Case Report
A 27-day-old female infant was born in another hospital on the 35th week of gestation, with unilateral CA. Respiratory distress and cyanosis were documented since birth. However, she was discharged at age 16 days and admitted to our hospital 11 days later.
On admission, she presented with short attacks of respiratory distress and cyanosis causing temporary oxygen desaturations (down to 75%) and severe feeding difficulties. She had no clinical or laboratory signs of infection (normal body temperature, blood tests, and chest X-ray) or cardiopulmonary insufficiency. Her echocardiogram showed a small atrial septal defect with a patent foramen ovale, with normal blood flows and pressures that did not explain the events. Head ultrasound and electroencephalogram were normal for her age. Fiberoptic nasoendoscopy demonstrated a unilateral left CA and normal right nasal and choanal passage. The pharynx and larynx looked normal, without adenotonsillar hypertrophy, but posterior commissure edema was apparent. Therefore, anti-reflux treatment was initiated together with topical nasal steroid drops. Later on, she underwent rigid laryngoscopy and flexible bronchoscopy, which showed no signs of tracheoesophageal fistula or laryngeal cleft, and a normal bronchial tree. A computed tomography (CT) scan of the head showed unilateral left CA and a patent right nasal and choanal passage (Figure 1).

Figure 1
Preoperative coronal (A) and axial (B) bone CT shows left choanal atresia (marked with arrows). Thickening of the vomer and medial bowing of the posterior maxilla are seen. The right nasal cavity appears normal. CT indicates computed tomography.
During 2 weeks of hospitalization, no improvement occurred with medical therapy and no other medical pathology was known to explain the clinical picture. She subsequently underwent endoscopic nasal surgery, to open and repair the left CA using posterior septal mucosal flap and placement of an intranasal stent. The desaturation attacks ceased immediately, and feeding improved markedly (Figure 2).
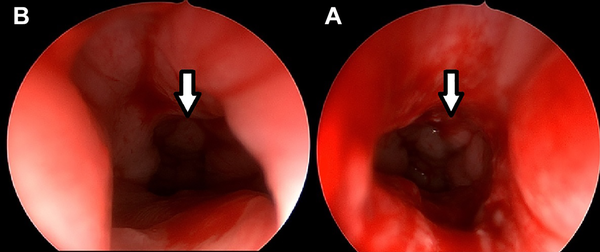
Figure 2
Postoperative photographs. The repaired left choanal atresia (A) and the patent right choanal passage (B). Arrows are pointing to the choanal passages and the nasopharynx.
After 3 more weeks, the stent was removed under general anesthesia, with re-debridement of granulation tissue on the left choana. The patient was discharged without respiratory or feeding problems and had no signs of recurrent attacks on follow-up examinations.
Discussion
Unilateral CA generally does not cause respiratory distress in the neonatal period. Therefore, surgical treatment is usually delayed; this enables growth of the nasal cavity and reduces the risk of postoperative complications and restenosis.
Our patient presented with a unique condition of unilateral CA, characterized by congenital recurrent cyanotic episodes and respiratory distress, which typically presents in bilateral CA. The inability to breathe normally through the right open nasal passage could not be explained by any central or peripheral reason.
We recently described 2 patients with unilateral CA and contralateral mid-nasal stenosis that caused congenital dyspnea. For these patients, a pediatric fiberoptic nasal endoscope could not be passed on both sides of the nose. The obstruction was also observed on CT examination. The symptoms due to the mid-nasal stenosis improved after several days of conservative topical steroid treatment, while the CA was treated later. However, unlike the patient described in the present report, those babies showed problems of both nasal passages, on physical examination and CT scans.
To the best of our knowledge, no patient was previously reported with a unilateral CA and a patent contralateral nasal airway, presenting with respiratory distress and recurrent cyanotic episodes. In a systematic review of surgeries performed for congenital CA, only 4 (8 neonates) of 23 reports described surgeries for congenital unilateral CA done in the neonatal period. None of these publications specified the reason for the very early operation for unilateral CA. - International Pediatric Otolaryngology Group consensus recommendations stated that the timing of surgery for unilateral CA should be delayed at least to after the age of 6 months, ideally to 1 year or more. The recommendations addressed the possibility of respiratory distress, which may prompt an earlier surgery; however, specific reference to such an occurrence was not provided. This contrasts with an earlier review that stated that children with unilateral CA do not have medical emergencies, and surgical treatment may always be delayed.
To the best of our knowledge, no patient was previously reported with a unilateral CA and a patent contralateral nasal airway, presenting with respiratory distress and recurrent cyanotic episodes. Therefore, both neonatologists and otolaryngologists should be aware of this extremely rare possibility.
Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding The author(s) received no financial support for the research, authorship, and/or publication of this article.
Dror Gilony
https://orcid.org/0000-0002-7802-9589
References
- 1. Elluru RG. Congenital and acquired malformations of the nose and nasopharynx. 7th ed. Cummings Otolaryngology. 2020;190:2859–2870.
- 2. Levi L, Kornreich L, Hilly O, Raveh E, Gilony D. Clinical and imaging evaluation of congenital midnasal stenosis. Int J Pediatr Otorhinolaryngol. 2020;132:109918. doi:10.1016/j.ijporl.2020.109918 Epub February 1, 2020
- 3. Murray S, Luo L, Quimby A, Barrowman N, Vaccani JP, Caulley L. Immediate versus delayed surgery in congenital choanal atresia: a systematic review. Int J Pediatr Otorhinolaryngol. 2019;119:47–53.
- 4. Uzomefuna V, Glynn F, Al-Omari B, Hone S, Russell J. Transnasal endoscopic repair of choanal atresia in a tertiary care centre: a review of outcomes. Int J Pediatr Otorhinolaryngol. 2012;76(5):613–617.
- 5. Schwartz ML, Savetsky L. Choanal atresia: clinical features, surgical approach, and long-term follow-up. Laryngoscope. 1986;96(12):1335–1339.
- 6. Lazar RH, Younis RT. Transnasal repair of choanal atresia using telescopes. Arch Otolaryngol Head Neck Surg. 1995;121(5):517–520.
- 7. Gordts F, Clement PA, Rombaux P, Claes J, Daele J. Endoscopic endonasal surgery in choanal atresia. Acta Otorhinolaryngol Belg. 2000;54(2):191–200.
- 8. Moreddu E, Rizzi M, Adil E, et al. International pediatric otolaryngology group (IPOG) consensus recommendations: diagnosis, pre-operative, operative and post-operative pediatric choanal atresia care. Int J Pediatr Otorhinolaryngol. 2019;123:151–155.
- 9. Corrales E, Koltai PJ. Choanal atresia: current concepts and controversies. Curr Opin Otolaryngol Head Neck Surg. 2009;17(6):466–470.
