig. 1
Measurement method: measurement of the CBD diameter by placing an electronic calliper at the widest estimated portion of the CBD inner diameter on MRCP. CBD, common bile duct.
We subdivided all the patients of both samples (asymptomatic and cholelithiasis) into 8 groups, regardless of their gender, each having a range of 10 years to facilitate statistical assessment: group 1, ≤20 years; group 2, 21–30 years; group 3, 31–40 years; group 4, 41–50 years; group 5, 51–60 years; group 6, 61–70 years; group 7, 71–80 years; and group 8, >80 years old. Data evaluation and statistical interpretation were made independently for each sample (shown in Fig. 2).
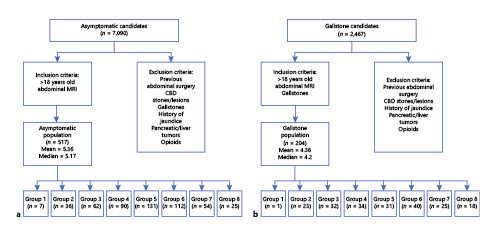
Fig. 2
Charts showing inclusion and exclusion criteria for the asymptomatic (a) and gallstone population (b).
Statistical Analysis
After having collected all the data, we proceeded with descriptive statistics for our whole sample. Data analyses were performed with the Statistical Package for the Social Sciences for Mac (SPSS 26.0; IBM, Armonk, NY, USA), and values were computed as means, standard deviation, median, and range. The total means of both the age and the CBD size for both the asymptomatic and the cholelithiasis populations were recorded. The Spearman correlation test was used to determine the presence of an association between the CBD diameter and age. Next, the mean CBD diameter of the male patients was compared with the female patients using the independent sample t test. Furthermore, the mean age and mean CBD diameter and median of the CBD of each of the 8 subgroups were calculated and recorded for further evaluation.
Assessment of the CBD diameter among each subgroup was done using one-way ANOVA to compare the mean values between the different age groups. The Games-Howell test was used as a post hoc test for multiple comparisons. A p value < 0.05 was considered statistically significant. Each age group from the asymptomatic population was compared with their respective cholelithiasis population using the independent t test.
Result
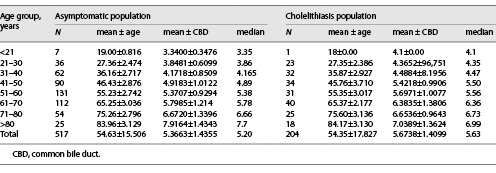
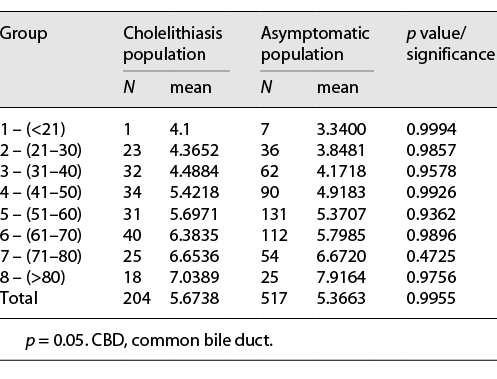
Our study is composed of 721 patients divided into 2 groups: 517 asymptomatic patients with a mean age of 54.63 ± 15.506 ranging from 18 to 92 years and a mean CBD diameter of 5.3663 mm ± 1.43546 and median of 5.20 mm, ranging from 2.51 mm to 11.1 mm, and 204 patients with cholelithiasis having a mean age 54.53 ± 17.827 ranging from 18 to 90 years and an average CBD diameter of 5.6738 mm ± 1.40986 and median of 5.63 mm, ranging from 2.65 mm to 10.12 mm. Each population was further subdivided into 8 groups, as shown in Table 1.
Asymptomatic Population
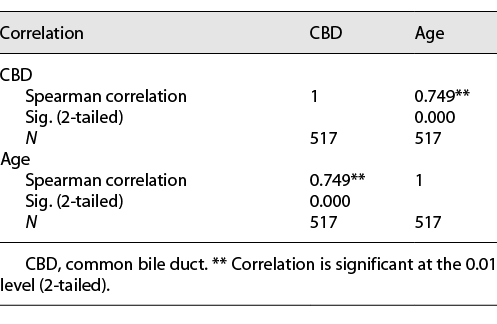
The Spearman correlation test between the CBD diameter and age, as shown in Table 2, was statistically significant at the p < 0.01 level (2-tailed) (r = 0.749). According to the linear periodic model, the regression equation for the CBD diameter was as follows: Y = 0.07X + 1.517. Thus, the duct gradually dilated by 0.07 mm/year (shown in Fig. 3).
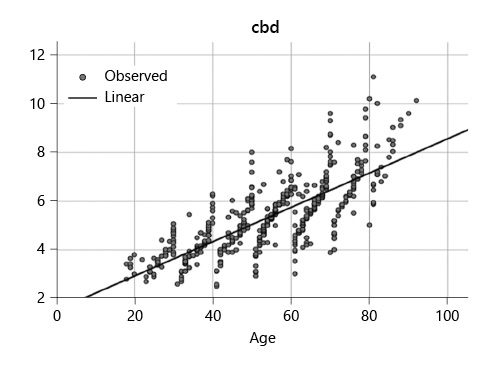
Fig. 3
Linear regression model between the CBD diameter of asymptomatic population and age (Y = 0.07X + 1.517). CBD, common bile duct.
Among the 517 subjects, the mean CBD diameter in female patients was larger than that in male patients (5.4474 ± 1.46757 vs. 5.2706 ± 1.39360) (median = 5.39 vs. 5.23), but this difference in values did not prove to be statistically significant (t = 1.397, p = 0.163). Since a correlation was previously found, we investigated the presence of an increase in CBD length within each decade among each subgroup using ANOVA.
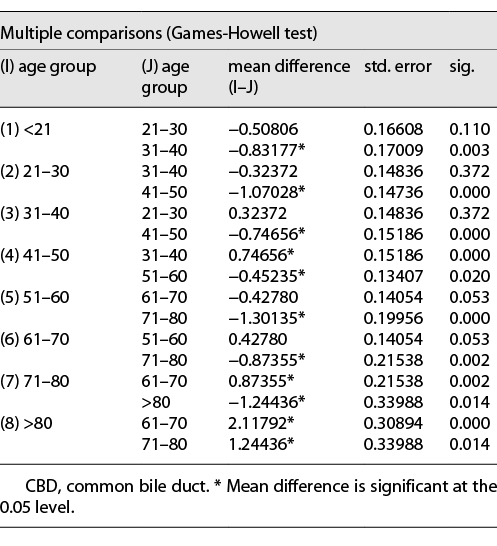
The mean CBD of each age group was plotted on a graph, and an increase in the size of the CBD was noted and is shown in Figure 4. The 2 obvious turning points where an increase in CBD size was relatively more drastic were observed to be the 2 age groups 31–40 and 61–70 years. Further statistical analysis was done. Levene’s test showed that equal variance was not assumed, and since samples were not of equal sizes, the Games-Howell test was used as a post hoc test for multiple comparisons among the means. The result of the homogeneity of variance from ANOVA is shown in Table 3. (Note: comparison of each subgroup with each subgroup is not shown in the table to facilitate understanding of the results. Only the result for each subgroup in relation to their 10-year differences is shown in the table.)
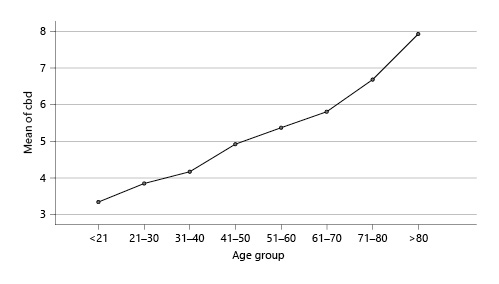
Fig. 4
CBD means for asymptomatic population plotted against age groups. CBD, common bile duct.
Cholelithiasis Population
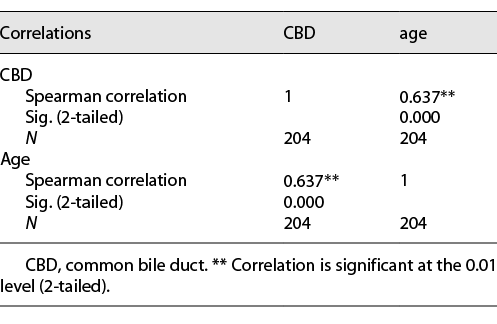
The Spearman correlation test between the CBD diameter and age, as shown in Table 4, was significant at the p < 0.01 level (2-tailed) (r = 0.637) (Table 4). According to the linear periodic model, the regression equation for an increase in the CBD diameter as our cholelithiasis sample aged was Y = 0.049X + 2.994 (shown in Fig. 5). The mean CBD diameter in male patients was larger than that in female patients (5.7027 ± 0.16783 vs. 5.6571 ± 1.12233) (median = 5.72 vs. 5.6), but this difference in values did not prove to be statistically significant (t = 0.22, p = 0.689).
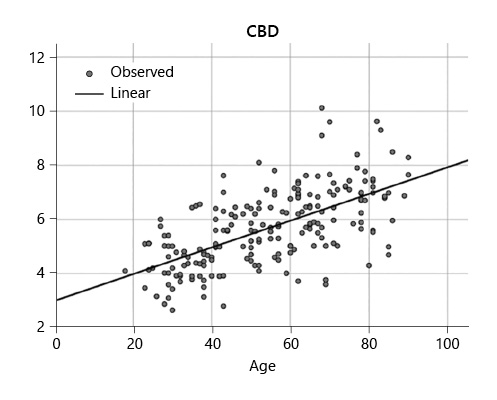
Fig. 5
Linear regression model between the CBD diameter of cholelithiasis patients and age (Y = 0.049X + 2.994). CBD, common bile duct.
The mean CBD of each age group was plotted on a graph, and an increase in the size of the CBD is shown in Figure 6. Similarly, for this population, ANOVA showed a statistically significant increase in the CBD diameter in each subgroup (p < 0.05).
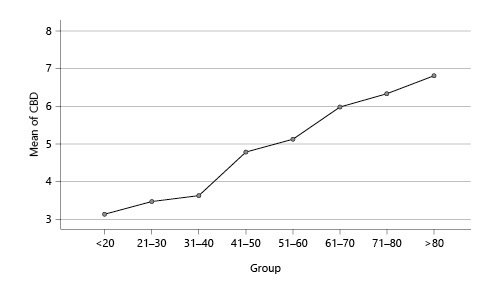
Fig. 6
CBD means for cholelithiasis population plotted against age groups. CBD, common bile duct.
Comparison of Each Population
The means of all age groups from the asymptomatic population were compared, respectively, with those in the cholelithiasis population to investigate the presence of statistical differences between the mean CBD of the 2 populations. The results are shown in Table 5. There are no statistical differences between the CBD size among the respective age groups.
Discussion
Over the last 3 decades, many studies were published attempting to reach a consensus regarding the physiological scale of the CBD diameter. Wu et al.’s [] cohort, which consisted of 256 patients without biliary, pancreatic, or hepatic disease, established that there is an increase in the CBD diameter and age. Moreover, they claimed that a CBD size of 10 mm could be considered normal as one gets older. Similarly, in our study, we have observed in our asymptomatic population that with increasing age, the diameter of the CBD also increases (r = 0.749) (p < 0.05). Although the majority of the study subjects (95%) had a CBD diameter of <6 mm, the largest CBD diameter recorded in this experiment was 11.1 mm, and our oldest subgroup, which had a mean age of 83 years, recorded a mean CBD size of 7.9 mm ± 1.43546. Therefore, from our data, we can assume, on average, the largest diameter that can be considered reasonable to be 8 mm.
Concurrently, Bowie stated the standard upper limit to be 7 mm in his review article, and Bachar set his upper limit as 8.5 mm [, ]. Likewise, Parulekar [] in this study including 73 fasting patients between 20 and 65 years set the upper limit for the CBD diameter to be 7.0 mm.
Conversely, in a prospective study of 258 patients, Horrow et al. [] found that there was no increase in the size of the CBD with age. This may be explained by the fact that 50% of their patients’ age ranged from 45 to 60 years and may be considered unevenly distributed across all age groups. Meanwhile, Perret et al. [] observed 1,018 healthy subjects and claimed that the mean CBD diameter of patients aged 60 years and younger to have a mean value of 3.6 mm, while those between 60 and 96 years old to have a mean diameter of 4.0 mm, thus indicating the presence of a significant increase in CBD diameter among subjects older than 60 years.
Nevertheless, Horrow was not the only one to deny claims about physiological dilation of the CBD. Reinus et al. [] have also stated that there was no association between age and CBD diameter, but rather with an underlying disease.
In their study, Reinus et al. [] made use of ultrasound to evaluate the diameter of the CBD. However, recently, several studies have shown that MRCP has superiority over ultrasound in the assessment of the biliary tree []. Ultrasound has less sensitivity and specificity than MRCP and highly depends on the technician skills and experience, thus increasing human error margin [, , ]. The use of specific imaging modalities may be a factor influencing findings in the CBD size evaluation.
Several studies have denied any relationship between gender and CBD diameter [, ]. Our experiment had similar evidence to support these claims as we did not see any statistically significant difference in CBD diameter among male and female patients.
Kaude [] established a mean diameter of 4.1 mm for a sample of 350 subjects. These included patients were from 20 to 71 years old. In our experiment, the mean CBD diameter was 5.3663 ± 1.43546. This difference in our mean values may be explained by the fact that almost 30% of Kaude’s patients were younger than 30 years. Consequently, this may imply that there is a difference in the CBD diameter among different age groups. Likewise, Wu et al. [] have reported an increase of 1 mm every decade.
That being said, in our asymptomatic population, we observed that prior to the age of 31–40 years, there was a statistically significant increase in the CBD diameter every 2 decades. However, past this age, the increase was then notable every decade. We also identified 2 obvious age groups where the CBD diameter demonstrated a relatively sharper increase than other age groups (shown in Fig. 3), the first cut-off point being the age group of 31–40 years and the second cut-off point being 61–70 years. Peng et al. [] likewise reported his cut-off age to be 60, while Kaim et al. [] stated that people older than 75 years had a considerably wider CBD width than younger individuals. Yet, between the age groups 51–60 and 61–70 years of our research, the increase in CBD diameter was not statistically significant, with a p value of 0.053, which is close to 0.05. A larger sample size might have given a statistically significant value. Nevertheless, Park et al. [] stated that individuals aged 50 years had a larger CBD diameter than those aged <50 years.
We can assume that a trend exists in between decades, and this result coincides partly with some other experiments done in the past. After taking into consideration the CBD mean diameters for every decade, Bachar et al. [] concluded that the duct would gradually dilate at a rate of 0.04 mm/year. Another more recent study stated that the duct would progressively dilate by 0.03 mm/year []. Further studies later on supported this statement [, , ]. Similarly, our findings denote a close rapport; according to our mean diameters in every decade for our asymptomatic population, we found that the CBD would dilate at a rate of 0.07 mm every year (shown in Table 2).
To this day, the exact mechanism behind the physiological changes in CBD size is not fully understood; however, several hypotheses have been put forward. Takahashi et al. [], in their study on morphometric evaluation of the bile duct, theorised this increase in diameter to be due to the loss of elastic fibres within the CBD. Meanwhile, Nakada [] gave a slightly modified perspective on that matter. As one gets older, proliferation and fibrosis of both the submucosal and intermuscular glands lead to the thickening and sclerosis of the pre-ampullary portion of the CBD. Moreover, an increase in collagen fibres accompanied by a spread of fragmented elastic fibres causes diffuse sclerosis of the pancreatic part of the extrahepatic bile duct. Collectively, this leads to a compensatory dilation of the proximal CBD [].
On the other hand, Kialian stated that CBD expansion resulted from decreased hypotonic activity and contractility of the duct. They further suggested that this was mainly due to the characteristic fragmentation of the longitudinal smooth myocyte bands, interspersed connective tissue, and a decrease in the reticular-elastic framework of the duct wall over time []. Also, the use of calcium antagonists and nitroglycerine in the ageing population has been suggested to influence contractility and tonicity of the CBD wall, thus contributing to the variations in CBD [].
Nevertheless, insufficient understanding of the exact mechanism by which the CBD physiologically dilates does not implicate that such phenomenon does not occur, which begs the question if pathological processes such as cholelithiasis could affect or change the physiological process of CBD dilation. However, we found no studies reporting the relationship between gall bladder stones and CBD size. To investigate the possibility of a relationship between gallstones and CBD size, we first performed a Spearman correlation test which showed a positive correlation between the CBD diameter and increasing age (r = 0.637). A linear equation was calculated for this sample, and an increase of 0.049 mm was noted annually in our cholelithiasis sample. This leads us to wonder whether in the presence of pathological processes, the CBD diameter is still under the influence of physiological dilation. This was further supported when we computed ANOVA where an increase in the CBD diameter was seen among the different age groups in a linear manner.
Nonetheless, this increase in the CBD diameter in our cholelithiasis population might be explained by the presence of stones in the gall bladder. In order to elucidate this matter, we further compared these results against the results in the asymptomatic population where we found the mean diameter of groups 1–7 from our gallstone population showed a slightly bigger CBD diameter than groups 1–7 of the asymptomatic population. Nevertheless, none of those was statistically significant (p > 0.05).
From our results, we conclude the general increase in the CBD for the gallstone population to be because of the dilation of the CBD that happens physiologically as one ages and not because of gallstones independently affecting this process. It should be pointed out that group 8 from the asymptomatic population showed a bigger CBD diameter than the cholelithiasis population, but this difference was not deemed significant.
Our 2 samples showed comparable results, which support the claims of an increase in CBD size as one gets older. There are a few limitations that we did not account for in this study. First, Wachsberg [] showed that the maximal bile duct measurement could increase during deep inspiration. We did not consider the respiratory phase while measuring the CBD. Our cohort did not control variables such as height and weight. Moreover, in this trial, the age group below 21 years was not well represented. Our second sample was relatively less than the first sample, and a bigger cholelithiasis sample might have yielded a better correlation and closed the gap between the mean CBD diameter of both samples.
Finally, this experiment was performed in a single-centre setting, thus consisting of only the Chinese population. This result may not generalise others with a different ethnical background.
In conclusion, this investigation demonstrated a significant relationship between age and CBD diameter in a healthy population. The result of our cohort showed dilation of the CBD at a rate of 0.049–0.07 mm per annum in our population and an average size of 8 mm in the asymptomatic older population to be considered reasonable. This is a useful reference to consider when evaluating the extrahepatic duct of advanced aged patients. Furthermore, there was also a general increase in the CBD diameter in our cholelithiasis population as age was increasing. Therefore, we conclude that there is the presence of physiological dilation of the CBD diameter as one ages and that gallstones do not play an independent role in this process. Generally, CBD dilation suggests an obstructive pathology; but, in this study, we have established that the CBD also dilates as one gets older; thus, changes in the CBD should not only be considered as a pathological process but also as a physiological process. Clinically, CBD dilation in the absence of obstructive pathologies in older patients should not lead to a rushed initial diagnosis that would require further invasive evaluations such as ERCP. Hence, a good estimation of the appropriate range of the CBD size for different age groups is valuable to prevent misdiagnosis and unnecessary diagnostic investigation. Furthermore, this opens room for further studies to concentrate on how to distinguish better physiological dilation versus pathological dilation in the CBD.
Acknowledgements
This article does not include any non-author contributors to acknowledge.
Statement of Ethics
This retrospective study protocol was reviewed and approved by the Nanjing First hospital affiliated with Nanjing Medical University committee (approval number: not applicable, approval date: October 7, 2019).
Informed consent: The Institutional Review Board classified this study as exempt, and informed consent was not required.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This study did not receive any funding.
Author Contributions
Shankara Subramanyam Govindan, Nebiyu Elias Tamrat, and Zi Jun Liu contributed to conception and design. Zi Jun Liu provided administrative support. Shankara Subramanyam Govindan, and Zi Jun Liu provided study materials or patients. Shankara Subramanyam Govindan, and Nebiyu Elias Tamrat contributed to collection and assembly of data. Shankara Subramanyam Govindan, Nebiyu Elias Tamrat, and Zi Jun Liu analysed and interpreted the data. Shankara Subramanyam Govindan, Nebiyu Elias Tamrat, and Zi Jun Liu wrote the manuscript. Shankara Subramanyam Govindan, Nebiyu Elias Tamrat, and Zi Jun Liu approved the final version of the manuscript.
Data Availability Statement
All data generated or analysed during this study are included in this published article. Additional data may be obtained from the corresponding author on reasonable request.
References
- 1. Bowie JD. What is the upper limit of normal for the common bile duct on ultrasound: how much do you want it to be. Am J Gastroenterol. 2000 Apr;95(4):897–900.
- 2. Rumack CM, Wilson SR, Charboneau JW. Diagnostic ultrasound. In: Laing FC, editor. The gallbladder and bile ducts. St. Louis, MO: Mosby-Year Book, Inc. Co.; 1991. p. 106–444.
- 3. Wu CC, Ho YH, Chen CY. Effect of aging on common bile duct diameter: a real-time ultrasonographic study. J Clin Ultrasound. 1984 Oct;12(8):473–8. http://dx.doi.org/10.1002/jcu.1870120804.
- 4. Horrow MM, Horrow JC, Niakosari A, Kirby CL, Rosenberg HK. Is age associated with the size of adult extrahepatic bile duct: sonographic study. Radiology. 2001 Nov;221(2):411–4.
- 5. Freitas ML, Bell RL, Duffy AJ. Choledocholithiasis: evolving standards for diagnosis and management. World J Gastroenterol. 2006 May 28;12(20):3162–7. http://dx.doi.org/10.3748/wjg.v12.i20.3162.
- 6. Romagnuolo J, Bardou M, Rahme E, Joseph L, Reinhold C, Barkun AN. Magnetic resonance cholangiopancreatography: a meta-analysis of test performance in suspected biliary disease. Ann Intern Med. 2003 Oct 7;139(7):547–57. http://dx.doi.org/10.7326/0003-4819-139-7-200310070-00006.
- 7. Hekimoglu K, Ustundag Y, Dusak A, Erdem Z, Karademir B, Aydemir S, et al. MRCP vs. ERCP in the evaluation of biliary pathologies: review of current literature. J Dig Dis. 2008 Aug;9(3):162–9. http://dx.doi.org/10.1111/j.1751-2980.2008.00339.x.
- 8. Uysal F, Obuz F, Uçar A, Seçil M, Igci E, Dicle O. Anatomic variations of the intrahepatic bile ducts: analysis of magnetic resonance cholangiopancreatography in 1011 consecutive patients. Digestion. 2014;89(3):194–200. http://dx.doi.org/10.1159/000358558.
- 9. Chen T, Hung CR, Huang AC, Lii JM, Chen RC. The diameter of the common bile duct in an asymptomatic Taiwanese population: measurement by magnetic resonance cholangiopancreatography. J Chin Med Assoc. 2012 Aug;75(8):384–8. http://dx.doi.org/10.1016/j.jcma.2012.06.002.
- 10. Chiu NC, Chiou YY. Role of MRCP in the measurement of the CBD diameter. J Chin Med Assoc. 2012 Sep;75(9):423–4. http://dx.doi.org/10.1016/j.jcma.2012.06.013.
- 11. Bachar GN, Cohen M, Belenky A, Atar E, Gideon S. Effect of aging on the adult extrahepatic bile duct: a sonographic study. J Ultrasound Med. 2003 Sep;22(9):879–5; quiz 883–5. http://dx.doi.org/10.7863/jum.2003.22.9.879.
- 12. Parulekar SG. Ultrasound evaluation of common bile duct size. Radiology. 1979 Dec;133(3 Pt 1):703–7. http://dx.doi.org/10.1148/133.3.703.
- 13. Perret RS, Sloop GD, Borne JA. Common bile duct measurements in an elderly population. J Ultrasound Med. 2000 Nov;19(11):727–31; quiz 731. http://dx.doi.org/10.7863/jum.2000.19.11.727.
- 14. Reinus WR, Shady K, Lind M, Scott R. Ultrasound evaluation of the common duct in symptomatic and asymptomatic patients. Am J Gastroenterol. 1992 Apr;87(4):489–92.
- 15. Yeh BM, Liu PS, Soto JA, Corvera CA, Hussain HK. MR imaging and CT of the biliary tract. Radiographics. 2009 Oct;29(6):1669–88. http://dx.doi.org/10.1148/rg.296095514.
- 16. O’Connor OJ, O’Neill S, Maher MM. Imaging of biliary tract disease. AJR Am J Roentgenol. 2011 Oct;197(4):W551–8. http://dx.doi.org/10.2214/AJR.10.4341.
- 17. Daradkeh S, Tarawneh E, Al-Hadidy A. Factors affecting common bile duct diameter. Hepatogastroenterology. 2005 Nov–Dec;52(66):1659–61.
- 18. Chen T, Hung CR, Huang AC, Lii JM, Chen RC. The diameter of the common bile duct in an asymptomatic Taiwanese population: measurement by magnetic resonance cholangiopancreatography. J Chin Med Assoc. 2012 Aug;75(8):384–8. http://dx.doi.org/10.1016/j.jcma.2012.06.002.
- 19. Kaude JV. The width of the common bile duct in relation to age and stone disease. An ultrasonographic study. Eur J Radiol. 1983 May;3(2):115–7.
- 20. Peng R, Zhang L, Zhang XM, Chen TW, Yang L, Huang XH, et al. Common bile duct diameter in an asymptomatic population: a magnetic resonance imaging study. World J Radiol. 2015;7(12):501. http://dx.doi.org/10.4329/wjr.v7.i12.501.
- 21. Kaim A, Steinke K, Frank M, Enriquez R, Kirsch E, Bongartz G, et al. Diameter of the common bile duct in the elderly patient: measurement by ultrasound. Eur Radiol. 1998;8(8):1413–5. http://dx.doi.org/10.1007/s003300050563.
- 22. Park JS, Lee DH, Jeong S, Cho SG. Determination of diameter and angulation of the normal common bile duct using multidetector computed tomography. Gut Liver. 2009 Dec;3(4):306–10. http://dx.doi.org/10.5009/gnl.2009.3.4.306.
- 23. Matcuk GR, Grant EG, Ralls PW. Ultrasound measurements of the bile ducts and gallbladder: normal ranges and effects of age, sex, cholecystectomy, and pathologic states. Ultrasound Q. 2014 Mar;30(1):41–8. http://dx.doi.org/10.1097/RUQ.0b013e3182a80c98.
- 24. Takahashi Y, Takahashi T, Takahashi W, Sato T. Morphometrical evaluation of extrahepatic bile ducts in reference to their structural changes with aging. Tohoku J Exp Med. 1985 Nov;147(3):301–9. http://dx.doi.org/10.1620/tjem.147.301.
- 25. Nakada I. Changes in morphology of the distal common bile duct associated with aging. Gastroenterol Jpn. 1981;16(1):54–63. http://dx.doi.org/10.1007/BF02820425.
- 26. Kialian GP, Aznaurian AV. [The age-related characteristics of the muscular layer of the common bile duct in man]. Morfologiia. 1995;108(1):10–2. Russian.
- 27. Wachsberg RH. Respiratory variation of extrahepatic bile duct diameter during ultrasonography. J Ultrasound Med. 1994 Aug;13(8):617–21. http://dx.doi.org/10.7863/jum.1994.13.8.617.