Introduction
In a recent study by , ), 105 United Kingdom (UK) general population participants determined that pharmacies with available National Health Service (NHS) support from general practitioners (GPs) and mental health workers are more suitable primary vendors of cannabis (marijuana) than regulated shops or the black market (p < 0.001). Support for legislated cannabis availability in pharmacies, for therapeutic use and as part of a harm reduction strategy, was observed to be highest amongst the university-educated and medical healthcare practitioner subgroups (). A majority of the participants also determined that being legally permitted to consume cannabis is a human right (). The aim of the study reported in this article was to further the research of the previous survey and to determine more specifically how such a regulated market would function.
Cannabis is a genus of flowering plants in the family Cannabaceae and has been cultivated by humans for thousands of years for a variety of purposes including: the production of clothing, use as a food source, material to produce paper and rope, as a fuel source, in textiles such as ships’ sails and carpets, as a medicine and as a source of psychoactive effects for use in spiritualistic, healing and recreational settings (; ; ; ; ; ; ). Cannabis is reported to originate from Central Asia and/or upper South Asia and the plant can now be found growing in numerous environments and locations globally (; ). Cannabis sativa was classified by Carl Linneaus in 1753 upon its discovery in the Himalayan foothills and Cannabis indica was classified by Jean-Baptiste Lamarck in 1785 following its discovery in India (; ). Modern cannabis is often a hybrid of sativa and indica strains.
In the early 20th century, cannabis was criminalised in the United States (US) with global repercussions for reasons still considered by many to be controversial (; Jonnes, 1999; ). More recently, countries such as Canada (), Uruguay (), the majority of US states (; ), the Netherlands (), Thailand () and the UK () have been exploring alternative approaches to cannabis regulation. Cannabis use is broadly considered a binary issue, namely: medical use and recreational use (). Although both uses remain illegal under US federal law, a majority of states have legalised medical marijuana and some states such as California have legalised cannabis for non-medical use ().
Unlike most medicines, which typically consist of one pharmacologically active compound (e.g. paracetamol), herbal cannabis contains at least 144 compounds referred to as cannabinoids – the most well recognised being tetrahydrocannabinol (THC) and cannabidiol (CBD) (Supplementary Figure 1) (). THC is the primary psychoactive compound whereas CBD does not exhibit psychoactive properties, however, both THC and CBD are reported to have applications for medical disorders (; ). The many chemical components in cannabis such as terpenes (Supplementary Figure 1) produce what is referred to as the ‘entourage effect’ when cannabis is consumed as a naturally occurring mixture of compounds from the raw plant material (; ). The genetic lineage or strain (e.g. Afghan Kush/Lemon Haze/Girl Scout Cookies) of cannabis and the environmental conditions in which the cannabis is grown have an impact on the biosynthesis and relative concentrations of the different compounds in cannabis. Consequently, herbal cannabis as a medicine presents a significant divergence from standard pharmaceutical small molecule therapeutics which are approved by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) which require medicines to be standardised in quantity, quality, dosage and route of administration (; ).
The UK government has attempted to appease changes in public perceptions towards cannabis use – particularly regarding access to cannabis for medical purposes – and has amended the status of cannabis to Schedule 2 (; ). This change of Schedule implies an acceptance of potential therapeutic use and in theory facilitates research into the development of cannabis-derived medicines (; ; ; ). However, despite rescheduling of cannabis-based medicinal products (CBMPs) under the Misuse of Drugs Act in November 2018 access remains poor. The commissioned a survey into medical cannabis use in the UK. Sixty-three percent of survey respondents reported discussing CBMPs with their GP and 72% had turned to illicit markets to source cannabis for therapeutic use. Of those using CBMPs, 83% reported great relief for their condition and 90% reported experiencing no or mild-only side effects. The Group estimated 300,000–1,000,000 UK residents use cannabis therapeutically, however, no NHS prescriptions had been written as of February 2019 and less than 100 were estimated to have been written by May 2019 (; ).
Despite rescheduling to Schedule 2, Epidiolex, a cannabis formulation developed to treat specific types of epilepsy, was rejected by the National Institute of Health and Care Excellence (NICE) for availability on the NHS on the grounds of the treatment not being cost effective and a lack of evidence supporting clinical efficacy (; Smith, 2019b). However, as of 11th November 2019 NICE released new guidelines allowing GPs to prescribe Sativex (Nabiximols) on the NHS in England and Epidiolex to patients with two rare forms of epilepsy: Lennox-Gastaut Syndrome and Dravet Syndrome (). With the aforementioned exception of Sativex, an oromucosal spray containing 1:1 THC:CBD licensed for the treatment of spasticity in multiple sclerosis, Epidiolex and dronabinol, most CBMPs are currently considered unlicensed medicines (; ).
Access to CBMPs requires prescriptions to be written by specialist doctors on the Specialist Register of the General Medical Council on a named patient basis (; ). Guidance from England’s Chief Medical Officer stipulates that doctors should prescribe products only for disorders within their speciality when there is clear published evidence or UK guidelines to support treatment, when clinical need cannot be met by a licensed medicine and when established treatment options have been exhausted (). UK law also requires specific importation licenses, which increase the cost and complexity of prescriptions (; Smith, 2019a; ). As a result, NHS trusts and professional bodies are unwilling to recommend prescribing CBMPs and access to CBMPs is almost entirely limited to private-care patients. Most patients are therefore presented with the same choice that existed prior to rescheduling: reliance on prescribed medicines often with high incidence of side effects and addictive potential, such as opiates, or risk legal repercussions on access to cannabis through illicit markets (; ; ; ).
In addition to the complex legal situation regarding access to cannabis for medical purposes the legal position on the use of cannabis for non-medical purposes is similarly nebulous. Despite UK law officially holding a zero tolerance stance for the possession and cultivation of cannabis in reality the possession, cultivation and even sale of cannabis are increasingly being ignored and tolerated by the criminal justice system (). However, in a situation mirroring that of the US, ethnic minorities such as people of Afro-Caribbean descent are often disproportionately represented in arrests and criminal convictions despite use not being higher in such groups (). It has been estimated that in excess of 10 million 16–59 year olds in England and Wales have used cannabis at least once in their lifetime (). In a country with a population estimated to be approximately 67 million at the time of writing, if the law was effectively applied in its most severe form this would lead to the imprisonment of at least 15% of the population accompanied by inevitable economic damage and social unrest.
Whilst there are potential benefits to cannabis use becoming increasingly tolerated by society the illicit market presents numerous harms which in many cases outweigh the potential negative impacts of cannabis use (; ). Violence and theft are commonplace in unregulated markets regardless of the type of product; it has been argued that the association between crime and cannabis is due to its illegality and would diminish significantly in the case of a regulated cannabis market (). Indeed, it has been reported that elderly and sick members of the general population attempting to obtain cannabis for medical purposes have been robbed and cheated by black market distributors (). Furthermore, the lack of legal oversight of the market means that the harms to physical and mental health posed by cannabis use are ineffectively monitored by healthcare professionals or mitigated by an effective regulatory system. Use of cannabis (i.e. THC) can lead to higher likelihood of developing psychosis whereas CBD, which is typically present in low or trace quantities in illicit cannabis, has antipsychotic properties and can attenuate THC harms (, ; ; ; ; ; ). Cannabis use can lead to severe health problems and prohibition of cannabis does little to reduce the likelihood of incidences of negative health impacts (). As a result, previous work has demonstrated that a UK population sample would likely be supportive of legal availability of cannabis in a healthcare context to reduce the harms it poses wellbeing ().
The Netherlands has been and continues to be a location of much drug tourism largely due to the existence of “coffee shops” (). Amsterdam’s coffee shops operate in a legal grey area in which the production and cultivation of cannabis and supply to these shops is prohibited but the sale of small quantities and onsite consumption is tolerated by the Dutch police and authorities (). However, the use and supply of cannabis within the Netherlands has continually been a topic of contention and disagreement across Dutch society. Drug tourism whilst bringing income to the local economy has been an issue of concern for many in the Netherlands and the topic of cannabis sale and use remains a highly contested issue (). As previously highlighted, cannabis regulation is a multifaceted and complex topic and as yet there is little international consensus on how to effectively manage the production, sale and use of the plant for medical and non-medical purposes (; ; ; ).
The present authors hypothesise that the widely-held belief that cannabis use can be viewed as a binary issue of therapeutic or recreational use may not be accurate in all cases and that cannabis consumption is on a spectrum of recreational-therapeutic use. Consequently, the authors developed what could be referred to as the recreational-therapeutic crossover hypothesis which predicates that some recreational uses of cannabis can concurrently present a psychotherapeutic component and that some medical uses of cannabis, particularly regarding treatment of psychiatric disorders such as anxiety and stress, may have a complementary psychotherapeutic mechanism of action effectively indistinguishable from those which can contribute to recreational use (Figure 1). Whilst being diagnosed or not diagnosed with a mental or physical disorder could be described as being binary, cannabis users have attested that cannabis use for recreational and therapeutic purposes are not easily distinguishable in all cases (). Therefore, any effective legal regulatory model which can incorporate the broad range of applications of cannabis would likely have to take this aspect of the plant’s therapeutic idiosyncrasy into account.
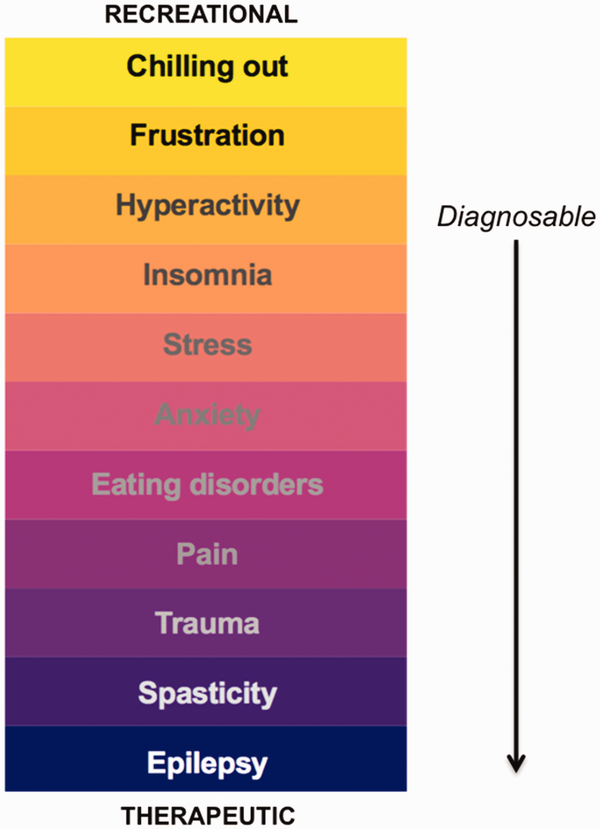
Figure 1
Diagram representing a simplified general model of the proposed spectrum of recreational-therapeutic use. The disorders from hyperactivity onward are diagnosable but most doctors would likely be unwilling to prescribe cannabis to treat these disorders in the majority of cases.
The Multidisciplinary Association for Psychedelic Studies (MAPS) is a non-profit organisation whose aim is to investigate beneficial uses of psychedelics and cannabis (www.maps.org). MAPS has received media attention in part due to the MAPS-funded clinical trials for MDMA-assisted psychotherapy which has been categorised as a breakthrough therapy by the FDA. The survey described in this article was advertised via MAPS’ social media accounts and monthly newsletter and being a US-based organisation had the advantage of facilitating the recruitment of an international sample with participants who have experience in growing, consuming, buying, and selling cannabis in both illicit and licit markets of various types. Consequently, a sample of participants obtained via MAPS could be an excellent sample of individuals experienced in the complexities of cannabis markets to help inform regulatory and policy changes in the UK.
In the original study by , the participants were presented the three options of pharmacies, regulated shops and the black market as possible suitable vendors for cannabis sales. Amsterdam-style coffee shops, cannabis social clubs and shisha-type bars were not explicitly mentioned. Whilst the statistically significant result that pharmacies are the preferred primary legal vendors of cannabis (according to a UK sample) is arguably reliable and rational, this result does not completely discount the existence of non-pharmacy locations for onsite purchase and consumption (). Therefore, alternative complementary legal vendors of Amsterdam-style coffee shops or shisha-type bars for onsite consumption were covered in this study (; ). A standard retail outlet was not offered as an option as previous data suggested a statistically significant conclusion that regulated shops are not the favoured type of vendor for cannabis in the UK (). In addition to asking questions about using the pharmacy retail model for legal availability of cannabis and the existence of locations for onsite purchase and consumption, questions were asked relating to the legalities of growing cannabis at home and public use.
In summary, the current study aimed to develop a model legal framework for the sale and use of cannabis which would allow full access to cannabis as a medicine, minimise potential harms caused by cannabis use, take into consideration the full complexities of cannabis culture, mitigate the emergence or persistence of illicit markets and respect individual liberties (; ;).
Methods
The research described in this article was approved by the Cardiff University School of Psychology ethics committee and was carried out with the informed consent of the participants.
Participant recruitment
Participants were recruited via the Multidisciplinary Association for Psychedelic Studies’ Facebook, Instagram and Twitter social media accounts and monthly newsletter. The general aim of the study was described as: “To develop a model for the sale of cannabis in the UK”.
Survey administration
The study was advertised via an organisation (the Multidisciplinary Association for Psychedelic Studies) which aims to promote and investigate therapeutically beneficial uses of psychedelics and cannabis. Therefore, the survey was designed so that it could be completed by members of the general public of any nationality with some knowledge of the topic. Due to the likelihood of some participants not being familiar with specific UK or other European aspects of the survey a short glossary was provided with definitions of specific terms (Amsterdam style coffee shop; NHS; GP; Shisha bar). The survey was administered using Qualtrics software involving an online survey and data collection tool. The data were collected between April 10th–June 13th 2019.
Inclusion criteria
Participants were required to consent to participating in the survey. The aim was to recruit a heterogeneous (diverse) sample from the MAPS database. Information on demographics and current/historic drug use were recorded to allow secondary analyses if required.
Questions
The majority of questions were administered requiring either a simple Yes/No response or a Likert Scale response: Strongly disagree; Somewhat disagree; Neither agree nor disagree/Don’t know; Somewhat agree; Strongly agree. A minority of questions required answering using prespecified, specifically worded answers. At the end of the survey participants were provided with a comments box.
Demographics
Participants were asked to provide demographic information regarding: nationality, age, education, gender, occupation and experience of cannabis purchase and use.
Results
Survey completion
397 individuals out of a total 411 consented to participating in the survey and completed it.
Valid percentages convention
All reported percentages for responses are valid percentages (unless stated otherwise), i.e. percentages of total participants who answered the question as opposed to percentages of the total participant sample number (397). For example, 364 participants answered the question on cannabis use at least once in their lifetime (92% of the total participant number). Three hundred and fifty seven out of 364 reported they had (90% of the total participants; 98% of the valid participant answers), and 2% (1.8% of total participants) indicated that they had never used cannabis.
Participant characteristics
In brief, the demographics of the 397 participants were as follows. Here, as per the convention described above, the number of responses for each category are expressed with valid percentages of the responses in parentheses. There were 252 male (69%) and 113 female (31%) participants. Two hundred and eighty one (77%) had been educated at a university and this number included current students. One hundred and seven participants (38%) were from the UK and 106 (38%) from the US. The remaining participants’ nationalities (present in smaller numbers) are detailed in the supplementary material. Participants were of a range of ages with the majority grouped within their 20 s and 30s (see supplementary material). A broad range of participant occupations were reported, including people working in the cannabis industry, with 84 (23%) working in a health related field (see supplementary material).
Participant cannabis use
Three hundred and fifty seven respondents (valid 98%) reported having used cannabis at least once in their lifetime. Of those 357 respondents, 61% reported having used cannabis medically; 77% both recreationally and therapeutically; and 98% reported having used cannabis recreationally. Thirteen percent reported having experienced health problems due to their cannabis use. Fifty four percent reported having ever bought cannabis in a legal regulated market (such as in California); 36% ever bought in a decriminalised market such as Portugal; and 82% ever bought in an illegal black market (such as in the UK). Sixty two percent of respondents reported that they use cannabis regularly (a couple of times a week) or frequently (everyday or every other day).
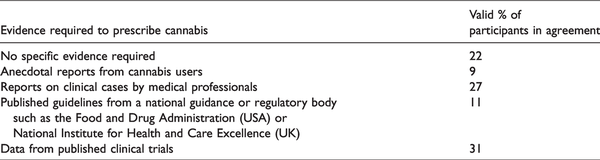
Pharmacies providing cannabis on prescription
When asked if cannabis should be available in pharmacies for therapeutic use with a doctor’s prescription, 98% of the valid respondents were in agreement. Participants were then questioned on how much evidence should be required to prescribe cannabis for the treatment of specific medical conditions (Table 1).
Participants were then asked for which of a provided list of diseases or disorders is there enough evidence for a GP/specialist to prescribe cannabis without further clinical trials and research (Figure 2) and then which healthcare professionals should be able to prescribe cannabis (Figure 3).
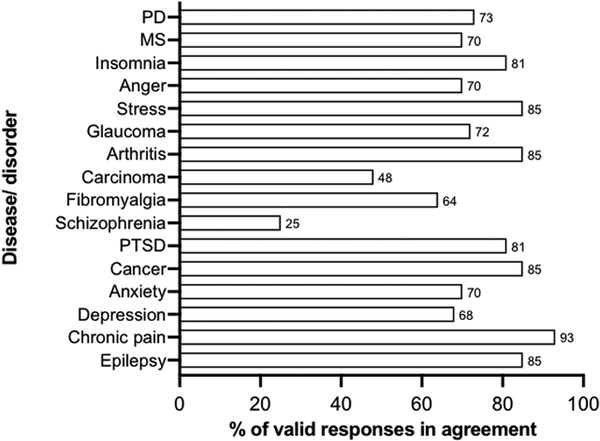
Figure 2
Percentage of valid participant responses in agreement with the proposed prescription of cannabis for 16 common diseases or disorders. PD: Parkinson’s disease; MS: multiple sclerosis; PTSD: post-traumatic stress disorder.
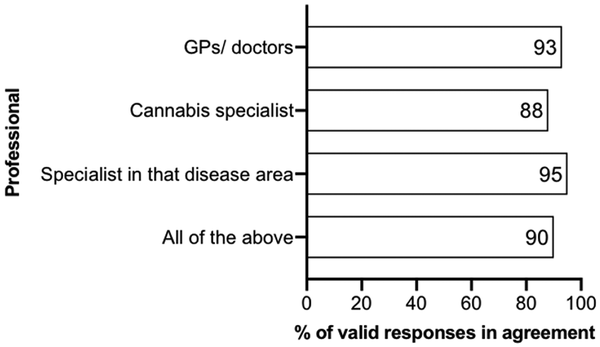
Figure 3
Percentage (valid) of survey participants who thought that each of the specified professionals should be able to prescribe cannabis.
Pharmacies providing harm reduction services for cannabis users
When questioned on the role pharmacies should play in cannabis regulation, 80% of participants agreed that they should provide harm reduction services including selling cannabis to recreational users. Of this 80%, 87% agreed that pharmacies should be more closely integrated with mental health services to assist cannabis users. This 80% were additionally asked if pharmacies should be able to provide on-site mental health services (e.g., counselling), and 76% agreed, however, a greater 87% agreed that pharmacists should be trained to deal with cannabis related mental health issues.
Cannabis consultation
Participants were asked if potential users of cannabis should undergo a consultation or screening to determine whether using cannabis for a particular individual is safe and how specifically cannabis could affect them both positively and negatively. Sixty six percent of participants agreed that this should be carried out and these participants were further questioned on who the screening should be carried out by (Figure 4).
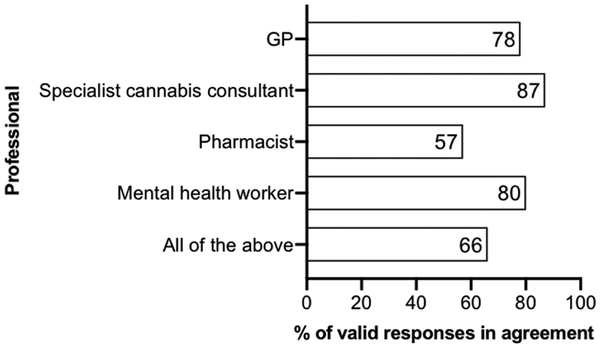
Figure 4
Valid percentages of a valid 66% of survey participants who supported a cannabis consultation prior to access and who thought that each of the specified professionals should carry out the screening.
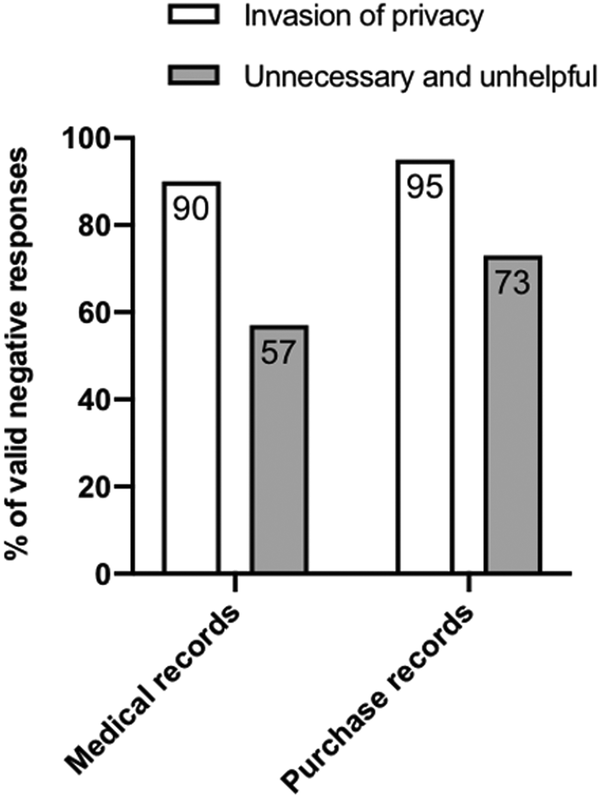
Figure 5
Percentage of valid negative responses which agreed medical records (53%) and cannabis purchase records (60%) being available online for pharmacists to view was an invasion of privacy and/or unnecessary and unhelpful.
Survey participants were subsequently asked, “For recreational users or users who want to access cannabis for therapeutic purposes but for which there is not enough supporting evidence for a doctor or specialist to prescribe cannabis; in order to access cannabis in pharmacies should the user have to pay to have a consultation with a private specialist doctor?”, however only 22% agreed. Fifty six percent agreed that it would be preferable to have a consultation with a regular NHS (tax funded) specialist, e.g. a GP.
Cannabis first use clinic
Forty eight percent of the (valid) survey participants agreed that there should be a specialist clinic where people can use cannabis for the first time.
Cannabis card
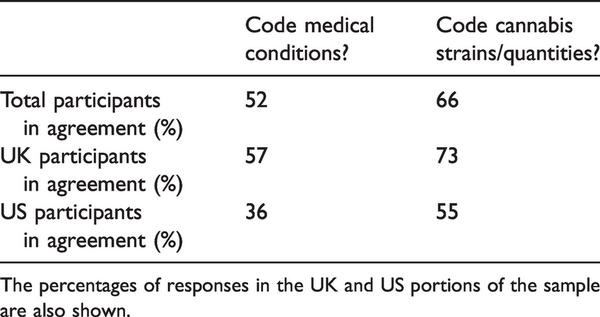
When asked if people who use cannabis could or should carry a card that could be presented in pharmacies to prove they can purchase cannabis, 57% of the participants agreed and within this, 64% of the UK participants and 52% of the US participants agreed. The 57% of total participants answered subsequent questions on this (Table 2).
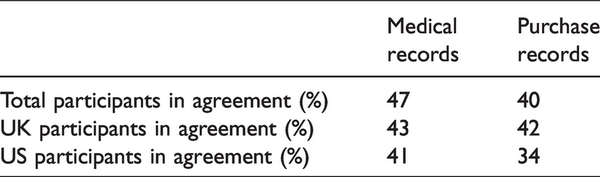
Medical and purchase records
The survey participants were asked if users’ medical and purchase records should be available online for pharmacists in a network (Table 3 and Figure 5). Of the total participants that answered the questions, 47% agreed that medical and 40% agreed that purchase records should be available (Table 3).
Methods of consumption
When asked whether cannabis should be sold in pharmacies in forms for vaporising and ingesting solely, and not for smoking, only 25% of participants agreed.
Pharmacy aesthetics
Participants were asked about the aesthetics of pharmacies that would sell cannabis, with 45% of the opinion that they should be sterile clinical environments and 35% agreeing that they could be completely stylised so that they are indistinguishable from “head shops”. However, the majority opinion was that the pharmacies could be somewhat stylised (65%).
Non-pharmacy vendors
When asked if pharmacies should be the only legal outlet for recreational use, 87% answered no. This 87% was then questioned on where cannabis should be sold (Figure 6).
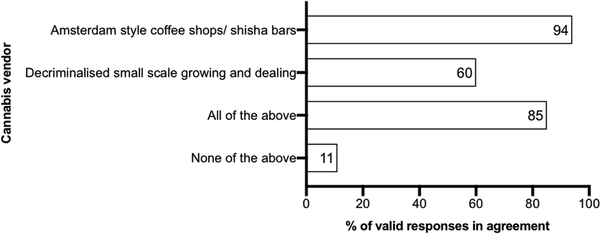
Figure 6
Participants were asked whether pharmacies should be the only legal outlet for non-medical cannabis sales, and 87% disagreed. This 87% were then questioned further on the type of cannabis vendor they would agree with and this is detailed on the graph. Valid responses are expressed as a percentage of this 87%.
Participants were additionally asked if Amsterdam style coffee shops or shisha bars were to exist for consuming cannabis in the UK, should they only be allowed to sell low-risk strains of cannabis (those approved to be sold in a healthcare environment e.g. a pharmacy). Only 35% of participants agreed and 26% were of the opinion that such bars should be part of a pharmacy chain of stores regulated by the pharmacy regulators.
Home cultivation
Participants were asked if cannabis were available in pharmacies should it also be legal to grow cannabis at home for a number of reasons (Figure 7).
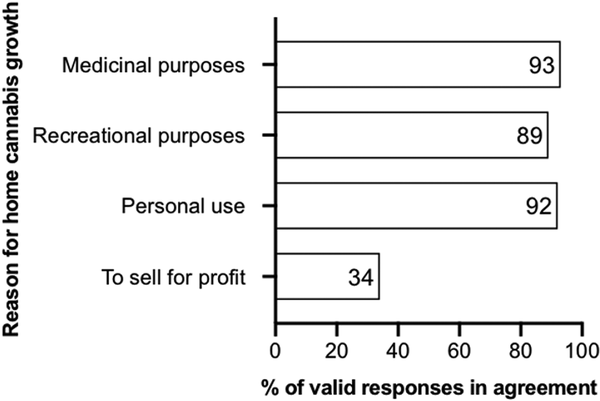
Figure 7
Percentage of survey participants in agreement with home cannabis cultivation for the specified reasons.
Public and private consumption
Ninety eight percent of the survey participants thought that it should be permissible to use cannabis at home. Participants were then questioned on its use in public (Figure 8).
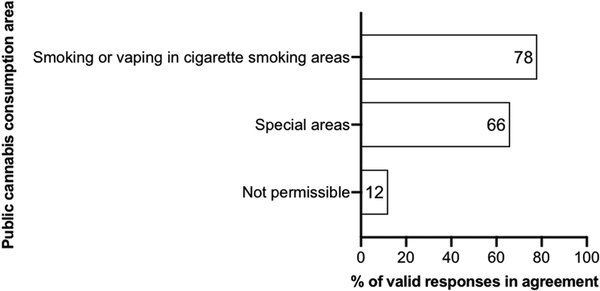
Figure 8
Percent of survey participants that agreed with the specified options on public cannabis consumption areas. Special areas include cannabis clubs, specialist bars and treatment centers.
Participant comments
Below are some selected participant comments. Incorrect spelling and grammar have been amended. Where participants used all capitals, this has been modified to italics. All original participant comments can be viewed in the online supplementary material.
Cannabis decriminalization is important, as well as the creation of standards of proper lab testing for such products and available public training about its properties and effects.
I believe it to be paramount in aiding our mental health crisis that is slowly sweeping the country. In an age where pharmaceutical choices are at the highest but side effects at their most dangerous, a natural universal alternative with minimal side effects should be considered without question. This to be combined with talking therapies grants untapped potential into healing and supporting our society and can't be ignored.
I believe that the decriminalisation of cannabis, and medical consultation by a mental health professional would be much more beneficial if caught in possession by the police- in a similar model to Portugal.
I have used cannabis for over 45 years in moderation recreationally and believe it has helped me manage pain and low moods. I do feel concern for young people using strong strains of weed. I believe cannabis has many therapeutic properties.
I’m a medicinal cannabis user and a trauma recovery therapist. The consumer experience of the medicinal user is my priority- controlling access is the overall concern but big mistake to try and micromanage adult medical users.
If taxed fairly and the population is re-educated about the benefits of medicinal cannabis, I can see a strong future for the UK and the NHS. Also, people should be allowed to grow cannabis at home for personal use. I really hope we can move forward progressively and create a system that works alongside our current healthcare system.
In terms of medical use: Individuals who wish to use cannabis therapeutically should be given the support from healthcare professionals. GPs could refer patients keen on trying cannabis for X medical condition to a specialist/consultant to determine whether it would be suitable for them. Pharmacies specialised for cannabis could then support this through dispensing the cannabis and monitor these patients. In terms of public and recreational use: The use of cannabis should be limited to specific areas and at home to reduce exposure to others. It should not be grown at home under any circumstances to ensure that cannabis strains and quality are kept regulated. If people were to use cannabis recreationally, they should not be adding more strain to healthcare. Rather their safe use should be controlled through cannabis product regulation.
Public consumption sites need to be adopted and implemented. In the United States we have legalized the consumption of cannabis in several states, but these states have not legalized consumption sites as well, which leads tourists (and there are many for cannabis) with no good location to consume their cannabis.
Any policy regarding recreational use of cannabis must be made with caution and not resemble past/current policy around cigarettes and alcohol. Regulating sales of recreational cannabis must be based upon its potential for addiction and the effect of its abuse on mental health.
As a victim of cannabis induced mental disorders such as dissociation and anxiety, patients should be properly examined.
As someone who has worked in the cannabis industry and has seen first hand the therapeutic value of the plant I think it’s essential for the allowed use of this substance. While I think it should be in some ways regulated for the healing properties, it should also be allowed to be grown at home. It’s a plant, let’s treat it as such.
Cannabis should be legalized in some contexts. It should certainly not be normalized, however it should be made available to those with an illness (under strict regulation and supervision).
Cannabis should be supplied in regulated pharmacies, bars and specific locales where users could choose strains that best fit their purposes. Everyone should be allowed to grow their own (of course, it's a plant!) but regulation should avoid an empowered black market.
Cannabis should never be legalised for non medicinal use and even then should only be prescribed for conditions such as epilepsy not for pain relief. Cannabis was a gateway drug for myself and lots of people I knew growing up, it had a detrimental effect on myself and many of my friends. Anything that would likely increase its acceptability and use among young people should be avoided at all costs.
Do not let pharma run the cannabis industry.
I really feel the public need more options in the management of chronic pain instead of just opiate-based painkillers.
I think people should be provided with the resources to make up their own minds about cannabis use. I think that there should be integration with health care for medical use as well as a free market for recreational use.
I would dislike big pharma having anything to do with cannabis.
It’s insane that a plant is illegal.
It should be allowed to grow for personal use up to 8 plants. If grown for profit, sales should be taxed.
It's long past time to legalise cannabis use. Both for harm reduction, tax base, and medical as well as recreational use. I barely use any more yet still feel strongly that legalisation can only improve many many lives, and reduce the strain on the legal and medical systems.
Please refer to best practices as they are emerging in legal US states such as Washington, Massachusetts, Colorado, California, Oregon, etc. Please take this seriously. Please recognize that humans have been consuming cannabis for generations with minimal negative consequences. Thank you.
The current situation is intolerable for people like myself who have to still resort to illegal usage with the risk of criminalisation it currently attracts.
Discussion
This study was designed to generate a model for a legal regulated market for cannabis in the UK. The results were obtained from a sample of experienced cannabis users and healthcare professionals from many countries with the majority being from the UK and the US. The sample is inherently biased as the study was advertised via the MAPS social media sites and monthly newsletter and most of the participants will therefore likely have a significant personal interest in psychedelics and cannabis. Whilst this choice of participant recruitment may result in a pro-cannabis selection bias, these participants may be more informed about cannabis and policies in various international jurisdictions. Engaging this group in the research is useful for developing a workable regulatory framework which is accepted by cannabis users. This is important to prevent an illicit market from remaining in the case of a change in regulation. It should be noted that, whilst the majority had used cannabis at least once in their life, participant responses indicated that many had concerns about the potential harms posed by cannabis and did not support complete deregulation.
The results can be summarised as follows: The majority of participants supported cannabis being legally available in pharmacies for medical use and for the purposes of reducing harms caused by recreational use. Participant answers and comments suggest that the current model of access to medicinal cannabis in the UK is ineffective and does not effectively assist patients who may benefit from accessing cannabis as a legal medicine (). A medical consultation prior to legally accessing cannabis from vendors was generally favoured; UK participants were particularly supportive of the use of cannabis cards to be presented to licensed vendors to verify their legal eligibility to purchase cannabis. The participants endorsed pharmacies being further integrated with mental health services to help with cannabis-related mental health issues. Interestingly, many participants also supported the existence of specialist locations such as shisha-type bars or Amsterdam style coffee shops for the sale and onsite consumption of cannabis and the participants preferred that these outlets were separate from pharmacies. Participants tended to support it being legal to grow a limited number of cannabis plants at home for personal consumption, for both medical and non-medical purposes. However, participants were not largely supportive of home-grown cannabis being sold for profit in unregulated markets (see participant comments). The participants’ comments regarding public consumption of cannabis suggested that the rules for smoking cannabis should be consistent with existing tobacco smoking legislation.
Almost all (valid 98%) of the respondents in this survey supported cannabis being available on prescription in pharmacies for therapeutic use. The respondents considered that there is sufficient evidence for cannabis to be prescribed to treat many conditions with the exception of schizophrenia. These results are not supportive of the current system regarding cannabis prescriptions in the UK. The participants appeared to favour a relatively relaxed regulatory system regarding cannabis prescriptions in contrast to the current system which, at the time of writing, is complex and caters to a very small number of patients ().
The participants did not agree upon the level of evidence which should be required in order for cannabis to be prescribed to treat specific medical conditions. As with the participants in this survey, this question has been found to cause disagreement amongst healthcare professionals (). Clinicians are hampered by a lack of clinically relevant information on the efficacy of cannabis, side effects and co-use with other medications such as opioids (; ; ). There are reports of possible cannabis-derived treatments for numerous physical and psychiatric disorders but the evidence for therapeutic efficacy is often weak (; ; ; ). Unlike completely novel small molecule therapeutics with an unknown safety profile and side effects, the safety profile of cannabis is comparatively well understood (). Consequently, the opinion that no specific evidence should necessarily be required in order to prescribe cannabis for a specific medical condition may have some merit as, unlike many clinically available therapeutics such as opioids, cannabis is relatively safe with few harmful side effects. Perhaps the results regarding the evidence base required for prescription could be interpreted to suggest that reliable evidence from clinical trials is preferable, however, doctors should be permitted to prescribe cannabis for medical conditions at their discretion – even if the evidence base is weak. Due to the difficulty of private companies to generate intellectual property (IP) and therefore profit from investing in clinical trials for treatments utilising herbal cannabis; either alternative funding strategies for clinical trials such as via non-profit or governmental organisations or a reduced evidence base requirement with adequate postmarket surveillance would facilitate greater access to cannabis as a prescribed medicine ().
Despite only a handful of UK residents currently possessing valid cannabis prescriptions (; ), 49% of UK respondents reported using cannabis for medicinal purposes (see online supplementary material). These results indicate that many people who use cannabis medicinally remain dependent on illicit markets to source their therapeutics. In this case, legal changes which were intended to grant patients with medical conditions access to cannabis based medicinal products still leave many in legally precarious situations. These results suggest that the current regulatory model functions poorly for patients whose condition and financial resources do not facilitate access to legal cannabis based medicines ().
A question was devised in the study in order to test the recreational-therapeutic crossover hypothesis alluded to in the introduction, and the results of this study regarding the cannabis use history of the participants (61% reported having used cannabis medically; 77% both recreationally and therapeutically; and 98% reported having used cannabis recreationally) are supportive of recreational-therapeutic crossover as these results indicate that medical and non-medical use are not mutually exclusive. These results further indicate that the current model for legal access to medicinal cannabis does not reflect the reality of cannabis use as a medicine. In light of the data obtained in the study the following two track access system can be proposed:
Conventional prescription
Recreational-therapeutic crossover and harm reduction
It is likely that the majority of people who would legally access cannabis would do so via the recreational-therapeutic crossover track which would be designed to enable access to cannabis as a medicine in cases where evidence of efficacy is insufficient to merit a prescription. However, medical healthcare professionals would not be liable for any lack of efficacy or harm occurred to individuals accessing cannabis via this route. This means of access to cannabis also would be designed to cover non therapeutic use and, as healthcare professionals, pharmacists’ role would be to minimise harms and highlight any potentially beneficial medical uses.
Eighty percent of the total sample, and 84% of UK respondents (see online supplementary material), preferred that pharmacies provide additional harm reduction services to those who use cannabis including the selling of cannabis for this purpose (; ; ; ). It is well-reported that cannabis use has been linked with mental illnesses such as psychosis and harm reduction services would be for the purpose of reducing the likelihood of the emergence of such disorders (; ; ). Whilst non-medical cannabis use can cause severe harm to the user, especially regarding mental illness, providing legal access to cannabis for non-medical use may effectively reduce overall recreational drug harms from other illicit and licit drugs used in a recreational context by providing a less harmful alternative (; ; ). Furthermore, allowing access to cannabis for medical purposes could be beneficial for reducing the harms of widely prescribed medications such as opioids which exhibit more severe side effects and negative consequences of use (; ). Synthetic cannabinoids can have more serious effects on health than naturally occurring phytocannabinoids and allowing access to phytocannabinoids could be an intervention to reduce the harm from synthetic cannabinoids by providing a safer alternative (; ; ; ).
Cannabis use has been associated with lower academic achievement in some consumers, increased odds of negative psycho-somatic and depressive symptoms, and reduced or inversely associated optimism, happiness and family satisfaction (). In light of this it is unsurprising that, of the 80% of participants who were supportive of pharmacies providing harm reduction services, 87% supported pharmacies aiding cannabis users by providing integrated mental health services to help monitor and reduce the likelihood of the emergence of cannabis-related mental health conditions such as psychosis (; ; ; ). Whilst greater integration of pharmacies with mental health services to help cannabis users would be a progressive change, it is unclear how this can be achieved utilising existing services. Pharmacists could provide an important gatekeeper role by signposting customers toward mental health services and providing information to people who use cannabis. A majority of participants were supportive of pharmacies offering onsite mental health services such as counselling and were also supportive of pharmacists being trained to deal with cannabis-related mental health issues (; ). These results are indicative of pharmacies expanding their role from predominantly focusing on physical ailments to also managing and dealing with issues relating to the mind by not only providing psychopharmacological therapies, but also complementary talking psychiatric therapies (see participant comments). A multi-agency response will likely be necessary to fulfill these requirements.
In the UK, most pharmacies are privately owned enterprises and can choose whether or not to provide harm reduction services such as needle-exchanges. Pharmacists may be concerned about displaying and selling products perceived as vice commodities or may be concerned about the perceptions of other customers who may be wary about the sale of cannabis (). Further development of a pharmacy retail model should therefore seek input from pharmacists to clarify their perspectives as medical professionals and businesses. The field of harm reduction is becoming a more frequent topic for debate amongst those who work in the healthcare profession. For example, the Royal Pharmaceutical Society has debated the sale of nicotine-based vaping products within pharmacies, particularly those which are not registered as medical devices, for assisting smoking cessation ().
Sixty six percent of participants supported a pre-sale consultation with a healthcare professional in order to purchase cannabis. Such a consultation would be for the purposes of determining the risks of cannabis use for a particular individual, focusing on the potential positive and negative effects of use (; ; ; ). Potential health professionals included GPs, cannabis specialist consultants, pharmacists and mental health workers. A specialist consultant was the preferred option (with 87% agreeing), this was followed by mental health professionals (80% agreeing), GPs (78% agreeing) and finally pharmacists (57% agreeing). These results suggest that the participants recognised that specialist knowledge of cannabis and its potential effects on physical and mental health would be of value in the consultation (). Existing NHS specialists are reportedly overworked and may be resistant to spending their time speaking with people so that they can access cannabis for non-medical use (). The results indicate the need for the creation of a new specialist role rather than adding this new work requirement to pre-existing healthcare professionals. As there are millions of self-reported cannabis users in the UK there is sufficient demand for such a specialism although how many jobs would be required and the specifics of the role remain speculative at this stage.
When asked about the funding of these consultations, over 50% of UK respondents stated that they would not want to pay directly for consultations. Instead, over 60% stated that this consultation should be paid for via taxation. The concept of tax-payers’ money being used to grant legal access to cannabis from licensed vendors for non-medical purposes could be politically controversial and undesirable to many members of the general public. However, an objective of a harm reduction approach towards cannabis regulation would be to encourage people to purchase cannabis from regulated licensed vendors and consequently prevent them using the black market. It has previously been proposed that government-funded cannabis interventions could at least in part be funded by a levy on all cannabis sales (). With an estimated market value of £2.6bn (), tax raised from cannabis sales may cover the costs of specialist consultations as well as contribute to the overall healthcare budget.
Participants were relatively ambivalent towards the concept of there being a clinic or supportive environment in which people use cannabis for the first time. Due to the safety profile of cannabis and generally low risks posed to health, the result of a slight majority of participants not supporting this concept was unsurprising. Such clinics are arguably not necessary for cannabis, though may be more suitable for substances with a greater potential for adverse reactions (e.g. MDMA) if they were to be sold by pharmacies for harm reduction purposes ().
UK participants were more supportive of the concept of a cannabis card than US participants and were also more supportive of specific recommendations such as strains being coded into the card for pharmacists to view. Whilst this UK-US difference was not statistically significant when subjected to chi-squared tests the slight dissimilarity perhaps reflects cultural differences. People in the US may be more likely to have libertarian views with greater resistance to government and private companies intervening in their lives (). Whilst a nation-wide cannabis card policy would likely not prove to be popular in the US, the results from this survey suggest that UK residents would be less resistant.
A proposed benefit of a cannabis card system is that the card would act as proof that the purchaser has spoken with relevant healthcare professionals and has some understanding of the potential risks cannabis could pose to their health (; ; ; ; ). Participants were somewhat supportive of personal recommendations such as strains being coded into the card although the proposal that the card could also have the individual’s medical conditions encoded was less well received. Information tailored to consumers could be coded into the card and could likely be continually updated as the consumer tries different strains and varieties of cannabis and finds what could be more beneficial, and also less beneficial, for them as individuals. Additionally, a card system could act as a deterrent for the emergence of drug tourism in which people would visit the UK for the purposes of buying cannabis for non-medical use. As previously discussed, drug tourism in the Netherlands has proven to be a contentious issue and many may wish to avoid the emergence of similar tourism in the UK.
The idea of users’ medical records and purchase records being available to pharmacists was met with resistance from the present sample on the grounds of an invasion of privacy. The questions were asked as such information could in theory help pharmacists to maximise therapeutic utility of cannabis and minimise harms. Also, information about frequency of purchases could make pharmacists aware if a particular individual is consuming cannabis so frequently as to give cause for concern. However, as no such provisions are in place for the purchase and sale of alcohol and tobacco, such a system could possibly feel unjustified and intrusive when these systems are not applied to more harmful drugs which are freely sold in regulated markets. Pharmacists may have to develop a more informal relationship based on trust and confidence rather than having the consumers’ personal information divulged to pharmacists without the patients’ explicit consent. Potentially, cannabis cards could have specified purchase limits encoded so that individuals are unable to buy more than a realistically consumable amount in a specific time frame; this would be in order to reduce the risks of people abusing the system and selling cannabis accessed in pharmacies on the black market ().
The sample widely disapproved of pharmacies only selling cannabis for the purposes of consuming via vaporising and ingesting. With the emergence of edibles and medibles, ingestion is a route of consumption of growing popularity (). Compared to traditional methods of consumption, ingestion results in a slower onset of effects and accurate dosing can be more difficult to achieve (; ). With this in mind, vaporising may be the recommended route of administration due to its lower potential for harm compared with smoking (). Whilst studies have suggested that smoked cannabis presents significantly less risk to health than smoked tobacco (; ; ; ), cannabis is often mixed with tobacco when smoked. As previously discussed, pharmacists should stress the importance of avoiding mixing cannabis with tobacco, which is more common in the UK than the US and Canada, as smoking cannabis with tobacco has additive adverse effects including addiction, increased risk of cardiovascular diseases and cancer ().
The present sample preferred that pharmacies that sell cannabis are somewhat stylised as opposed to head shop style environments or sterile clinical environments. Completely stylised head shop environments being significantly the least popular option was somewhat unexpected as over 60% of the participants in this survey were regular cannabis users and nearly all the sample had used cannabis at least once in their life. This suggests that cannabis users may prefer that cannabis ceases to be perceived as a counter-cultural substance and moves into the more mainstream medical field and is accepted by society as a whole. Indeed, most pharmacies could already be described as being somewhat stylised rather than sterile clinical environments as they are private enterprises which wish to attract customers. The results are indicative of the participants preferring that cannabis be sold in pre-existing pharmacies or, if pharmacies that specialise in cannabis are opened, that these differ little from the current aesthetics of a pharmacy environment.
Many participants supported the existence of complementary sites for purchase and consumption of cannabis in the style of Amsterdam coffee shops or UK-style shisha bars. The participants did not prefer these locations being part of a pharmacy chain of stores or regulated by pharmacy regulators. Additionally, the participants did not prefer that such locations are only permitted to sell strains which have been allocated as “low risk”. Whilst the primary objective of this survey was to further ascertain how the role of pharmacies could be adapted to cater for medicinal cannabis and harm reduction services, the relative popularity of shisha-type bars for onsite consumption is a result that should be considered. It is unlikely that pharmacies would be widely perceived to be a suitable location for onsite consumption – especially for non-medical use. Data from a previous survey suggested that some members of the general population are averse to the smell of cannabis and pre-existing smoking legislation would limit the number of legally permissible locations for cannabis consumption (). In addition, many landlords do not permit smoking on their property. Shisha-type bars could take into consideration the social and legal pressures on people who wish to use cannabis and grant them a suitable location for consumption.
In order to avoid the emergence of a competing market between shisha-type bars and pharmacies the price of cannabis in shisha-type bars should perhaps be higher than in pharmacies and cannabis must be consumed onsite. Due to the smell, contemporary laws regarding smoking in bars and other social factors it would likely be difficult to obtain a license to have a shisha-type bar which sells cannabis. Many cities, towns and villages across the UK have pre-existing pharmacies which could be adapted to supply cannabis, however, shisha-type bars would possibly be mainly located in urbanised areas and may generally not be the mainstream route of accessing cannabis. A possibility is that specialist cannabis dispensary pharmacies could have an associated shisha bar social club. The requirement to present a cannabis card could be applied across both types of vendor with information of the customer’s recommended strains possibly being updated upon visiting either of them.
Research suggests that enjoyment of listening to music is greater when under the effects of cannabis with CBD relative to cannabis containing trace or no CBD (b). This has been attributed to CBD modulating the dampening effects of THC on brain regions sensitive to reward and emotion. Consequently for an enjoyable experience in shisha-type bars and to offset some reported negative effects of THC, such as an increase in diastolic blood pressure and decreased response to music, while preserving or potentiating desirable effects, such as enhanced sound perception, cannabis with notable levels of CBD is recommended for use in shisha-type bars (b). Set and setting are highly influential on the subjective experiences of cannabis users and shisha-type bars and regulations thereof should account for this to minimise potential harms and increase positive, and ideally therapeutic, outcomes (). Ultimately, specific training will inevitably be required for all customer-facing staff working in shisha-type bars and such bars will require robust regulation and oversight (;).
The participants determined that it should be legal to grow a limited number of cannabis plants at home for personal medical and non-medical use but not to sell for profit (see comments). The participants’ preference that it not be legal to sell cannabis for profit is likely based on the assumption that such sales would be on the unregulated black market. Granting cannabis supply licenses to small-scale growers would allow pharmacies and shisha-type bars to be supplied by local producers. Shisha-type bars could incorporate aspects of cannabis social clubs and be supplied by local growers although the cannabis would have to be subject to regulatory oversight consistent with that of pharmacies and have adequate controls for potency and microbiological and pesticide screening to supply local vendors (; ; ).
A regulatory model which facilitates small-scale growers to supply vendors would enfranchise current black market growers who are often among marginalised populations to participate in the legal economy and allow economically-deprived communities to benefit from legalisation (). New markets could additionally provide income to developing countries such as Morocco (). Promoting local and international competition would reduce costs to the end-user whilst also preventing monopolistic practices by larger corporations which may use their economic leverage to distort policy priorities such as harm reduction and economic enfranchisement (). During legalisation in Massachusetts, lawmakers specifically legislated the granting of licenses to those previously convicted of cannabis-supply offences under its “Social Equity” program. This program has been credited with helping communities disproportionately affected by previous prohibitionist policies and allows those who qualify to access professional training opportunities and assistance in raising capital to ensure they are able to operate competitively under the new legal framework (). The Borland Regulated Market Model is a potential model for the production and supply of cannabis which would be consistent with these aims and encompasses manufacturers/importers, Cannabis Products Agency (government/health agency) and distribution to retail outlets. The aim of a governmental Cannabis Products Agency would be to control packaging, marketing prices and incentivise harm reduction with continual review of policies based on emerging evidence (;; ).
In the absence of legal access to cannabis there is a large demand for CBD-based products in the UK (). Provided that the level of THC does not exceed 0.2% these products are legal and widely available online from high street health food retailers and community pharmacies. This market has been estimated to be worth up to £1bn to the UK economy – indicating there is substantial interest in the potential health benefits of these products (). CBD has been implicated as a potential treatment for a range of conditions including addictions and as an anxiolytic but evidence is inconclusive and more research is needed (; ; ; ). At the time of writing, CBD products in the UK are poorly regulated and lack effective quality standards and are therefore of questionable medicinal value (). Moreover, a recent industry report found that many products sold in the UK contained no active components or were contaminated with heavy metals and solvents which exceed legal safety limits (). Given the size of the market and prevalence of use this issue requires addressing by legislators ().
Despite being mostly cannabis users themselves, several respondents commented that normalisation of drug use amongst young people could be an unintended consequence of cannabis legalisation (see participant comments). These concerns may be explained by persistent beliefs in the gateway hypothesis which proposes that cannabis use precedes that of “harder” drugs. Whilst some evidence suggests that this may be true for people experiencing psychiatric comorbidities, it should be noted that the hypothesis was developed during a time in which cannabis could only be accessed through black market sellers (). It has been suggested by third-sector organisations, researchers and MPs that legal regulation may instead protect cannabis users from using other drugs by reducing their contact with criminalised environments and exploitative black market sellers (; ; ).
In Colorado, which legalised recreational cannabis use in 2014, self-reported cannabis use amongst school-aged children was found to have not changed significantly according to two separate self-reporting surveys (). Research has suggested that ‘liberalisation’ does not lead to an increase in adolescent cannabis use and results in decreased youth arrests (; ). Objective examination of figures suggests that drug-related school suspensions, expulsions and referrals to law enforcement in fact decreased sharply from 2014/15 to 2015/16 and that this decrease occurred the year immediately following legalisation (Figure 9). These data suggest that legalisation beneficially impacts the lives of young people and protects against educational inequalities and criminalisation related to drug use. Zoning ordinances vary by locality but typically restrict cannabis dispensaries to being located within 1000 feet of schools (). Whilst there is a lack of evidence as to whether this is an effective deterrent to youth cannabis use, proximity of alcohol outlets has been associated with increased drinking frequency by Scottish adolescents (). To address public concerns of normalisation it may be beneficial for the UK to follow a similar zoning model and allow local communities, perhaps legislated at the devolved level, to decide rules on dispensary locations. At a national level, marketing controls similar to those which exist for tobacco products may also be utilised restricting advertisements, point of sale displays and stylised packaging. Early exposure to cannabis can have serious effects on cognitive functioning and many users who develop cannabis use disorders do so at a younger age than other substances such as alcohol. Therefore a minimum age requirement of 18 (consistent with tobacco and alcohol purchase laws in the UK) and monitoring of young people in particular seems prudent (; ; ; ; ; ; ).
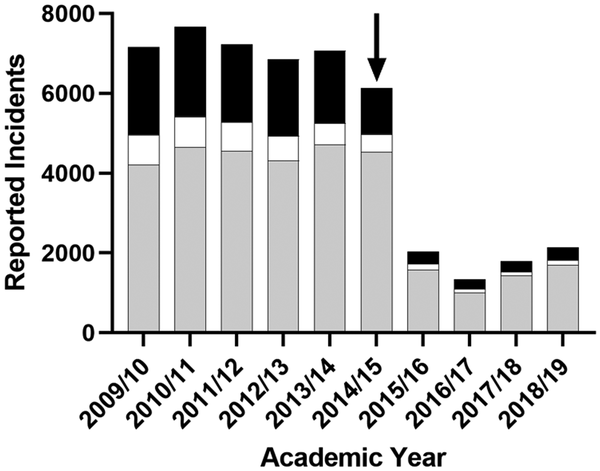
Figure 9
Reported incidents of drug-related school suspensions (grey), expulsions (white) and referrals to law enforcement (black) in Colorado from 2009–2019. Note the sharp decrease following legalisation of recreational cannabis use in 2014 (arrow). Data plotted from .
This study was designed to provide information to policy makers to help develop a rational series of legislative changes, however, it is well-known that scientific evidence and policy often have little relation to each other. In order for an effective regulatory system for cannabis to be enacted, issues regarding the gulf between scientific thinking and those who decide legislative changes need to be addressed (). A number of countries are developing regulated cannabis markets although global drug policy has been described as being at an impasse with organisations such as the United Nations being unable to agree internally upon appropriate action (). As such, there is plenty of reason to predict that the results in this survey will largely go ignored by legislators unless public pressure or a perceived change in public opinion sways government ministers to consider further changes to the law and health policy.
Future research in the area should involve the participation of healthcare professionals such as doctors and pharmacists to develop a model which is practical and consistent with the results in this study and preceding studies (, ). Despite the potential drawbacks of the present sample being biased (due to a large proportion of cannabis users), the results of this survey are indicative of a system that people who use cannabis would be able to work within and therefore help to resolve an issue which has distracted law enforcement for decades. Cannabis policy affects millions of people worldwide and as such it is an issue which requires global cooperation to resolve ().
Acknowledgements
This article is dedicated to the memory of Paul Flynn, MP for Newport West. The authors would like to thank the participants in addition to Martin Powell (Transform), Cristoph Klein and Nat Gissanadilok who provided information on the topic.
Declaration of conflicting interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material Supplemental material for this article is available online.
References
- Abouk R, Adams S (2018) Examining the relationship between medical cannabis laws and cardiovascular deaths in the US. International Journal of Drug Policy 53: 1–7.
- Abuhasira R, Schleider LBL, Mechoulam R, et al. (2018) Epidemiological characteristics, safety and efficacy of medical cannabis in the elderly. European Journal of Internal Medicine 49: 44–50.
- Addlesperger E (2015) Hemp. Journal of Agricultural & Food Information 16(3): 196–202.
- Aguinaco A, Barra A (2017) Cannabis for personal use in the supreme court of Mexico: Legal case and potential for policy change. International Journal of Drug Policy 50: 9–10.
- Aldington S, Williams M, Nowitz M, et al. (2007) Effects of cannabis on pulmonary structure, function and symptoms. Thorax 62(12): 1058–1063.
- All-Party Parliamentary Group for Drug Policy Reform (2016) Access to medicinal cannabis: Meeting patient needs. Available at: https://drive.google.com/file/d/1mx0Q33DCm4OsGnw3L3GDYpMHvwOq7nVw/view (accessed August 2019).
- Anderson DM, Rees DI, Tekin E (2018) Medical marijuana laws and workplace fatalities in the United States. International Journal of Drug Policy 60: 33–39.
- Andre CM, Hausman JF, Guerriero G (2016) Cannabis sativa: The plant of the thousand and one molecules. Frontiers in Plant Science 7: 19–17.
- Barnett RE (2009) The harmful side effects drug prohibition. Utah Law Review 1: 11–34.
- Barton C (2019) The battle for medicinal cannabis is a chronic pain in the heart. The Huffington Post. Available at: http://www.huffingtonpost.co.uk/entry/medicinal-cannabis-opioid-nice_uk_5d4c4398e4b09e729742e27c (accessed August 2019).
- Belackova V, Wilkins C (2018) Consumer agency in cannabis supply – Exploring auto-regulatory documents of the cannabis social clubs in Spain. International Journal of Drug Policy 54: 26–34.
- Bezinga. (2020). GW Pharmaceuticals receives positive NICE recommendation for EPIDYOLEX® (cannabidiol) oral solution for the treatment of seizures in patients with two rare, severe forms of childhood-onset epilepsy. Global Newswire. Available at: http://www.benzinga.com/pressreleases/19/11/g14775264/gw-pharmaceuticals-receives-positive-nice-recommendation-for-epidyolex-cannabidiol-oral-solution-f (accessed 14 July 2020).
- Bhattacharyya S, Morrison PD, Fusar-Poli P, et al. (2010) Opposite effects of Δ-9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology. Neuropsychopharmacology 35(3): 764–774.
- Bhattacharyya S, Wilson R, Appiah-Kusi E, et al. (2018) Effect of cannabidiol on medial temporal, midbrain, and striatal dysfunction in people at clinical high risk of psychosis: A randomised clinical trial. JAMA Psychiatry 75(11): 1107–1117.
- Booth JK, Page JE, Bohlmann J (2017) Terpene synthases from Cannabis sativa. PLoS One 12(3): e0173911–20.
- Borodovsky JT, Budney AJ (2017) Legal cannabis laws, home cultivation, and use of edible cannabis products: a growing relationship? International Journal of Drug Policy 50: 102–110.
- Bosely S (2019) Watchdog declines to back NHS cannabis treatment for epilepsy. The Guardian. Available at: http://www.theguardian.com/society/2019/aug/08/watchdog-declines-to-back-nhs-cannabis-treatment-for-epilepsy (accessed August 2019).
- Bowden G (2019) Woman growing her own medicinal cannabis has her plants confiscated by the police. The Huffington Post. Available at: http://www.huffingtonpost.co.uk/entry/medicinal-cannabis-carly-barton_uk_5cdd75f1e4b0b4728ba44490 (accessed August 2019).
- Brañas A, Barrigón ML, Garrido-Torres N, et al. (2016) U-shaped curve of psychosis according to cannabis use: New evidence from a snowball sample. Journal of Psychopharmacology 30(12): 1331–1338.
- Brancato A, Castelli V, Lavanco G, et al. (2020) In utero Δ9-tetrahydrocannabinol exposure confers vulnerability towards cognitive impairments and alcohol drinking in the adolescent offspring: Is there a role for neuropeptide Y? Journal of Psychopharmacology 34(6): 663–679.
- Brewster D (2018) The structured ambivalence of cannabis control in England & Wales. International Journal of Drug Policy 53: 125–132.
- Bruins J, Pijnenborg MGHM, Bartels-Belthuis AA, et al. (2016) Cannabis use in people with severe mental illness: The association with physical and mental health – A cohort study. A pharmacotherapy monitoring and outcome survey study. Journal of Psychopharmacology 30(4): 354–362.
- Buckner JD, Zvolensky MJ, Ecker AH, et al. (2016) Cannabis craving in response to laboratory-induced social stress among racially diverse cannabis users: The impact of social anxiety disorder. Journal of Psychopharmacology 30(4): 363–369.
- Burdette AM, Webb NS, Hill TD, et al. (2018) Religious involvement and marijuana use for medical and recreational purposes. Journal of Drug Issues 48(3): 421–434.
- Cambron C, Guttmannova K, Fleming C B (2017) State and national contexts in evaluating cannabis laws: A case study of Washington state. Journal of Drug Issues 47(1): 74–90.
- Caulkins J P, Bao Y, Davenport S, et al. (2018) Big data on a big new market: Insights from Washington state’s legal cannabis market. International Journal of Drug Policy 57: 86–94.
- Cerda M, Kilmer B (2017) Uruguay’s middle-ground approach to cannabis legalization. International Journal of Drug Policy 42: 118–120.
- Chouvy PA (2019) Cannabis cultivation in the world: Heritages, trends and challenges. Echogéo 48(48): 1–20.
- Chouvy PA, Macfarlane J (2018) Agricultural innovations in morocco’s cannabis industry. International Journal of Drug Policy 58: 85–91.
- Cohen D (2019) The cannabis debate: 63 per cent of Londoners think UK should follow Canada and make drug legal. The Evening Standard. Available at: http://www.standard.co.uk/news/uk/the-cannabis-debate-63-per-cent-of-londoners-think-uk-should-follow-canada-and-make-cannabis-legal-a4179291.html (accessed August 2019).
- Colorado Department of Education (2019) Suspension/expulsion statistics. Available at: http://www.cde.state.co.us/cdereval/suspend-expelcurrent (accessed March 2020).
- Colorado Springs (2014) Medical marijuana land use regulations. Coloradosprings.gov. Available at: https://coloradosprings.gov/sites/default/files/city_council/business_licensing_medical_marijuana_land_use_regulations.pdf (accessed March 2020).
- Cooke AC, Knight KR, Miaskowski C (2019) Patients’ and clinicians’ perspectives of co-use of cannabis and opioids for chronic non-cancer pain management in primary care. International Journal of Drug Policy 63: 23–28.
- Crippa JA, Zuardi AW, Martin-Santos R, et al. (2009) Cannabis and anxiety: A critical review of the evidence. Human Psychopharmacology 24(7): 515–523.
- Curran HV, Freeman TP, Mokrysz C, et al. (2016) Keep off the grass? Cannabis, cognition and addiction. Nature Reviews Neuroscience 17(5): 293–306.
- Davies SC, Powis S, Ridge K (2018) Cannabis-based products for medicinal use. Available at: http://www.england.nhs.uk/wp-content/uploads/2018/10/letter-guidance-on-cannabis-based-products-for-medicinal-use.pdf (accessed August 2019).
- de Faria SM, Fabricio DDM, Tumas V, et al. (2020) Effects of acute cannabidiol administration on anxiety and tremors induced by a simulated public speaking test in patients with Parkinson’s disease. Journal of Psychopharmacology 34(2): 189–196.
- Di Forti M, Quattrone D, Freeman TP, et al. (2019) The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): A multicentre case-control study. The Lancet Psychiatry 6(5): 427–436.
- Disa.com (2020) Map of marijuana legality by state. Available at: https://disa.com/map-of-marijuana-legality-by-state (accessed November 2020).
- Diver D (2019) People who bring medicinal cannabis into the UK should not have the drug confiscated, MPs say. The Telegraph. Available at: http://www.telegraph.co.uk/news/2019/07/02/people-bring-medicinal-cannabis-uk-should-not-have-drug-confiscated/ (accessed August 2019).
- ElSohly MA, Mehmedic Z, Foster S, et al. (2016) Changes in cannabis potency over the last 2 decades (1995–2014): Analysis of current data in the United States. Biological Psychiatry 79(7): 613–619.
- FDA (2020) Guidances and manuals on pharmaceutical quality. FDA.gov. Available at: http://www.fda.gov/drugs/pharmaceutical-quality-resources/guidances-and-manuals-pharmaceutical-quality (accessed January 2020).
- Freeman TP, Hindocha C, Green SF, et al. (2019) Medicinal use of cannabis based products and cannabinoids. British Medical Journal 365: 1–7.
- Freeman TP, Mehta MA, Neill JC, et al. (2018) Restrictions on drugs with medical value: Moving beyond stalemate. Journal of Psychopharmacology 32(10): 1053–1055.
- Freeman TP, Pope RA, Wall MB, et al. (2018b) Cannabis dampens the effects of music in brain regions sensitive to reward and emotion. International Journal of Neuropsychopharmacology 21(1): 21–32.
- Gage SH (2019) Cannabis and psychosis: Triangulating the evidence. Lancet Psychiatry 6(5): 364–365.
- Gallily R, Yekhtin Z, Hanuš L O (2018) The anti-inflammatory properties of terpenoids from cannabis. Cannabis and Cannabinoid Research 3(1): 282–290.
- Gibbs B, Yates A, Liebling J (2019) CBD in the UK. Available at: https://irp-cdn.multiscreensite.com/51b75a3b/files/uploaded/Exec%20Summary%20-%20CBD%20.pdf (accessed March 2020).
- Gittins R, Sessa B (2020) Can prescribed medical cannabis use reduce the harms of other more harmful drugs? Drug Science, Policy and Law 6: 205032451990006–205032451990004.
- Gobira PH, Lima IV, Batista LA, et al. (2017) N-arachidonoyl-serotonin, a dual FAAHand TRPV1 blocker, inhibits the retrieval of contextual fear memory: Role of the cannabinoid CB1 receptor in the dorsal hippocampus. Journal of Psychopharmacology 31(6): 750–756.
- Godlee F (2018) Medical cannabis on the NHS. British Medical Journal 362(1). k3357. doi:10.1136/bmj.k3357. Link – https://www.bmj.com/content/362/bmj.k3357
- Griffith ADD, Cohall DH (2018) Conceptualising a policy framework for the implementation of medical marijuana in the Caribbean territory of Barbados. Drug Science, Policy and Law 4: 205032451879634–205032451879638.
- Grucza RA, Vuolo M, Krauss MJ, et al. (2018) Cannabis decriminalization: A study of recent policy change in five U.S. states. International Journal of Drug Policy 59: 67–75.
- Haberkorn L (2016) A majority of pharmacists in Uruguay don’t want to sell pot, here’s why. The cannabist.co. Available at: http://www.thecannabist.co/2016/07/06/uruguay-marijuana-pharmacies/57627/ (accessed October 2020).
- Hall LH, Johnson J, Watt I, et al. (2016) Healthcare staff wellbeing, burnout, and patient safety: A systematic review. PLoS One 11(7): e0159015.
- Hartogsohn I (2017) Constructing drug effects: A history of set and setting. Drug Science, Policy and Law 3: 205032451668332–205032451668317.
- Hay GL, Baracz SJ, Everett NA, et al. (2018) Cannabidiol treatment reduces the motivation to self-administer methamphetamine and methamphetamine-primed relapse in rats. Journal of Psychopharmacology 32(12): 1369–1378.
- Hill KP, George TP (2019) Cannabis legalization in Canada: A crucial trial balloon. The Lancet Psychiatry 6(1): 5–6.
- Hill KP, Palastro MD, George TP (2019) Therapeutic cannabis use in 2018: Where do we stand? Lancet Psychiatry 6(2): 88–89.
- Hillig KW (2005) Genetic evidence for speciation in Cannabis (Cannabaceae). Genetic Resources and Crop Evolution 52(2): 161–180.
- Hobbs M, Patel R, Morrison PD, et al. (2020) Synthetic cannabinoid use in psychiatric patients and relationship to hospitalisation: A retrospective electronic case register study. Journal of Psychopharmacology 34(6): 648–653.
- Home Office (2018) Explanatory memorandum to the misuse of drugs (amendments) (cannabis and licence fees) (England, Wales and Scotland) regulations 2018. No. 1055. Available at: http://www.legislation.gov.uk/uksi/2018/1055/pdfs/uksiem_20181055_en.pdf (accessed August 2019).
- Hundal H, Lister R, Evans N, et al. (2018) The effects of cannabidiol on persecutory ideation and anxiety in a high trait paranoid group. Journal of Psychopharmacology 32(3): 276–282.
- Hurley R (2018) Cannabis, cannabis everywhere: UK to review medical cannabis policy as Canada plans imminent legalization for all uses. British Medical Journal 361: 1–3.
- Hurley R (2019) Medical cannabis: No NHS patients have benefited from law change, say campaigners. British Medical Journal 364: 1–2. Available at: http://www.bmj.com/content/364/bmj.l753 (accessed August 2019).
- Iuvone T, Esposito G, Esposito R, et al. (2004) Neuroprotective effect of cannabidiol, a non‐psychoactive component from Cannabis sativa, on β‐amyloid‐induced toxicity in PC12 cells. Journal of Neurochemistry 89(1): 134–141.
- Iyer R, Koleva S, Graham J, et al. (2012) Understanding libertarian morality: The psychological dispositions of self-identified libertarians. PLoS One 7(8): e42366.
- Jacobson S (2019) Britain’s first medicinal cannabis clinic opens in greater Manchester. The Guardian. Available at: http://www.theguardian.com/society/2019/mar/09/britains-first-medicinal-cannabis-clinic-opens (accessed August 2019).
- James E, Robertshaw TL, Pascoe MJ, et al. (2019) Using the pharmacy retail model to examine perceptions and biases of a UK general population sample towards regulation of specific psychoactive drugs. Drug Science, Policy and Law 5: 205032451987612–205032451987614.
- James E, Robertshaw TL, Westwell AD, et al. (2018) Pharmacies as potential providers of harm reduction services: A preliminary online survey. Drug Science, Policy and Law 4: 205032451876744–205032451876714.
- Jonnes J (1999). Hep-Cats, Narcs, and Pipe Dreams. Baltimore: John Hopkins University Press.
- Jonnes J (1999) Hep-Cats, Narcs, and Pipe Dreams. Baltimore: John Hopkins University Press.
- Kelly JF, Greene MC, Bergman BG (2018) Is recovery from cannabis use problems different from alcohol and other drugs? Results from a national probability-based sample of the United States adult population. International Journal of Drug Policy 53: 55–64.
- Kevin RC, Wood KE, Stuart J, et al. (2017) Acute and residual effects in adolescent rats resulting from exposure to the novel synthetic cannabinoids AB-PINACA and AB-FUBINACA. Journal of Psychopharmacology 31(6): 757–769.
- Klein A, Potter GR (2018) The three betrayals of the medical cannabis growing activist: From multiple victimhood to reconstruction, redemption and activism. International Journal of Drug Policy 53: 65–72.
- Korn L, Haynie DL, Luk JW, et al. (2018) Prospective associations between cannabis use and negative and positive health and social measures among emerging adults. International Journal of Drug Policy 58: 55–63.
- Lachenmeier D, Rehm J (2015) Comparative risk assessment of alcohol, tobacco, cannabis and other illicit drugs using the margin of exposure approach. Scientific Reports 5(1): 8126.
- Lake S, Kerr T, Buxton J, et al. (2020) Does cannabis use modify the effect of post-traumatic stress disorder on severe depression and suicidal ideation? Evidence from a population-based cross-sectional study of Canadians. Journal of Psychopharmacology 34(2): 181–188.
- Lamb N (2018) Cannabis (legalisation and regulation). House of Commons Hansard. Available at: https://hansard.parliament.uk/commons/2018-12-11/debates/55AA41F8-DA50-491F-B2AF-F7F22C8BD431/Cannabis%28LegalisationAndRegulation%29 (accessed March 2020).
- Lamb N, Rolles S, Barton M, et al. (2016). A framework for a regulated market for cannabis in the UK: Recommendations from an expert panel. Available at: https://d3n8a8pro7vhmx.cloudfront.net/libdems/pages/10794/attachments/original/1457398164/A_framework_for_a_regulated_market_for_cannabis_in_the_UK.pdf?1457398164 (accessed May 2020).
- Lankenau SE, Kioumarsi A, Reed M, et al. (2018) Becoming a medical marijuana user. International Journal of Drug Policy 52: 62–70.
- Lawn W, Freeman TP, Pope RA, et al. (2016) Acute and chronic effects of cannabinoids on effort-related decision-making and reward learning: An evaluation of the cannabis ‘amotivational’ hypothesis. Psychopharmacology 233(19–20): 3537–3552.
- Li HL (1973) An archaeological and historical account of cannabis in China. Economic Botany 28(4): 437–448.
- Lu E, Willits D, Stohr MK, et al. (2021) The cannabis effect on crime: Time-series analysis of crime in Colorado and Washington state. Justice Quarterly 38(4): 565–595.
- Lucas P, Baron EP, Jikomes N (2019) Medical cannabis patterns of use and substitution for opiods & other pharmaceutical drugs, alcohol, tobacco, and illicit substances; results from a cross-sectional survey of authorized patients. Harm Reduction Journal 16(1): 9–11. (1-
- Maij DLR, van de Wetering BJM, Franken IHA (2017) Cognitive control in young adults with cannabis use disorder: An event-related brain potential study. Journal of Psychopharmacology 31(8): 1015–1026.
- Manthey J (2019) Cannabis use in Europe: Current trends and public health concerns. International Journal of Drug Policy 68: 93–96.
- Martinez IF, Atuesta LH (2018) Mourning the dead: The impact of Mexico’s war on drugs on citizens’ depressive symptoms. International Journal of Drug Policy 60: 65–73.
- Masson K, Bancroft A (2018) Nice people doing shady things’: Drugs and the morality of exchange in the darknet cryptomarkets. International Journal of Drug Policy 58: 78–84.
- Mathis W (2018) U.K. doctors can prescribe cannabis now. They may not know how. Bloomberg. Available at http://www.bloomberg.com/news/articles/2018-11-01/u-k-doctors-can-prescribe-cannabis-now-they-may-not-know-how?fbclid=IwAR2_tZn676kHxiIiN4HSRT-YdF7K13VbYDjoBmPATg_-9rIM1Wp4C-dV8Jo (accessed August 2019).
- Mayor S (2019) WHO proposes rescheduling cannabis to allow medical applications. British Medical Journal 364(1). l574 doi:10.1136/bmj.l574, Link – https://www.bmj.com/content/364/bmj.l574
- McCusker P (2020) UK medicinal cannabis impasse – Companies won’t invest in clinical trials; medics only want clinical trials. Bussinesscann.com. Available at: https://businesscann.com/uk-medicinal-cannabis-impasse-companies-wont-invest-in-clinical-trials-medics-only-want-clinical-trials/ (accessed October 2020)
- Meacham MC, Ramo DE, Kral AH, et al. (2018) Associations between medical cannabis and other drug use among unstably housed women. International Journal of Drug Policy 52: 45–51.
- Memedovich KA, Dowset LE, Spackman E, et al. (2018) The adverse health effects and harms related to marijuana use: An overview review. CMAJ Open 6(3): E339–E346.
- Mercuri K, Terrett G, Henry JD, et al. (2018) Episodic foresight deficits in regular, but not recreational, cannabis users. Journal of Psychopharmacology 32(8): 876–882.
- Mokrysz C, Landy R, Gage SH, et al. (2016) Are IQ and educational outcomes in teenagers related to their cannabis use? A prospective cohort study. Journal of Psychopharmacology 30(2): 159–168.
- Morales-Muñoz I, Martinez-Gras I, Ponce G, et al. (2017) Psychological symptomatology and impaired prepulse inhibition of the startle reflex are associated with cannabis-induced psychosis. Journal of Psychopharmacology 31(8): 1035–1045.
- Nasehi M, Shahbazzadeh S, Ebrahimi-Ghiri M, et al. (2018) Bidirectional influence of amygdala β1-adrenoceptors blockade on cannabinoid signaling in contextual and auditory fear memory. Journal of Psychopharmacology 32(8): 932–942.
- National Academies of Sciences, Engineering, and Medicine (2017) The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington: The National Academies Press.
- Nia AB, Medrano B, Perkel C, et al. (2016) Psychiatric comorbidity associated with synthetic cannabinoid use compared to cannabis. Journal of Psychopharmacology 30(12): 1321–1330.
- Nicholls J (2019) Legalisation of cannabis in the UK would help protect cannabis users from harm. The Guardian. Available at: http://www.theguardian.com/commentisfree/2019/feb/15/legalisation-cannabis-protect-users-mental-health (accessed March 2020).
- Noble T (2016) More proof that British police no longer give a shit about weed. Vice. Available at: http://www.vice.com/en_uk/article/zn7zae/police-cannabis-legalisation-drop-arrests-uk (accessed January 2020).
- Nutt DJ (2020) Groundhog decade not brave new world. Drug Science, Policy and Law 6: 205032451989896.
- Nutt DJ, King LA, Phillips LD (2010) Drug harms in the UK: A multicriteria decision analysis. The Lancet 376(9752): 1558–1565.
- Ozturk H M, Erdogan M, Alsancak Y, et al. (2018) Electrocardiographic alterations in patients consuming synthetic cannabinoids. Journal of Psychopharmacology 32(3): 296–301.
- Palali A, van Ours JC (2017) Cannabis use and support for cannabis legalization. Empirical Economics 53(4): 1747–1770.
- Pardal M (2018) An analysis of Belgian cannabis social clubs’ supply practices: A shapeshifting model? International Journal of Drug Policy 57: 32–41.
- Parnes JE, Smith JK, Conner BT (2018) Reefer madness or much ado about nothing? Cannabis legalization outcomes among young adults in the United States. International Journal of Drug Policy 56: 116–120.
- Pereira TFPD, de Paula LD (2016) Drug tourism: General overview, case studies and new perspectives in the contemporary world. European Journal of Tourism, Hospitality and Recreation 7(3): 188–202.
- Philbin M M, Mauro P M, Santaella-Tenorio J, et al. (2019) Associations between state-level policy liberalism, cannabis use, and cannabis use disorder from 2004 to 2012: Looking beyond medical cannabis law status. International Journal of Drug Policy 65: 97–103.
- Piper BJ, DeKeuster RM, Beals ML, et al. (2017) Substitution of medical cannabis for pharmaceutical agents for paid, anxiety and sleep. Journal of Psychopharmacology 31(5): 569–575.
- Pollio A (2016) The name of cannabis: A short guide for nonbotanists. Cannabis and Cannabinoid Research 1(1): 234–238.
- Quaglio G, McGuinness M, Rübig P, et al. (2015) Building bridges between neuroscientific evidence and policy. The Lancet 14(3): 242–245.
- Reddon H, Fast D, DeBeck K, et al. (2019) Prevalence and correlates of selling illicit cannabis among people who use drugs in Vancouver, Canada: A ten-year prospective cohort study. International Journal of Drug Policy 69: 16–23.
- Reed JK (2018) Effects of marijuana legalization in Colorado. Available at: https://cdpsdocs.state.co.us/ors/docs/reports/2018-SB13-283_Rpt.pdf (accessed March 2020).
- Ribeiro LI, Ind PW (2016) Effects of cannabis smoking on lung function and respiratory symptoms: A structured literature review. Nature Partner Journals 26: 1–8.
- Rogeberg O (2018) Prohibition, regulation or laissez faire: The policy trade-offs of cannabis policy. International Journal of Drug Policy 56: 153–161.
- Rogeberg O, Bergsvik D, Phillips LD, et al. (2018) A new approach to formulating and appraising drug policy: A multi-criterion decision analysis applied to alcohol and cannabis regulation. International Journal of Drug Policy 56: 144–152.
- Russell C, Rueda S, Room R, et al. (2018) Routes of administration for cannabis use – Basic prevalence and related health outcomes: A scoping review and synthesis. International Journal of Drug Policy 52: 87–96.
- Russo E (2011) Taming THC: Potential cannabis synergy with phytocannabinoid-terpenoid entourage effects. British Journal of Pharmacology 163(7): 1344–1364.
- Russo E, Guy GW (2006) A tale of two cannabinoids: The therapeutic rationale for combining tetrahydrocannabinol and cannabidiol. Medical Hypotheses 66(2): 234–246.
- Sachs J, McGlade E, Yurgelun-Todd D (2015) Safety and toxicology of cannabinoids. Neurotherapeutics 12(4): 735–746.
- Sami MB, Bhattacharyya S (2018) Are cannabis-using and non-using patients different groups? Towards understanding the neurobiology of cannabis use in psychotic disorders. Journal of Psychopharmacology 32(8): 825–849.
- Sartim AG, Sales AJ, Guimaraes FS, et al. (2018) Hippocampal mammalian target of rapamycin is implicated in stress-coping behavior induced by cannabidiol in the forced swim test. Journal of Psychopharmacology 32(8): 922–931.
- Schipper R, Dekker M, de Haan L, et al. (2018) Medicinal cannabis (bedrolite) substitution therapy in inpatients with a psychotic disorder and a comorbid cannabis use disorder: A case series. Journal of Psychopharmacology 32(3): 353–356.
- Schlag AK, Hindocha C, Zafar R, et al. (2020) Cannabis based medicines and cannabis dependence: A critical review of issues and evidence. Journal of Psychopharmacology 35(7): 773–785. https://journals.sagepub.com/doi/10.1177/0269881120986393
- Secades-Villa R, Garcia-Rodrigues O, Jin CJ, et al. (2015) Probability and predictors of the cannabis gateway effect: A national study. International Journal of Drug Policy 26(2): 135–142.
- Setboonsarng C (2020) Thailand rolls out cannabis clinic based on traditional medicine. Reuters. Available at: http://www.reuters.com/article/us-thailand-cannabis-idUSKBN1Z50MI?fbclid=IwAR2yXl-u8enx9iEaD6bAsCKlhIEhT3tjJCnCmFrvM-dfjE-vBO3z55hSymA (accessed January 2020).
- Shahzad A (2018) Use of hemp fiber in textiles. Latest Trends in Textile and Fashion Designing 3(1): 271.
- Sischy J, Blaustein J (2018) Global drug policy at an impasse: Examining the politics of the 2016 United Nations general assembly special session. International Journal of Drug Policy 60: 74–81.
- Smith A (2019a) ECH makes moves toward facilitating medical cannabis importation in UK, EU. PharmaTimes Online. Available at: http://www.pharmatimes.com/news/ech_makes_moves_toward_facilitating_medical_cannabis_importation_in_uk,_eu_1288838 (accessed March 2020).
- Smith A (2019b) NICE to work with GW pharma after epidolex rejection. PharmaTimes Online. Available at: http://www.pharmatimes.com/news/nice_to_work_with_gw_pharma_after_epidiolex_rejection_1299577 (accessed November 2019).
- Snowden C (2018) IEA Discussion Paper No.90. Joint Venture. Estimating the Size and Potential of the UK Cannabis Market. London: Institute of Economic Affairs.
- Sohn E (2019) Weighing the dangers of cannabis. Nature. Available at: http://www.nature.com/articles/d41586-019-02530-7 (accessed January 2020).
- Stevens A (2018) Medical cannabis in the UK: Patients should not be criminalised for seeking benefits. British Medical Journal 363: 1–2.
- Stevens A (2019) Is policy ‘liberalization’ associated with higher odds of adolescent cannabis use? A re-analysis of data from 38 countries. International Journal of Drug Policy 66: 94–99.
- Stokes P R A, Egerton A, Watson B, et al. (2012) History of cannabis use is not associated with alterations in striatal dopamine D2/D2 receptor availability. Journal of Psychopharmacology 26(1): 144–149.
- Subritzky T (2018) Beyond deficit and harm reduction: Incorporating the spectrum of wellness as an interpretive framework for cannabis consumption. International Journal of Drug Policy 60: 18–23.
- Sumnall H (2019) Medicinal cannabis: Legalised yet impossible to access. Independent. Available at: http://www.independent.co.uk/life-style/health-and-families/health-news/medicinal-cannabis-legalised-access-marijuana-nhs-a8903051.html (accessed August 2019).
- Tashkin DP (2013) Effects of marijuana smoking on the lung. Annals of the American Thoracic Society 10(3): 239–247.
- Todd T (2018) The benefits of marijuana legalization and regulation. Berkeley Journal of Criminal Law 23(1): 100–119.
- Transform (2016) How to Regulate Cannabis: A Practical Guide. Transform Drug Policy Foundation, Link – https://www.amazon.co.uk/How-Regulate-Cannabis-Practical-Guide/dp/095564285X
- van den Elsen GAH, Tobben L, Ahmed AIA, et al. (2017) Effects of tetrahydrocannabinol on balance and gait in patients with dementia: A randomised controlled crossover trial. Journal of Psychopharmacology 31(2): 184–191.
- van Os J, Linscott RJ, Myin-Germeys I, et al. (2009) A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychological Medicine 39(2): 179–195.
- Vingerhoets WAM, Koenders L, van den Brink W, et al. (2016) Cue-induced striatal activity in frequent cannabis users independently predicts cannabis problem severity three years later. Journal of Psychopharmacology 30(2): 152–158.
- Wade NE, Bagot KS, Cota CI, et al. (2019) Orbitofrontal cortex volume prospectively predicts cannabis and other substance use onset in adolescents. Journal of Psychopharmacology 33(9): 1124–1131.
- Wall MB, Pope R, Freeman TP, et al. (2019) Dissociable effects of cannabis with and without cannabidiol on the human brain’s resting-state functional connectivity. Journal of Psychopharmacology 33(7): 822–829.
- Walsh F (2019) Cannabis meds: ‘I risk criminal record to help my child’. BBC News. Available at: http://www.bbc.co.uk/news/health-48283242 (accessed August 2019).
- Wang LN (2012) e-Cigarettes: Should pharmacists be helping to turn smokers into “vapers”? The Pharmaceutical Journal. Available at: http://www.pharmaceutical-journal.com/news-and-analysis/features/e-cigarettes-should-pharmacists-be-helping-to-turn-smokers-into-vapers/11105264.article?firstPass=false
- Watts G (2006) Cannabis confusions. British Medical Journal 332(7534): 175–176.
- Weissenborn R, Nutt DJ (2012) Popular intoxicants: What lessons can be learned from the last 40 years of alcohol and cannabis regulation? Journal of Psychopharmacology 26(2): 213–220.
- Wiens T, Lenk KM, Fabian LEA, et al. (2018) Law enforcement practices in the first two states in the U.S. to legalize recreational marijuana. International Journal of Drug Policy 61: 38–43.
- Wilkins C, Romeo JS, Rychert M, et al. (2018) Determinants of high availability of methamphetamine, cannabis, LSD and ecstasy in New Zealand: Are drug dealers promoting methamphetamine rather than cannabis? International Journal of Drug Policy 61: 15–22.
- Wilson RP, Bhattacharyya S (2016) Antipsychotic efficacy in psychosis with co-morbid cannabis misuse: A systematic review. Journal of Psychopharmacology 30(2): 99–111.
- Wood J (2018) Second chances: How ex-convicts are lighting up the cannabis industry. The Guardian. Available at: http://www.theguardian.com/society/2018/jul/19/massachusetts-marijuana-social-equity-program-ex-convicts (accessed March 2020).
- Yates D, Speer J (2018) Over and under-regulation in the Colorado cannabis industry – A data-analytic perspective. International Journal of Drug Policy 59: 63–66.
- Yeung P (2020) Medical cannabis and the ongoing fight for access. Raconteur. Available at: http://www.raconteur.net/healthcare/medical-cannabis-nhs (accessed April 2020)
- Young R, Macdonald L, Ellaway A (2013) Associations between proximity and density of local alcohol outlets and alcohol use among Scottish adolescents. Health Place 19(100): 124–130.
- Zafar RR, Schlag AK, Nutt DJ (2020) Ending the pain of children with severe epilepsy? An audit of the impact of medical cannabis in 10 patients. Drug Science, Policy and Law 6: 205032452097448–205032452097446.
- Zolotov Y, Vulfsons S, Zarhin D, et al. (2018) Medical cannabis: An oxymoron? Physicians’ perceptions of medical cannabis. International Journal of Drug Policy 57: 4–10.
- Zuardi AW (2006) History of cannabis as a medicine: A review. Revista Brasileira de Psiquiatria (Sao Paulo, Brazil: 1999) 28(2): 153–157.