Introduction
Unilateral vocal fold paralysis (UVFP) is common in clinical practice, although the true incidence remains unknown. It implies vocal fold immobility due to neurologic injury and may be due to many causes including iatrogenic (thyroid, carotid, thoracic, or cervical spine surgery) or noniatrogenic trauma, neurologic disease, infection, malignancy (thyroid, lung, and others), or idiopathic disease. , Idiopathic vocal fold paralysis is not well understood. Some suspect a viral cause because many patients report an upper respiratory infection before the onset of vocal symptoms.
Patients with UVFP may demonstrate different degrees of voice perturbation depending on the position of the paralyzed vocal fold, and it can have a significant impact on patient’s quality of life. Uncompensated UVFP has been associated with dysphagia and impairment of vocal quality due to inadequate closure of the vocal folds and loss of vocal fold bulk and tonicity, resulting in bowing, flaccidity, and weakness of the paralyzed vocal fold. Nevertheless, the degree of voice complaint depends not only on the amount of glottal incompetence but also on the type of compensatory behaviors that the patient may carry out in order to improve vocal intensity. ,
Currently, reported treatment comprises either conservative or surgical treatment. The main goals of voice therapy are increase the coordination of glottis and supraglottic sphincters, increase elevation and stabilization of the larynx, improve glottal adduction as well as intrinsic muscle strength and agility, decrease parafunctional compensation during phonation (supraglottic hyperfunction), increase expiratory flow (exhalation rate), and improve voluntary control of the expiratory muscles. , Usually, for similar complaints and endoscopic findings, the therapy protocol is quite similar for all adult patients. However, anatomical and physiological changes in the larynx and respiratory system occur during the aging process, and little is known about the influence of aging on the rehabilitation’s success rate obtained by voice therapy in patients with UVFP. , Many anatomical and physiological changes have been associated with aging process. Neurologic changes include psychomotor slowing, decreased auditory acuity, especially for spoken language, decreased muscle bulk, and mild motor slowing. Muscular changes throughout the body affect areas involved in phonation. Specifically, decrease in muscle bulk (sarcopenia), strength, and general decrease in speed and movement with aging contributes to the changes in other systems throughout the aging body. These changes are most relevant to phonation when viewed through the lens of the respiratory system. Anatomical changes such as an increase in chest wall stiffness and decreased respiratory muscle strength are noted in the aging respiratory system and lungs and have direct impact on phonation. Also, in the larynx, aging modifications occur and might include changes in size and density of neuromuscular junctions. These changes in the neuromuscular junction precede atrophy in aging muscle fibers. Other laryngeal changes in the elderly adult include cartilage calcification, reduction in the amount and quality of mucus, thickening of epithelium, decrease in elastic fibers in the lamina propria, increase in collagen fibers, and changes in hyaluronic acid concentration. - These changes collectively result in vocal folds that become less elastic and less pliable with increasing age. To date, little is known about how this might influence the response of phonatory system to voice therapy in the rehabilitation of patients with UVFP.
The aim of the present study was to use multidimensional assessment, including objective and subjective measures, to analyze potential influence of aging in the functional outcomes achieved by a group of patients with recent onset of UVFP who underwent voice therapy. To the best of our knowledge, the present study is the first regarding evaluation of the “age” factor on the outcomes achieved by voice therapy in UVFP.
Materials and Methods
Ethical Considerations
This study was carried out in accordance with the guidelines of the Declaration of Helsinki on human studies.
Study Design
This is retrospective, observational, and cross-sectional study.
Setting and Participants
Patients with UVFP who underwent voice therapy between 2013 and 2017 at the Department of Otolaryngology, Head and Neck Surgery in a tertiary center. No patient had voice therapy or laryngeal surgery before being involved in the study. Patients with unilateral vocal fold immobility due to a progressive lesion (those with a mechanical cause such as laryngeal malignancy or cases with a neurological cause such as multiple sclerosis), or those with arytenoid dislocation, were excluded from the study.
Intervention and Outcomes
Objective and subjective evaluations were performed on all patients, and each one was assessed jointly by an otolaryngologist and a speech and language pathologist at the beginning and 1 month after the end of voice therapy program. Voice therapy started 30 days after the appearance of the UVFP. Data regarding gender, age, side and position of the paralyzed vocal fold, etiology, comorbidities, and Voice Handicap Index (VHI) before and after voice therapy were collected. Glottal insufficiency was also evaluated, by endoscopic laryngoscopy, before and after voice therapy.
Voice therapy
Voice therapy program was based on an evidence-based therapy protocol published by Vaz-Freitas et al. All patients involved in the study had several voice therapy sessions with the same experienced speech and language pathologist. Frequency of therapy sessions was twice a week on the first and second weeks of treatment and then once a week until the end of the program; the mean number of sessions was 12 (range: 10-15). Exercises were performed in office, and the patient got a prescription workout plan to repeat daily, every 2 hours, for 10 minutes. Initially, the voice therapy exercises used the reflex mechanism of glottal adduction with no sound associated with head and lower limbs movements. The patient was seated and complied with 5 seconds of inspiratory apnea, during which, he assumed different positions of the head and/or movements of the lower limbs. Then, usually on the second week, the exercises were based on the movement of the head with audible sounds, therefore combining the variation in the head position, after maintenance within 5 seconds inspiratory apnea, with the production of specific voiced sounds, during expiration, in maximum phonation time. On the third week, emphasis was placed on the vocal strength, by performing pushing and pulling exercises/effort and then on syllabic reduplication. By the fifth week, preference was given to tasks closer to spontaneous speech or reading of texts, and then, a set of exercises were performed in order to increase vocal resistance to sound production using semi-occluded vocal tract techniques. In the last sessions, the focus was reading with speech techniques such as mesa di voce, pitch and loudness variations, and chanted voice. There was also the need to prioritize the difficulty in the exercise, starting with the variation between sentences to the changes applied between each word. Finally, exercises were performed in order to maintain all acquisitions. Training in auditory and proprioceptive biofeedback was instilled at every step of the behavioral treatment program, in order to enable the patient to hear and feel the appropriate voice production.
Objective assessment
Each patient underwent fiberoptic videolaryngoscopy with stroboscopy (XION EndoSTROB E, type CD11F/R, XION; GmbH Pankstraße, Berlin, Germany) before and after intervention of voice therapy. Video recordings were obtained with a charge-coupled device camera, and on the basis of videolaryngoscopic images, glottal closure was rated, independently, by 2 experienced otorhinolaryngologists as follows: complete glottal closure, incomplete closure of the membranous portion of the vocal fold, and incomplete glottal closure of the entire glottis.
Self-assessment
Each patient completed the VHI, before and after voice therapy, with 30 questions to have self-assessment data on the perceived quality of life.
Statistical analysis
All analyses were performed in the software SPSS version 24, and P values below .05 were considered statistically significant. A descriptive analysis of patient characteristics was performed considering absolute and relative frequencies (for categorical variables) and mean and standard deviation (SD; for continuous variables). The normality of variable distribution was tested by skewness and kurtosis and variance homogeneity by Levene test.
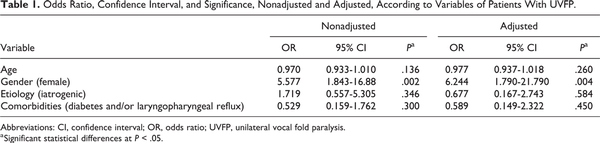
The intraclass coefficient (ICC) with 95% confidence intervals (95% CIs) were calculated to evaluate the level of agreement between observers. An ICC higher than 0.4 was considered as an acceptable level of agreement. In order to evaluate potential factors that might influence the improvement in endoscopic findings, multiple univariate logistic regression modeling was used to determine the odds ratios (ORs) of having age, gender, etiology, or comorbidities associated with an improvement in glottal closure after voice therapy.
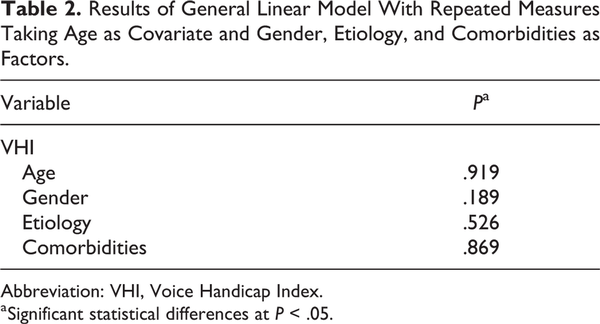
Difference between VHI before and after voice therapy was tested by paired sample t test, and to evaluate the influence of age on both VHI, it was used a general linear model with repeated measures taking age as a covariate. To assess the potential influence of gender, etiology, or comorbidities on VHI, they were used as factors in a general linear model with repeated measures taking age as a covariate.
Results
Study Population
The study population included a total of 100 Caucasian patients with UVFP who underwent voice therapy. Seventy-six (76.0%) were female and 24 (24.0%) were male. Their mean age was 61.04 years (±14.7 SD; range: 21-88 years) and 46 (46.0%) patients were older than 65 years old. Fifty (50.0%) patients had right vocal fold paralysis, and 50 (50.0%) had left vocal fold paralysis. As concerns the etiology, 21.0% was idiopathic and 79.0% was iatrogenic (72 patients after thyroidectomy, 3 patients after parathyroidectomy, 3 patients after cervical spine surgery, and 1 case after carotid endarterectomy). The most prevalent comorbidities were diabetes (19 patients; all older than 65 years old) and laryngopharyngeal reflux (9 patients ≤ 65 years old and 8 patients > 65 years old). Thirty (30.0%) patients had at least diabetes or laryngopharyngeal reflux as comorbidities. Other comorbidities found in this study population were high blood pressure and dyslipidemia.
Objective Assessment
The ICC obtained to evaluate the level of agreement between otorhinolaryngologists was 0.601 (95% CI: 0.458-0.714, P < .001), indicating a moderate to substantial level of agreement. Before commencement of voice therapy, incomplete glottal closure of the entire glottis was found in all patients. Following voice therapy (1 month after the last session), 80 (80.0%) patients exhibited an improvement in glottal closure (P < .001). Complete glottal closure was observed in 69 (69.0%) cases (43 patients ≤ 65 years old; 26 patients > 65 years old) and better but still an incomplete closure of the membranous portion of the vocal folds in 11 (11.0%; 2 patients ≤65 years old; 9 patients >65 years old). Thus, 83.3% of patients ≤65 years old and 76.1% of patients older than 65 years exhibited improvement in glottal closure.
Most of the patients exhibited better glottis closure after voice therapy (P < .001), and this was not influenced by age (P = .136; Table 1). Nevertheless, for each 10-year increase in age, the chance of endoscopic improvement reduced 3%.
From all potential predictive factors for better endoscopic findings after voice therapy, only gender exhibited statistically significant influence (OR = 6.244, P = .004; Table 1). Females with UVFP presented 5.6 greater chance for endoscopic improvement after voice therapy.
Self-Assessment
Mean value for VHI total score before voice therapy was 50.5 (47.4 for patients ≤65 years old; 54.0 for patients >65 years old). The mean values for functional, physical, and emotional subscales were, respectively, 14.77, 22.31, and 12.35.
After voice therapy, the mean value for VHI total score was 21.2 (17.3 for patients ≤65 years old and 26.6 for patients >65 years old). The mean values for functional, physical, and emotional subscales were, respectively, 6.19, 10.26, and 5.13.
The mean score of VHI, before and after voice therapy, was statistically different (P < .001) with a lower score after therapy. The score of VHI was not influenced by age (P = .717). However, for each 10-year increase in age, the score of VHI, before and after voice therapy, increased 1.91 and 2.86 units, respectively. Neither gender, etiology, nor comorbidities affected the difference in VHI after voice therapy (P > .05; Table 2).
Discussion
New Findings and Comparisons With Other Studies
Unilateral vocal fold paralysis may have many causes, but generally it happens due to 1 of 3 reasons: nerve injury during surgeries of the thyroid and other head and neck procedures, malignant growth causing pressure on the nerve, or inflammatory process usually caused by viral infection. We reported in this study that surgical trauma (iatrogenic) was the most encountered etiology (79.0%), and thyroid surgery was the most commonly reported procedure accounting for 91.1% of iatrogenic etiologies. According to other reports, the incidence of postoperative UVFP ranged from 11.0% to 66.0%, - and the rate of post-thyroid surgery patients in the total number of paralysis was 7% to 28%. ,, The number of iatrogenic paralysis was higher in our study, since progressive malignant conditions were excluded, and probably, most of the cases were due to thyroid surgery because in our hospital there is no thoracic or cardiac surgery. Because thyroid pathology is more prevalent in females, this may also justify the predominance of female gender in our study. A higher prevalence of females had also been reported in other studies. ,
In 21 (21.0%) cases of this study, the cause was not revealed and labeled as idiopathic, which corresponds to the rates of idiopathic paralysis in previous reports (ranged from 2% to 24%). ,,
In the management of patients with UVFP, the otolaryngologist and speech pathologist must work as a team, and previous studies supported the utility of voice therapy in such patients. ,,, Deciding whether to use medical, surgical, and behavioral therapies, individually or jointly, is determined by the patient’s vocal performance and history. Guidelines for when to offer voice therapy have been based on laryngeal behavior, etiology, objective ratings, and patient’s gender. A period of voice therapy should be considered for those patients with UVFP and strong cough, milder symptoms, and adequate airway protection. Several studies have suggested that 4 to 6 weeks are the minimum time required for patients to achieve sustained benefit from voice therapy. All this recommendations have been taken into account in this study.
The results of the present study show that, on average, a significant improvement in voice quality can be achieved through voice therapy alone. Despite being controversial among laryngologists, in our department, surgery is therefore to be delayed and reserved only for those cases that fail to benefit from voice therapy or those that show additional symptoms besides dysphonia, especially dysphagia and aspiration. ,
Since voice is not a single, numeric outcome, but a multidimensional function, evaluation of voice therapy efficacy required carefully selected assessment measures. Morphofunctional laryngeal analysis cannot be directly related to the treatment outcomes of patients with UVFP. In fact, strobovideolaryngoscopic findings do not always correspond to the degree of vocal impairment. The purpose of the therapy for UVFP is to address the symptoms that bother the patient. The patient’s perception of dysphonia, rather than clinician and instrumental measures, is now considered to be the strongest primary outcome measure. The VHI is currently the most widely used questionnaire for the assessment of voice-related quality of life and has been shown to have test–retest reliability and to be sensitive for a wide variety of voice disorders. The VHI scores of patients with UVFP tend to reveal greater perceived vocal dysfunction than dysphonia from other causes and other types of dysphonia. In the present study, the mean value for VHI total score, before voice therapy, was 50.61, which denotes a moderate amount of handicap. After voice therapy, mean values for total scores significantly decreased as did those for the physical, functional, and emotional subscales.
In our study, the prevalence of complete glottal closure was significantly higher than before therapy. An increase in glottal closure was observed after voice therapy and may be due not only to adequate compensation of the contralateral vocal fold but also to the paralyzed vocal fold advancing to the midline, owing to the activity of the interarytenoid muscle or to passive lengthening induced by the cricothyroid muscle. Moreover, glottal closure may improve due to the compensatory activity of the inferior pharyngeal constrictor muscle. In this study, not only endoscopic findings but also self-assessment measures showed a significant improvement, thus suggesting that quality of life reaches a more satisfactory level after voice therapy.
When considering the age of the patients in this study, it ranged from 21 to 88 years (61.04 ± 14.7 years). In the literature, there has been only 1 report addressing the age of vocal fold paralysis patients in which vocal fold paralysis was found to increase with age, rising rapidly in the fourth decade and peaking in the sixth decade. In our study, almost a half of the study population was older than 65 years old, and aging has not influenced the success rate obtained by voice therapy in the management of UVFP.
Clinical Applicability of the Study
Regardless physiologic aging changes in the phonatory system, older patients benefited from it. For each 10-year increase, the chance of endoscopic improvement reduced 3% and for each 10-year increase, the score of VHI, before and after voice therapy, increased 1.91 and 2.86 units, respectively. These findings are in accordance with the expected consequences of presbylarynx. However, in our opinion, an effort has to be made in order to encourage elderly patients with UVFP to attend the multiple voice therapy sessions, because the prognosis is as good as expected for youngers. Our results also highlight the importance of voice therapy in presbyphonia because, as demonstrated, even in older larynxes voice therapy might induce favorable alterations, with significantly improvement in vocal quality and advantageous benefits in VHI.
Limitations
First of all, it is possible that some patients may have had arytenoid fixation rather than vocal fold paralysis because laryngeal electromyography was not used for the diagnosis in our department. Second of all, data regarding perceptual and acoustic analysis were not collected but should be assessed in future studies in order to get a more detailed evaluation of voice therapy in patients with UVFP of different ages. Maximum phonation time, which correlates well with glottic insufficiency, should be included in future studies. Third of all, the test–retest reliability of provided ratings was not tested, since the self-assessment was performed only once by each patient before and after voice therapy.
Although the data in the present study described a significant improvement in voice quality, despite the aging factor, further research with a larger number of patients and a control group not undergoing any kind of rehabilitation is needed to assess the efficacy of voice therapy in patients with UVFP of different age groups. Nevertheless, to our knowledge, this is the first explorative study that evaluates the factor “age” in objective and subjective outcomes obtained in patients with UVFP after voice therapy. We will continue this research by increasing the sample size and including aerodynamic, perceptual, and acoustic analysis to increase the power of findings in this study.
Conclusion
The most common cause of UVFP in our study was surgery, and thyroidectomy continues to be the single most common surgical procedure responsible for unilateral vocal cord paralysis. A clear and significant improvement was visible in the endoscopic and self-assessment ratings after rehabilitation by isolated voice therapy. Despite anatomical and physiological aging changes in the phonatory system, age did not compromise the successful rate obtained by voice therapy.
Authors’ Note All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
Mariline Santos
https://orcid.org/0000-0001-7041-0994
References
- 1. Schindler A, Bottero A, Capaccio P, Ginocchio D, Adorni F, Ottaviani F. Vocal improvement after voice therapy in unilateral vocal fold paralysis. J Voice. 2008;22(1):113–118.
- 2. Miller S. Voice therapy for vocal fold paralysis. Otolaryngol Clin North Am. 2004;37(1):105–119.
- 3. D’Alatri L, Galla S, Rigante M, Antonelli O, Buldrini S, Marchese MR. Role of early voice therapy in patients affected by unilateral vocal fold paralysis. J Laryngol Otol. 2008;122(9):936–941.
- 4. Vaz-Freitas S, Melo Pestana P. Glottal Incompetence: Proposal of an Evidence Based Therapy. Voice Disorders: Epidemiology, Treatment Approaches and Long-Term Outcomes. New York, NY: Nova; 2016.
- 5. Pontes P, Yamasaki R, Behlau M. Morphological and functional aspects of the senile larynx. Folia Phoniatr Logop. 2006;58(3):151–158.
- 6. Sharma G, Goodwin J. Effect of aging on respiratory system physiology and immunology. Clin Interv Aging. 2006;1(3):253–260.
- 7. Fillit H, Rockwood K, Woodhouse K. Brocklehurst’s Textbook of Geriatric Medicine and Gerontology. 7th ed. Philadelphia, PA: Saunders/Elsevier; 2010.
- 8. Larsson L, Grimby G, Karlsson J. Muscle strength and speed of movement in relation to age and muscle morphology. J Appl Physiol Respir Environ Exerc Physiol. 1979;46(3):451–456.
- 9. Burggraf V, Kim K, Knight A. Healthy Aging: Principles and Clinical Practice for Clinicians. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins; 2014.
- 10. Connor NP, Suzuki T, Lee K, Sewall GK, Heisey DM. Neuromuscular junction changes in aged rat thyroarytenoid muscle. Ann Otol Rhinol Laryngol. 2002;111(7):579–586.
- 11. Deschenes MR, Roby MA, Eason MK, Harris MB. Remodeling of the neuromuscular junction precedes sarcopenia related alterations in myofibers. Exp Gerontol. 2010;45(5):389–393.
- 12. Gregory ND, Chandran S, Lurie D, Sataloff RT. Voice disorders in the elderly. J Voice. 2012;26(2):254–258.
- 13. Kendall K. Presbyphonia: a review. Curr Opin Otolaryngol Head Neck Surg. 2007;15(3):137–140.
- 14. Pontes P, Brasolotto A, Behlau M. Glottic characteristics and voice complaint in the elderly. J Voice. 2005;19(1):84–94.
- 15. Jacobson BH, Johnson A, Grywalski A, et al. The Voice Handicap Index (VHI): development and validation. Am J Speech Lang Pathol. 1997;6(3):66–70.
- 16. Al-Khtoum N, Shawakfeh N, Al-Safadi E, Al-Momani O, Hamasha K. Acquired unilateral vocal fold paralysis: retrospective analysis of a single institutional experience. N Am J Med Sci. 2013;5(12):699–702.
- 17. Rosenthal LH, Benninger MS, Deeb RH. Vocal fold immobility: a longitudinal analysis of etiology over 20 years. Laryngoscope. 2007;117(10):1864–1870.
- 18. Takano S, Nito T, Tamaruya N, Kimura M, Tayama N. Single institutional analysis of trends over 45 years in etiology of vocal fold paralysis. Auris Nasus Larynx. 2012;39(6):597–600.
- 19. Maisel RH, Ogura JH. Evaluation and treatment of vocal cord paralysis. Laryngoscope. 1974;84(2):302–316.
- 20. Parnell FW, Brandenburg JH. Vocal cord paralysis. A review of 100 cases. Laryngoscope. 1970;80(7):1036–1045.
- 21. Tucker HM. Vocal cord paralysis: etiology and management. Laryngoscope. 1980;90(4):585–590.
- 22. Colton RH, Casper JK. Understanding Voice Problems: A Physiological Perspective for the Diagnosis and Treatment. Philadelphia, PA: Lippincott Williams & Wilkins; 1996: 358–360.
- 23. Heuer RJ, Sataloff RT, Emerich K, et al. Unilateral recurrent laryngeal nerve paralysis: the importance of “preoperative” voice therapy. J Voice. 1997;11(1):88–94.
- 24. Stemple JC, Lee L, D´Amico B, Pickup B. Efficacy of vocal function exercises as a method of improving voice production. J Voice. 1994;8(3):271–278.
- 25. Flint PW, Purcell LL, Cummings CW. Pathophysiology and indications for medialization thyroplasty in patients with dysphagia and aspiration. Otolaryngol Head Neck Surg. 1997;116(3):349–354.
- 26. Vila PM, Bhatt NK, Paniello RC. Early-injection laryngoplasty may lower risk of thyroplasty: a systematic review and meta-analysis. Laryngoscope. 2018;128(4):935–940.