Introduction
Transcatheter aortic valve implantation (TAVI) has increased in recent years with rates now exceeding those of surgical aortic valve replacement (SAVR)., Whilst the expanding indications for TAVI are supported by evidence, there are variations in the delivery of TAVI care across the European Society of Cardiology (ESC) member countries, with an overall procedural volume ranging from 0.6 to 200 per million people. National registries have played an important role in exploring the patterns of TAVI care and outcomes. However, heterogeneity in design and delivery of TAVI registries limits the robust investigation of the effectiveness and safety of novel TAVI devices and adjunctive medications across countries.
There is a lack of standardized definitions for TAVI registry variables. Even though the Valve Academic Research Consortium (VARC) provides endpoint definitions for heart valvular interventions including TAVI, the definitions of clinical outcomes vary between TAVI studies., Besides, VARC harmonizes outcome definitions, but there remains a need to standardize the methods by which the processes of TAVI care delivery are captured. Such a harmonization across TAVI registries, randomised controlled trials (RCTs), and quality improvement initiatives, improves the efficiency of data collection and help generate new knowledge relevant to TAVI. The American College of Cardiology (ACC) and the American Heart Association (AHA) have developed data standards for a range of cardiovascular diseases, but no ACC/AHA data standards exist for TAVI.
The European Unified Registries On Heart Care Evaluation and Randomised Trials (EuroHeart) is an ESC initiative that aims to improve the quality of cardiovascular care through the continuous capture of individual patient data by standardizing the definitions of variables and offering a common IT platform for data collection, analysis, and reporting. To date, EuroHeart has developed data standards for acute coronary syndrome and percutaneous coronary intervention (PCI), heart failure and atrial fibrillation. This document presents the EuroHeart data standards for TAVI, which have been developed in collaboration with the European Association of Percutaneous Cardiovascular Interventions (EAPCI), the European Association of Cardiovascular Imaging (EACVI) and the Working Group on Cardiovascular Surgery of the ESC.
Methods
The Data Science Group of EuroHeart was established in August 2019. It comprises a project chair (C.G.), two medical experts (S.A. and G.B.), a biostatistician (J.W.) and a project manager.
Working group and reference group
The Working Group for the development of the 2022 EuroHeart data standards for TAVI included 29 members from 12 countries. The Group comprised members of the EuroHeart Data Science Group and nominees from the EAPCI, EACVI and the Working Group on Cardiovascular Surgery, as well as leaders of existing TAVI registries and a patient representative. Further 19 experts from 18 countries formed the Reference Group (Acknowledgment) and provided feedback on the selection and definitions of the included variables in the EuroHeart TAVI dataset.
European Unified Registries On Heart Care Evaluation and Randomised Trials data standards methodology
We followed the EuroHeart methodology for cardiovascular data standard development. In brief, this involved: (1) identification of the cardiovascular domain for the development of data standards; (2) conduction of a systematic review of the literature to synthesise a list of ‘candidate’ variables; (3) selection and prioritisation of variables by domain experts using a modified Delphi method; (4) Reference Group feedback, and (5) programming the final data variables into the EuroHeart IT platform.
Variable level
In EuroHeart, variables are classified as Level 1 variables if they are needed for the assessment of the quality of care (for example, information that would be required for the calculation of quality indicators), risk stratification, case-mix adjustment, or clinical outcomes. The Level 1 variables are defined in the EuroHeart data standard documents and are programmed into the EuroHeart IT platform.
Level 2 variables collect information that may prove useful for quality assessment and observational, or randomised research, but which may not be universally available, routinely used, or a pre-requisite for the evaluation of quality. The Level 2 variables are defined in the EuroHeart data standard documents but are not implemented into the EuroHeart IT platform.
For the countries which adopt the EuroHeart IT platform, a third level of variables can be programmed into the platform to address unique centre- or country-specific requirements. Thus, the Level 3 variables are not defined in the EuroHeart data standard documents. EuroHeart aims to align international data collection activities and therefore countries with existing registries may not choose to implement the EuroHeart IT platform, but harmonize their data standards with the EuroHeart variables.
Scope
The Working Group agreed that the EuroHeart-TAVI registry should capture pre-procedural care processes as well as procedural details, in-hospital events and follow up data. As far as possible, the data definitions were aligned with these collected in other EuroHeart registries including heart failure, acute coronary syndrome, PCI and atrial fibrillation, allowing re-utilization of existing information and avoiding duplication in different registries. Thereby, the TAVI registry may, especially in the EuroHeart IT-platform, be integrated with these databases to form a unified system for data collection and quality improvement (Figure 1).
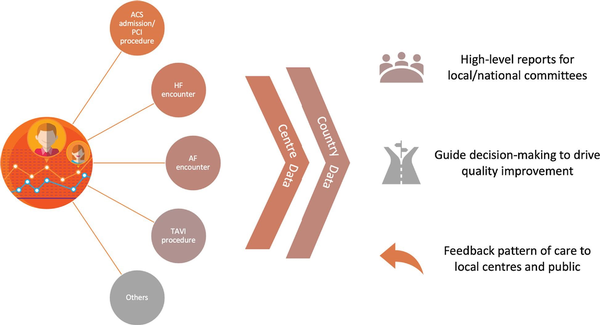
Figure 1
Role of EuroHeart registries in monitoring individual patients care. ACS, acute coronary syndrome; AF, atrial fibrillation; HF, heart failure; PCI, percutaneous coronary intervention; TAVI, transcatheter aortic valve implantation.
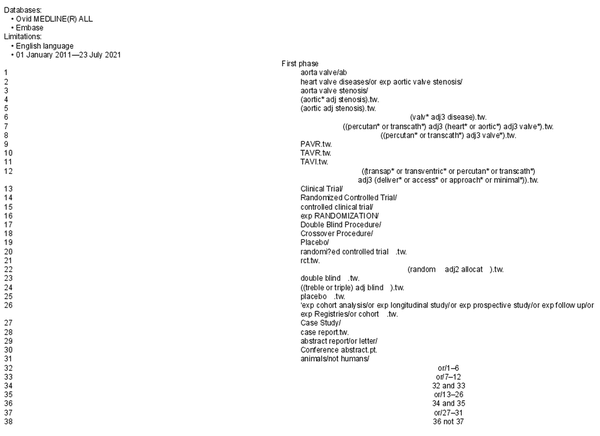
Systematic literature review
The EuroHeart Data Science Group conducted a systematic review of the literature to identify a list of candidate variables for potential inclusion in the EuroHeart TAVI dataset. The search included two databases (Embase and MEDLINE via OVID®) and captured peer reviewed RCTs and prospective observational studies that provided definitions for at least one variable relevant to TAVI diagnosis, management, or outcomes published between 01 January 2011 and 23 July 2021 (Appendix). Two reviewers (SA and GB) assessed retrieved articles against a pre-specified eligibility criteria and extracted potential variables from included studies. Existing TAVI registries and Clinical Practice Guidelines were also reviewed for potential data variables relevant to TAVI.
Selection of the final set of variables
Using a modified Delphi method, the Working Group voted on the list of candidate variables that were identified from the literature review. In total, two voting rounds and nine virtual meetings were conducted between April 2021 and January 2022, with a large volume of e-mail correspondence between meetings. The EuroHeart criteria for data standard development (importance, evidence base, validity, reliability, feasibility and applicability) were used to guide the selection process. The Working Group members voted on each of the candidate variables with include as Level 1, include as Level 2 or exclude. Variables achieved ≥75% agreement were included whilst those did not were carried to a second voting round and discussed in the subsequent meetings. The final set of variables was presented to the Reference Group for feedback on their validity and feasibility.
Implementation
After arriving at the final set of variables, the Data Science Group collaborated with the Registry Technology groups of the EuroHeart project to programme the Level 1 variables into the EuroHeart IT platform. The variables were structured in a chronological order from the pre-procedural details to the outcomes of TAVI. The platform was designed to improve the data entry consistency and reduce the burden of data entry.
Results
The systematic review retrieved 3225 articles. Of these, 372 met the inclusion criteria and were used to extract candidate variables. Following the modified Delphi method, 93 Level 1 variables (Supplementary material online, Table S1) and 113 Level 2 variables (Supplementary material online, Table S2) were selected for 10 domains of TAVI care.
The domains of care in the EuroHeart TAVI registry are: (1) Demographics, (2) Patient characteristics and comorbidities, (3) Health-related quality of life, (4) Prior interventions, (5) Presentation details, (6) Pre-procedural tests, (7) Procedural details, (8) Outcomes, (9) Discharge details and (10) Follow up.
Demographics
This domain is purposefully aligned with the EuroHeart registries for acute coronary syndrome-PCI, heart failure and atrial fibrillation., This reduces the amount of data that is needed to be entered for patients who are enrolled in more than one EuroHeart registry. The domain captures patient-identifiable information to allow data linkages (Supplementary material online, Table S1) and is therefore only stored at the local centre or at country-level in accordance with the each country's data-sharing regulations. De-identified, aggregated data may be shared with the EuroHeart Data Science Centre to create high-level reports following agreements from relevant parties (Supplementary material online, Table S1).
Patient characteristics and comorbidities
This domain contains information about the patient's characteristics (e.g. height and weight) at the time of hospital admission for the TAVI procedure. Baseline comorbidities (e.g. heart failure) and prognostic variables (e.g. frailty) are also captured because of the role of such variables in risk adjustment models and risk stratification scores for TAVI outcomes. Although the definitions of the variables are the same as those in the other EuroHeart registries, the domain also records TAVI specific variables such as the assessment of aortic calcification (Supplementary materials online, Tables S1 and S2).,
Health-related quality of life
Patient health-related quality of life (HRQoL) is important prior to invasive procedures, but its systematic collection in routine clinical practice is difficult. Thus HRQoL has been included as Level 2 variable in the EuroHeart-TAVI data standards (Supplementary material online, Table S2).
Prior interventions
This domain captures information about aortic valve or other cardiac interventions (e.g. PCI) prior to the TAVI procedure (Supplementary materials online, Tables S1 and S2). The collection of information about prior SAVR and TAVI procedures contributes to the understanding of the characteristics and outcomes following valve-in-valve procedures given that TAVI in failed surgical bioprosthetic valves is now an established treatment and TAVI-in-TAVI may become an important treatment in the future.
Presentation details
This domain includes information about a patient's clinical status at the time of admission to hospital. It includes the presenting symptoms, New York Heart Association (NYHA) class and some ECG parameters (Supplementary material online, Tables S1). The EuroHeart TAVI data standards enables patient risk stratification from the submitted variables and allows the entry of the EuroSCORE II (Supplementary material online, Table S1). Data about cardiogenic shock, the Canadian Cardiovascular Society (CCS) grade of angina and the Society of Thoracic Surgeons (STS) score are included as Level 2 variables (Supplementary material online, Table S2).
Pre-procedural tests
The ESC guidelines recommend an assessment of coronary artery disease prior to invasive valve intervention. This domain collects information about concomitant coronary artery disease prior to a TAVI procedure, as well as biochemical (e.g. haemoglobin, creatinine) and echocardiographic parameters (e.g. left ventricular ejection fraction, mean aortic valve gradient) prior to the procedure (Supplementary material online, Table S1). Information concerning the extent of aortic, leaflet and left ventricular outflow tract calcification are captured in this domain in addition to concomitant valvular (e.g. mitral) disease (Supplementary material online, Table S1). A selection of the Level 1 variables is shown in Figure 2.
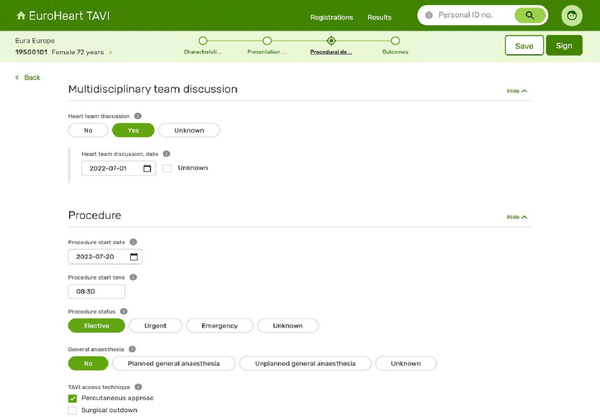
Figure 2
An illustration of the IT platform. AV, aortic valve; LAD, left anterior descending artery; Lcx, left circumflex artery; LMS, left main stem; RCA, right coronary artery.
Procedural details
The specifications of the TAVI procedure are captured in this domain including the date of the procedure, type of anaesthesia, access site and valve types used (Supplementary material online, table S1). This domain collects information such as the planned concomitant interventions (e.g. PCI) as well as the use of cerebral embolic protection and/or vascular closure devices (Supplementary material online, Table S1). Procedural events are included in this domain as Level 1 variables (Supplementary material online, TableS1) with additional details (e.g. pacing, circulatory support) as Level 2 (Supplementary material online, Table S2).
In-hospital data
This domain captures the findings from echocardiography undertaken after the TAVI procedure and before hospital discharge (Supplementary material online, Table S1). In-hospital events that occur after the TAVI procedure are also recorded here. These events include cardiac interventions during the same admission, in-hospital myocardial infarction, stroke, bleeding or death (Supplementary material online, Table S1). The definitions of these events are aligned with the VARC-3 criteria.
Discharge details
This domain records information about antithrombotic therapy and some ECG findings at the time of discharge from hospital (Supplementary material online, Table S1). Biomarkers (e.g. haemoglobin, creatinine) other medications and referral for cardiac rehabilitation are included as Level 2 variables (Supplementary material online, Table S2).
Follow up
All of the variables in this domain are Level 2. This is because concerns were raised about the feasibility of efficiently collecting patient information beyond the hospital stay. The domain defines variables to be collected after hospital discharge and specifies the intervals for their collection (Structured Graphical Abstract).
Discussion
The EuroHeart data standards for TAVI processes of care and in-hospital outcomes comprise 93 mandatory (Level 1) and 113 optional (Level 2) variables across 10 TAVI domains. They set forth an internationally agreed and ESC endorsed standards for the conduct of observational studies and RCTs that are relevant to TAVI, provide a platform for monitoring the effectiveness and safety of new devices and treatment strategies, and align with published EuroHeart data standards for other cardiovascular diseases., The standardisation of the definitions of TAVI-related data variables enables the conduction of international comparative analyses and facilitates the development of a comprehensive registry for various forms of valvular heart disease regardless of its treatment strategy.
Despite previous efforts, there remains a need for a harmonised, internationally endorsed and feasible set of data standards for TAVI encompassing both processes of care and key outcomes., For instance the ACC and the Society of Thoracic Surgeons (STS) Transcatheter Valve Therapy (TVT) registry comprises 216 variables, 160 of which are mandatory. To reduce the burden of data collection, a recent collaboration between various stakeholders in the US was established to develop a ‘Minimum Core Data Elements' for TAVI. However, this dataset defined 132 mandatory variables and maintained an additional 35 variables as mandatory in the ACC/STS TVT registry increasing the total number to 167. Moreover, the definitions of the variables in the updated ACC/STS TVT registry have not been fully aligned with these in other relevant registries. For example, the definition of cerebrovascular disease varies between the ACC PCI and TVT registries limiting the opportunity to combine data from different resources.
In Europe, national registries had an important role in illustrating the patterns of TAVI care and understanding its outcomes. However, the heterogeneity in the data standards between these registries hampers the conduction of pragmatic registry-based RCTs (R-RCT) and the performance of post-marketing surveillance of new TAVI technologies across borders. Furthermore, the lack of harmonisation between national TAVI registries and existing databases for other cardiovascular diseases (e.g. PCI) results in redundancy and unnecessary duplication of healthcare data collection. EuroHeart provides an umbrella under which standardised data definitions are developed and harmonised across various cardiovascular disease domains.
The data standards for TAVI presented in this document have been developed in collaboration with the EAPCI the EACVI and the ESC Working Group on Cardiovascular Surgery and with involvement of a patient representative. Furthermore, the definitions of the selected variables were aligned with the ESC guidelines for valvular heart disease and the VARC endpoints., Consequently, these standards were endorsed by the ESC Association of Cardiovascular Nursing and Allied Professions (ACNAP) and the ESC Committee for Young Cardiovascular Professionals, highlighting their potential role in evaluating and addressing the variation in TAVI care and outcomes within and between countries.,
Developing internationally recognised standards for data collection may not necessarily guarantee their uptake in practice. For instance, the VARC clinical endpoints which aimed to harmonize the methods by which TAVI outcomes are defined have not been adopted in over 40% of TAVI studies., This may be explained by the need to integrate process variables with outcomes in a single system, which the VARC lacks. Additionally, the implementation of the developed variables into a web-based interface may facilitate the uptake of the data collection system. The EuroHeart-TAVI data standards comprise key processes and in-hospital outcomes as Level 1 variables which are embedded into an IT platform, with additional variables that capture follow up data as Level 2. We anticipate that the EuroHeart-TAVI registry will provide the means for a wider valvular heart disease registry that capture data relevant to various treatment strategies.
We recognise that countries may be interested in adopting the EuroHeart definitions and not implementing the EuroHeart-IT platform. Those countries can, of course, use the data standards presented in this document and modify their existing registries accordingly. Whilst long-term follow up outcomes are developed as Level 2 variables in the EuroHeart-TAVI dataset, harmonized clinical outcomes will be an integral component of the EuroHeart Data Standards for Clinical Outcome module which is currently under development. Adjudication of the imaging parameters or outcomes can be implemented to serve a future R-RCT that is conducted using the EuroHeart-TAVI IT platform. We acknowledge that the EuroHeart standards are not mapped to an electronic health record coding system that facilitates their syntactic interpretation—presently, this is beyond the remit of EuroHeart. The EuroHeart methodology relies on expert opinion to select the final set of variables and therefore may have been influenced by the participant bias. However, inclusiveness of the Working and Reference Groups, and the use of a modified Delphi method enabled the standardization of the selection process.
Conclusions
The EuroHeart data standards for TAVI processes of care and in-hospital outcomes are an internationally agreed and ESC endorsed set of standards that may be used for the conduct of observational studies, RCTs and TAVI devices surveillance. In total, 93 mandatory Level 1 variables are programmed into the EuroHeart IT platform and provide the core TAVI dataset.
Acknowledgements
We thank the ESC Association of Cardiovascular Nursing & Allied Professions (ACNAP), the ESC Patient Forum, the ESC Committee for Young Cardiovascular Professionals for their endorsement of the EuroHeart Data Standards for TAVI.
We also thank the following experts for being part of the Reference Group for the 2022 EuroHeart Data Standards for TAVI:
Vilhelmas Bajoras (Lithuania), Darko Boljevic (Serbia), Haim Danenberg (Israel), Nicolas Dumonteil (France), Andrejs Erglis (Latvia), Alan Fraser (UK), Ingibjorg J. Gudmundsdottir (Iceland), Raban Jeger (Switzerland), Gudrun Lamm (Austria), Ivo Petrov (Bulgaria), Elton Pllaha (Malta), Andreas Rück (Sweden), Magnus Settergren (Sweden), Oleg Polonetsky (Belarus), Peter Smits (Netherland), Nikoly Stoyanov (Bulgaria), Konstantinos Toutouzas (Greece), Wojciech Wojakowski (Poland), Jonathan Yap (Singapore).
Finally, we thank Dr Benjamin Beska and Dr Tanina Younsi for their help with the systematic review of the literature.
Appendix
References
- 1. Carroll JD, Mack MJ, Vemulapalli S, Herrmann HC, Gleason TG, Hanzel G, et al STS-ACC TVT Registry of Transcatheter Aortic Valve Replacement. Ann Thorac Surg. 2021;111:701–722.
- 2. NATIONAL CARDIAC AUDIT PROGRAMME. ANNUAL REPORT 2021. Available at: https://www.nicor.org.uk/wp-content/uploads/2021/10/NCAP-Aggregate_-Report_2021_FINAL.pdf. Accessed 26 April 2022.
- 3. Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al 2021 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021;43:561–632.
- 4. Barbato E, Noc M, Baumbach A, Dudek D, Bunc M, Skalidis E, et al Mapping interventional cardiology in Europe: the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Atlas Project. Eur Heart J. 2020;41:2579–2588.
- 5. Bekeredjian R, Szabo G, Balaban Ü, Bleiziffer S, Bauer T, Ensminger S, et al Patients at low surgical risk as defined by the Society of Thoracic Surgeons Score undergoing isolated interventional or surgical aortic valve implantation: in-hospital data and 1-year results from the German Aortic Valve Registry (GARY). Eur Heart J. 2019;40:1323–1330.
- 6. Blackman DJ, Saraf S, MacCarthy PA, Myat A, Anderson SG, Malkin CJ, et al Long-Term Durability of Transcatheter Aortic Valve Prostheses. J Am Coll Cardiol. 2019;73:537–545.
- 7. Nilsson K, Buccheri S, Christersson C, Koul S, Nilsson J, Pétursson P, et al Causes, pattern, predictors, and prognostic implications of new hospitalizations after transcatheter aortic valve implantation: a long-term nationwide observational study. Eur Heart J Qual Care Clin Outcomes. 2022;8:150–160.
- 8. Beyersdorf F, Bauer T, Freemantle N, Walther T, Frerker C, Herrmann E, et al Five-year outcome in 18 010 patients from the German Aortic Valve Registry. Eur J Cardiothorac Surg. 2021;60:1139–1146.
- 9. Dawson LP, Biswas S, Lefkovits J, Stub D, Burchill L, Evans SM, et al Characteristics and Quality of National Cardiac Registries: A Systematic Review. Circ Cardiovasc Qual Outcomes. 2021;14:e007963.
- 10. COMMITTEE V-W, Généreux P, Piazza N, Alu MC, Nazif T, Hahn RT, et al Valve Academic Research Consortium 3: updated endpoint definitions for aortic valve clinical research. Eur Heart J. 2021;42:1825–1857.
- 11. Zhang S, Kolominsky-Rabas PL. How TAVI registries report clinical outcomes-A systematic review of endpoints based on VARC-2 definitions. PLoS One. 2017;12:e0180815.
- 12. Erlebach M, Head SJ, Mylotte D, Leon MB, Serruys PW, Kappetein AP, et al VARC endpoint definition compliance rates in contemporary transcatheter aortic valve implantation studies. EuroIntervention. 2016;12:375–380.
- 13. ACC/AHA Clinical Data Standards. Available at: https://www.jacc.org/guidelines/data-standards. Accessed 01 December 2021.
- 14. Batra G, Aktaa S, Wallentin L, Maggioni AP, Ludman P, Erlinge D, et al Data standards for acute coronary syndrome and percutaneous coronary intervention: the European Unified Registries for Heart Care Evaluation and Randomised Trials (EuroHeart). Eur Heart J. 2022;43:2269–2285.
- 15. Aktaa S, Batra G, Cleland JGF, Coats A, Lund LH, McDonagh T, et al Data standards for heart failure: the European Unified Registries for Heart Care Evaluation and Randomized Trials (EuroHeart). Eur Heart J. 2022;43 :2185–2195.
- 16. Batra G, Aktaa S, Wallentin L, Maggioni AP, Wilkinson C, Casadei B, et al Methodology for the development of international clinical data standards for common cardiovascular conditions: European Unified Registries for Heart Care Evaluation and Randomised Trials (EuroHeart). Eur Heart J Qual Care Clin Outcomes. 2021;2021:qcab052.
- 17. Zhang S, Gaiser S, Kolominsky-Rabas PL. Cardiac implant registries 2006-2016: a systematic review and summary of global experiences. BMJ Open. 2018;8:e019039.
- 18. Mills S, Lee JK, Rassekh BM, Zorko Kodelja M, Bae G, Kang M, et al Unique health identifiers for universal health coverage. J Health Popul Nutr2019;38:22.
- 19. Carroll JD, Mack MJ, Vemulapalli S, Herrmann HC, Gleason TG, Hanzel G, et al STS-ACC TVT Registry of Transcatheter Aortic Valve Replacement. J Am Coll Cardiol. 2020;76:2492–2516.
- 20. Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE, et al 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the Diagnosis and Management of Patients With Thoracic Aortic Disease. Circulation. 2010;121:e266–e369.
- 21. Johansson I, Joseph P, Balasubramanian K, McMurray JJV, Lund LH, Ezekowitz JA, et al Health-Related Quality of Life and Mortality in Heart Failure: The Global Congestive Heart Failure Study of 23 000 Patients From 40 Countries. Circulation. 2021;143:2129–2142.
- 22. Hahn Rebecca T, Webb J, Pibarot P, Ternacle J, Herrmann Howard C, Suri Rakesh M, et al 5-Year Follow-Up From the PARTNER 2 Aortic Valve-in-Valve Registry for Degenerated Aortic Surgical Bioprostheses. JACC: Cardiovascular Interventions. 2022;15:698–708.
- 23. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2021;42 :3599–3726.
- 24. Okuno T, Asami M, Heg D, Lanz J, Praz F, Hagemeyer D, et al Impact of Left Ventricular Outflow Tract Calcification on Procedural Outcomes After Transcatheter Aortic Valve Replacement. JACC Cardiovasc Interv. 2020;13:1789–1799.
- 25. STS/ACC TVT Registry - Trancatheter Aortic Valve Replacement (TAVR): Data Collection Form (V3.0). Available at: https://www.ncdr.com/WebNCDR/docs/default-source/tvt-public-page-documents/tvt_v3_tavr_dcf_1_26_2021-(1).pdf?sfvrsn=bfb3d49f_2. Accessed 27 July 2022.
- 26. Simonato M, Vemulapalli S, Ben-Yehuda O, Wu C, Wood L, Popma J, et al Minimum Core Data Elements for Evaluation of TAVR: A Scientific Statement by PASSION CV, HVC, and TVT Registry. JACC: Cardiovascular Interventions. 2022;15:685–697.
- 27. NCDR - CathPCI Registry: Coder's Data Dictinary (V5.0). Available at: https://cvquality.acc.org/docs/default-source/pdfs/2019/01/10/pci-v5-0-data-dictionary-coders-rtd-07242018-uploaded-jan-10-2019.pdf?sfvrsn=b95981bf_2. Accessed 03 August 2022.
- 28. STS/ACC TVT Registry - Trancatheter Aortic Valve Replacement (TAVR): Coder's Data Dictionary (V3.0). Available at: https://www.ncdr.com/WebNCDR/docs/default-source/tvt-v3-documents-for-the-private-side/tvt_v3-0_datadictionarycoderspecifications-(3).pdf?sfvrsn=9ba9d69f_4. Accessed 03 August 2022.
- 29. Restoring the Story and Creating a Valuable Clinical Note. Ann Intern Med. 2020;173:380–382.
- 30. Timmis A, Vardas P, Townsend N, Torbica A, Katus H, De Smedt D, et al European Society of Cardiology: cardiovascular disease statistics 2021. Eur Heart J. 2022;43:716–799.
- 31. Miller RS, Mitchell K, Myslinski R, Rising J. Health Information Technology (IT) and Patient Registries. In: Gliklich RE, Leavy MB, Dreyer NA, editors. Tools and Technologies for Registry Interoperability, Registries for Evaluating Patient Outcomes: A User's Guide, 3rd Edition, Addendum 2 [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2019. Chapter 1. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551883/.
- 32. Liyanage H, Krause P, de Lusignan S. Using ontologies to improve semantic interoperability in health data. BMJ Health & Care Informatics2015;22:309–315.