Introduction
Acute bacterial rhinosinusitis (ABRS) has well-known and well-described complications, such as retropharyngeal abscess (RPA) formation, cavernous sinus thrombosis (CST), and intracranial extensions of infection. The incidences of these complications have fallen steadily in recent years due to advancements in antibiotic treatment. In the setting of COVID-19, we have seen extremely advanced stages of disease due to patient hesitations to seek medical attention. Here, we present the first reported case of bilateral longus colli abscesses as a complication of advanced ABRS, which was successfully treated with antibiotics and functional endoscopic sinus surgery (FESS) with abscess drainage.
Case Report
A 56-year-old female with a past medical history of hypertension was directly transferred to our neurological intensive care unit (ICU) for management of severe sepsis, left-sided pansinusitis, bilateral intramuscular deep neck space abscesses, viral pneumonitis, and subacute cerebral infarction.
She experienced 2 weeks of fevers and upper respiratory infection symptoms before presenting to an outside hospital with altered mental status and hypoxemic respiratory distress necessitating intubation. Workup revealed ABRS, Streptococcal bacteremia, large subacute right middle cerebral artery (MCA) infarction, elevated white blood cell count at 49 000 cells/mm3, and severe sepsis presumed secondary to viral pneumonitis and evidenced by multifocal ground-glass opacities on imaging, despite negative COVID-19 testing. She required intubation for 6 days, and upon extubation, exhibited significant expressive aphasia. Brain imaging showed a stable MCA stroke, new bilateral retro-nasopharyngeal abscesses, and concern for left cavernous sinus and superior ophthalmic vein thromboses. The patient was transferred to our institution for further management.
She was admitted directly to the neurological ICU on low flow nasal cannula, somnolent, and anarthric, but intermittently following commands. Physical examination was notable for left sided: cranial nerve IV and VI palsies, proptosis, maxillary and frontal sinus tenderness, lower facial weakness, and extremity hemiparesis. Magnetic resonance imaging (MRI) confirmed bilateral longus colli muscles abscesses (Figure 1) extending from the skull base to C1, bilateral cavernous sinus thromboses (left > right), subacute right MCA stroke, and intracranial right Sylvain fissure abscess with abnormal leptomeningeal enhancement. She was treated with intravenous metronidazole, cefepime, and vancomycin at central nervous system doses, and she continued intranasal Flonase and saline sprays. She was started on therapeutic intravenous heparin for the venous sinus thromboses, following a thorough discussion with family members about risks and benefits, including the possibility of infarct hemorrhagic conversion. Due to her severe condition, source control and bacterial cultures were recommended by infectious disease.
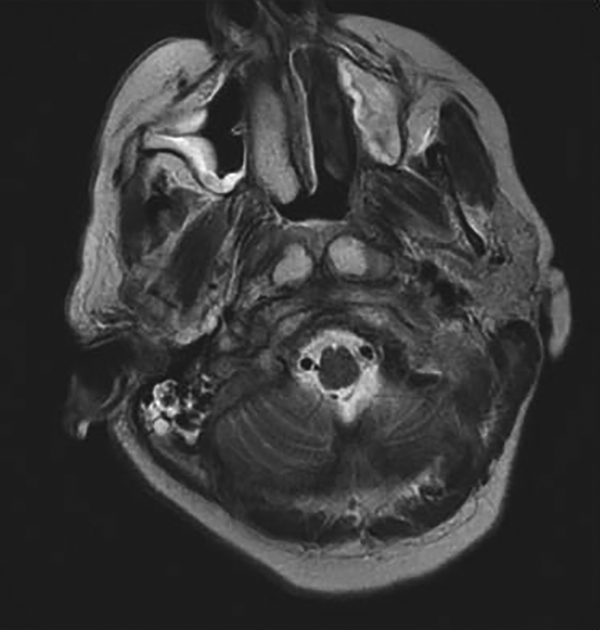
Figure 1
Axial T2 magnetic resonance imaging (MRI) showing bilateral longus colli muscles abscesses extending from the skull base to C1.
In the operating room, stereotactic image-guided FESS was performed for left-sided maxillary antrostomy, left total ethmoidectomy, left frontal sinusotomy, and bilateral sphenoidotomies that evacuated overt purulence. In the nasopharynx, a vertical superolateral incision was made using sharp needle-tip electrocautery, through the mucosa, deep into the longus colli muscles. The abscess pocket immediately expressed purulent drainage. The same procedure was completed on the contralateral side, as the abscesses had separate capsules. Heparin was held 1 hour before the case and restarted 3 hours afterward. On postoperative day 4, MRI revealed interval decompression of the longus colli abscesses (Figure 2). Abscess cultures yielded Staphylococcus hominis; sinus cultures were without bacterial growth. The patient steadily improved in mental status but exhibited a persistent left cranial nerve VI palsy and right-sided torticollis. She was successfully extubated after 9 days and was ultimately discharged to an inpatient rehabilitation facility on postoperative day 12. At time of discharge, the patient had residual neurologic deficits and torticollis, but no signs of hemorrhage or hydrocephalus via head computed tomography. Discharge medications included therapeutic enoxaparin for 6 months, vancomycin, ceftriaxone, and metronidazole for 6 weeks via a peripherally inserted central catheter, Flonase, and sinus rinses.
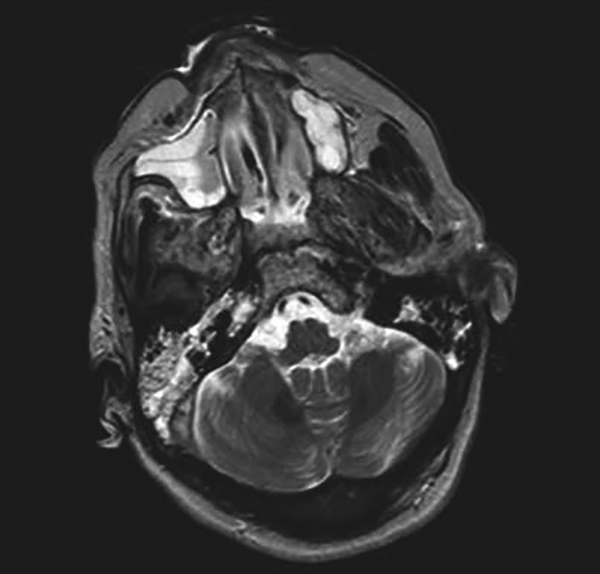
Figure 2
Postoperative axial T2 magnetic resonance imaging (MRI), showing decompression of the longus colli abscesses.
Discussion
We describe a patient with advanced bacterial pansinusitis complicated by bilateral longus coli muscle abscesses, bilateral cavernous sinus thromboses, superior ophthalmic vein thrombosis, and transverse sinus thrombosis. Although orbital and intracranial infections, CST, and RPA are well-known complications of ABRS, , the extension of infection into the longus colli muscles with development of abscesses has not previously been reported.
The longus colli muscles span the length of the neck from C1 to T3 as part of the anterior cervical prevertebral muscles and serve to flex and rotate the neck. , We postulate the bacteria spread from the sphenoid sinuses via direct adjacent extension, through the retropharyngeal space and prevertebral fascia, to seed within the longus colli muscle body. This is analogous to a Bezold’s abscess, a rare complication of acute otitis media, in which infection spreads through the mastoid to form an abscess within the sternocleidomastoid muscle. An alternative pathophysiology to consider would be septic phlebitic spread from the cavernous sinus into the longus colli muscles. However, our patient did not have septic emboli discovered elsewhere in the neck, and her longus colli abscesses were in distinct capsules adjacent to the purulent sphenoid sinuses on either side.
The few previous reports of acute inflammatory processes related to longus colli mostly described acute calcific tendonitis of longus coli, which is an aseptic process, without the rim enhancement via imaging characteristic of abscess collections. Inflammatory processes affecting the longus colli and longus capitis can manifest with neck pain, torticollis, rigidity, and dysphagia or globus sensation. Precautions for upper airway obstructions are typically indicated, requiring intubation and mechanical ventilation. Bacterial abscess formation within muscles involves a localized acute host inflammatory response, resulting in a peripheral fibroblastic capsule, necrotic center of leukocytes, live bacteria, and tissue debris, and the release of inflammatory cytokines and coagulases. Treatment, as exhibited in our case, includes abscess incision and drainage and administration of systemic antibiotics.
Another interesting point to consider is our patient’s severe disease presentation in the setting of COVID-19. The pandemic has led to wide reductions in hospital and clinic visits, with an estimated 40% of American adults delaying or avoiding medical care and 12% avoiding even urgent or emergency care. , Emergency department visits and 911 dispatch calls have each fallen over 30% in major cities. The delay in seeking essential treatments poses a superimposed threat of additional health consequences, especially for patients with chronic health conditions.
Conclusion
We describe the first case of bilateral longus colli abscesses as a complication of advanced ABRS and CST. This case highlights the advanced progression and a previously unreported complication of a common disease process. Increased clinical awareness and utilization of objective measures in critically ill patients can guide prompt interventions for future patients with a rapidly progressive clinical course.
Authors’ Note This report was considered IRB exempt by Vanderbilt University Medical Center, due to its nature as a clinical case report and not a research study.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
Jaclyn Lee
https://orcid.org/0000-0001-9804-6995
References
- 1. Plewa MC, Tadi P, Gupta M. Cavernous Sinus Thrombosis. StatPearls Publishing; 2020. Accessed May 5, 2021. https://pubmed.ncbi.nlm.nih.gov/28846357
- 2. Levine SR, Twyman RE, Gilman S. The role of anticoagulation in cavernous sinus thrombosis. Neurology. 1988;38(4):517–522. doi:10.1212/wnl.38.4.517
- 3. Jain H, Knorr TL, Sinha V. Retropharyngeal Abscess. StatPearls Publishing; 2020. Accessed May 5, 2021. http://www.ncbi.nlm.nih.gov/pubmed/28722903
- 4. Mnatsakanian A, Minutello K, Bordoni B. Anatomy, Head and Neck, Retropharyngeal Space. StatPearls Publishing; 2020. Updated July 27, 2020. Accessed September 26, 2020. https://www.ncbi.nlm.nih.gov/books/NBK537044/
- 5. Parson SH. Clinically Oriented Anatomy, 6th edition. J Anat. 2009;215(4):474. doi:10.1111/j.1469-7580.2009.01136.x
- 6. Koroulakis A, Agarwal M. Anatomy, Head and Neck, Lymph Nodes. StatPearls Publishing; 2020. Accessed May 5, 2021. http://www.ncbi.nlm.nih.gov/pubmed/30020689
- 7. Nasir F, Asha’ari ZA. Bezold’s abscess: a rare complication of acute otitis media. Malays Fam Physician. 2017;12(2):26–28.
- 8. Rahmanian R, Diamond C. Calcific tendonitis of the longus colli muscle: a noninfectious cause of retropharyngeal fluid collection. Case Rep Otolaryngol. 2014;2014. doi:10.1155/2014/286190
- 9. Shawky A, Elnady B, El-Morshidy E, Gad W, Ezzati A. Longus colli tendinitis. A review of literature and case series. SICOT J. 2017;3:48. doi:10.1051/sicotj/2017032
- 10. Kobayashi SD, Malachowa N, Deleo FR. Pathogenesis of Staphylococcus aureus abscesses. Am J Pathol. 2015;185(6):1518–1527. doi:10.1016/j.ajpath.2014.11.030
- 11. Czeisler MÉ, Marynak K, Clarke KEN, et al. Delay or Avoidance of Medical Care Because of COVID-19–Related Concerns — United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250–1257. doi:10.15585/mmwr.mm6936a4
- 12. Rosenbaum L. The untold toll—the pandemic’s effects on patients without Covid-19. N Engl J Med. 2020;382(24):2368–2371. doi:10.1056/nejmms2009984
- 13. KFF Health Tracking Poll – May 2020 – Health and Economic Impacts – 9474 | KFF. 2020. Accessed May 5, 2021. https://www.kff.org/report-section/kff-health-tracking-poll-may-2020-health-and-economic-impacts/
