Introduction
In the last years, drug overdose deaths have increased in the United States. Since 2000, the number of deaths related to drug overdose has doubled. In 2014, as well as in 2017, opioids were involved in over 60%. Also, the rate of deaths involving semisynthetic opioids like morphine, oxycodone, or hydrocodone has increased. This trend has continued in the last years. After sinonasal surgery, most patients received postoperative opioid analgesics, although the majority were not used. According to Riley et al, up to 90% of the patients had leftover opioid pills. Of these patient, about 70% kept the opioid analgesics, which could possibly lead to improper use. The literature suggests that a large proportion of opioid abuser addiction was initiated by the prescription of opioids. Consequently, a well-considered reduction of opioids after (sinonasal) surgery could also decrease the number of unused pills which could potentially be used in an illicit way., There have been previous studies that recommended the use of non-opioid analgesics like nonsteroidal antirheumatic drugs (NSAIDs) or acetaminophen, as these analgesics could also ensure appropriate pain control after functional endoscopic sinonasal surgery (FESS)., However, the need for, use of, timing and side effects of opioid and non-opioid analgesics after sinonasal surgery are still unclear and are controversially discussed. The objective of the following study was to solve these shortcomings.
Methods
Patient Population
This was an institutional review board–approved retrospective study of (n = 280) patients who underwent sinonasal surgery, septoplasty, or sinonasal surgery in combination with septoplasty in the Otolaryngology Department of the University Erlangen-Nürnberg between January and December 2018. Included patients underwent FESS of any extent (selective frontal, ethmoidal, or maxillary sinus surgery, up to “full house FESS”) or septoplasty and turbinoplasty. Patients undergoing open septorhinoplasty were excluded. For all patients, the postoperative pain (3-5 days after surgery) using the numeric rating scale (NRS) and the postoperative need for non-opioid analgesics were prospectively collected and related to demographic and surgical parameters. Patients received analgesics on demand or if a high pain score (≥4) was indicated. Only postoperative analgesics were counted. Medical history, demographic information, comorbidities, procedural data, and sinonasal complications were collected.
All patients undergoing septoplasty received splints for 7 days. All patients undergoing FESS received a nasal packing for 1 day. The nasal packing consisted of a merocele tamponade (10-cm, polyvinyl alcohol; Medtronic Xomed). Postoperative nasal care was started directly after removal of the nasal packing on postoperative day 1 (POD1). Nose care included xylometazoline spray and a xylometazoline emulsion after septoplasty or an emulsion containing a topical steroid after FESS, respectively. Xylometazoline is an α-sympathomimetic that is to be routinely found in decongestant nasal spray. The emulsion also contained dexamethasone as well as menthol and was used as a spray 3 times daily. There was no ingredient that provided pain relief. Data were extracted from patient files and the clinical information system.
Outcome Measures
The primary outcome measure was the change in NRS per POD. The secondary outcome measures were the amount of non-opioid and opioid analgesics used as well as complication rates.
Statistical Measures
Standard descriptive statistics were reported as mean ± SD for continuous variables and a frequency count (%) for categorical variables. The analysis of variance and the paired t test were used to compare changes in pain scores. A P value of < .05 was considered statistically significant. Statistical analyses were performed using the statistical software STATA version 14.2 (StataCorp LP).
Results
Patient Demographics
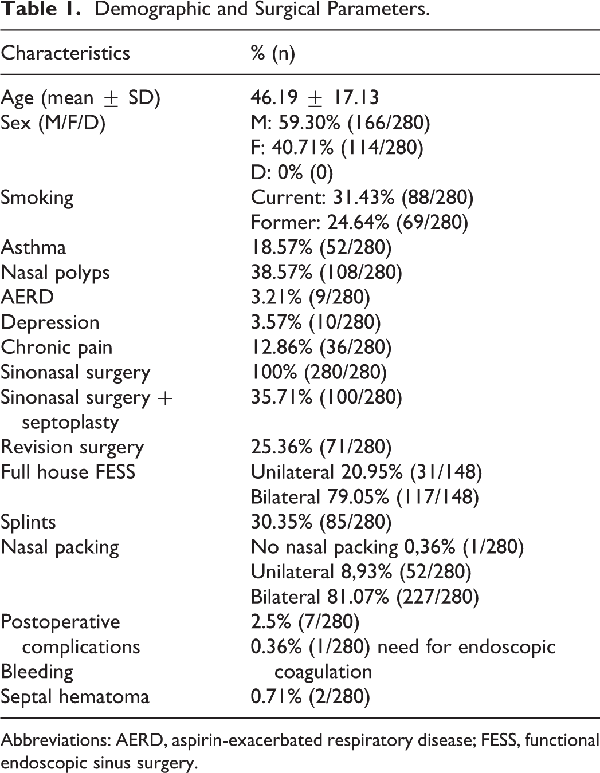
Patient demographics are displayed in Table 1. In our study, the mean age at the time of surgery was 46.2 (± 17.3, range 9-83), almost 60% were men (166/280). Of total, 38.6% of the patients (108/280) presented with nasal polyps during surgery, 18.6% (52/280) had asthma, and 3.2% of all patients (9/280) showed the clinical presentation of an aspirin-exacerbated respiratory disease (AERD) including NSAR intolerance. Around one-third of the patients smoked at the time of surgery, and 24.6% were former smokers.
Surgical parameters
In our study, all patients underwent FESS. In 100 (35.71%) patients, a septoplasty was additionally performed. In more than 50% (148/280) of patients, all sinuses were operated on, either unilaterally (31/148) or bilaterally (117/148). All remaining patients underwent circumscribed surgery: 40.36% (113/280) maxillary sinus, 28.93% (81/280) ethmoidal sinus, 16.70% (47/280) frontal sinus, and 5% (14/280) sphenoidal sinus. Most of the patients needed bilateral packing (n = 227, 81.07%), a few patients at least unilateral nasal packing (n = 25, 8.93%), and only 1 patient no packing (n = 1, 0.4%).
Postoperative complications
Seven (2.5%) of the patients presented with a postoperative bleeding complication, but only 1 (0.36%) patient needed endoscopic coagulation. A septal hematoma occurred in 2 (0.71%) patients. For draining of the septal hematoma, 1 (1%) patient needed revision surgery on POD2.
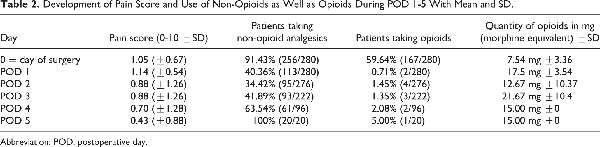
Pain scores
Patients after FESS showed low pain scores throughout the 5-day follow-up (0.85 ± 0.25, range 0.43-1.14). As shown in Figure 1, there was a peak on the POD1 with a mean pain score of 1.14 (± 0.54) that decreased significantly on the POD2 (0.88 ± 1.26, P = .01) and decreased further with time (POD3 0.88 ± 1.26, P < .01; POD4, 0.70 ± 1.28, P < .01; POD5 0.43 ± 0.88, P < .01). Septoplasty led to increased pain scores compared to FESS alone on POD1 (0.99 vs 1.42, P = .003). There was no significant difference on POD2-5 although the splints remained at least until POD5.
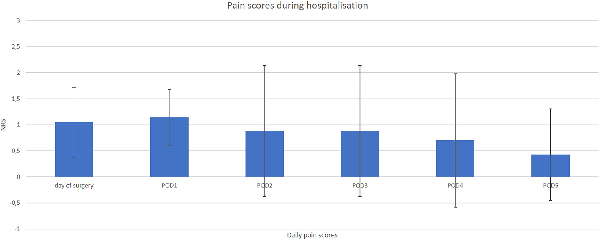
Figure 1
Bar graph showing the pain scores during hospitalization (day of surgery until POD5) with mean and SD. POD indicates postoperative day.
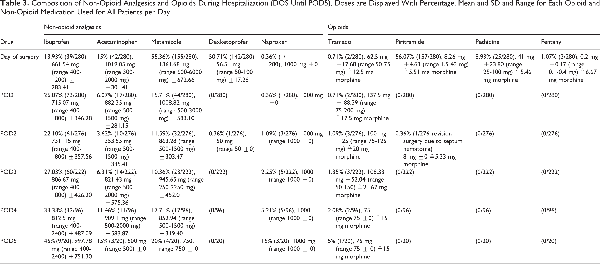
Analgesics
Proportional distribution of analgesics is displayed in Figure 2. Not counting the opioids used during surgery, 167 (59.64%) patients needed opioids on the day of surgery (56.07% piritramide; 8.93% pethidine, 1.07% fentanyl, and 0.71% tramadol). In addition to the opioids, 256 (91.43%) patients needed at least one of the following non-opioid analgesics: metamizole (n = 155, 55.36%), dexketoprofen (n = 142, 50.71%), acetaminophen (n = 42, 15%), ibuprofen (n = 39, 13.93%), and naproxen (n = 1, 0.36%). Simultaneously, the mean quantity of opioid and non-opioid analgesics reached the highest values on the day of surgery (DOS).
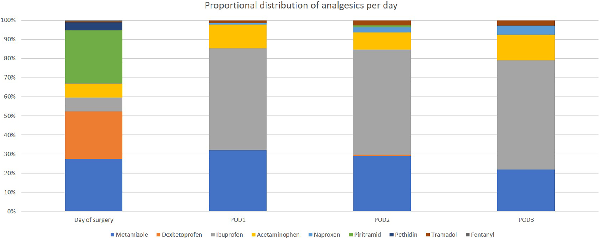
Figure 2
Bar graph showing the proportional distribution of analgesics per day (DOS-POD3). The dark blue color represents pethidine, the light blue color metamizole, the blue-green color naproxen, the yellow color acetaminophen, the orange color dexketoprofen, the red color tramadol, the green color piritramide, the light gray color ibuprofen, and the dark gray color fentanyl.
Already on POD1, only 0.71% of the patients needed opioids and 40.36% non-opioid medication, leaving 58.93% of the patients not needing any pain medication at all. The percentage of patients needing no medication at stable low pain scores increased with each POD (Table 2).
As shown in Figure 3 from the DOS to POD5, metamizole (34.01%) was the non-opioid analgesic most frequently prescribed (dexketoprofen 17.72%, ibuprofen 33.95%, acetaminophen 12.02%, and naproxen 2.23%). Piritramide (79.4%) was the most frequently used opioid (pethidine 12.56%, tramadol 6.53%, and fentanyl 1.51%). From POD1 on, ibuprofen was used most (54.91% of all non-opioid analgesic prescriptions vs 28.04% metamizole vs 12.85% acetaminophen vs 3.97% naproxen). Altogether (DOS-POD5), all patients needed a total of 14.90 mg (±4.73 mg) opioids in morphine equivalent. However, this equals only 1.8% (5/280) of the patients who needed the opioid analgesic on POD 1-5 (for details, see Table 3).
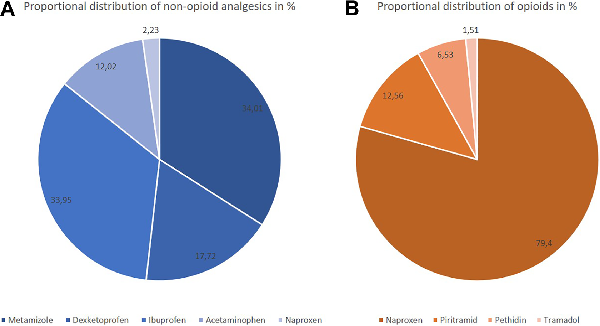
Figure 3
Pie charts of the overall proportional distribution of (A) non-opioids (left) and (B) opioids (right), both displayed as percentages.
Discussion
Due to the increasing abuse of leftover opioids, it is crucial to reconsider postoperative pain scores as well as the need for, use of, timing and side effects of opioid and non-opioid analgesics after sinonasal surgery.
As in other similar studies, the overall pain score after sinonasal surgery was low. The pain score was highest on the POD1 and decreased significantly afterward. But although pain scores were highest on the POD1, only 0.71% of the patients needed opioid and only 40.36% non-opioid analgesics. This means that 58.93% of the patients did not request or need any pain medication on the POD1 at all.
A similar trend of decreasing pain scores over time was discovered by various other studies.,,, However, the pain scores in our study were even lower, for example, 1.14 (±0.54) on POD1 in our study compared to 3.61 or 4.1. This might be explained by the different ways of collecting the pain score values. While in our study the patients were asked to give a pain score between 0 and 10, the patients in the study of Wise et al received a questionnaire where they had to mark their pain level on a straight line. The mark was converted to a pain level afterward. Also, there may be intercultural or interregional differences in pain perception and tolerance for expressing pain. However, as pain scores themselves are very subjective, the differences might even be explained by the large interindividual variance between patients.
Additionally, it has to be discussed whether there might be an association between the highest pain scores on the day of surgery and the usage of a nasal packing which was removed on the morning of the POD1. Several studies showed that the application of nasal packings led to higher pain scores compared to matched patient groups who did not receive a nasal packing., Other studies, however, did not show significant differences in pain scores with or without a nasal packing., Future randomized studies with a sufficiently large sample size will have to be performed to answer this question.
The majority (59.64%) of the patients needed a combination of opioids and non-opioid analgesics on the day of surgery. However, from POD1-5, only 1.8% of the patients needed postoperative opioids in our study. During these days, pain was controlled with non-opioid analgesics or even without any pain medication at all. Those patients who continued the opioid therapy were mainly patients who had chronic pain in their previous history. Our observation confirms Newberry’s hypothesis that the common use of opioids after sinonasal surgery should be reduced, as well as the presumption of Wu et al that the need for opioids can be reduced by using non-opioids like NSAIDs. Our data support previous literature showing that the use of opioids decreased significantly after surgery, while the use of non-opioid analgesics remained approximately steady.
In our study, metamizole was the most frequently prescribed non-opioid analgesic. In the majority of comparable studies, metamizole was not used as it had not been approved by the Food and Drug Administration (FDA) due to the risk of agranulocytosis., In a previous survey, the most frequently prescribed drug after sinonasal surgery was hydrocodone–acetaminophen. Less than half of the participants were prescribed ibuprofen or other NSAIDs. The authors feared increased bleeding complications, and elevated pain scores may explain these prescription behavior patterns. In our study, only 2.5% of the patients experienced bleeding after surgery, and electronic coagulation was needed for only one patient. In our study, we mostly used non-opioid analgesics, and our data underlined previous data that did not observe higher bleeding rates using NSAIDs compared to using opioid drugs., Our results also confirm previous literature which states that a reduction of opioids still guarantees satisfactory pain control and does not lead to increased second prescriptions.
Conclusion
Our results indicate that the majority of patients need opioid analgesics almost exclusively on the day of surgery. In the postoperative phase (POD1-5), non-opioid analgesics are sufficient for pain control on demand, and most patients do not need any analgesia at all with sufficiently low pain scores. There were no major complications in patients taking either opioids or non-opioids. Our results indicate that the postoperative pain regimen should initially be started using non-opioid analgesics and be further escalated to opioid analgesics in individual cases. This could lead to a reduction of opioids and leftover pills presenting an illicit source of opioids in the community.
Authors’ Note This research was performed in fulfillment of the requirements for obtaining the degree “Dr. med.” at the Friedrich-Alexander-University Erlangen-Nürnberg (FAU).
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
Konstantinos Mantsopoulos
https://orcid.org/0000-0002-4948-8882
Sarina K. Mueller
https://orcid.org/0000-0001-5790-0841
References
- 1. Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths—United States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2018;67(5152):1419–1427. doi:10.15585/mmwr.mm675152e1
- 2. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths—United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016;65(50-51):1445–1452.
- 3. Becker SD, Becker DG. Review and update on postoperative opioid use after nasal and sinus surgery. Curr Opin Otolaryngol Head Neck Surg. 2018;26(1):41–45.
- 4. Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription opioid analgesics commonly unused after surgery: a systematic review. JAMA Surg. 2017;152(11):1066–1071. doi:10.1001/jamasurg.2017.0831
- 5. Riley CA, Kim M, Sclafani AP, et al. Opioid analgesic use and patient-reported pain outcomes after rhinologic surgery. Int. Forum Allergy Rhinol. 2018;9(4):339–344.
- 6. Newberry CI, Casazza GC, Pruitt LC, Meier JD, Skarda DE, Alt JA. Prescription patterns and opioid usage in sinonasal surgery. Int Forum Allergy Rhinol. 2020;10(3):381–387.
- 7. Vadivelu N, Kai AM, Kodumudi V, Sramcik J, Kaye AD. The opioid crisis: a comprehensive overview. Curr Pain Headache Rep. 2018;22(3):1–6.
- 8. Locketz GD, Brant JD, Adappa ND, et al. Postoperative opioid use in sinonasal surgery. Otolaryngol Head Neck Surg. 2019;160(3):402–408.
- 9. Svider PF, Nguyen B, Yuhan B, Zuliani G, Eloy JA, Folbe AJ. Perioperative analgesia for patients undergoing endoscopic sinus surgery: an evidence-based review. Int Forum Allergy Rhinol. 2018;8(7):837–849.
- 10. Kemppainen T, Kokki H, Tuomilehto H, Seppä J, Nuutinen J. Acetaminophen is highly effective in pain treatment after endoscopic sinus surgery. Laryngoscope. 2006;116(12):2125–2128.
- 11. Wu AW, Walgama ES, Genç E, et al. Multicenter study on the effect of nonsteroidal anti-inflammatory drugs on postoperative pain after endoscopic sinus and nasal surgery. Int Forum Allergy Rhinol. 2020;10(4):489–495.
- 12. Wise SK, Wise JC, DelGaudio JM. Evaluation of postoperative pain after sinonasal surgery. Am J Rhinol. 2005;19(5):471–477.
- 13. Al-Harthy M, Ohrbach R, Michelotti A, List T. The effect of culture on pain sensitivity. J Oral Rehabil. 2016;43(2):81–88.
- 14. Mane RS, Patil B, Mohite A. Comparison of septoplasty with and without nasal packing and review of literature. Indian J Otolaryngol Head Neck Surg. 2013;65(suppl 2):406–408.
- 15. Awan MS, Iqbal M. Nasal packing after septoplasty: a randomized comparison of packing versus no packing in 88 patients. Ear Nose Throat J. 2008;87(11):624–627.
- 16. Coey JG, Whittaker PJ, Williams G, Ikram UH, Page OJR. Fibrin tissue adhesive versus nasal packing in endoscopic nasal surgery: a systematic review and meta-analysis. Rhinology. 2019;57(1):21–31.
- 17. Seol JH, Kim JM, Kim SS, et al. Comparison of polyvinyl alcohol coated nasal packing with non-absorbable nasal packing. Rhinology. 2013;51(2):137–142.
- 18. Arzneimittelkommission der deutschen Ärzteschaft. Agranulozytose nach Metamizol—sehr selten, aber häufiger als gedacht. Dtsch Arztebl. 2011;108(33):A1758–A1759.
- 19. Stammschulte T, Ludwig WD, Mühlbauer B, Bronder E, Gundert-Remy U.Metamizole (dipyrone)-associated agranulocytosis. An analysis of German spontaneous reports 1990-2012. Eur J Clin Pharmacol. 2015;71(9):1129–1138
- 20. Gray ML, Fan CJ, Kappauf C.Postoperative pain management after sinus surgery: a survey of the American Rhinologic Society. Int Forum Allergy Rhinol. 2018;8(10):1199–1203.
- 21. Miller C, Humphreys IM, Davis GE. Effect of over the counter ibuprofen dosing after sinus surgery for chronic rhinosinusitis: a prospective cohort pilot study. Ann Otol Rhinol Laryngol. 2020;129(7):677–683. doi:10.1177/0003489420906179
- 22. Aulet RM, Trieu V, Landrigan GP, Millay DJ. Changes in opioid prescribing habits for patients undergoing rhinoplasty and septoplasty. JAMA Facial Plast Surg. 2019;21(6):487–490. doi:10.1001/jamafacial.2019.0937